Abstract
Purpose
To systematically map available evidence for school-based interventions led by allied health (i.e., occupational therapy, physiotherapy, and/or speech and language therapy).
Materials and methods
We searched for studies in pre-school, primary, secondary, or post-secondary settings, published 2004–2020. We coded study, population, and intervention characteristics. Outcomes were coded inductively, categorised, and linked to the International Classification of Functioning, Disability, and Health.
Results
We included 337 studies (33 countries) in an interactive evidence map. Participants were mainly pre-school and primary-aged, including individuals with neurodisability and whole-school populations. Interventions targeted wide-ranging outcomes, including educational participation (e.g., writing, reading) and characteristics of school environments (e.g., educators’ knowledge and skills, peer support). Universal, targeted, and intensive interventions were reported in 21.7%, 38.9%, and 60.2% of studies, respectively. Teachers and teaching assistants delivered interventions in 45.4% and 22.6% of studies, respectively. 43.9% of studies conducted early feasibility testing/piloting and 54.9% had ≤30 participants. Sixty-two randomised controlled trials focused on intervention evaluation or implementation.
Conclusions
In the United Kingdom, future research should take forward school-based allied health interventions that relate directly to agreed research priorities. Internationally, future priorities include implementation of tiered (universal, targeted, intensive) intervention models and appropriate preparation and deployment of the education workforce.
Allied health professionals (occupational therapists, physiotherapists, and speech and language therapists) work in schools supporting children and young people affected by neurodisability but the content, impact, and cost-effectiveness of their interventions are not well-understood.
We systematically mapped the available evidence and identified that allied health school-based interventions target highly diverse health-related outcomes and wider determinants of children and young people’s health, including educational participation (e.g., literacy) and characteristics of the school environment (e.g., educators’ knowledge and skills).
Our interactive evidence map can be used to help stakeholders prioritise the interventions most in need of further evaluation and implementation research, including tiered models of universal, targeted, and intensive allied health support.
Teachers and teaching assistants play a central role in delivering allied health interventions in schools – appropriate preparation and deployment of the education workforce should therefore be a specific priority for future international allied health research.
IMPLICATIONS FOR REHABILITATION
Introduction
Approximately 8% of 0–19 year olds are disabled and neurodisability comprises one of the largest groups of disabled children and young people [Citation1,Citation2]. Neurodisability includes individuals affected by congenital or acquired long-term conditions related to impairment of the brain and/or neuromuscular system [Citation3].
Disabled children and young people, including those affected by neurodisability, are at higher risk of adverse health, social, and educational outcomes than their non-disabled peers [Citation4,Citation5]. For example, adolescents with cerebral palsy report significantly lower quality of life in terms of social support and peer relationships [Citation6], disabled children and young people are more likely to experience bullying victimisation and violence [Citation7,Citation8], and individuals identified as having special educational needs are more frequently excluded, absent, or missing from school, and are more likely to lag behind in educational and employment outcomes in adulthood [Citation9–11]. Disabled children and young people also experience higher levels of poverty and social disadvantage, being more likely to live with low-income, deprivation, debt, and poor housing, to live in a lone-parent household, and to live with a disabled parent, all of which further compound their risk of adverse health outcomes [Citation4,Citation5].
Allied health professionals, defined here as occupational therapists, physiotherapists, and speech and language therapists, are a key part of the workforce supporting children and young people affected by neurodisability. Although allied health professionals are commonly employed by health services, for example the National Health Service (NHS) in the United Kingdom (UK), much of their support is actually delivered in schools and education settings [Citation12,Citation13]. As well as the practical reality that school is where children and young people spend most of their time during the day, the rationale for school-based allied health service delivery is underpinned by a number of factors. Traditionally, allied health services have focused on reducing morbidity and impairment in children and young people and improving their capacities and skills. However, more contemporary practice has shifted towards targeting social environmental determinants of children and young people’s health, particularly their participation in education [Citation11–15]. Service delivery models over the last 15–20 years have been primarily consultative whereby allied health professionals design intervention programmes and advise teaching assistants, teachers, and parents on delivering them at school and home [Citation12]. However, services are slowly moving towards tiered intervention models whereby different levels of universal, targeted, and intensive support are embedded within school systems, with a particular emphasis on whole-school universal approaches that build educators’ capacity to create inclusive environments for all children and young people’s learning and development [Citation16]. From a policy perspective, greater joint working between allied health and education systems is increasingly mandated as part of providing for the needs of individuals with special educational needs and disabilities in schools and improving their health, social, and educational outcomes [e.g., Citation17].
Whilst allied health support delivered in schools is part of usual care for children and young people affected by neurodisability, it is not well understood in terms of its content, impact, or cost-effectiveness. For example, across the UK, practice varies widely according to factors such as different philosophical positions on the purpose of allied health support, geographical area, and resource constraints [Citation12,Citation18]. Furthermore, in some regions allied health support in schools is poorly integrated with other interventions and many parents report severe difficulties with accessing services and dissatisfaction with the amount of support their child receives [Citation18]. This practice variation stems primarily from uncertainty about what works, a lack of consensus about what should be implemented, and inequitable provision of services between towns and regions, and does not reflect legitimate differences in how local service commissioners provide appropriate support tailored to the unique needs and priorities of their own distinct populations [Citation12,Citation18].
In the context of these issues, multidisciplinary professionals, parents, and children and young people have collectively identified and prioritised research topics focused on evaluating the effectiveness of allied health support, including in schools, for key health, social, and educational outcomes (e.g., self-care and independence, social participation, and educational inclusion) [Citation19–22]. Historically, allied health research conducted over the last 10–15 years has produced a number of landmark studies, including several randomised controlled trials and economic evaluations of language, social communication, handwriting, and exercise interventions, and service delivery models [e.g., Citation23,Citation24–27]. However, whilst these studies have certainly provoked discussion amongst practitioners and have likely had some influence on practice in some geographical areas, it is not clear how they could and should inform future evaluation and implementation research in the topics more recently prioritised by stakeholders.
In the present study, we aimed to identify and map the available evidence for allied health interventions in schools, i.e., interventions led by occupational therapists, physiotherapists, and/or speech and language therapists. We did not aim to synthesise evidence about intervention effectiveness, but rather to catalogue the available evidence base and make it more visible and accessible. This would support research funder, service commissioner, service provider, and researcher decision-making by: (i) highlighting clusters of evidence that could help guide future implementation efforts and evidence synthesis, (ii) identifying gaps in evidence where further primary research may be needed, and (iii) raising awareness of common elements in how diverse interventions are designed and delivered, which could help advance theory and research around intervention effectiveness.
