Abstract
Purpose
The aim of this study was to describe differences in long-term outcomes for patients discharged to inpatient rehabilitation facilities (IRFs) following stroke compared to patients discharged directly home or to residential aged care facilities (RACFs).
Materials and methods
Cohort study. Data from the Australian Stroke Clinical Registry were linked to hospital admissions records and the national death index. Main outcomes: death and hospital readmissions up to 12 months post-admission, Health-related Quality of Life (HRQoL) 90-180 days post-admission.
Results
Of 8,555 included patients (median age 75, 55% male, 83% ischemic stroke), 4,405 (51.5%) were discharged home, 3,442 (40.2%) to IRFs, and 708 (8.3%) to RACFs.
No between-group differences were observed in hazard of death between patients discharged to IRFs versus home. Fewer patients discharged to IRFs were readmitted to hospital within 90, 180 or 365-days compared to patients discharged home (adjusted subhazard ratio [aSHR]:90-days 0.54, 95%CI 0.49, 0.61; aSHR:180-days 0.74, 95%CI 0.67, 0.82; aSHR:365-days 0.85, 95%CI 0.78, 0.93). Fewer patients discharged to IRFs reported problems with mobility compared to those discharged home (adjusted OR 0.54, 95%CI 0.47, 0.63), or to RACFs (aOR 0.35, 95%CI 0.25, 0.48). Overall HRQoL between 90-180 days was worse for people discharged to IRFs versus those discharged home and better than those discharged to RACFs.
Conclusions
Several long-term outcomes differed significantly for patients discharged to different settings after stroke. Patients discharged to IRFs reported some better outcomes than people discharge directly home despite having markers of more severe stroke.
People with mild strokes are usually discharged directly home, people with moderate severity strokes to inpatient rehabilitation, and people with very severe strokes are usually discharged to residential aged care facilities.
People discharged to inpatient rehabilitation reported fewer problems with mobility and had a reduced risk of hospital readmission in the first year post-stroke compared to people discharged directly home after stroke.
The median self-reported health-related quality of life for people discharged to residential aged care equated to ‘worst health state imaginable’.
Implications for rehabilitation
Introduction
Stroke is a leading cause of death and disability globally, and it is estimated that one in five Australians will have a stroke within their lifetime [Citation1]. Strong evidence exists to support immediate medical attention and access to stroke unit (SU) care for all people with stroke [Citation2]. Following admission to the SU, recommendations regarding care become more divergent, being dependent on clinical factors, health system resources and patient preferences.
There are no clear recommendations regarding when and where to discharge patients from the acute hospital, but patterns regarding discharge from Australian SUs have been observed [Citation3]. Lengths of stay have been steadily decreasing (from median 7 days in 2010 [Citation4] to 4 days in 2017 [Citation5]). Stroke survivors with mild or no apparent signs of stroke tend to be discharged directly home; survivors who are alert with obvious sensorimotor or language impairment tend to be discharged to inpatient rehabilitation facilities (IRFs); and survivors with severe symptoms like dense hemiplegia, dysphagia and reduced alertness tend to be discharged directly to residential aged care facilities (RACFs, sometimes referred to as nursing homes) [Citation3] which provide long-term care for people who can no longer live at home.
Little is known about differences in long-term outcomes of patients discharged to different settings after stroke. By comparing the patterns within the cohorts of patients discharged to different settings using data from our national stroke registry, we may be able to identify opportunities to improve long-term outcomes for all patients with stroke.
The objective of this multicentre, prospective, observational study was to describe long-term outcomes (mortality, hospital readmissions, and quality of life) for patients following acute stroke either discharged to home, IRFs or to RACFs.
Given the observed patterns of different patient cohorts being discharged to different destinations, we hypothesized that patients discharged to IRFs would i) have worse long-term outcomes than patients discharged directly home, and ii) better long-term outcomes than patients discharged directly to RACFs.
Methods
Datasets
This study originates from the Stroke123 project whereby patient-level data from the Australian Stroke Clinical Registry (AuSCR) were linked and merged with routinely collected administrative data from five jurisdictions, previously described [Citation6,Citation7]. Data from patients admitted to 39 acute hospitals with stroke or transient ischaemic attack (TIA) who were registered in the AuSCR between 2009 and 2013 were linked to the National Death Index, as well as hospital emergency department and admissions records from four Australian states (Victoria, New South Wales, Queensland, Western Australia) using patient identifiers with 98% matching. All hospitals contributing data to the AuSCR were included. Hospital administrative data included a 5-year look-back period (including the index event) to maximize information on comorbidities.
