Abstract
Aim
To conduct a detailed investigation into changes in activity limitations and participation restrictions over 10 years in people with mild, moderate and severe multiple sclerosis.
Methods
This study was a 10-year longitudinal study of 264 people with multiple sclerosis living in Stockholm County, Sweden. Ten-year changes in personal and instrumental activities in daily living were assessed using the Katz Activities in Daily Living Index Extended and participation in social/lifestyle activities using the Frenchay Activities Index.
Results
While people with moderate multiple sclerosis, compared to baseline, demonstrated significantly higher proportions of dependency in most activities of personal and instrumental activities in daily living at the 10-year follow-up, the mild group primarily increased their dependency in instrumental activities and the severe group in personal activities. Significantly higher proportions of the moderate group showed restricted participation in domestic and outdoor activities whereas the mild group only showed restrictions in a few domains of participation. A majority of people with severe multiple sclerosis showed restricted participation in all social/lifestyle activities at baseline and the 10-year follow-up.
Conclusions
Prominent long-term increases in activity limitations and participation restrictions occurred across the spectrum of disease severity but was most pronounced in those more moderately affected.
This study provides guidance with regard to specific activities that are prone to deteriorate across 10 years and thereby reflect important targets and outcomes for interventions.
Increases in activity limitations and participation restrictions were most pronounced in those moderately affected by multiple sclerosis.
Those mildly affected by multiple sclerosis primarily increased their dependency in instrumental activities of daily living while those severely affected increased their dependency in personal activities of daily living.
Implications for rehabilitation
Introduction
Multiple sclerosis (MS) is a neuroinflammatory demyelinating disease causing progressive disability and resulting in a substantial burden for the individual and society [Citation1,Citation2]. As MS progresses, people with MS experience reduced ability to perform activities of daily living (ADL) and to participate in various life situations [Citation2–6]; which in turn have a negative impact on their quality of life [Citation2,Citation7,Citation8]. MS often results in different types of disability (e.g. in walking, manual dexterity and cognition) that could impact work participation and cause sickness absence [Citation9,Citation10] which in turn is associated with increased costs for society [Citation11]. From a health-care point of view, a major aim of the management of people with MS is to minimize the impact of activity limitations and participation restrictions. It is therefore important to conduct longitudinal observational studies to identify which specific activities are prone to long-term deterioration (i.e. across 10 years or more) in people with MS. This line of research is especially important to tailor health care to address the needs of the person with MS [Citation12,Citation13].
Previous longitudinal studies have demonstrated increased proportions of people with MS with dependency in personal ADL (e.g. feeding) and instrumental ADL (e.g. cleaning) over 10 years [Citation3,Citation4]. In contrast, inconsistent findings have been reported with regard to participation in more complex social/lifestyle activities (e.g. work and social occasions); most studies have shown restricted participation in people with MS across 10 years [Citation3,Citation14,Citation15] whereas others have demonstrated sustained [Citation4] or improved participation [Citation16]. The aforementioned longitudinal studies have reported changes in the sum score of items compromising instruments assessing ADL or participation. However, to the authors knowledge, no previous study has assessed changes in ADL and participation on an item specific level, i.e. explored changes in activity limitations and participation restrictions in the specific activities (e.g. feeding, bathing and dressing) included in the instruments. As previous studies have also demonstrated varying disability courses between people with MS with different disease severity [Citation3,Citation17] it is important to explore changes in activity limitations and participation restrictions in people with MS with different disease severity.
The aim of this study was therefore to conduct a detailed investigation into changes in activity limitations and participation restrictions over 10 years in people with MS with mild, moderate and severe MS at baseline.