Materials and methods
Our study was designed to answer the research question: what evidence is available regarding allied health interventions in schools for children and young people affected by neurodisability? We used systematic evidence mapping as a method for identifying and bringing together a multi-faceted body of evidence involving diverse populations, interventions, outcomes, and study designs. Our intended outputs were a user-friendly interactive evidence map for stakeholders (i.e., research funders, service commissioners, service providers, and researchers) and a descriptive summary of the existing evidence base. Evidence maps have been defined as “a systematic search of a broad field to identify gaps in knowledge and/or future research needs that presents results in a user-friendly format, often a visual figure or graph, or a searchable database” [Citation28 p.18]. There are currently no agreed methodological standards for systematic evidence mapping; therefore, we drew on general principles proposed by the Campbell Collaboration and published systematic evidence mapping processes [Citation28,Citation29]. For example, we determined the type of evidence to be included, developed a search strategy and coding framework in advance, included on-going studies by searching registries for primary studies and reviews, and produced a descriptive report [Citation29]. We did not publish a study protocol in advance.
We convened a multidisciplinary research team with service user experience of neurodisability and allied health interventions in schools (KKB, AG) as well as expertise in allied health practice and research (JMc, JLG, LP, SC), mainstream and special education practice and research (RW, KKB), and health and education service commissioning for children and young people with special educational needs and disabilities (KKB). Our service user co-investigators (KKB, AG) were involved in preparing the funding application, developing the research question, conducting the evidence mapping, designing the interactive evidence map, and reviewing the present manuscript.
Search strategy
Our search strategy was structured around four core concepts: children and young people, neurodisability, allied health, and schools and education settings. We generated search terms by selecting key words and coupling these with relevant medical subject headings and thesaurus-controlled standard terms, where available. All key words were truncated as appropriate and variant spellings were used. Search terms within each concept were combined using the Boolean operator “OR” and the results for each concept were combined using “AND”. We piloted the search strategy to ensure it was sensitive enough to identify seminal papers we would expect to see included.
The search strategy was developed in MEDLINE (see Supplementary Materials 1(a)) and then adapted for other bibliographic databases, specifically EMBASE, PsycINFO (both via Ovid), CINAHL, ERIC, British Education Index (all via EBSCO), Education Collection, IBSS, Social Science Database, Sociology Collection (all via Proquest), Cochrane Library, PEDro, OTseeker, speechBITE, and NIHR PROSPERO. Final searches were conducted 5–13 June 2019 and updated 15–21 May 2020. We also hand-searched the reference lists of relevant systematic reviews identified in the search results and two UK research funder websites (National Institute for Health Research and Education Endowment Foundation).
Eligibility criteria
One researcher (JMc) drafted preliminary eligibility criteria and piloted these using the results of MEDLINE searches. The criteria were critically discussed, refined, and finalised at a full research team meeting to ensure they could be consistently interpreted and applied systematically between researchers. The final eligibility criteria are presented in .
Table 1. Final eligibility criteria.
Screening and selection
Search results were de-duplicated in EndNote X8 (Thomson Reuters, San Francisco, CA) and then exported into Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) for screening and selection. One researcher (JMc) screened titles and abstracts of all records and excluded those clearly not meeting population, intervention, or context criteria. Two researchers (LP, RW) each double checked 10% of the excluded titles and abstracts. One researcher (JMc) screened the remaining full-text records against the eligibility criteria. A proportion (25%) of the excluded full texts was checked by another researcher (JLG, LP, or SC). All included full texts were double checked (KKB or AG). Errors or disagreements at each stage were resolved through discussion.
Data analysis
The final included studies were transferred from Covidence to EPPI-Reviewer research synthesis software version 4.12.2.0 (EPPI-Centre, University College London) for coding and analysis. A coding framework with definitions and rules for each individual code was developed and refined through research team meetings (). One researcher (JMc) completed all coding, drawing on topic expertise from research team members throughout the process.
Table 2. Coding framework.
For study characteristics, we coded study status (ongoing or completed), type, year, and country of publication. Quality assessments and risk of bias assessments have not consistently been incorporated into evidence mapping but are increasingly recommended. These were beyond the resources we had available, so instead we coded three methodological characteristics to characterise the overall nature of the evidence base: (i) study purpose, to establish how much of the existing evidence is concerned with feasibility testing/piloting, evaluating, or implementing interventions [Citation30], (ii) study design (e.g., before-after study, randomised controlled trial) [Citation31], to enable consideration of the potential strengths and weaknesses associated with particular study design features, and (iii) sample size, to highlight the scale of the existing evidence overall and of particular study designs. For study populations, we coded participants’ health conditions (e.g., cerebral palsy) and educational stages (e.g., pre-school). For interventions, we coded intervention leadership (i.e., occupational therapy, physiotherapy, speech and language therapy, or multidisciplinary), tier (i.e., universal, targeted, and/or intensive) [Citation16,Citation32,Citation33], and delivery (e.g., by teaching assistants). Within comparative studies, we did not code usual or standard care interventions.
For study outcomes, we took an inductive approach to coding that was informed by the International Classification of Functioning, Disability, and Health [Citation34] and responsive to the diversity in how included studies described their outcomes. First, we worked our way through the included studies individually and identified all outcomes. Where studies did not explicitly define their outcomes, we relied on background sections, measurement instruments, and results sections to aid our interpretation. Then, as we progressed through, we sorted conceptually similar outcomes into overall outcome categories and, embedded within these, more specific outcome sub-categories. We continuously checked and refined the consistency of our decision-making as we went along. Next, we selected verbatim examples of individual study outcomes to illustrate the variety within the sub-categories. Finally, we linked each sub-category to corresponding items within the ICF to further illustrate sub-categories’ meaning and content.
When all coding was completed, we explored the included studies by using frequency counts and cross-tabulation in EPPI-Reviewer to produce graphs in Microsoft PowerPoint. These visual displays enabled the research team to summarise and critically discuss the existing evidence. We used EPPI-Mapper version 2.1.0 (Digital Solution Foundry and EPPI-Centre, University College London) to create an interactive evidence map. To ensure the map would be a user-friendly and stand-alone resource, one researcher (JMc) produced multiple prototypes and obtained several rounds of feedback from both within the research team and from wider multidisciplinary stakeholders.
