Abstract
Purpose: To develop and evaluate an interdisciplinary group intervention for patients with myotonic dystrophy regarding healthy nutrition, meal preparation, and consumption, called Meet and Eat.
Materials and methods: A design-based approach was used, exploring experiences and needs of patients with myotonic dystrophy and their next of kin. This resulted in a 4-week interdisciplinary outpatient group intervention to increase awareness and change behavior. In a mixed-method feasibility study this intervention was evaluated with participants and facilitators.
Results: Participants reported on social impact of difficulties with eating and drinking (speaking, swallowing, and social embarrassment) and a variety of complaints affecting meal preparation and consumption. Patients and family members expressed the wish to learn from others. After delivery of the intervention, self-reported outcome measures demonstrated improvement on eating and drinking issues in daily life. The qualitative evaluation showed increased awareness and appreciation of the following design principles: peer support, multidisciplinary approach, active involvement of patient with myotonic dystrophy and their next of kin by using personal goals and motivational interviewing.
Conclusion: Participation in Meet and Eat seemed to increase insight in patients’ condition and ways of management. However, a longer self-management life style program is recommended to change behavior.
Patients with myotonic dystrophy experience physical, cognitive and psychosocial problems to manage healthy nutrition, meal preparation, and consumption;
This multidisciplinary group intervention Meet and Eat in patients with myotonic dystrophy appears to be feasible and seems to result in increased insight and management strategies;
Peer support, multidisciplinary approach, personal goals, and involvement of family were key factors;
To change eating and drinking behavior, a 4-week intervention is too short.
Implications for rehabilitation
Introduction
Myotonic dystrophy type 1 (DM1), or Steinert’s disease, is a slowly progressive neuromuscular disease characterized by muscular weakness, myotonia, and additional multisystem disorder symptoms including internal, cardiovascular, ophthalmic, cognitive, and effective changes. DM1 is one of the most common adult forms of muscular dystrophy, with a prevalence of approximately 10 per 100,000 people affected [Citation1–4]. The diversity and complexity of symptoms in patients with DM1 often lead to difficulties in the accomplishment of daily activities and participation, including preparing and eating nutritious meals [Citation5,Citation6].
One of the most critical and life-threatening problems is dysphagia, defined as difficulty swallowing foods or liquids safely, which may result in malnourishment or an aspiration pneumonia or may even result in choking and sudden death [Citation7,Citation8]. Dysphagia in DM1 is aggravated by poor understanding and late subjective perception until advanced stages of the disease. Dysphagia is common in DM1 and may affect between 25 and 80% of the patients [Citation7,Citation8]. At our outpatient clinic at Radboudumc, dysphagia is present in 86% of the patients with different neuromuscular diseases, including patients with DM1 [Citation9,Citation10].
Besides dysphagia, other gastrointestinal involvement and complications like constipation or diarrhea are often reported [Citation11]. Due to metabolic alterations, there is a higher risk of underweight and overweight, stressing the need to strive for healthy nutrition and eating behavior [Citation12].
In addition, poor diet choice is common in patients with DM1, possibly due to poverty and food insecurity (lower food expenditures, low fruit and vegetable consumption and lower quality diets). More particularly, patients with DM1 have generally higher fat and carbohydrate intake than the daily intake recommendations [Citation5,Citation13]. The prevalence of unhealthy lifestyle risk factors, poor social, and economic status prevailing in DM1 is related to the severity of the disease [Citation14].
At the level of occupational performance and participation, patients with DM1 experience several problems that influence meal preparation and consumption. These vary from difficulties deciding and planning what to eat, difficulties doing the shopping and cooking and avoidance of social participation such as having dinner in a restaurant [Citation6]. Relationships with caregivers may also be negatively affected by an individual’s inability to share meals. These participation problems gradually increase and affect daily life of patients with DM1, and next of kin even more than the symptoms [Citation6,Citation15].
Over the past decade, all the above-mentioned symptoms and problems have been assessed and recognized during consultations of over 100 DM1 patients at the neuromuscular expert and consultation center at the Radboud University Medical Center Nijmegen (Radboudumc) [Citation9,Citation10]. Although prevalent, serious and urgent, the complex problems related to nutrition, meal preparation and consumption may be hidden, due to lack of awareness and understanding. As described in a previous study, individuals with DM1 may minimize their symptoms. This may impact their ability and/or willingness to recognize and manage problems related to healthy nutrition, meal preparation and consumption [Citation16].
Despite our vast clinical experience, concerns and willingness to address these problems, it was felt that patients’ needs and experiences needed to be the starting point to develop an intervention. Therefore, aims of current study were to:
Evaluate patients’ experiences of these multisystem implications related to nutrition, meal preparation and consumption in daily life.