AuSCR includes information from all patients with stroke and TIA admitted to participating hospitals who do not opt out of the registry. Data are collected during the hospital admission based on a nationally endorsed minimum dataset including demographic and clinical information, quality of care indicators and discharge outcomes including discharge destination [Citation8]. Follow-up data [health-related quality of life (HRQoL)] were collected once per patient via questionnaires posted to eligible patients 90-180 days after their stroke, with telephone follow-up if questionnaires were not returned. Surveys could be completed by patients or their caregivers. Eligibility for participation in the follow-up survey included having a first-recorded stroke, having data registered in AuSCR within 180 days of stroke and being alive at 90 days post-stroke.
Data from 2010 to 2103 were used for the current study. Additional exclusion criteria were: admission for TIA (by definition, there is no permanent neurological damage, so any requirement for rehabilitation or long term care would be related to factors other than the TIA); discharge to settings other than home/private residence, IRF or RACF; missing discharge destination; age under 18 years.
Hospital admissions data contain morbidity data (International Classification of Diseases, 10th revision, Australian modification [ICD-10-AM] diagnosis codes), and administrative data on all admitted patient episodes to public or private hospitals. Data from emergency department presentations were not used in this study.
The National Death Index provides information on date and primary and secondary ICD-10-AM coded cause of death. These data are linked with AuSCR annually to update mortality information.
Outcomes and definitions
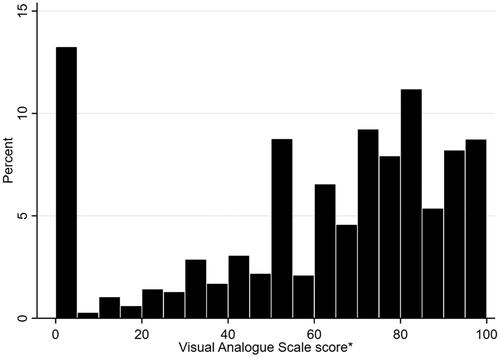
The outcomes were all-cause death and all-cause hospital readmissions during the first 12-months following discharge from the acute hospital for the index stroke event, and self-reported HRQoL at 90-180 days post-stroke. Acute hospital readmissions were obtained from the linked hospital administrative records. All cases where patients were admitted and separated on the same date (related to rehabilitation, chemotherapy, radiotherapy, dialysis and palliative care) were excluded. HRQoL was assessed using the generic EuroQoL 5-dimensional questionnaire (EQ-5D) [Citation9] with three levels of responses for each domain. The EQ-5D has been shown to be valid and responsive for stroke [Citation10], and displays acceptable accuracy when filled out by a proxy [Citation11]. Answers were dichotomized as ‘no problems’ or ‘any problems’ for each domain, and a visual analog scale (VAS) for overall HRQoL, ranging from 0 (worst health state imaginable) to 100 (best health state imaginable). For the 478 patients who died within 180-days, the VAS was coded as ‘zero’ to address survivor bias.
Patient demographic data, clinical characteristics, quality of care indicators, discharge destination and HRQoL were obtained from the AuSCR. Information on comorbidities was obtained from the hospital admissions data, allowing Charlson Comorbidity Index (CCI) scores [Citation12] to be calculated using a validated algorithm for ICD-10-AM codes [Citation13]. The CCI has consistently been shown to be a valid and reliable prognostic indicator [Citation14], including for patients with stroke [Citation15]. Patients were assigned to categories defined by the CCI score 0 (none), 1 (moderate), 2 (severe), and 3 or more (very severe) [Citation15].
Information about the acute hospitals (e.g., location, bed numbers and teaching status) was provided by the hospitals to the AuSCR Office. Patients’ socioeconomic positions were determined using the postcode-based Index of Relative Socioeconomic Advantage/Disadvantage using information provided by the Australian Bureau of Statistics [Citation16].