Results
Overview of included studies
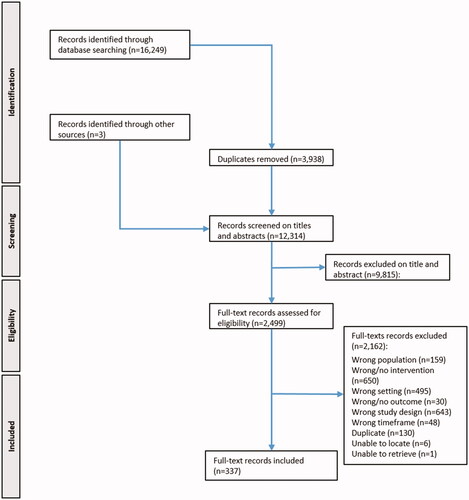
Screening and selection are summarised in . We identified 16 249 potentially relevant records, of which 12 314 remained after 3938 duplicates were removed. Screening of titles and abstracts resulted in exclusion of a further 9815 records. The remaining 2499 were subjected to full-text screening, of which we excluded 2162 and included 337.
Figure 1. PRISMA flowchart. A flowchart displaying that we identified 16 249 potentially relevant records, of which 12 314 remained after 3938 duplicates were removed. Screening of titles and abstracts resulted in exclusion of a further 9815 records. The remaining 2499 were subjected to full-text screening, of which we excluded 2162 and included 337.
The final 337 included studies are presented within the interactive evidence map, which contains the study titles, abstracts, digital object identifiers, and a downloadable Research Information Systems (RIS) file for importing the references into citation management software (see Supplementary Material 2 - available at https://researchportal.northumbria.ac.uk/en/publications/school-based-allied-health-interventions-for-children-and-young-p). Within the map, studies are displayed according to their outcome categories and sub-categories, participants’ educational stages, and intervention leadership, which is colour-coded and can be presented in different styles (e.g., a bubble-map or heat-map) to show the proportion of studies led by the different allied health disciplines. The display can also be filtered according to each parameter in our coding framework. The references for the 337 studies are also available in the Supplementary Materials (1b).
Overall, 325/337 included studies (96.4%) were completed and 12 (3.6%) were ongoing (eight randomised controlled trials and four systematic reviews). The majority of studies were research papers (291/337, 86.3%), 23 were conference papers (6.8%), 12 were protocols for the ongoing studies (3.6%), and 11 were PhD theses (3.3%). Speech and language therapy-led interventions accounted for 117/337 studies (34.7%), occupational therapy-led for 96 (28.5%), multidisciplinary-led for 85 (25.2%), and physiotherapy-led for 39 (11.6%). Across the studies of multidisciplinary-led interventions (n = 85), occupational therapists and speech and language therapists were each involved in delivering 45/85 (52.9%) and physiotherapists in 23/85 (27.1%).
The studies were conducted in 33 countries () with the United States (US) accounting for almost half of included studies and the top five countries (US, UK, Australia, Canada, Israel) accounting for three quarters. The remaining 28 countries accounted for one quarter of included studies. As the two biggest producers of research, the US and UK produced considerably fewer physiotherapy-led studies, and the UK also produced relatively fewer occupational therapy-led studies, even when occupational and physiotherapy involvement in multidisciplinary-led studies was taken into account.
Table 3. Country of publication for the included studies (n = 337).
Year of publication is presented in . Ignoring studies published between 2004 and 2008 (because we included selected exemplar studies only) and 2020 (because our final searches were conducted in May 2020), there appeared to be an overall slight upward trajectory in the number of studies being published each year between 2009 and 2019 (). This may be attributable to small increases in research from the UK and Australia across that time period (6/8 ongoing randomised controlled trials were UK-based and 4/4 ongoing systematic reviews were Australia-based) as well as a slight increase in the number of speech and language therapy-led studies ().
Figure 2. Total number of studies published per year. A line graph displaying the total number of studies published per year between 2009 and 2019. 21 studies were published in 2009, 23 in 2010, 30 in 2011, 25 in 2012, 28 in 2013, 28 in 2014, 20 in 2015, 20 in 2016, 40 in 2017, 28 in 2018, and 36 in 2019.
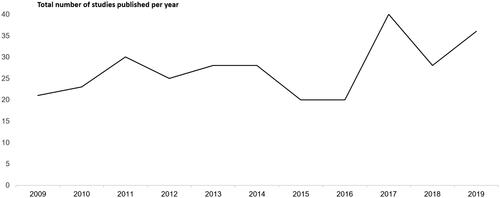
Figure 3. Total number of studies published per year by intervention leadership. A line graph displaying the total number of occupational therapy-led, physiotherapy-led, speech and language therapy-led, and multidisciplinary-led studies published per year between 2009 and 2019. Respectively, these were: 2009 - 9, 1, 9, 2; 2010 - 8, 4, 7, 4; 2011 - 9, 3, 4, 14; 2012 - 7, 2, 9, 7; 2013 - 7, 5, 11, 5; 2014 - 5, 1, 13, 9; 2015 - 9, 6, 3, 2; 2016 - 6, 0, 7, 7; 2017 - 13, 4, 12, 11; 2018 - 8, 6, 9, 5; 2019 - 8, 4, 18, 6.
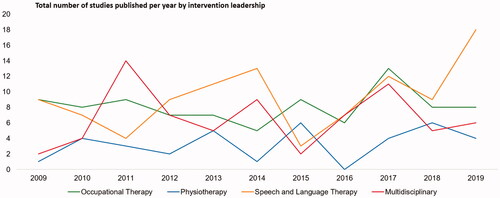
Table 4. Year of publication for the included studies (n = 337).
Methodological characteristics
Variable quality of reporting made it challenging to screen and analyse studies. For example, it was often difficult to establish whether interventions were delivered in schools as opposed to clinical or other community settings. Multiple publications arising from the same research programme and similar-looking studies from the same research groups were not always cross-referenced or differentiated, which necessitated further checking to identify related studies and compare them for duplication.