Develop and test an innovative integrated interdisciplinary group intervention called Meet and Eat with focus on strengthening the remaining health potential combining efforts to increase awareness, change behavior and create healthy environments.
Methodology
Design
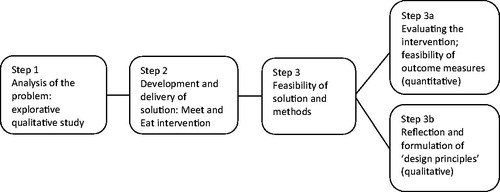
A pragmatic approach was used by designing an intervention, grounded in theory, clinical observations and patient experiences [Citation17]. A variety of research methods was used from both qualitative and quantitative research paradigms, following the steps of design-based research, as demonstrated in [Citation18].
At first a qualitative study explored the experiences and needs of patients with DM1 and their next of kin (step 1). Subsequently, an interdisciplinary outpatient group intervention called Meet and Eat was developed (step 2) to address issues raised in step 1 to promote healthy nutrition, meal preparation and consumption. Finally, the Meet and Eat intervention was tested for its feasibility (step 3). The feasibility of self-reported quantitative outcome measures was explored (step 3a) as well as reflections of participating patients with DM1 and the allied healthcare providers on the content and organizational aspects of the intervention (step 3b).
Step 1. Analysis of the problem: explorative qualitative study
Participants
Patients with DM1, and a family member if available and willing to participate, were recruited through purposive sampling from the patient list of the neuromuscular expert and consultation center of the Radboudumc. In this center, every week one patient with a neuromuscular disease, mainly myotonic dystrophy, is admitted for extensive interdisciplinary screening and advice. Inclusion criteria were: (1) genetically diagnosed with DM1, (2) willing to share their experiences and needs, (3) aged 18 years or over, and (4) able to understand written and spoken Dutch. Informed consent was given by all participants before each step and ethical approval was received from the Medical Ethics Committee of Radboudumc (registration number 2014/1327 and 2016/2809). Participants were approached by an information letter, followed by a telephone call one week later to ask if they were willing to participate.
Procedure and data collection
Semi-structured interviews lasting 30–60 min were conducted with the patients and, if available, a family member. The topic list included questions about experiences, routines and problems concerning nutrition, preparing meals, eating and drinking, social part of eating and drinking as well as possible needs of the patient with DM1 or family member related to these topics. Interviews were conducted by research assistants at the participants’ home with the patients and family member at the same time. They were trained by experienced qualitative researchers (EC + TS).
Data analysis
All interviews were transcribed by the research assistants and were analyzed with supervision of senior researchers (EC + TS) using a qualitative inductive approach to aid an understanding of meaning in complex data through the development of summary themes from raw data [Citation19]. The analysis process included open, axial and selective coding, with use of data analysis software program Atlas.Ti 7.1.5. After coding and categorizing, the findings were discussed with senior researchers which supported the process of the themes to emerge.
Step 2. Development and delivery: intervention meet and eat
Based on the results of the study in step 1, a meeting was organized between representatives from the DM1 patient support organization (three patients with DM1, one parent of two daughters with DM1 and a policy advisor) and two allied health professionals from the neuromuscular expert and consultation center of the Radboudumc (occupational therapist EC and speech therapist SK). The representative’s advice was to pursue the development and evaluation an interdisciplinary intervention addressing problems related to healthy nutrition, meal preparation, and consumption even though patients that were interviewed did not express the need or urgency. Next, an expert meeting took place with experienced healthcare professionals (physician, occupational therapist, speech-language therapist, and dietician) to design and develop an interdisciplinary outpatient group intervention called Meet and Eat. Input from the representatives and the expert meeting led to an intervention containing aspects of group therapy, self-management interventions, and motivational interviewing [Citation20–23]. Two manuals were produced by SH, SK, and HD, one for therapists as facilitators and one for participants. The manuals were again discussed and revised by the members of the expert meeting.
Step 3. Pilot testing of solution and methods (feasibility study)
Participants
Again, a convenience sample of patients with DM1 was approached via nurses and physicians at the neuromuscular expert and consultation center of the Radboudumc. Flyers about the intervention were put in the waiting rooms and handed out by the neurologist and rehabilitation physician. Patients with DM1 of whom the clinicians thought they might benefit from such an intervention were approached by the therapists who facilitated the Meet and Eat intervention. Of the 13 patients approached, 5 responded to participate in this feasibility study. Other patients indicated that they could not get time off work or did not have transport to attend to the sessions. Similar inclusion criteria as in step 1 were used, and in addition, they had to be willing to participate in the feasibility study. By phone the content and procedure of the intervention was explained and one could decide to participate up to two weeks before the start of the intervention. All participants received a short (A4) notice one week in advance about the content, schedule and location of the Meet and Eat intervention.