Materials and methods
Study design and ethics
This study was a 10-year prospective study including two MS cohorts in Stockholm, Sweden. Despite differences in participant recruitment between the two MS cohorts (see below), combined they can be seen as providing a representative sample of people with MS living in Stockholm. The first cohort was a population-based study including a random sample of 321 people with MS from a data pool consisting of 2129 patients from all the hospital neurology clinics in Stockholm County [Citation4,Citation6]. Baseline assessment was performed between September 1999 and September 2002, and participants were re-assessed between 2009 and 2012 for a 10-year follow-up. To the second cohort, 255 people with MS were recruited from the MS Center at Karolinska University Hospital, Stockholm, between February 2002 and June 2002. Participants were re-assessed 2012 for a 10-year follow-up [Citation2,Citation3]. All participants were diagnosed with MS according to Poser criteria [Citation18] and were free of other severe neurological or psychiatric illness. All participants received information about the study aims and procedures and written informed consent was obtained afterwards. This study was approved by the Regional Board of Ethics in Stockholm (registration numbers 2018/876–32/3 and 2018/963–32).
Data collection
Data collection in both cohorts comprised standardized face-to-face interviews and self-reported questionnaires and occurred at the MS Center or in the participant’s home. summarizes the instruments used and variables studied in this study. Data on age, sex, living situation, work status, prescribed immunomodulatory treatment and disease duration (years) were collected. The course of MS was determined as relapsing-remitting or progressive MS. Disease severity was determined by the use of the Expanded Disability Status Scale (EDSS) [Citation19] and classified as mild MS (EDSS 0–3.5), moderate MS (EDSS 4–6.5) and severe MS (EDSS 7–9.5).
Table 1. Instruments and domains of the variables collected in this study.
For the activity domain, the Katz ADL Index Extended (KATZ Index) was used to assess personal ADL (feeding, bathing, dressing, continence, toileting, transferring) and instrumental ADL (cleaning, shopping, transportation and cooking) [Citation20,Citation21]. Each activity was scored as being “dependent” (i.e. requiring assistance) or “independent” (i.e. able to perform the activity without assistance). To gain information about the overall changes in dependency in ADL, the participants who reported dependency in one or more items of the two sub-domains of KATZ Index were classified as dependent in personal or in instrumental ADL. To gain information regarding activity specific changes, dependency in ADL for each item of the KATZ Index was analyzed. The KATZ Index has been shown to be reliable and valid in older adults [Citation22,Citation23].
For the participation domain, participation in social and lifestyle activities was assessed with the Frenchay Activities Index (FAI) [Citation24] which evaluates engagements in more complex activities; often involving more than one task/action, which require initiative, organization and planning on the part of the individual; as compared to the evaluation of ADL which primarily focuses on more isolated tasks/actions. The FAI contains 15 items covering three sub-domains: domestic (preparing meals, washing up after meals, washing clothes, light and heavy housework), leisure/work (social occasions, pursuing hobby, travel/outings, household maintenance, reading books and gainful work) and outdoor activities (local shopping, walking outside, driving car/public transport and gardening) [Citation24]. Contrasting the original classification of the FAI-domains [Citation24], “reading books” was classified as an activity within the leisure/work domain. Based on how often the activities have been performed the last 3 or 6 months, each item is scored between 0 and 3 (0 = “never” and 3 = “at least weekly”) and summarized as a total score of all items. The FAI has been shown to be reliable and valid in older adults and people with MS [Citation25,Citation26] and adequate to detect change over time in people with stroke [Citation27]. A total score of FAI <15 points was used to indicate overall restrictions in participation in social/lifestyle activities [Citation28]. To gain information about specific restrictions in participation, people with MS who reported 0 or 1 (i.e. reflecting that the activity is never or seldom performed) for each item of FAI were classified as being restricted in that activity.
Analysis
Statistical analyses were carried out using IBM Statistical Package for the Social Sciences, version 23.0 (SPSS Inc., Chicago, Illinois, USA). Descriptive statistics, mean (standard deviation), median (interquartile range, IQR) and numbers (percentages), were used to present demographics (age, sex, living situation and work status) and MS characteristics (disease duration, EDSS score, disease course and immunomodulatory treatment) at baseline. Changes in EDSS score between baseline and the 10-year follow-up for participants with mild, moderate and severe MS were analyzed with the Wilcoxon signed-rank test. Item specific data obtained from KATZ Index and FAI were binominal (i.e. dependent/independent in ADL and restriction/no restriction in participation) and presented separately as numbers and percentages for the different disease severity groups. Changes in proportions between baseline and 10-year follow-up were analyzed with the McNemar test. To decrease the risk of a Type 1 error related to multiple statistical tests, the significance level was set at p ≤ 0.01.