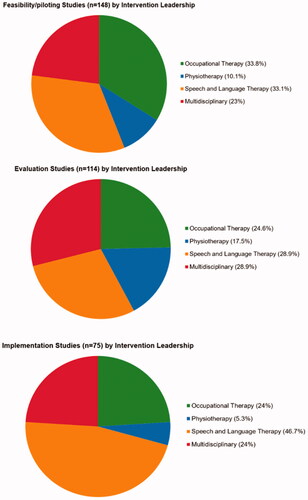
Methodological characteristics are presented in . Overall, almost half the studies focused on feasibility testing/piloting, a third on evaluation, and almost a quarter on implementation. It was challenging to code for study purpose because studies were not usually framed in these terms. We made judgements on a case-by-case basis, taking into account the code definitions (), study design and sample size, how the study rationale was presented in the background section, and what kinds of limitations were noted in the discussion section.
Table 5. Methodological characteristics of included studies (n = 337).
Before-after was the most common study design for included studies overall, for feasibility/pilot studies, and for implementation studies (). Randomised controlled trial was the second most common study design overall and the most common design for evaluation studies. Of all included studies, just over half had a sample size of ≤30, just over a quarter had ≤10 participants, just under half had a sample size of ≥31, and almost one sixth had >100 participants ().
Evaluation studies (114/337), particularly those using randomised controlled trial designs, were distributed across all four intervention leadership categories and a substantial proportion fell within physiotherapy ( and ). This was noteworthy given that physiotherapy-led interventions accounted for only a small proportion of included studies overall. Conversely, very few implementation studies related to physiotherapy. Almost half of the implementation studies related to speech and language therapy and implementation was the purpose of almost a third of all speech and language therapy-led studies (). These proportions were greater than other intervention leadership categories, suggesting a more established tradition within speech and language therapy of research on topics such as training, models of intervention delivery, and service delivery models.
Figure 4. Study purpose by intervention leadership. Three pie charts displaying study purpose by intervention leadership. 33.8% of feasibility/piloting studies, 24.6% of evaluation studies, and 24% of implementation studies were occupational therapy-led. 10.1% of feasibility/piloting studies, 17.5% of evaluation studies, and 5.3% of implementation studies were physiotherapy-led. 33.1% of feasibility/piloting studies, 28.9% of evaluation studies, and 46.7% of implementation studies were speech and language therapy-led. 23% of feasibility/piloting studies, 28.9% of evaluation studies, and 24% of implementation studies were multidisciplinary-led.
Population characteristics
Participants’ health conditions are presented in . The five most commonly reported health conditions were autism spectrum disorder, physical disabilities (a broad code incorporating cerebral palsy, neuromuscular conditions, spinal cord injuries, spina bifida, multiple disabilities, and medical complexity), cerebral palsy only, developmental language disorder, and learning/intellectual disability. Almost a quarter of studies reported no health conditions, meaning that these studies either related to whole-school populations, which we assumed would include children and young people affected by neurodisability even if this was not explicitly reported, or used unspecific, descriptive terms such as “fine motor difficulties” or “speech and language difficulties”, which were not coded (see for coding definitions).
Table 6. Health conditions of participants across the included studies (n = 337).
Many studies included participants across different educational stages (e.g., pre-school and primary school). Overall, almost half of the studies included pre-school participants, almost two thirds included primary school participants, just over a quarter included secondary school participants, and a very small proportion included post-secondary school participants or participants transitioning between educational stages (). When studies focused specifically on participants at only one educational stage, this was more commonly only the primary school stage, followed by only pre-school, only secondary, only transitions, and only post-secondary ().
Table 7. Educational stages of participants in the included studies (n = 337).
Educational stage is set out by intervention leadership in . We noted that few studies including or focusing only on pre-school participants were led by physiotherapy and that over half of studies focusing specifically on secondary school participants were led by speech and language therapy.
Figure 5. Educational stage by intervention leadership. Six pie charts displaying educational stage by intervention leadership. Respectively, studies of occupational therapy, physiotherapy, speech and language therapy, and multidisciplinary interventions accounted for the following proportion of studies for each educational stage: studies including pre-school children (n = 145) - 24.8%, 6.2%, 37.2%, 31.7%; studies of pre-school children only (n = 92) - 26.1%, 4.4%, 37%, 32.6%; including primary school (n = 210) - 29%, 14.8%, 32.9%, 23.3%; primary school only (n = 115) - 33.9%, 8.7%, 35.7%, 23.3%; including secondary school (n = 88) - 20.5%, 25%, 28.4%, 26.1%; secondary school only (n = 23) - 21.7%, 8.7%, 52.2%, 17.4%.

Intervention characteristics
It was challenging to differentiate and code for intervention tiers (i.e., universal, targeted, and intensive) because these are relatively recent concepts in allied health and studies were not usually framed in these terms. Universal interventions were reported in almost a quarter of included studies (73/337, 21.7%), targeted interventions in just over a third (131/337, 38.9%), and intensive interventions in almost two thirds (203/337, 60.2%).
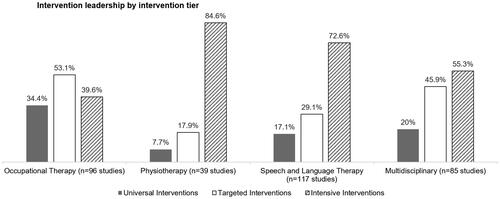
and present intervention tier and intervention leadership. We noted that almost half of all universal interventions were occupational therapy-led and that just over a third of all occupational therapy-led studies reported a universal intervention. The predominance of occupational therapy-led universal interventions is consistent with the finding that almost half of studies reporting no health conditions amongst participants were also occupational therapy-led (). We noted few universal interventions involving physiotherapy. Studies reporting targeted interventions were distributed across all four intervention leadership categories, suggesting an established tradition across allied health of research on topics such as “at risk” groups and co-delivery of interventions with education staff.
Figure 6. Intervention tier by intervention leadership. Three bar charts displaying intervention tier by intervention leadership. Respectively, studies of occupational therapy, physiotherapy, speech and language therapy, and multidisciplinary interventions accounted for the following proportion of studies of universal, targeted, and intensive interventions: universal (n = 73) - 45.2%, 4.1%, 27.4%, 23.3%; targeted (n = 131) - 38.9%, 5.3%, 26%, 29.8%; intensive (n = 203) - 18.7%, 16.3%, 41.9%, 23.2%.