Step 3a. Testing the intervention: outcome measures (quantitative)
Data collection
A small-scale study was performed to evaluate the feasibility of the Meet and Eat intervention and the feasibility of the outcome measures. All outcome measures were administered before (t0) and two weeks after (t1) the intervention.
The Dietary History [Citation24,Citation25] was used to assess the food intake of patients with DM1. A tailored swallowing questionnaire was developed. Because of the specific focus of Meet and Eat, we hypothesized that none of the existing questionnaires was sensitive enough to measure changes. Thirteen questions were gathered from the M.D. Anderson dysphagia inventory (MDADI) [Citation26] (i.e., my swallowing ability limits my day-to-day activities), the Dysphagia Handicap Index (DHI) [Citation27] (i.e., I don’t enjoy eating as much as I used to) and the Swal-qol [Citation28] (i.e., it is a problem to find out what I can eat). The questions were scored on a four-point Likert scale ranging from “always experiencing problems” to “never experiencing problems”.
The Canadian Occupational Performance Measure (COPM) [Citation29] was used to evaluate occupational performance and satisfaction of self-reported priorities in occupations regarding nutrition, meal preparation and consumption.
Data analyses
Data were analyzed descriptively (frequencies, means) using IBM SPSS Statistics 23 (IBM Corp., Armonk, NY). No statistical tests were used because of the small number of participants in the feasibility study.
Step 3b. Reflection on the intervention and formulation of “design principles” (Qualitative)
Procedure and data collection
Participants, one family member and facilitating healthcare professionals were interviewed within 2 weeks after the intervention. The topic list contained topics regarding the experience of the intervention, as well as recruitment, reason for participation, organizational and delivery aspects of intervention, expertise of facilitators, used materials, relevance of content, implementation of learned lessons in daily life, and self-reported behavioral change. Research assistants were trained in interviewing by an experienced qualitative researcher (SH).
Data analyses
Qualitative data were analyzed using qualitative inductive analyses [Citation19] including open, axial and selective coding, with support of data analysis software program Atlas.Ti 7.1.5. All transcripts were read by SH and a subsample was read by SK. After discussion (SH, SK, EC) a coding frame was developed and the transcripts were reread and coded by SH. This rigorous and systematic reading and coding of the transcripts allowed major themes to emerge. These themes led to “design principles”, according to the design-based approach of this study [Citation17,Citation18].
Results
Step 1. Analysis of the problem: Explorative qualitative study
Characteristics of participants
Participants
Nine patients with DM1 participated, four women and five men, age ranging from 31 to 68 years and mean age of 45. All had a genetically confirmed DM1, of whom two had a juvenile type of MD1. Most participants had complaints varying from mild to severe swallowing problems including frequent choking incidents. Other clinical complaints included bowel complaints and sometimes problems of incontinence, fatigue and daytime sleepiness, diminished hand function, and myotonic flexors of the underarm. Also, some mild frontal cognitive impairments were described including lack of initiative. So, although the genetic diagnosis was myotonic dystrophy type 1 for all nine participants, the clinical complaints varied. Six participants lived with at least one family member. Seven family members participated, two mothers, two wives, and three husbands.
Analysis of the data led to four themes, described below and illustrated with quotations.
Mixed feelings regarding eating and drinking as a social moment
Meals were often reported as a social moment, where speaking and safe swallowing at the same time is a challenge: “it goes wrong every time, when I try to speak. I then choke continuously”. Most participants reported they should focus on one thing at the time and were therefore less involved in conversations during meals. Being social during meals with others than family members was of great importance for the participants. Some participants reported social embarrassment to eat with others, “as I will eat less because I am slower than others, especially when the others do not know about my problem”. Besides, not going out for dinner was mentioned, because of the cosmetic changes due to DM1 and fear for incontinence. The experience of “being afraid when I am at a public place to get abdominal pain and in need of a toilet nearby” was regularly reported. Strategies are to eat less or not at all to prevent “accidents”. Some patients with DM1 use medication to reduce their gastrointestinal complaints. However, those strategies are not perceived as resolved thereafter. Others reported how eating with others is also encouraging, to eat more or being more relaxed when eating. Family members reported no social obstructions as they mainly expressed their support.
Other complaints affect eating and healthy meal preparation
Abdominal pain, diarrhea, and constipation were reported by most participants. The majority reported either underweight or overweight as challenges related to their nutrition. Fatigue was mentioned by participants to highly influence body weight and swallowing, “I wish to eat more but eating more means chewing and swallowing more, and that makes me very tired”. Most family members expressed fear for choking while eating. Also, to plan and prepare a healthy meal is challenging, as one family member cited “when it will be an easy meal my wife [with DM1] will cook it, but once it becomes a bit more complicated I will take over the cooking”.