Results
Participants’ baseline characteristics
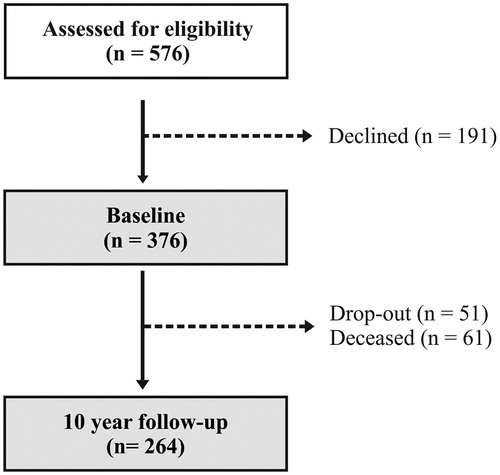
From the two original cohorts, 376 people with MS were enrolled and 264 participated in the 10-year follow-up (see ). Of those not participating in the 10-year follow-up, 61 were deceased and 51 declined to participate. Of those completing the study, 142 (54%) of the participants were classified as having mild MS, 84 (32%) had moderate MS and 38 (14%) had severe MS at baseline. The baseline characteristics of the participants who completed the study and those lost to follow-up are presented in .
Table 2. Baseline data for participants with mild, moderate and severe MS completing the study and those lost to the 10-year follow-up.
Changes in disease severity
Compared to baseline, significant decline in median (IQR) EDSS score was demonstrated at the 10-year follow-up for the entire MS cohort (3.5 (1.5) vs 4.5, (4.0), Z = −12.92, p ≤ 0.001) and for all severity groups; mild MS (1.5 (1.5) vs 3.0 (3.0), Z = −9.53, p ≤ 0.001), moderate MS (5.5 (1.5) vs 6.5 (1.4), Z = −7.51, p ≤ 0.001) and severe MS (8.0 (0.5) vs 8.5 (1.0), Z = 4.36, p ≤ 0.001).
Changes in activity limitations
At the 10-year follow-up, significantly higher proportions of people with MS with mild and moderate MS were dependent in personal ADL (mild: 20% vs 3%, moderate: 49% vs 12%, p < 0.001) and instrumental ADL compared to baseline (mild: 42% vs 16%, moderate: 88% vs 70%, p ≤ 0.001, ). For the moderate group, the item specific analysis demonstrated significantly higher proportions of dependency in all personal ADL except feeding (p ≤ 0.001) and for all instrumental ADL except cleaning (p ≤ 0.002, ). The mild group showed higher proportions of dependency at the 10-year follow-up with regard to urinary continence and in all instrumental ADL (p ≤ 0.001, ). At the 10-year follow-up, significantly higher proportions of people with severe MS were dependent in personal ADL compared to baseline (95% vs 68%, p = 0.002) which derived from increased dependency in all personal activities (p ≤ 0.001, ). All people with severe MS were dependent in instrumental ADL at baseline and at the 10-year follow-up ().
Figure 2. Percentages of people in the (A) mild, (B) moderate and (C) severe MS groups demonstrating dependency in personal and instrumental activities of daily living at baseline and the 10-year follow-up. Each activity was scored as being “dependent” (i.e. requiring assistance) or “independent” (i.e. able to perform the activity without assistance) according to the Katz ADL Index Extended. Data presents the percentages of people with MS who reported dependency. *Significant difference (p ≤ 0.01) between baseline and the 10-year follow-up.