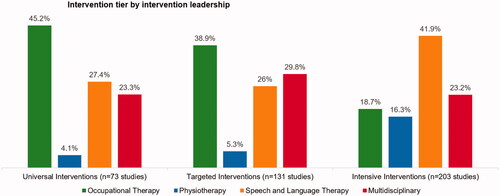
Figure 7. Intervention leadership by intervention tier. Four bar charts displaying intervention leadership by intervention tier. Respectively, studies of universal, targeted, and intensive interventions accounted for the following proportion of studies of occupational therapy, physiotherapy, speech and language therapy, and multidisciplinary interventions: occupational therapy (n = 96) - 34.4%, 53.1%, 39.6%; physiotherapy (n = 39) - 7.7%, 17.9%, 84.6%; speech and language therapy (n = 117) - 17.1%, 29.1%, 72.6%; and multidisciplinary (n = 85) - 20%, 45.9%, 55.3%.
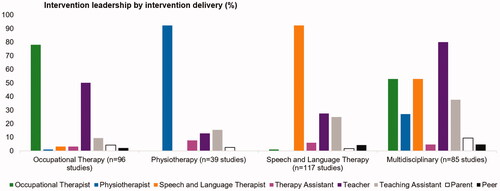
and set out intervention delivery both overall and according to intervention leadership. As would be expected, occupational therapy-led, physiotherapy-led, and speech and language therapy-led interventions were delivered in large part by occupational therapists, physiotherapists, and speech and language therapists, respectively. Otherwise, we noted the frequent involvement of teachers and teaching assistants in delivering interventions. Teachers were particularly involved in delivering occupational therapy-led and multidisciplinary-led interventions. Teaching assistants were particularly involved in delivering speech and language therapy-led and multidisciplinary-led interventions.
Figure 8. Intervention delivery across included studies. A bar chart displaying who delivered the interventions across the 337 included studies, in descending order of frequency. Speech and language therapists were involved in intervention delivery in 46.3% of included studies. Teachers in 45.4%. Occupational therapists in 35.9%. Teaching assistants in 22.6%. Physiotherapists in 17.8%. Therapy assistants in 5%. Parents in 4.5%. Peers in 2.3%.
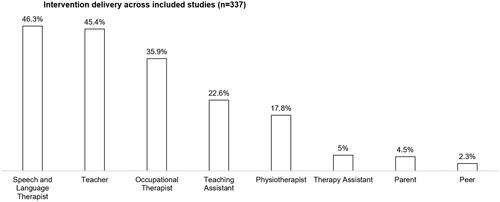
Figure 9. Intervention leadership by intervention delivery. Four bar charts displaying intervention leadership by intervention delivery. Respectively, interventions were delivered by occupational therapists, physiotherapists, speech and language therapists, therapy assistants, teachers, teaching assistants, parents, and peers as follows: for occupational therapy-led interventions (n = 96) - 78.1%, 1%, 3.1%, 3.1%, 50%, 9.4%, 4.2%, 2.1%; physiotherapy-led (n = 39) - 0%, 92.3%, 0%, 7.7%, 12.8%, 15.4%, 2.6%, 0%; speech and language therapy-led (n = 113) - 0.9%, 0%, 92.3%, 6%, 27.4%, 24.8%, 1.7%, 4.3%; and multidisciplinary-led (n = 85) - 52.9%, 27.1%, 52.9%, 4.7%, 80%, 37.6%, 9.4%, 4.7%.
Outcomes
Across the included studies, our coding produced eight overall outcome categories and, embedded within these, 46 sub-categories ().
Table 8. Outcome categories and sub-categories across the included studies (n = 337).
presents the eight overall outcome categories in order of number of studies included in each category. The eight overall outcome categories were: (i) social communication, interaction, and behaviour, (ii) support within the educational environment (e.g., teacher and teaching assistant knowledge and skills; support from peers; school and local authority policy), (iii) voice, speech, language, and communication, (iv) engaging in school and education (e.g., writing and learning to write; reading, learning to read, and literacy; making academic progress), (v) mobility, movement, and motor skills, (vi) using assistive technology, (vii) other outcomes (e.g., quality of life and subjective wellbeing), and (viii) play, recreation, and leisure.
presents the 46 sub-categories in order of number of studies included in each sub-category. The top ten outcome sub-categories were: (i) expressive language and communication, (ii) receptive language and communication, (iii) broad social communication and interaction (e.g., social skills, shared attention, pragmatic language skills), (iv) teacher and teaching assistant knowledge and skills, (v) gross motor skills, (vi) writing and learning to write, (vii) on task behaviour and engagement in the classroom, (viii) fine motor skills, (ix) using speech-generating devices, and (x) social interaction specifically with peers. also sets out outcome sub-categories by intervention leadership. Overall, intervention leadership reflected field of expertise for outcome sub-categories, for example interventions targeting language and communication outcomes were primarily led by speech and language therapists. Otherwise, it was noteworthy that teacher and teaching assistant knowledge and skills was the fourth largest outcome sub-category, indicating that these professionals are commonly receiving as well as delivering allied health interventions.
Table 9. Outcome sub-categories by intervention leadership.
The Supplementary Materials (1c) set out the outcome categories and sub-categories along with verbatim examples of individual study outcomes that illustrate each sub-category and corresponding items within the ICF. As much as was possible, we developed categories and sub-categories that were distinct from each other. However, study outcomes were not always clearly reported or explicitly defined and there was some overlap, particularly in corresponding ICF items.
Across the included studies, we identified sixty-two randomised controlled trials concerned with evaluation (47/62) or implementation (15/62) of allied health interventions. Collectively, the trials covered all eight outcome categories and 37/46 outcome sub-categories. The Supplementary Materials (1d) present the trials according to country, intervention leadership, sample size, educational stages, and outcome categories and sub-categories. Across the trials, the five most common overall outcome categories were: (i) mobility, movement and motor skills (21/62 trials), (ii) engaging in school and education (18/62), (iii) voice, speech, language, and communication (17/62), (iv) social communication, interaction, and behaviour (15/62), and (v) support within the educational environment (14/62). The ten most common outcome sub-categories were: (i) gross motor skills (12/62 trials), (ii) fine motor skills (11/62), (iii) expressive language and communication (11/62), (iv) receptive language and communication (9/62), (v) broad social communication and interaction (9/62), (vi) writing and learning to write (9/62), (vii) teacher and teaching assistant knowledge and skills (7/62), (viii) quality of life and subjective wellbeing (7/62), (ix) on-task behaviour and engagement in the classroom (6/62), and (x) confidence, self-efficacy, and self-perception (6/62).