Ways to manage eating pace, swallowing, and handling tools for eating
Patients with DM1 mentioned to eat slower and reported to manage themselves well, especially at home. Family members reported how they got used to the eating pattern and adjustments during the meals, for example, the choice of food that is easier to chew and swallow. Besides, more time needed for eating was reported by family members as a change, however “this becomes part of our daily routine, the speed of eating might be different but we are all used to it and it is necessary, so that’s just how it is”. Patients with DM1 also report the adjustments and tools they use to prepare and eat food, mostly due to “reduced power to open cans or need for thicker grip of utensils”. Other reported adjustments were to chop and eat food in small portions, to replace fresh fruit by juices and to position oneself properly when seated on the dining chair.
Wishes for treatment or advice
In general, participants reported a high satisfaction of the adjustments they made to optimize their eating habits and felt no direct need for coaching or therapy. On the other hand, they said they would like to hear experiences and tips from others with DMI how to lose or gain weight, whether to use food supplements, how to improve swallowing or what practicalities are in meal preparations. “It is good to hear how others handle similar problems”. Family members surely wished to receive support on instructions for themselves and their relative with DM1. One expressed “We explored everything over time and by attending the consultations with the clinicians, but it would be good that one does not need to explore everything on his own”. Moreover, they wished to be prepared for the future problems, especially choking.
Step 2. Development and delivery of solution: intervention meet and eat
The themes of the explorative study (step 1) were taken into account for designing the intervention. The Meet and Eat intervention was designed as an interdisciplinary outpatient group intervention. This intervention aimed to raise awareness, to increase disease-related knowledge, and self-management skills to promote healthy dietary behavior. The specific aims of the intervention are presented in .
Table 1. Aims of the intervention Meet and Eat.
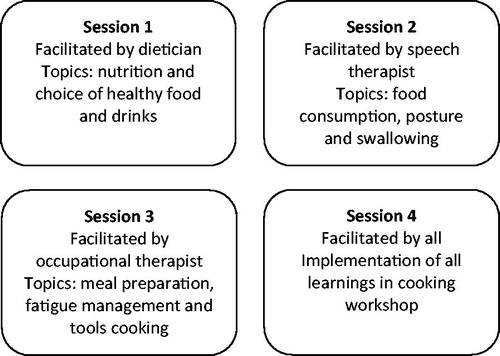
The intervention consisted of four group sessions, each session lasting two hours, see . All sessions were facilitated by the allied health professional specialized in that particular topic. However, to ensure the interdisciplinary approach towards raised topics all facilitators were present during each session. A highly interactive character was given to the group sessions. Each participant in the intervention was encouraged to invite his or her next of kin to participate as well.
Step 3. Pilot testing of solution and methods (feasibility study)
Step 3a. Testing the intervention: Outcome measures (Quantitative)
Characteristics of participants in the Meet and Eat intervention
Five patients with genetically confirmed DM1 (two had the juvenile type, three the adult type), who did not participate in step 1, participated in the intervention. One men and four women ranging from 25 to 43 years of age (mean age 33), of whom all but two were living with others. Family members were committed to join, however, the frequency and time schedule (during office hours) made it only feasible for one family member to attend the sessions. This family member was the mother of one participant.
Participants’ goals for the meet and eat intervention
Participants were assessed using motivational interviewing to explore their motivation to participate in this group intervention. The COPM was administered with all participants to identify the occupational performance priorities regarding eating and drinking and meal preparation. Based on these priorities, personal goals were formulated on what the participants wished to achieve. Most participants wished to receive general information on the management of daily life problems related to a healthy diet, meal preparation, and eating. Specific goals of participants included “finding an alternative for sugary unhealthy snacks and emotional eating”, “reduce the amount of choking during dinner”, “eating at a slower pace”, “having a healthy diet to feel less tired all the time”, “cooking simple fresh meals and reduce the amount prepared meals”, and “being able to peel potatoes by myself”.
Exploration of outcomes of Meet and Eat Intervention
Dietary history
Mean dietary intakes from the participants differed slightly (1605 Kcal per day) from the population norm (1700–2500 Kcal per day) [Citation30], with a lower energy, protein and fiber intake. Means of carbohydrates, fiber and fats slightly changed after the intervention, with a decrease of intake of carbohydrates and fiber below the population norm, and an increase of fats in line with the norm.
Swallowing questionnaire
At t0, participants did not report a lot of problems regarding swallowing, except for the time it takes to eat a meal. At t1, no obvious differences were reported.
