Abstract
Purpose
Supported self-management (SSM) is an important part of adapting to life after stroke however it is a complex concept. It is unclear what SSM in stroke consists of or how stroke survivors, families, and clinicians can most effectively work together to support person-centred self-management. In this study, we aimed to explore what was most important in making SSM work in community stroke rehabilitation.
Methods
We conducted a Q-methodology study with stroke survivors (n = 20), community-based stroke clinicians (n = 20), and team managers (n = 8) across four health boards in Scotland, United Kingdom. Participants ranked 32 statements according to their importance in making SSM work. Factor analysis was used to identify shared viewpoints.
Results
We identified four viewpoints: (i) A person-centred approach to build self-confidence and self-worth; (ii) Feeling heard, understood, and supported by everybody; (iii) Preparation of appropriate resources; and (iv) Right thing, right place, right time for the individual. Important across all viewpoints were: a trusting supportive relationship; working in partnership; focusing on meaningful goals; and building self-confidence.
Conclusions
Differing views exist on what is most important in SSM. These views could be used to inform quality improvement strategies to support the delivery of SSM that considers the preferences of stroke survivors.
Clinicians should be aware of their own viewpoint of supported self-management and consider how their perspective may differ from stroke survivors’ and colleagues’ perspectives of what’s important to support self-management.
Working in partnership with stroke survivors plus developing a trusting and supportive relationship with them are core components of supporting self-management in the longer term after stroke.
Building a sense of self-worth and self-confidence, a focus on meaningful goals, training and support for staff, and tailoring support to people’s needs at the right time are important considerations for supporting longer-term engagement in self-management.
IMPLICATIONS FOR REHABILITATION
Introduction
There are currently 1.3 million stroke survivors in the UK [Citation1], and over 80 million stroke survivors worldwide [Citation2]. The complex and enduring physical, cognitive, and psychosocial consequences of stroke require effective long-term support across inpatient and community settings [Citation3–5]. SSM is a core component of policies and frameworks on long-term condition management across the UK and internationally, and is a recognized, multidisciplinary approach for supporting people after stroke [Citation6–8]. SSM has been found in clinical trials to improve quality of life, disability, and self-efficacy amongst stroke survivors [Citation9–11]. Despite the importance of SSM, evidence shows that the provision of SSM in practice does not consistently address stroke survivor’s self-management needs or priorities. Also, the implementation of SSM is variable across different geographical and organisational contexts of community-based stroke rehabilitation [Citation12–14]. The impact of the global pandemic is likely to have compounded unmet self-management needs [Citation1].
Interpretation of SSM has ranged from SSM being viewed as compliance with professional advice or treatment plans, to being seen as a more collaborative approach centered around the person’s needs [Citation15,Citation16]. Our previous research suggests that such different interpretations are likely to contribute to the variation in SSM provision in community rehabilitation settings [Citation16]. Furthermore, confusion remains about what SSM in stroke is, where it fits in the life after stroke pathway and how best to deliver SSM that meaningfully addresses stroke survivors’ longer-term needs [Citation16,Citation17]. Thus, whilst there is evidence to suggest SSM is effective, challenges in its implementation in practice [Citation18] mean that stroke survivors can continue to report unmet needs in the longer term after stroke.
We designed a realist evaluation study to understand more about how SSM is implemented and what makes it work in different settings of community stroke rehabilitation [Citation19]. An embedded Q-methodology study was undertaken in the first phase of the realist evaluation study to explore the views of stroke survivors, clinicians working in stroke community teams, and managers of community teams to identify how SSM is understood by them and their perceptions of what is important to make SSM work in community stroke care. The findings from the Q-methodology study are reported in this paper and help to offer an understanding of what SSM involves and what is required in facilitating the delivery of consistent, tailored, and sustainable SSM in community stroke care.
Material and methods
Combining realist evaluation and Q methodology
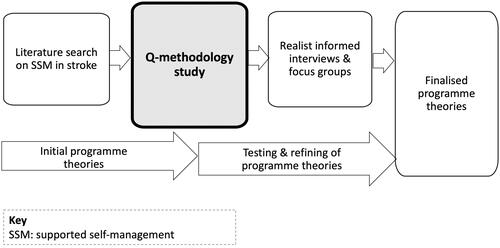
Realist evaluation is a form of theory-driven evaluation that aims to derive a deeper understanding of how, why, and for whom interventions or programmes work [Citation20–22]. In a realist evaluation, programme theories, or hypotheses, are developed about how interventions or programmes are proposed to work which are then empirically tested (confirmed, refuted) and refined using the best available evidence [Citation23]. Since the concept of SSM in stroke is still largely ill-defined, a Q-methodology was seen as a valuable approach in the early phases of the realist evaluation study to offer insights into what was important in relation to SSM and to help develop and prioritise the range of ideas underpinning the programme theories, about how SSM works. demonstrates how the Q-methodology was embedded into the larger realist evaluation study [Citation19].
Figure 1. Q methodology study informing programme theory development and testing within the IMPETUS realist evaluation.