Discussion
Summary of results
We systematically mapped 337 studies investigating the effectiveness of allied health interventions in schools and education settings for children and young people affected by neurodisability. A number of features were noteworthy across this evidence base. First, the interventions targeted highly diverse outcomes, many of which related to educational participation (e.g., writing and learning to write; reading, learning to read, and literacy; making academic progress) and characteristics of the school environment (e.g., teacher and teaching assistant knowledge and skills; support from peers; school and local authority policy). This suggests that, at least implicitly, allied health professionals emphasise educational participation and school environments as central to children and young people’s wider health and social outcomes. Second, many of the interventions were multidisciplinary, in that they involved multiple allied health disciplines, as well as teachers and teaching assistants, in their design and delivery. Third, a significant proportion of studies included universal and targeted interventions, reflecting an emphasis on tiered models of interventions. Fourth, interventions focused primarily on pre-school and primary school populations and settings, and considerably less on secondary, post-secondary, or transitions.
Finally, almost half the included studies conducted early feasibility testing/piloting of interventions and just over half had sample sizes of ≤30 participants, indicating that much of the evidence base is concerned with smaller-scale preliminary research rather than definitive evaluation and systematic implementation. We identified a significant number of randomised controlled trials (n = 62) focused on evaluation and implementation. However, the trials were widely distributed over all eight of our overall outcome categories and 37/46 outcome sub-categories, suggesting a thinly spread evidence base with limited opportunity for synthesising evidence about effectiveness. It was beyond our scope to determine whether the randomised controlled trials had followed on from and directly built upon the results of preliminary feasibility testing/piloting studies. Therefore, we are unable to assess the extent to which research in this field is adopting a strategic and cumulative approach to developing, testing, evaluating, and implementing allied health interventions.
Strengths and limitations of the systematic evidence mapping
We have brought together a large and diverse body of evidence to be accessible for stakeholders including research funders, service commissioners, and allied health service providers, educators, and researchers. A key factor in achieving this was the multidisciplinary nature of our research team. Our sensitive search strategy, comprehensive eligibility criteria, and detailed screening mean we can state with certainty that the included allied health interventions were delivered specifically in schools, which likely indicates their feasibility and acceptability in education settings. Our interactive evidence map can be continuously updated to incorporate relevant studies flagged by wider stakeholders and identified through regular searches. The evidence map could potentially be used to identify intervention options for particular outcomes or educational stages and cross-reference these with other peer-reviewed resources that summarise the strength of evidence for some interventions, for example the “What Works” online database of interventions to support children and young people’s speech, language and communication, hosted by the children’s communication charity “I CAN” and the “Teaching and Learning Toolkit” summary of education evidence from the Education Endowment Foundation.
The main limitation is that we did not conduct a quality or risk of bias assessment of the included studies and our scope did not extend to synthesising evidence about intervention effectiveness. A further limitation is that our searches were most recently updated in May 2020 and more recent studies will not have been included. However, our study is comprehensive in that it includes 337 papers, and our search strategy and coding framework are clearly reported and can be replicated to further update the evidence map. We recognise that, as one researcher conducted the screening and only 20% of titles and abstracts and 25% of excluded records were double-checked, some relevant studies may have been missed. However, the topic expertise within our multidisciplinary research team likely mitigated this risk somewhat.
How the results compare with wider literature
Our study highlights the diverse health, social, and educational outcomes towards which school-based allied health interventions are directed internationally. As well as seeking to improve outcomes typically considered health-related (e.g., language, communication, and motor skills), the interventions also target educational participation (e.g., literacy, academic achievement, participation across the school day) and characteristics of the school environment (e.g., educators’ knowledge and skills, peer support, school policy). This illustrates how, across countries and health systems, allied health operates at the intersection of health and education, recognising at least implicitly that these outcomes are inextricably linked, and conceptualising educational participation as both a consequence and determinant of children and young people’s health. Previous research has reported similar views amongst children and young people affected by neurodisability and their parents, exploring how they also conceptualise educational participation as an important health outcome that impacts on and is impacted by other aspects of health [Citation35].
From a UK perspective, our results are directly relevant to recent Priority Setting Partnerships (PSPs) facilitated by the James Lind Alliance (JLA). The JLA brings service users, carers, and professionals together in PSPs to identify and prioritise unanswered questions or evidence uncertainties that they agree are the most important [Citation36]. The PSPs aim to make sure that health research funders are aware of the issues that matter most to the people who need to use the research in their everyday lives and the methods used are designed to change the way research funding is granted [Citation36]. As children and young people spend a good deal of their time in school, it is unsurprising that stakeholders in the PSPs for autism [Citation21], childhood disability [Citation19], learning difficulties [Citation20], and mental health [Citation22], all of which included children and young people, parents, and professionals, highly prioritised research questions related to supporting educational participation and improving characteristics of school environments (). Our study has demonstrated that allied health interventions delivered in schools are geared towards many of the same outcomes and should therefore be eligible for future health research funding to better understand their impact and cost-effectiveness.
One important finding of our study is that teachers and teaching assistants play a central role in allied health interventions in schools. They deliver many of the interventions and our results suggest that improving teacher and teaching assistant knowledge and skills is a common mechanism of how allied health supports children and young people’s health outcomes. Our research team’s lived experience suggests that teaching assistants in particular are significantly more involved than our results estimate in both delivering and receiving allied health interventions. For example, in the UK health and education system, teaching assistants are relied heavily upon to deliver school-based programmes designed by physiotherapists, as well as occupational therapists and speech and language therapists, particularly for children and young people whose special educational needs and disabilities are legally recognised within education, health, and care plans. Allied health professionals spend significant amounts of time training teaching assistants to carry out school-based tasks such as using hoists and toilet seats, delivering postural care and mobility programmes, and facilitating language interventions in small groups. In addition, many individuals employed as teaching assistants in schools also perform personal assistant roles at home and in the wider community, supporting children and young people’s participation in self-care, recreation, and leisure. Therefore, optimally preparing and appropriately deploying this section of the education workforce in relation to allied health interventions could enhance children and young people’s wider health and social outcomes. Wider evidence has demonstrated that a comprehensive, whole-school approach to preparing, deploying, and training teaching assistants has a positive impact on students’ outcomes, including students with special educational needs and disabilities [Citation37]. This existing evidence base could form a theoretical and practical starting point for developing, testing, evaluating, and implementing a programme to maximise how allied health professionals work with teaching assistants to support children and young people affected by neurodisability.