COPM
After intervention, three participants improved 1.0 or 2.0 points on the COPM performance scale, see . One participant had no change in performance score and one participant demonstrated a decrease of 0.8 points. All but one demonstrated improvement on COPM satisfaction (range 0.7–2.2 points). A clinically relevant change of 2 points on a COPM performance or satisfaction scale was reached in two participants.
Table 2. Results COPM, mean performance and satisfaction scores per participant and difference before and after intervention.
Step 3b: reflection on the intervention and formulation of “design principles” (Qualitative)
Participants
Participants were the same patients as in step 3a. One family member participated in this step to share experiences. Facilitators were the healthcare professionals who delivered the Meet and Eat intervention: a dietician, a speech-language therapist and an occupational therapist. Analysis led to the following themes from participants’ (including family member) and facilitators’ reflections on the Meet and Eat intervention.
Relevant information and raised awareness by Meet and Eat intervention
Participants
All patients with DM1 reported that covered topics in the four sessions were relevant and useful for them. The participants expressed that they were satisfied that their reported problems and goals in the COPM interview prior to the intervention were tailored in the sessions. However, participants reported not yet to need all the given information and some “already found a solution, for example sitting down and taking time to chop the vegetables is what I usually do to save energy while cooking”. The last session (workshop) was perceived as useful to integrate all received advises, especially “to try aids and ways to make cooking easier and still healthy, and it gave me some new recipes”. The family member appreciated the sessions as well, “as I was surrounded by all persons with DM1, I fully imagined how this condition feels for my relative, and I will be more able to advise her at home also about eating”. The given homework, for example, to photograph one self’s posture when eating, was not considered to have additional value. A participant expressed: “I am not at secondary school here, but I understand why they asked us”. Reported benefits of this intervention were the information about tools for cooking and to which therapy the participants could go with certain complaints. The program also led to raised awareness. For example, about certain ingredients and posture, “I am more conscious now on my posture when I am eating but I did not yet experience problems with swallowing”.
Facilitators
Four sessions were experienced as adequate to provide relevant information and to raise awareness. “It was good to know the goals of each participant so we could adjust the content mostly to what they wished to achieve”. All facilitators agreed that two hours per session was quite short. “Our aim was now to start with general information about healthy food related to their goals, but if we would have had more time we could have gone deeper into discussion of specific soft and still healthy foods”.
Learning from peers and feeling heard by the therapists
Participants
Being in a group was experienced as very useful. As one participant expressed: “to talk about it with others was good since they have more or less the same problems and solutions for some things”. All participants appreciated the dedicated attitude of therapists and the open and relaxed atmosphere during sessions. They could openly discuss their personal issues. A participant reported “Many persons with DM1 will always say to the clinician they have no complaints, that’s because it all comes so gradually that you forget it is because of the dystrophy. But when you hear others with the same complaints, then you can feel like yeah I need to ask or do something about this”. Especially acknowledgement of existing problems and room for discussion was perceived as valuable, as one participant mentioned: “I did not expect to share my own experiences as much as we did, that was a good way to also remember the information we received, better when you really discuss and practice it”. Four of the five participants wished to have a review meeting one or two months after the intervention, “to hear how they experienced the changes after the program”.
Facilitators
All facilitators positively reported about how participants learned from each other, “participants had a very active input and even without really noticing they advised each other mostly on the topics we raised”. Another therapist reported “Look, as a health care professional it is often hard to really help patients with DM1 due to sometimes rigid responses and little flexibility, although we try so hard by using the right motivational interviewing techniques. But if you are in the same position [peers], you just say it and the other takes it for true”. The interdisciplinary setup was “very good, we could add upon each other’s ideas and it helped to make given ideas more applicable at home”. Collaboration and input of all facilitators was reported as positive, with willingness to deliver this intervention again.
Good delivery of the intervention but more information in advance is needed
Participants
Three out of five participants were satisfied about the time and length of the four sessions. Two would prefer the sessions to take place in the morning due to fatigue. The frequency of once a week, was felt to be satisfactory. Two participants suggested to reflect shorter on the learned lessons the week before but to rather have more time for the topic of that session. Used location and materials were reported as adequate, without suggestions. Four of five participants wished to have received more specific information in advance about the content of the intervention, “Since many persons with DM1 have difficulties with information processing and remembering”.
Facilitators
The recruitment method (phone calls, flyers and announcement by clinicians) felt adequate. All facilitators agreed that patients with DM1 are not an easy target group to recruit due to the tendency of underreporting their complaints. One facilitator reported that “more time and more detailed information should be provided to prepare participants and their family members. If we want family members to join, we need to organize it differently, for example to motivate clearly why they should attend, or maybe doing the intervention during weekend hours”. They emphasized the value of the presence of family members during this intervention due to their important role on early identification and influencing healthy nutrition as well as meal preparation and consumption. Family members could not all avail themselves for the sessions.