Statistical methods
Patient and hospital-related factors of patients discharged to the three different discharge destinations were tallied (). Differences in mortality between groups (IRF versus home, IRF versus RACF) at 90, 180 and 365 days following the index stroke admission date were assessed using Cox proportional hazards regression analysis. Differences in hospital readmissions were evaluated using competing risks multiple regression models, with death as a competing risk, giving adjusted subhazard ratios (aSHR). Sensitivity analyses were conducted to account for the time spent in IRFs not captured in our data (median length of stay [LOS] in IRFs was 26 days in 2012 [Citation17]). This was done by comparing death and readmissions at 90, 180 and 365 days for patients discharged home and to RACF to these outcomes at 120, 210 and 395 days for patients discharged to IRFs (i.e., timepoint + 30 days), excluding deaths or readmissions within the first 30 days for this group. Differences between groups in HRQoL VAS scores were assessed using quantile regression analyses. Between-group differences for each of the five dichotomized dimensions of the EQ-5D were assessed using logistic regression.
Table 1. Description of sample.
All multivariable models were adjusted for the same pre-specified patient, clinical and hospital characteristics [age, sex, birthplace, socioeconomic advantage, CCI, dementia, previous stroke, stroke type, ability to walk unaided on admission (global measure of disability that can reliably predict survival and independence at time of hospital discharge [Citation18,Citation19]), in-hospital stroke (a stroke that occurs when a person has been admitted to hospital for a different condition), SU care, hospital location, size and teaching status]. Multi-level models were used with level defined as patient and hospital to adjust for patient clustering within hospitals. Data were analyzed using StataIC 14.0.
Ethical considerations
The Stroke123 data linkage project was approved by Monash University (CF13/1303-2013000641), in addition to site-specific approvals. Additional ethics approvals were obtained from the Australian Institute for Health and Welfare (EO2013/2/16) for linkage of the AuSCR registrants’ data to National Death Index data, and from the state health departments in New South Wales (HREC/14/CIPHS/66), Queensland (HREC/13/QPAH/31), Victoria (HREC/14/CIPHS/66) and Western Australia (#2015/33).
Results
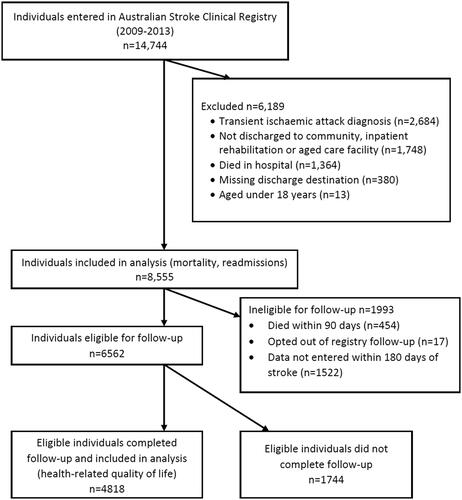
Data were available for 14,744 patients registered in AuSCR with stroke or TIA from 2010-2013. Data from 8,555 patients with stroke were included following exclusion of patients diagnosed with TIA (n = 2,684, 18.2%); discharged to settings other than home/private residence, IRF or RACF (n = 1,748, 11.9%), e.g., acute hospital transfer; died in hospital (n = 1,364, 9.3%); missing discharge destination (n = 380, 2.6%) and aged under 18 years (n = 13, 0.1%) (). The median age of included patients was 75 years, 54.9% were male and 82.6% experienced ischaemic strokes ().
Mortality
Overall, 961 (11%) of included patients died within 12 months of stroke.
After adjusting for baseline factors, there were no between-group differences in hazard of death for patients discharged to IRFs compared to those discharged directly home. Patients discharged to IRFs had a reduced hazard for death compared to patients discharged to RACFs; adjusted Hazard Ratio 0.27 (95%CI 0.19, 0.38) at 90 days (). This observation persisted up to 12-months post-stroke, and remained when sensitivity analysis accounted for the extra time the IRF cohort spent in the hospital system (Supplemental Table I).
Table 2. Cumulative survival up to 90, 180 and 365 days among patients accessing inpatient rehabilitation versus discharge to home or residential care.