It is noteworthy that, along with intensive, individualised support for children and young people with the most complex and persistent needs, universal and targeted support are key features of tiered allied health intervention models (see for definitions). A recent evidence review of approaches to supporting children and young people with special educational needs and disabilities concluded that tiered models are an effective way for allied health professionals and mainstream schools to work together to improve health, social, and educational outcomes [Citation38]. Such models are well-established in North America and are of increasing interest to UK allied health professionals and their commissioners [e.g., Citation27]. However, whilst specific models have been proposed [e.g., Citation39] and comprehensive universal resources are available [e.g., Citation40], formal testing of tiered models is lagging behind in the UK compared to our international colleagues.
Implications for future research
Our study has established that allied health interventions in schools directly relate to existing research priorities around improving educational participation and characteristics of school environments (). However, we understand that these research priorities have so far received limited attention from major health research funders in the UK [Citation41]. For example, the JLA PSP for childhood disability has been one of the most successful PSPs, attracting much-needed investment in at least twelve research priorities but little if any investment in the priorities set out in [Citation41,Citation42]. Three factors might explain this discrepancy. First, it may not be immediately clear how research priorities around educational participation and school environments fit within the scope of health research funding programmes accustomed to working with more conventional physical and mental health-related topics. Second, funders may be unaware of the extent to which NHS allied health professionals actually work in schools supporting children and young people’s function, participation, and inclusion in school environments. Third, allied health may need to put forward to funders more clearly and convincingly the candidate interventions they would prioritise for further research and set out how these could be compared with usual NHS care. The wider childhood neurodisability community has a strong track record in working with UK health research funders to develop commissioned calls based on JLA PSP research priorities [Citation42]. This approach could be extended to address the remaining unanswered research questions that children and young people, parents, and professionals have identified as the most important ().
Preparation and deployment of teaching assistants within allied health interventions and evaluation and implementation of tiered intervention models should be specific priorities for future research across allied health disciplines, both in the UK and in similar health and education systems internationally. These topics would also help to address the stakeholder research priorities set out in and would respond to parents’ concerns about the delivery and accessibility of allied health support [Citation18]. Research on the preparation and deployment of teaching assistants would need to take into account known concerns and potential unintended consequences identified in wider evidence, for example any potential risk of inappropriate over-reliance on teaching assistants to the detriment of direct support from an allied health professional [Citation43]. Within tiered intervention models, the relative benefits and cost-effectiveness of many of the interventions at each tier also need to be established [Citation39]. Our interactive evidence map can now be used to help stakeholders select candidate universal, targeted, and intensive interventions most in need of further evaluation and implementation research.
Summary
Whilst allied health professionals are largely employed by health services, much of their support for children and young people affected by neurodisability is delivered in schools and education settings. As well as targeting outcomes typically considered health-related (e.g., language, communication, and motor skills), allied health interventions routinely seek to support and improve wider determinants of children and young people’s health, including educational participation (e.g., literacy, academic progress) and characteristics of school environments (e.g., educators’ knowledge and skills, support from peers). In the UK, school-based allied health interventions relate directly to unanswered research questions prioritised highly by diverse stakeholders. The onus is now on the allied health and wider childhood neurodisability community to highlight for research funders the candidate interventions they would prioritise for further research. We have presented an interactive evidence map and descriptive summary of the existing evidence base that will support this decision-making.
We have also identified two common elements across diverse allied health interventions. First, the interventions rely heavily on teachers and particularly teaching assistants in terms of both their practical delivery and their underlying theory that improving these educators’ knowledge and skills in turn improves outcomes for children and young people. Second, tiered models of universal, targeted, and intensive allied interventions are common and their effectiveness is supported in the wider evidence. However, formal testing of tiered models is lagging behind in the UK compared to internationally. Therefore, preparation and deployment of teaching assistants within allied health interventions and evaluation and implementation of tiered intervention models should be specific priorities for future research across allied health disciplines, both in the UK and in similar health and education systems internationally.
Box 1. Stakeholder research priorities related to the educational participation and school environments of children and young people affected by neurodisability.
Supplementary_Materials_2_-_Interactive_Evidence_Map.html
Download HTML (1.7 MB)Supplementary_Materials_1_-_Allied_health_neurodisability_systematic_evidence_mapping.docx
Download MS Word (79.8 KB)Acknowledgements
We are very grateful for the input we received from Dr Melissa Bond (EPPI-Reviewer Support Officer & Trainer, University College London), Mr Zak Ghouze (Software and Information Technology Officer, University College London), and Dr Penny Williams (Consultant Speech and Language Therapist, Guy’s and St. Thomas’ NHS Foundation Trust). We would also like to acknowledge Newcastle University (Population Health Sciences Institute), Cambridge University (Faculty of Education), University College London (Institute of Education), Sussex Community NHS Foundation Trust, and Leeds Community Healthcare NHS Trust.
We are particularly grateful to our service user co-investigators (KKB, AG) and to Ria (young disability artist, Leeds) who designed a logo for the wider research programme towards which the systematic evidence mapping contributed. We also thank the peer reviewers whose constructive feedback improved our manuscript.
Disclosure statement
No authors have financial relationships with any organisations that might have an interest in the submitted work in the previous three years. No authors have other relationships or activities that could appear to have influenced the submitted work.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Department for Work and Pensions. National statistics. Family resources survey: financial year 2019 to 2020. United Kingdom; 2021.
- Department of Health. Annual report of the chief medical officer 2012, our children deserve better: Prevention pays. United Kingdom; 2013.
- Morris C, Janssens A, Tomlinson R, et al. Towards a definition of neurodisability: a delphi survey. Dev Med Child Neurol. 2013;55(12):1103–1108.
- Blackburn C, Spencer N, Read J. Prevalence of childhood disability and the characteristics and circumstances of disabled children in the UK: secondary analysis of the family resources survey. BMC Pediatr. 2010;10(1):21.
- Spencer NJ, Blackburn CM, Read JM. Disabling chronic conditions in childhood and socioeconomic disadvantage: a systematic review and meta-analyses of observational studies. BMJ Open. 2015;5(9):e007062.