This intervention is good for raising awareness in early stage of diagnosis
Participants
Participation in this intervention was generally driven by getting information, rather than the need for behavioral change, “we got useful advice but I am not yet sure if I will really change what I eat because I am not unhealthy really”. Most participants reported the information “good to have when you are recently diagnosed with DM1 because then you don’t know yet that swallowing or reduced hand function can be a problem”. It appeared that the participants in current feasibility study already knew quite a lot. All participants reported to recommend this intervention to other persons with DM1, “especially for those who really experience problems with eating, weight, swallowing or preparing food”.
Facilitators
All facilitators would recommend this intervention to patients with DM1 and to other professionals to refer patients for this group intervention. For a next intervention, “I would design two different interventions, one like this for patients who are recently diagnosed with DM1, and one more comprehensive self-management program that takes longer. And that should include more specific goals about eating patterns and life style”. All facilitators agreed to continue using motivational interviewing, “it was valuable to score how important it is for the person to change”.
Discussion
The aim of this project was to make a first step towards the development and evaluation of an interdisciplinary outpatient group intervention regarding healthy nutrition, meal preparation and consumption for DM1 patients and their family members. The themes of the explorative study (step 1) that were taken into account for designing the intervention (step 2) were: (1) mixed experience on social eating and drinking because of the difficulties with speaking and swallowing at the same time and social embarrassment, (2) other complaints affecting meal preparation and consumption including gastrointestinal problems, weight management, fatigue, reduced initiative, and executive problems in relation to complexity of meal preparation, (3) ways to manage their issues, and (4) wishes of participants and their next of kin to receive support and advice, especially from others with DM1. Reports of experiences in this explorative study overlapped between the patient with DM1 and their next of kin which is in line with other studies [Citation7,Citation16,Citation31]. Patients with DM1 tend to minimize their symptoms, and generally seem indifferent about their health [Citation7,Citation16]. Other studies reported that patients with swallowing or gastrointestinal problems themselves do not directly relate these to DM1, but in presence of family members during the consultation, a clear history of these problems is often reported [Citation32,Citation33]. This is a well-known mechanism in DM1 patients: physicians and therapists share concerns of underreporting complaints.
Beside the expressed problems of patients with DM1, the design of the intervention was also based on clinical experience of healthcare professionals and other self-management programs. Included were principles of goal setting, that is incorporated as an important feature where personalized information could apply easily to oneself as appropriate [Citation23]. One other principle to improving care for DM1 patients regarding behavioral or dietary modifications was to educate family members by including them in the assessment and management process of DM1 as they can positively influence the occupational performance of activities [Citation7,Citation8]. The results of our study underline the importance of involvement of family members in such an intervention, however organizational aspects to enable their participation need attention.
Outcome measures of the feasibility study of the Meet and Eat intervention (step 3a) were aimed to measure a behavioral change. The COPM appeared a feasible outcome measure to measure a self-reported change, especially on satisfaction with daily occupational performance. The dietary history did not show remarkable differences pre- and post-intervention which might be due to the short nature of this intervention to measure a different pattern in diet in a total time scope of 7 weeks (1 week before intervention, 4-week intervention and 2-week post-intervention). The swallowing questionnaire did not show large differences pre- and post-intervention, maybe due to the fact that we didn’t use a valid questionnaire. Other outcome measures on chewing and swallowing are needed for future research. Reflecting on this intervention, outcomes resulted more in awareness raising, rather than behavioral change, and therefore outcome measures should be reviewed. Also, a longer follow-up is needed to actually measure behavioral change [Citation34].
The qualitative evaluation of the feasibility study of the Meet and Eat intervention (step 3b) revealed positive experiences with full compliance of the participants as opposed to the often-poor adherence to healthy lifestyle behaviors [Citation14]. Participants in this study recommended an intervention like this to others, especially in early stages of the onset of the disease. It is an often-heard response from patients with DM1 that they manage themselves and have no need for support. However, if support is given in the “right” manner, it can be highly appreciated [Citation6]. Current experiences confirmed that the participants appreciated the Meet and Eat intervention, as it provided them with “relevant information and raised awareness and they appreciated learning from peers and feeling heard by dedicated therapists". Still, they typically articulated that it was especially useful for others who experience more problems or at an earlier stage of being diagnosed. Besides, the consultation within the team and expressing consistent messages including additional information from different professional perspectives might have positively affected the self-management skills of decision making. Decision making is based on having enough and appropriate information [Citation23]. A group intervention with DM1 patients seems promising in a short life style intervention like Meet and Eat, compared to an individual clinical consultation. As recommended by another study in development of group interventions for patients with DM1, information exchange among fellow patients, peer support, and sharing of experiences were felt as positive [Citation20]. Moreover, the increased time to inform patients in a group and ability to attend to psychosocial aspects seemed well incorporated in this intervention [Citation20]. Lastly, participation in a program like Meet and Eat seemed to increase insight in patients’ disease and ways of management. The low-profile exposure to professionals who are specialized in DM1 management may increase health-seeking behavior, that is often influenced by cognitive impairment and avoidant personality [Citation35,Citation36].