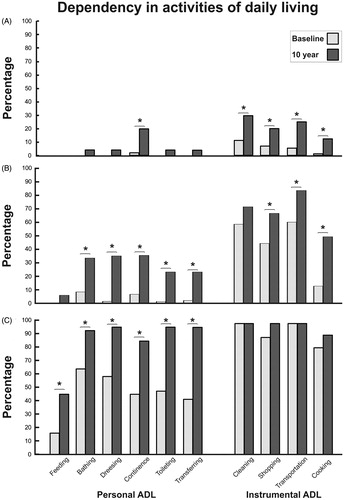
Table 3. Proportions (percentages) in the mild, moderate and severe MS group demonstrating activity limitations (i.e. dependency in ADL) and participation restrictions (i.e. restrictions in social/lifestyle activities) at baseline and 10-year follow-up.
Changes in participation restrictions
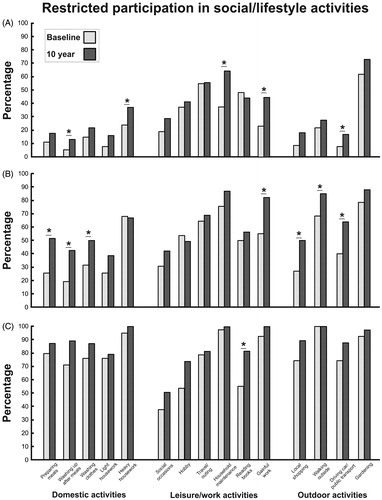
As shown in , overall participation restrictions (FAI total score <15 points) at baseline were most common in the severe group (71%), followed by the moderate (17%) and mild MS group (2%). While the moderate group demonstrated significantly higher proportions of overall participation restrictions at the 10-year follow-up than baseline (44% vs 17%), p < 0.001), no significant changes in proportions occurred in people with mild (p = 0.022) or severe MS group (p = 0.063, ). For the moderate group, the item specific analyses demonstrated increased proportions of people with participation restrictions between baseline and the 10-years follow-up in domestic activities, i.e. preparing meals (p < 0.001), washing up after meals (p = 0.001) and washing clothes (p = 0.009), gainful work (p < 0.001) and outdoor activities, i.e. local shopping (p = 0.001), walking outside (p < 0.001) and car driving/public transport (p < 0.001, ). The item-specific analyses – washing up after meals (p = 0.008), heavy housework (p = 0.010), household maintenance (p < 0.001), gainful work (p < 0.001) and driving car/public transport (p = 0.007, ) – also revealed increased proportions of participation restrictions in the mild MS group at the 10-year follow-up. A majority of the people with severe MS demonstrated restricted participation in most domestic, leisure/work and outdoor activities at baseline and at the 10-year follow-up (). Reading books was the only activity in the severe MS group with increased proportions of participation restrictions between baseline and the 10-years follow-up (p = 0.002).
Figure 3. Percentages of people in the (A) mild, (B) moderate and (C) severe MS groups demonstrating participation restrictions in domestic, leisure/work and outdoor activities at baseline and the 10-year follow-up. Each activity was scored between 0 and 3 (0 = “never” and 3 = “at least weekly”) according to the Frenchay Activities Index and people with MS who reported 0 or 1 were classified as being restricted in that activity. Data presents the percentages of people with MS who reported restricted participation. *Significant difference (p ≤ 0.01) between baseline and the 10-year follow-up.
Discussion
Although previous studies have provided important information about the changes in activity limitations and participation restrictions for people with MS [Citation3,Citation4], this study is the first to undertake an item-specific investigation on which specific activities and commitments that are prone to deteriorate in this population. The major findings were that while increases in activity limitations and participation restrictions occurred across the spectrum of disease severity the overall decline was most pronounced in those moderately affected. Those mildly affected by MS primarily increased their dependency in instrumental activities and those severely affected increased their dependency in personal activities. In the context of management of MS, while developing patient reported outcome measures and interventions for people with MS, the current findings shed light on the different courses of activity limitations and participation restrictions across the spectrum of disease severity and further emphasizes the importance of considering specific activities and engagements.