Study design
Q methodology is a mixed method approach that combines qualitative and quantitative techniques to study subjective opinions or beliefs [Citation24]. Q methodology allows us to identify and describe the shared viewpoints that exist on a topic, revealing areas of consensus and disagreement; in this case, the topic is SSM after stroke. Q methodology has been described in detail elsewhere [Citation24,Citation25] but the main stages in the design of this Q study are described here. A Q study is characterised by two key stages (1) data collection in a Q sort which involves the rank ordering of a set of statements called a Q set and (2) factor analysis to identify patterns of similarity between Q sorts [Citation24,Citation25].
Data collection
Q set statement development
The Q set was generated from the literature and expert opinion that informed the overarching realist evaluation’s initial programme theories about how SSM may work; 32 statements were included in the final Q set ensuring coverage and balance across all initial programme theories. The Q sort was piloted by the project research, and patient and public involvement teams with no changes needed. The final Q set of statements is presented in .
Table 1. Q set and factor scores.
Participants
Four research sites were purposively selected to include sites with different organisational structures and service delivery models for SSM in stroke. The four sites each covered different geographical areas of Scotland including remote and rural, and metropolitan communities with caseloads offering a range of sociodemographic backgrounds. At each site participants were identified and first approached by a local collaborator (a stroke clinician or service/clinical network manager based on each site) based on the following criteria:
adult stroke survivors six months or longer post-stroke who had been offered, received, or engaged with SSM services.
clinicians of any multidisciplinary profession who were involved in the delivery or provision of community-based SSM services for stroke.
managers or clinical team leads who had strategic responsibility for the organisation and delivery of community-based rehabilitation services including stroke in one of the cases study sites.
Participants were issued with an information sheet and a verbal explanation which included information about the research, including how we defined supported self-management. Potential participants submitted an expression of interest by mail, email, or telephone to one author (JDM) and were then screened to ensure they could provide informed consent and that they met the inclusion criteria. Eligible participants were then consented to inclusion and data collection was undertaken by one author (JDM), a physiotherapist with 10 years’ clinical and 8 years of research experience with stroke survivors. Participants were purposively sampled to seek differing views and experiences of SSM following stroke; the aim was to identify 12 participants in each study site (n = 48). Sample sizes were appropriate to the design of the study since in both realist and Q-methodology studies sample selection does not aim to achieve representativeness or saturation but aims to cover a range of views and contexts that might be relevant to the topic and the programme theories within the study [Citation26–28]. The sample sizes in the current study were informed by the numbers of potentially eligible stroke survivors in each case study site, the number of clinicians and managers working in community teams at each site, and the timelines for completion of the project.
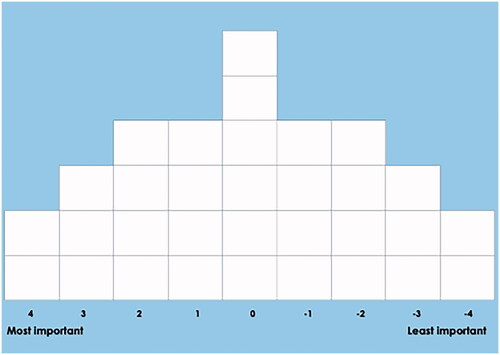
Q sort
The Q-methodology study was undertaken before the Covid-19 pandemic. The Q sorts were administered in a face-to-face interview for stroke survivors and managers, and a focus group for clinicians. Written informed consent was obtained before starting. Basic demographic data were collected: for stroke survivors this was age, sex, time since stroke, level of stroke disability using the modified Rankin Scale (mRS), cognition using short form Montreal Cognitive Assessment (MoCA), and language impairment using the National Institutes of Health Stroke Scale (NIHSS) language section; for clinicians, this was team setting, length of time working in community and work with stroke survivors; and for managers, this was the length of time managing community teams and types of teams. To ensure participants had a good understanding of the topic, before the Q sort, participants were given a brief explanation about supported self-management and the research aims. Participants were then issued with a showcard to refer back to throughout the session. The showcard contained a description of supported self-management, the brief aims of the research, and the Q questions. In the Q sort, participants were asked “What is most important to making SSM work from your perspective?” Participants were then given the pack of 32 Q set statement cards to read and were asked to sort each of the cards into one of three initial piles: “most important,” “important,” “least important.” The participant was then guided to refine these initial piles and rank order each statement onto the Q-grid (see ) from “most important” (+4 on the grid) to “least important” (−4 on the grid). Following the completion of the Q sort, the participant was asked open-ended questions about the statements placed in the +4 and −4 positions on the grid; for interview participants (stroke survivors and managers) this was asked verbally, and for focus group participants (clinicians) this was asked on paper since participants completed the Q sort at different times. All participants were asked “Is there anything else that you want to tell me about any of the statements in relation to what is important to making SSM work for you?” on the grid as well as general questions about the overall Q sort. These interviews were audio recorded to assist in the analysis. Field notes were taken and referred to during analysis if needed.