Strengths and weaknesses of the design and evaluation
Multiple data resources were used in this project to develop and evaluate an intervention, including perspectives of several patients with DM1, family members and multidisciplinary team of healthcare professionals. Besides, the different methods used, namely expert meeting, interviews, quantitative outcome measures pre-and post-intervention and observation during the interventions imply a high variety of perspectives and evidence in this study. Besides, to achieve high adequacy of data, we used purposive sampling of both family members and patients with DM1, resulting in rich descriptions of participants’ experiences. Both the variety of perspectives and evidence increase the trustworthiness of our findings [Citation37]. Nevertheless, there are some limitations due to the methods of recruitment and data collection.
During recruitment of participants and family members for the explorative study in step 1, we selected patients’ own family members. The concerns of family members often mirror those of patients because complaints evolve gradually [Citation7]. To gain a wider perspective of concerns, including other family members than family members of those patients with DM1 in this study, could have diminished this selection bias. Besides, interviews in step 1 and step 3 b were conducted with patients with DM1 and the family member in the same conversation. Conducting the interviews at home but in a separate conversation for both participants and their family members would reduce the response bias, especially on the experiences of family members whom often experience more burden than the patients with DM1 themselves [Citation38].
Conclusions
In summary, we obtained valuable insights from this study in the development of a interdisciplinary outpatient group intervention, Meet and Eat, to promote healthy nutrition and reduce problems in meal preparation and consumption. Design principles for such an intervention were: sessions in a group setting, interdisciplinary approach and active involvement of the patient with DM1 and his or her next of kin using goal setting and motivational interviewing. Future research might consider an assessment of patients’ condition-specific knowledge and self-management skills as this is the aim of the current short program. A distinction between a short preventive and informative intervention and a more extensive self-management program to change behavior and life style is recommended. Both types of interventions warrant further attention to positively impact health at the level of daily functioning and participation of patients with DM1.
Acknowledgments
The authors greatly acknowledge the time and willingness of patients with DM1 and family members to participate in the interviews and the intervention. We would like to thank the students from the Bachelor program of food and dietetics, speech-language therapy and occupational therapy of the HAN University of Applied Sciences, Nijmegen, who assisted in data collection especially their interdisciplinary teamwork during the development of research methods.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Harper P. Myotonic dystrophy: a multisystemic disorder. In: Harper P, Van Engelen B, Eymard B, Wilcox D, editors. Myotonic Dystrophy: present management, future therapy. Oxford: Oxford University Press; 2004. p. 3–13.
- Antonini G, Soscia F, Giubilei F, et al. Health-related quality of life in myotonic dystrophy type 1 and its relationship with cognitive and emotional functioning. J Rehabil Med. 2006;38:181–185.
- Gallais B, Gagnon C, Mathieu J, et al. Cognitive decline over time in adults with myotonic dystrophy type 1: a 9-year longitudinal study. Neuromuscul Disord. 2017;27:61–72.
- Norwood FL, Harling C, Chinnery PF, et al. Prevalence of genetic muscle disease in Northern England: in-depth analysis of a muscle clinic population. Brain. 2009;132:3175–3186.
- Motlagh B, MacDonald JR, Tarnopolsky MA. Nutritional inadequacy in adults with muscular dystrophy. Muscle Nerve. 2005;31:713–718.
- Cup EH, Kinebanian A, Satink T, et al. Living with myotonic dystrophy; what can be learned from couples? A qualitative study. BMC Neurol. 2011;11:86.
- LaDonna KA, Koopman WJ, Ray SL, et al. Hard to swallow: a phenomenological exploration of the experience of caring for individuals with myotonic dystrophy and dysphagia. J Neurosci Nurs. 2016;48:42–51.
- Timman R, Tibben A, Wintzen AR. Myotonic dystrophy: the burden for patients and their partners. J Rehabil Med. 2010;42:823–830.
- Knuijt S, Kalf JG, de Swart BJ, et al. Dysarthria and dysphagia are highly prevalent among various types of neuromuscular diseases. Disabil Rehabil. 2014;36:1285–1289.
- Seijger CG, Drost G, Posma JM, et al. Overweight is an independent risk factor for reduced lung volumes in myotonic dystrophy type 1. PLoS One. 2016;11:e0152344.