In the general population, previous research has identified three major trajectories of ADL; individuals who remain independent over time, individuals with a progressive increase in dependency and individuals with high dependency that remains unchanged over time [Citation29–31]. The present study found that the most progressive increase in proportions of people with ADL dependency occurred in the moderate group (EDSS score 4–6.5) whereas the mild group remained independent with regards to the most personal activities but revealed increased proportions of dependency in instrumental activities. Furthermore, the item specific analyses showed that the mild and moderate MS group had increased proportions of dependency for shopping, transportation and cooking (see ). Since dependency in these activities rarely increase in older adults without chronic diseases [Citation32] the current results highlight the likely downward transition toward ADL dependency in these subgroups, in particular people with moderate MS. These results are in line with previous cross-sectional findings showing high presence of disability in people moderately affected by MS [Citation2] and longitudinal findings demonstrating a more pronounced increase in disability over 10 years in a subgroup with predominantly moderate MS as compared to mild MS [Citation3]. In line with previous epidemiology studies [Citation33,Citation34], people moderately affected by MS have the greatest tendency towards functional decline since they often experience impairments in several domains (e.g. walking, cognition and manual dexterity) that might negatively influence both their independence in personal and instrumental ADL as well as their capacity to participate in more complex activities. In contrast, the high and unchanged dependency of instrumental ADL and participation restrictions in people with severe MS probably suggest that they had reached a plateau in activity limitations and participation. These results reflect the fact that this subgroup, as a consequence of the devastating effects of impaired physical and cognitive functioning in this phase of MS [Citation35,Citation36], have the greatest need for long-term care at any given time.
In the current study, while participation restrictions remained low in people with mild MS and high in people with severe MS, only the moderate MS group demonstrated an overall increase in participation restrictions (FAI total score <15 points). The moderate group’s participation restrictions in domestic (i.e. preparing and washing up after meals and washing clothes) and outdoor activities (shopping, walking and driving car/transport) had increased at the 10-year follow-up, whereas the mild group only showed restrictions in a few and varying domains of participation (see ). It is important to acknowledge that participation is a complex phenomenon which could be operationalized in different ways and have different significance for the individual. Therefore, the item-specific analyses (i.e. evaluation of specific activities/engagements) used in the present study to investigate changes in participation could provide an important complement as compared to previous studies which have focused on the overall changes in participation (i.e. evaluation of a sum-score of different items). In line with this reasoning, it is not surprising that previous studies have reported inconsistent results with regards to long-term changes in participation among people with MS; varying from reduced [Citation3, Citation14,Citation15], sustained [Citation4] and improved participation [Citation16]. Furthermore, there is no clear evidence from these studies that a certain disease group of MS would experience greater participation restrictions across time. As no previous study has used the FAI to assess overall participation restriction (i.e. sum score <15) or item specific restrictions in participation in people with MS, a direct comparison between the present findings and previous studies is difficult. It is therefore important to recognize the need for longitudinal and qualitative studies to identify which individuals sustained their participation and how people with MS perceive their participation.