Readmissions
More than half the sample (n = 4555, 53.2%) were readmitted to hospital in the 12 months following discharge. Circulatory system diseases (ICD-10 codes I00-I99) were the most common primary diagnosis of first readmissions, being responsible for 973 (21.4%) first readmissions. After adjusting for baseline factors, patients discharged to IRFs were less likely than patients discharged directly home to be readmitted within days 90, 180 and 365 following discharge from the acute hospital (aSHR:90-days 0.54, 95%CI 0.49, 0.61; aSHR:180-days 0.74, 95%CI 0.67, 0.82; aSHR:365-days 0.85, 95%CI 0.78, 0.93), . These differences remained when sensitivity analysis accounted for the extra time the IRF cohort spent in the hospital system (Supplemental Table II).
Table 3. Cumulative readmissions within 90, 180 and 365 days among patients accessing inpatient rehabilitation versus discharge to home or residential care.
Patients discharged to IRFs were more likely than patients discharged to RACF to be readmitted within 365 days (aSHR:365 days 1.34, 95%CI 1.16, 1.55). Results comparing readmissions between the IRF and RACF group for 90 and 180 days were less clear, with inconsistencies between the main and sensitivity analyses (Supplemental Table II).
Health-related quality of life at 90–180 days
Follow-up survey data were available for 4818 patients (73% of those eligible to participate, Supplemental Table III), with responses for 1001 (20.8%) participants completed by someone other than the person with stroke. Percentages of survey respondents who had been discharged to home, IRF and RACF were similar to the overall sample (Supplemental Table IV). Eligible patients who completed follow-up were older, with shorter LOS, less often identified as being Aboriginal and/or Torres Strait Islander, more often received SU care and experienced an ischaemic stroke than eligible patients who did a complete follow-up.
The median HRQoL VAS score reported by respondents was 70 (Q1 40, Q3 80), see . More than half of the sample reported problems with usual activities (59.9%) and mobility (55.3%). Problems with pain/discomfort (49.5%) and anxiety/depression (47.4%) were also commonly reported. After adjusting for baseline factors, patients discharged to IRFs reported lower HRQoL than patients discharged directly home (coefficient −6.50, 95%CI −8.34, −4.66) and higher HRQoL than patients discharged to RACFs (coefficient 43.42, 95%CI 39.60, 47.24). Patients discharged to IRFs were less likely to report problems with mobility compared to those discharged directly home or to RACFs (). However, these people were more likely to report problems with self-care, usual activities, pain/discomfort, and anxiety/depression than people discharged directly home.
Table 4. Health-related quality of life between 90 and 180 days among patients accessing inpatient rehabilitation versus discharge to home or residential care.
Discussion
This research provides new knowledge about the associations between discharge destination and mortality, hospital readmissions, and HRQoL in large numbers of people in the first year after stroke. The three patient groups compared in our analysis are likely to represent different bands of stroke severity, given the differing proportions of patients who could walk independently on admission to hospital, which has been shown to be a reliable proxy for stroke severity in large datasets [Citation19]. In the group discharged directly home, the majority (61.4%) could walk independently on admission, likely comprising patients with mild stroke. In contrast, only 24.1% of patients discharged to IRFs could walk independently on admission, likely representing those with moderate and severe stroke. In the group discharged to RACFs, only 11.5% of patients could walk independently on admission. We are unable to report how many of these patients lived in RACFs prior to their stroke.
Our data highlight unexpected advantages for patients discharged to IRFs over patients discharged directly home. We hypothesized that patients who were discharged to IRFs would have worse long-term outcomes than patients discharged directly home. However, despite the cohort who were discharged to IRFs being older and having indicators of more severe stroke, they had similar mortality (after adjusting for comorbidities), were less likely to be readmitted to hospital and reported fewer problems with mobility than patients discharged directly home. As anticipated, overall HRQoL was worse for these patients. It may be that the longer LOS for patients discharged to IRFs (8 days in hospital, plus approximately 3-4 weeks in IRF vs 4 days for patients discharged home) allows for comprehensive discharge planning which tends to occur suboptimally in Australia; in previous work, only 52% of patients who were discharged directly home after stroke received discharge care plans [Citation20], and only 18% received all aspects of discharge care planning [Citation21]. The extra time spent in inpatient settings by patients admitted to IRFs may assist in preparing patients and their families for living with the long-term effects of stroke, inclusive of ongoing rehabilitation and secondary stroke prevention. For those discharged directly home, we cannot report the proportion who received rehabilitation at home or in a community setting, but nationally only 4% of patients with stroke access home rehabilitation [Citation22]. Patients with mild physical impairments following stroke who do not receive rehabilitation can experience ongoing difficulties with community mobility [Citation23], which may account for the higher prevalence of self-reported mobility problems in the group discharged directly home. Given the unanticipated comparatively poor outcomes for patients discharged directly home, it would appear that supports such as information provision, discharge planning and rehabilitation routinely offered in IRFs should be considered for people discharged directly home through the use of services such as early supported discharge which have proven effectiveness in reducing disability and hospital LOS for people with mild to moderate disability following stroke [Citation24].