- Hilbert JE, Barohn RJ, Clemens PR, et al. 3rd and others. High frequency of gastrointestinal manifestations in myotonic dystrophy type 1 and type 2. Neurology. 2017;89:1348–1354.
- Cruz Guzmán O. d R, Chávez García AL, Rodríguez-Cruz M. Muscular dystrophies at different ages: metabolic and endoncrine alterations. Int J Endocrinol. 2012; 2012:1.
- Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16.
- Gagnon C, Chouinard MC, Laberge L, et al. Prevalence of lifestyle risk factors in myotonic dystrophy type 1. Can J Neurol Sci. 2013;40:42–47.
- Natterlund B, Sjoden PO, Ahlstrom G. The illness experience of adult persons with muscular dystrophy. Disabil Rehabil. 2001;23:788–798.
- Meola G, Sansone V. Cerebral involvement in myotonic dystrophies. Muscle Nerve. 2007;36:294–306.
- Van den Akker J, Gravemeiger K, McKenney S, et al. Introducing Educational Design Research. In: Van den Akker J, Gravemeiger K, McKenney S, Nieveen N, editors. Educational design research. London: Routledge; 2006.
- Reeves TC. Design research from a technology perspective. In: Van den Akker J, editor. Design methodology and developmental research in education and training. The Netherlands: Kluwer; 2006. p. 52–66.
- Saunders M, Lewis P, Thornhill A. Methoden en technieken van onderzoek. Amsterdam: Pearson Education Benelux; 2004.
- Seesing FM, Groenewoud HJ, Drost G, et al. Cost-effectiveness of shared medical appointments for neuromuscular patients. Neurology. 2015;85:619–625.
- Miller WR, Rollnick S. Motivational Interviewing: helping people change. New York: Guilford Press; 2012.
- DiClemente CC, Prochaska JO. Toward a comprehensive, trans- theoretical model of change: Stages of change and addictive behaviors. In: Miller WR, Heather N, editors. Treating addictive behaviors. Volume 2nd. New York: Plenum Press; 1998. p. 3–24.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7.
- van Staveren WA, de Boer JO, Burema J. Validity and reproducibility of a dietary history method estimating the usual food intake during one month. Am J Clin Nutr. 1985;42:554–559.
- Vries J, de., Boer E, de., Hulshof K. Informatorium voor voeding en diëtetiek - voedingsleer. Houten: Bohn Stafleu van Loghum; 2013.
- Chen AY, Frankowski R, Bishop-Leone J, et al. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg. 2001;127:870–876.
- Speyer R, Heijnen BJ, Baijens LW, et al. Quality of life in oncological patients with oropharyngeal dysphagia: validity and reliability of the Dutch version of the MD Anderson Dysphagia Inventory and the Deglutition Handicap Index. Dysphagia. 2011;26:407–414.
- Bogaardt HC, Speyer R, Baijens LW, et al. Cross-cultural adaptation and validation of the Dutch version of SWAL-QoL. Dysphagia. 2009;24:66–70.
- Dedding C, Cardol M, Eyssen IC, et al. Validity of the Canadian Occupational Performance Measure: a client-centred outcome measurement. Clin Rehabil. 2004;18:660–667.
- Health Council of the Netherlands. Dutch dietary guidelines. The Hague: Health Council of the Netherlands; 2016.
- Bostrom K, Ahlstrom G. Quality of life in patients with muscular dystrophy and their next of kin. Int J Rehabil Res. 2005;28:103–109.
- Bellini M, Biagi S, Stasi C, et al. Gastrointestinal manifestations in myotonic muscular dystrophy. WJG. 2006;12:1821.
- LaDonna KA, Koopman WJ, Venance SL. Myotonic dystrophy (DM1) and dysphagia: the need for dysphagia management guidelines and an assessment tool. Can J Neurosci Nurs. 2011;33:42–46.
- Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: an introduction and overview. Prev Med. 2008;46:181–188.
- Meola G, Sansone V, Perani D, et al. Executive dysfunction and avoidant personality trait in myotonic dystrophy type 1 (DM-1) and in proximal myotonic myopathy (PROMM/DM-2). Neuromuscul Disord. 2003;13:813–821.
- Okkersen K, Buskes M, Groenewoud J, et al. The cognitive profile of myotonic dystrophy type 1: a systematic review and meta-analysis. Cortex. 2017;95:143–155.
- Morrow S. Quality and trustworthiness in qualitative research in counseling psychology. J Counsel Psychol. 2005;52:250–260.
- Geirdal AO, Lund-Petersen I, Heiberg A. Understanding the experience of myotonic dystrophy. Mixed method study. J Genet Counsel. 2015;24:169–178.