There have been major advances regarding the development of disease modifying therapies (e.g. interferon beta, glatiramer acetate, teriflunomide, dimethyl fumarate, fingolimod, natalizumab, ocrelizumab), reducing relapse rates and slowing disease progression for people with MS [Citation37,Citation38]. Still, there is a continuing need to provide appropriate rehabilitation services to address activity limitations and participation restrictions in this population. Current findings regarding the effects of different rehabilitation modalities on the management of functioning in people with MS are promising [Citation39,Citation40], but there are several important limitations to the existing body of evidence. Firstly, while the number of rehabilitation trials for stroke [Citation41] and Parkinson’s disease [Citation39] have increased dramatically over the last 15 years, only a limited number of rehabilitation trials for MS have been carried out for people with MS [Citation40]. Additionally, although physical rehabilitation is important to sustain functioning for people with MS [Citation42,Citation43], there is also a need to establish multi-disciplinary rehabilitation programs that incorporate integrated rehabilitation interventions in MS [Citation44]. Such an approach would likely be of specific importance for long-term gains in activity and participation in people with MS as impairments in these domains due to their multi-factorial nature could be difficult for a single health-care profession to manage. For instance, irrespective of MS severity, the present results showed that greater proportions of people with MS were dependent due to urinary incontinence at the 10-year follow-up. This implies a great need for attention in rehabilitation since urinary dysfunction may impact quality of life [Citation45] and possibly be related to dependency in instrumental ADL or participation restrictions. There is also a lack of consensus regarding MS specific patient reported outcome measures that could be used in clinical trials to identify meaningful changes for people with MS [Citation12,Citation13]. The present results provide guidance to the specific activities that are prone to deteriorate across the different stages of MS which should be considered in the development of patient reported outcomes; e.g. the Patient-Reported Outcomes Measurement Information System [Citation46,Citation47]. For instance, the present study implies that important targets and outcomes for interventions differ between severity groups of MS as people mildly affected by MS primarily increased their dependency in instrumental ADL, those moderately affected in personal and instrumental ADL and those severely affected in personal ADL. Therefore, screening of the specific activities which are prone to decline in each severity groups of MS would important to identify the timepoint when early support or interventions are required in order to sustain activity and participation in this population.
Study limitations
This study has some limitations that require consideration. Firstly, compared to those completing the study, baseline demographics indicated that a larger proportion of those dropping out from the severe MS group (31% vs 57%) lived alone and from the mild and moderate MS groups were not working (54% vs 5–15%). The present results may have underestimated the changes in activity limitations and participation restrictions amongst members of these sub-groups of people with MS. In line with this, despite the extensive use of FAI to investigate participation in social/lifestyle activities [Citation24,Citation26,Citation48] it is possible that participants were active in ways not covered by FAI, such as maintaining social contacts and managing daily life by using the internet. The present study did not investigate other important aspects of independency and participation, such as vocational, social roles and self-efficacy [Citation49]. It is also important to highlight that there seems to be an overall ceiling effect of the FAI instrument in people severely affected by MS (see ). Accordingly, this raises concerns regarding the utility of the FAI to detect changes in participation in social/lifestyle activities in severe MS which in the current study might had led to an underestimation of the real change in this group. Furthermore, only 14% of those who completed the study had severe MS which increased the risk of type II errors due to decreased statistical power for analyses of this subgroup. Therefore, the interpretation of the results was guided by absolute proportions at baseline and the 10-year follow-up rather than solely relying on statistical significance. Nevertheless, the strengths of this study were the detailed long-term follow-up of specific activities across different severity groups of MS, the low drop-out rate (29%) and the similar distribution of drop-outs across the severity groups.
Conclusions
Prominent long-term increases in activity limitations and participation restrictions occurred across the spectrum of MS severity, but the overall decline was largest in the those more moderately affected; as evidenced by increased dependency in personal and instrumental ADL and restrictions in varying domains of participation among people with moderate MS. The results of the present study provide guidance of the specific activities and engagements that are prone to deteriorate across the different stages of MS and thereby reflect important targets and outcomes for interventions.
Disclosure statement
The authors report no declarations of interest.
Additional information
Funding
References
- Pugliatti M, Rosati G, Carton H, et al. The epidemiology of multiple sclerosis in Europe. Eur J Neurol. 2006;13:700–722.
- Johansson S, Ytterberg C, Claesson IM, et al. High concurrent presence of disability in multiple sclerosis. J Neurol. 2007;254:767–773.
- Conradsson D, Ytterberg C, von Koch L, et al. Changes in disability in people with multiple sclerosis: a 10-year prospective study. J Neurol. 2018;265:119–126.
- Chruzander C, Johansson S, Gottberg K, et al. A 10-year follow-up of a population-based study of people with multiple sclerosis in Stockholm, Sweden: changes in disability and the value of different factors in predicting disability and mortality. J Neurol Sci. 2013;332:121–127.