As anticipated, mortality and HRQoL outcomes for patients discharged directly to RACFs were worse than those of patients discharged to IRFs. The proportion of patients discharged directly to RACFs was relatively small (8.3% of sample). These patients were more likely to be aged over 85 years, have dementia and were less likely to receive SU care than patients discharged to IRFs. The current analysis cannot determine causality, so it is unclear whether the patients discharged to RACFs were less likely to survive so were managed palliatively in the acute hospital and following discharge. Another possibility is that the greater mortality rates may be associated with a nihilistic approach to service provision for this group, with less access to SU care and IRFs, despite evidence that patients with severe stroke and cognitive impairment benefit from inpatient rehabilitation [Citation25,Citation26]. Outcomes for these patients were extremely poor with median HRQoL VAS score of 0 equating to ‘worst health state imaginable’. The median LOS for this group was 13.5 days, therefore it would be logical to trial reorganization of the hospital system and provide rehabilitation during this inpatient stay for patients who are anticipated to survive their stroke with a view to improving outcomes, including HRQoL.
Study limitations
Strengths of this study include the large nationally representative cohort of patients with confirmed stroke diagnoses, and the use of linked data which has allowed increased information on comorbidities and examination of long-term mortality and readmissions for the first time in the Australian context. Limitations of this work are the lack of detailed information about stroke severity (the National Institutes of Health Stroke Scale has only recently been introduced as part of routine collection in AuSCR), impairments at time of discharge, pre-stroke place of residence and the infrastructure and activity of stroke rehabilitation services. Further, it is plausible that a person’s HRQoL may be affected by their post-discharge place of residence which we did not account for. There may also be other sources of bias or confounding. Not all eligible participants returned the follow-up questionnaire and there were some differences in patient profiles for those who did or did not respond which may have over or underestimated the estimates of HRQoL, including the fact that some responses were filled out by a proxy rather than the patient themselves.
Conclusions
Our findings suggest that patients discharged to IRFs after stroke experience disproportionately fewer hospital readmissions and problems with mobility than patients discharged directly home, despite having markers of more severe stroke. Rehabilitation provided to people in settings other than IRFs (i.e., provided to patients who are discharged directly home or to RACFs after stroke) may need to be improved to adequately address these patients’ ongoing needs.
Supplemental_tables.docx
Download MS Word (31.3 KB)Acknowledgments
We acknowledge staff from the Australian Stroke Clinical Registry (AuSCR) Office and contributions of The George Institute for Global Health, the Florey Institute of Neuroscience, and Mental Health, and the Stroke Foundation to AuSCR operations. We also thank the hospital staff for their diligence in data collection for the AuSCR.
Disclosure statement
Authors 1, 2, 3, 4, 5, 7 report no disclosures relevant to the manuscript. Authors 6, 8, 9: restricted educational grants from Allergan Australia (2009 and 2010), Ipsen (2010) and Boehringer (2013) awarded to the Management Committee of the AuSCR to improve aspects of the data tool or as contributions to support an annual national workshop. Author 9: data custodian and principal coordinating investigator for the AuSCR.
Data availability statement
This study is based on the secondary analysis of data as part of a data linkage study. Restrictions apply to the availability of these data, which were used under license for this study. Qualified investigators can request access to patient‐level data, analytic methods, and study materials after ethics clearance and approval by all authors and the data custodians of the primary sources of the data-sets.
Additional information
Funding
References
- The GBD 2016 Lifetime Risk of Stroke Collaborators Global, Regional, and Country-Specific Lifetime Risks of Stroke. New Eng J Med. 1990;379(25):2429–2437.