- Colver A, Rapp M, Eisemann N, et al. Self-reported quality of life of adolescents with cerebral palsy: a cross-sectional and longitudinal analysis. The Lancet. 2015;385(9969):705–716.
- Chatzitheochari S, Parsons S, Platt L. Doubly disadvantaged? bullying experiences among disabled children and young people in England. Sociology. 2016;50(4):695–713.
- Jones L, Bellis MA, Wood S, et al. Prevalence and risk of violence against children with disabilities: a systematic review and meta-analysis of observational studies. Lancet. 2012;380(9845):899–907.
- Chatzitheochari S, Platt L. Disability differentials in educational attainment in England: primary and secondary effects. Br J Sociol. 2019;70(2):502–525.
- Office for National Statistics. Outcomes for disabled people in the UK: 2020. 2021.
- World Health Organization & World Bank. World report on disabiliity. Geneva: World Health Organization & World Bank; 2011.
- Beresford B, Clarke S, Maddison J. Therapy interventions for children with neurodisabilities: a qualitative scoping study. Health Technol Assess. 2018;22(3):1–150.
- Anaby DR, Campbell WN, Missiuna C, GOLDs (Group for Optimizing Leadership and Delivering Services), et al. Recommended practices to organize and deliver school-based services for children with disabilities: a scoping review. Child Care Health Dev. 2019;45(1):15–27.
- Maciver D, Rutherford M, Arakelyan S, et al. Participation of children with disabilities in school: a realist systematic review of psychosocial and environmental factors. PLOS One. 2019;14(1):e0210511.
- Ford J, et al. Rapid review of the impact of allied health professionals on health inequalities. 2021. Cambridge: University of Cambridge.
- World Federation of Occupational Therapists, Position statement on occupational therapy services in school-based practice for children and youth. 2016.
- Children and Families Act. United Kingdom; 2014.
- Office for Standards in Education Children's Services and Skills (Ofsted). SEND: old issues, new issues, next steps. United Kingdom: Ofsted; 2021.
- Morris C, Simkiss D, Busk M, et al. Setting research priorities to improve the health of children and young people with neurodisability: a British academy of childhood disability-James lind alliance research priority setting partnership. BMJ Open. 2015;5(1):e006233–e006233.
- Lim AK, Rhodes S, Cowan K, et al. Joint production of research priorities to improve the lives of those with childhood onset conditions that impair learning: the james lind alliance priority setting partnership for ‘learning difficulties. BMJ Open. 2019;9(10):e028780.
- Autistica. Your questions: shaping future autism research. United Kingdom: Autistica; 2016.
- McPin Foundation. Research priorities for children and young peoples mental health - interventions and services. United Kingdom: McPin Foundation; 2018.
- Boyle JM, McCartney E, O'Hare A, et al. Direct versus indirect and individual versus group modes of language therapy for children with primary language impairment: principal outcomes from a randomized controlled trial and economic evaluation. Int J Lang Commun Disord. 2009;44(6):826–846.
- Adams C, Lockton E, Freed J, et al. The social communication intervention project: a randomized controlled trial of the effectiveness of speech and language therapy for school-age children who have pragmatic and social communication problems with or without autism spectrum disorder. Int J Lang Commun Disord. 2012;47(3):233–244.
- Zwicker JG. and A.F. Hadwin. Cognitive versus multisensory approaches to handwriting intervention: a randomized controlled trial. OTJR: Occupation, Participation and Health. 2009;29(1):40–48.
- Verschuren O, Ketelaar M, Gorter JW, et al. Exercise training program in children and adolescents with cerebral palsy: a randomized controlled trial. Arch Pediatr Adolesc Med. 2007;161(11):1075–1081.
- Missiuna CA, Pollock NA, Levac DE, et al. Partnering for change: an innovative School-Based occupational therapy service delivery model for children with developmental coordination disorder. Can J Occup Ther. 2012;79(1):41–50.
- Miake-Lye IM, Hempel S, Shanman R, et al. What is an evidence map? a systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016;5(1):28.
- Saran A, White H. Evidence and gap maps: a comparison of different approaches. Campbell Syst Rev. 2018;14(1):1–38.
- Craig P, Dieppe P, Macintyre S, Medical Research Council Guidance, et al. Developing and evaluating complex interventions: the new medical research council guidance. BMJ. 2008;337:a1655.
- Seo H-J, Kim SY, Lee YJ, et al. A newly developed tool for classifying study designs in systematic reviews of interventions and exposures showed substantial reliability and validity. J Clin Epidemiol. 2016;70:200–205.
- Chu S. Supporting children with special educational needs (SEN): an introduction to a 3-tiered school-based occupational therapy model of service delivery in the United Kingdom. World Federation Occup Ther Bull. 2017;73(2):107–116.
- Hutton E, Tuppeny S, Hasselbusch A. Making a case for universal and targeted children’s occupational therapy in the United Kingdom. British J Occup Ther. 2016;79(7):450–453.
- World Health Organization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization; 2001.
- Allard A, Fellowes A, Shilling V, et al. Key health outcomes for children and young people with neurodisability: qualitative research with young people and parents. BMJ Open. 2014;4(4):e004611.
- Lind Alliance J. The James Lind Alliance. Available from: https://www.jla.nihr.ac.uk/
- Webster R, et al. Maximising the impact of teaching assistants in primary schools: a practical guide for school leaders. Oxon: Routledge; 2021.
- Cullen M, et al. Special educational needs in mainstream schools: Evidence review. London: Education Endowment Foundation; 2020.
- Ebbels SH, McCartney E, Slonims V, et al. Evidence-based pathways to intervention for children with language disorders. Int J Lang Commun Disord. 2019;54(1):3–19.
- Maciver D, Hunter C, Johnston L, et al. Using stakeholder involvement, expert knowledge and naturalistic implementation to Co-Design a complex intervention to support children’s inclusion and participation in schools: the CIRCLE framework. Children. 2021;8(3):217.
- Lind Alliance J. Priority Setting Partnerships. Funded research. 2020. Available from: https://www.jla.nihr.ac.uk/making-a-difference/funded-research.htm
- Parr J. Ten years of the BACD strategic research group: maximizing opportunities for paediatric neurodisability research. Dev Med Child Neurol. 2018;60(6):531–531.
- Webster R, De Boer AA. Where next for research on teaching assistants: the case for an international response. Eur J Special Needs Education. 2021;36(2):294–305.