- Minden SL, Frankel D, Hadden L, et al. The Sonya Slifka Longitudinal Multiple Sclerosis Study: methods and sample characteristics. Mult Scler. 2006;12:24–38.
- Einarsson U, Gottberg K, Fredrikson S, et al. Activities of daily living and social activities in people with multiple sclerosis in Stockholm County. Clin Rehabil. 2006;20:543–551.
- Goverover Y, Chiaravalloti N, Gaudino-Goering E, et al. The relationship among performance of instrumental activities of daily living, self-report of quality of life, and self-awareness of functional status in individuals with multiple sclerosis. Rehabil Psychol. 2009;54:60–68.
- Mitchell AJ, Benito-Leon J, Gonzalez JM, et al. Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of wellbeing. Lancet Neurol.2005;4:556–566.
- Chruzander C, Tinghog P, Ytterberg C, et al. Longitudinal changes in sickness absence and disability pension, and associations between disability pension and disease-specific and contextual factors and functioning, in people with multiple sclerosis. J Neurol Sci. 2016;367:319–325.
- Forslin M, Fink K, Hammar U, et al. Predictors for employment status in people with multiple sclerosis: a 10-year longitudinal observational study. Arch Phys Med Rehabil. 2018;99:1483–1490.
- Gyllensten H, Wiberg M, Alexanderson K, et al. Costs of illness of multiple sclerosis in Sweden: a population-based register study of people of working age. Eur J Health Econ. 2018;19:435–446.
- Schaffler N, Schonberg P, Stephan J, et al. Comparison of patient-reported outcome measures in multiple sclerosis. Acta Neurol Scand. 2013;128:114–121.
- Khurana V, Sharma H, Afroz N, et al. Patient-reported outcomes in multiple sclerosis: a systematic comparison of available measures. Eur J Neurol. 2017;24:1099–1107.
- Gulick EE. Symptom and activities of daily living trajectory in multiple sclerosis: a 10-year study. Nurs Res. 1998;47:137–146.
- Beckerman H, Kempen JC, Knol DL, et al. The first 10 years with multiple sclerosis: the longitudinal course of daily functioning. J Rehabil Med. 2013;45:68–75.
- Solari A, Ferrari G, Radice D. A longitudinal survey of self-assessed health trends in a community cohort of people with multiple sclerosis and their significant others. J Neurol Sci. 2006;243:13–20.
- Wynia K, van Wijlen AT, Middel B, et al. Change in disability profile and quality of life in multiple sclerosis patients: a five-year longitudinal study using the Multiple Sclerosis Impact Profile (MSIP). Mult Scler. 2012;18:654–661.
- Poser CM, Paty DW, Scheinberg L, et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol. 1983;13:227–231.
- Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33:1444–1452.
- Asberg KH, Sonn U. The cumulative structure of personal and instrumental ADL. A study of elderly people in a health service district. Scand J Rehabil Med. 1989;21:171–177.
- Brorsson B, Asberg KH. Katz index of independence in ADL. Reliability and validity in short-term care. Scand J Rehabil Med. 1984;16:125–132.
- Ferretti-Rebustini RE, Balbinotti MA, Jacob-Filho W, et al. Validity of the Katz Index to assess activities of daily living by informants in neuropathological studies. Rev Esc Enferm USP. 2015;49:946–952.
- Reijneveld SA, Spijker J, Dijkshoorn H. Katz' ADL index assessed functional performance of Turkish, Moroccan, and Dutch elderly. J Clin Epidemiol. 2007;60:382–388.
- Wade DT, Legh-Smith J, Langton Hewer R. Social activities after stroke: measurement and natural history using the Frenchay Activities Index. Int Rehabil Med. 1985;7:176–181.
- Turnbull JC, Kersten P, Habib M, et al. Validation of the Frenchay Activities Index in a general population aged 16 years and older. Arch Phys Med Rehabil. 2000;81:1034.