- Stroke Foundation. Clinical Guidelines for Stroke Management 2017 Melbourne Australia. 2017. Available from: https://informme.org.au/Guidelines/Clinical-Guidelines-for-Stroke-Management-2017
- Lynch EA, Luker JA, Cadilhac DA, et al. Inequities in access to rehabilitation: Exploring how acute stroke unit clinicians decide who to refer to rehabilitation. Disabil Rehabil. 2016;38(14):1415–1424.
- Cadilhac DA, Lannin NA, Anderson C, et al. The Australian Stroke Clinical Registry Annual Report 2010. The George Institute for Global Health and National Stroke Research Institute; 2010. September 2010. Contract No.: 2.
- Cadilhac DA, Lannin NA, Breen S, et al. The Australian Stroke Clinical Registry Annual Report 2017. The Florey Institute of Neuroscience and Mental Health; December 2017, Report No 9, 60 pages.
- Andrew NE, Sundararajan V, Thrift AG, et al. Addressing the challenges of cross-jurisdictional data linkage between a national clinical quality registry and government-held health data. Aust N Z J Public Health. 2016;40(5):436–442.
- Kilkenny MF, Kim J, Andrew NE, et al. Maximising data value and avoiding data waste: a validation study in stroke research. Med J Aust. 2019;210(1):27–31.
- Cadilhac DA, Lannin NA, Anderson CS, et al. Protocol and pilot data for establishing the Australian stroke clinical registry. Int J Stroke. 2010;5(3):217–226.
- The EuroQoL Group. EuroQoL-a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
- Dorman PJ, Waddell F, Slattery J, et al. Is the EuroQol a valid measure of health-related quality of life after stroke? Stroke. 1997;28(10):1876–1882.
- Pickard AS, Johnson JA, Feeny DH, et al. Agreement Between Patient and Proxy Assessments of Health-Related Quality of Life After Stroke Using the EQ-5D and Health Utilities Index. Stroke. 2004;35(2):607–612.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–383.
- Sundararajan V, Henderson T, Perry C, et al. New ICD-10 version of the Charlson Comorbidity Index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–1294.
- de Groot V, Beckerman H, Lankhorst GJ, et al. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003;56(3):221–229.
- Schmidt M, Jacobsen JB, Johnsen SP, et al. Eighteen-year trends in stroke mortality and the prognostic influence of comorbidity. Neurology. 2014;82(4):340–350.
- Australian Bureau of Statistics. Socio-economic indexes for areas (SEIFA) 2011. 2011. Available from: http://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa
- National Stroke Foundation. National stroke audit – rehabilitation services report. 2012. Melbourne (Australia): National Stroke Foundation.
- Counsell C, Dennis M, McDowall M, et al. Predicting outcome after acute and subacute stroke: development and validation of new prognostic models. Stroke. 2002;33(4):1041–1047.
- Cadilhac DA, Kilkenny MF, Levi C, et al. Risk-adjusted hospital mortality rates for stroke: evidence from the Australian Stroke Clinical Registry (AuSCR). Med J Aust. 2017;206(8):345–350.
- Cadilhac DA, Andrew NE, Lannin NA, Australian Stroke Clinical Registry Consortium, et al. Quality of acute care and long-term quality of life and Survival: The Australian Stroke Clinical Registry. Stroke. 2017;48(4):1026–1032.
- Andrew NE, Busingye D, Lannin NA, et al. The quality of discharge Care Planning in Acute Stroke Care: Influencing Factors and Association with Postdischarge Outcomes. J Stroke Cerebrovasc Dis. 2018;27(3):583–590.
- Lynch EA, Mackintosh S, Luker JA, Hillier SL. Access to rehabilitation for patients with stroke in Australia. Med J Aust. 2019;210(1):21–26.
- Rochette A, Tellier M. Falling through the cracks: A literature review to understand the reality of mild stroke survivors. Top Stroke Rehabil. 2009;16(6):454–462.
- Langhorne P, Baylan S. Early Supported Discharge Trialists. Early supported discharge services for people with acute stroke. Cochrane Database Syst Rev. 2017;(7):CD000443.
- Pereira S, Graham JR, Shahabaz A, et al. Rehabilitation of individuals with severe stroke: synthesis of best evidence and challenges in implementation. Top Stroke Rehabil. 2012;19(2):122–131.
- Paker N, Buğdaycı D, Tekdöş D, et al. Impact of cognitive impairment on functional outcome in stroke. Stroke Res Treat. 2010;2010:652612.