- Kierkegaard M, Einarsson U, Gottberg K, et al. The relationship between walking, manual dexterity, cognition and activity/participation in persons with multiple sclerosis. Mult Scler. 2012;18:639–646.
- Schepers VP, Ketelaar M, Visser-Meily JM, et al. Responsiveness of functional health status measures frequently used in stroke research. Disabil Rehabil. 2006;28:1035–1040.
- Liman TG, Heuschmann PU, Endres M, et al. Impact of low mini-mental status on health outcome up to 5 years after stroke: the Erlangen Stroke Project. J Neurol. 2012;259:1125–1130.
- Han L, Allore H, Murphy T, et al. Dynamics of functional aging based on latent-class trajectories of activities of daily living. Ann Epidemiol. 2013;23:87–92.
- Deeg DJ. Longitudinal characterization of course types of functional limitations. Disabil Rehabil. 2005;27:253–261.
- Liang J, Xu X, Bennett JM, et al. Ethnicity and changing functional health in middle and late life: a person-centered approach. J Gerontol B Psychol Sci Soc Sci. 2010;65:470–481.
- Bleijenberg N, Zuithoff NPA, Smith AK, et al. Disability in the Individual ADL, IADL, and mobility among older adults: a prospective cohort study. J Nutr Health Aging. 2017;21:897–903.
- Manouchehrinia A, Beiki O, Hillert J. Clinical course of multiple sclerosis: a nationwide cohort study. Mult Scler. 2017;23:1488–1495.
- Leray E, Yaouanq J, Le Page E, et al. Evidence for a two-stage disability progression in multiple sclerosis. Brain. 2010;133:1900–1913.
- Brissart H, Morele E, Baumann C, et al. Cognitive impairment among different clinical courses of multiple sclerosis. Neurol Res. 2013;35:867–872.
- Smrtka J, Brown T, Bjorklund G. Loss of mobility and the patient burden of multiple sclerosis: expert opinion on relevance to daily clinical practice. Postgrad Med. 2016;128:145–151.
- Comi G, Radaelli M, Soelberg SP. Evolving concepts in the treatment of relapsing multiple sclerosis. Lancet. 2017;389:1347–1356.
- Filippi M, Bar-Or A, Piehl F, et al. Multiple sclerosis. Nat Rev Dis Primers 2018;4:43.
- Tomlinson CL, Patel S, Meek C, et al. Physiotherapy versus placebo or no intervention in Parkinson’s disease. Cochrane Database Syst Rev 2013;CD002817.
- Ploughman M. A new era of multiple sclerosis rehabilitation: lessons from stroke. Lancet Neurol. 2017;16:768–769.
- Pollock A, Baer G, Campbell P, et al. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst Rev. 2014;CD001920.
- Pearson M, Dieberg G, Smart N. Exercise as a therapy for improvement of walking ability in adults with multiple sclerosis: a meta-analysis. Arch Phys Med Rehabil. 2015;96:1339–1348 e7.
- Motl RW, Sandroff BM, Kwakkel G, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017;16:848–856.
- Khan F, Turner-Stokes L, Ng L, et al. Multidisciplinary rehabilitation for adults with multiple sclerosis. Cochrane Database Syst Rev. 2007;CD006036.
- Isaksson AK, Ahlstrom G, Gunnarsson LG. Quality of life and impairment in patients with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2005;76:64–69.
- Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45:S3–S11.
- Hahn EA, Beaumont JL, Pilkonis PA, et al. The PROMIS satisfaction with social participation measures demonstrated responsiveness in diverse clinical populations. J Clin Epidemiol. 2016;73:135–141.
- McPhail S, Lane P, Russell T, et al. Telephone reliability of the Frenchay Activity Index and EQ-5D amongst older adults. Health Qual Life Outcomes. 2009;7:48.
- Yorkston KM, Kuehn CM, Johnson KL, et al. Measuring participation in people living with multiple sclerosis: a comparison of self-reported frequency, importance and self-efficacy. Disabil Rehabil. 2008;30:88–97.