Data analysis
The Q sort data was entered into PQMethod [Citation29] and the data files were imported into KenQ [Citation30] for factor analysis. In the case of Q methodology, factor analysis uses the correlation matrix and, through the factor extraction and rotation process, determines from it how many basically different ways the Q statements are organised and thus how many different composite Q sorts (factors) there are [Citation31]. Factors are essentially a Q sort (known as a factor array) which best represents the configuration of a Q statement by participants who have created very similar Q sorts [Citation32]. This factor array is determined based on factor scores which are an average of the scores (i.e., +4 to −4) given to a statement by all of the Q sorts which are highly correlated with factor. These scores are then weighted to reflect that some Q sorts are more highly associated with a factor than others [Citation31].
There are several factor extraction and rotation techniques that exist, but in Q methodology it is typical to use centroid factor analysis followed by varimax rotation, and this process was performed for this study, further details on factor analysis methods in Q methodology can be found in Watts and Stenner [Citation32]. Factors were retained for interpretation and examination considering Eigen values, explained variance and the number of participants with significant factor loadings for each factor as well as the post Q sort qualitative comments. Interpretation of the factors was holistic, looking at the placement of each statement in relation to each other to identify and describe a coherent narrative for each factor. Attention was given to statements in the outer tails of the grid which are most salient to participants as well as distinguishing statements, which are those with a significantly (p < 0.01) different position in the composite Q sort of a factor as compared to the other factors.
Research ethics
Ethical approval was obtained by the East of Scotland Research Ethics Committee 19/ES/0055.
Results
Characteristics of participants
A total of 48 Q sorts were completed. This comprised n = 20 stroke survivors, n = 20 clinicians (across four focus groups), and n = 8 managers. Stroke survivors recruited to the study had a median age of 65.6 years (range 34–82 years), n = 7 were women (35%), median time post-stroke was 18 months (interquartile range {IQR} 1–3.5 years), median mRS of 3 (IQR 2–3, range 1–4), median NIHSS language score of 0 (IQR 0–1, range 0–2) and short form MoCA of 12 (IQR12–14, range 8–14). Twenty clinicians were recruited to the study and comprised the following clinical backgrounds: n = 6 physiotherapists; n = 6 occupational therapists; n = 3 nurses; n = 3 speech and language therapists; n = 2 clinical psychologists. Clinicians had a median of 16.5 years’ experience in stroke (IQR 14.5–22.8 years) and 12 median years’ experience working in a community setting (IQR 8–15.1 years) including stroke specific early supported discharge, stroke-specific community rehabilitation, generic community rehabilitation and other domiciliary settings. Managers had a median of 13.5 years in the management of community rehabilitation teams (IQR 9–18.5 years).
Participants experienced a range of different supported self-management strategies. Stroke survivors had attended, declined, or dropped out of formal self-management peer support programmes or rehabilitation programmes or had no experience of formal programmes for self-management and instead worked with clinicians to self-manage following stroke; clinicians had the experience of providing one to one self-management support with stroke survivors during clinical interactions, and others were involved in setting up and running peer support and rehabilitation programmes for stroke survivors.
Factor analysis
A range of factor solutions was examined. A four-factor solution was selected as it had a clearly interpretable account. The four factors explained 46% of the total variance. shows the positioning of each statement in each of the four factors (pictorial representations of each factor are given in Supplementary Material 1). Factors 1–4 were defined by 13, 5, 3, and 11 participants, respectively, see for details (the footnote to the table provides an explanation of the rules for a defining sort in this study). The remaining sorts did not define a factor, with either low loading across all factors or have similar loading across more than one factor (for example NC2 is a “mixed loader” with similar scores on F1 and F2).
Table 2. Respondents' stakeholder group and factor association.
Four distinct viewpoints about SSM were identified: (i) A person-centred approach to build self-confidence and self-worth; (ii) Feeling heard, understood, and supported by everybody; (iii) Training, preparation, and appropriate resources; and (iv) Right thing, right place, right time for the individual.
Each factor is described in more detail in the next four subsections. In each factor, description # indicates the statement number and is followed by the position of the statement within the factor. For example, (#1, +4) would indicate that statement 1 was placed in position +4 for that factor. Quotes from participants are included in the factor descriptions in italics.
Factor 1: a person-centred approach to build self-confidence and self-worth
Factor 1 is an account that emphasises the importance of a person-centred approach, focusing on stroke survivors' needs and meaningful goals (#9, +4). This person-centred approach includes all those working with the stroke survivor, such as clinicians, community and third sector groups, and in some cases, family members. This approach focusses specifically on developing stroke survivor’s skills and confidence in their abilities to self-manage, build hope, and restore a sense of self-worth (#32, +4; #16, +3; #4, +2).
In addition, it also emphasises the importance of reflecting on what works well and what does not with regards to SSM, sharing and learning about SSM from each other, and seeing how others in the same boat are doing in their recovery (#1, +2; #13, +1; #20, 0). In factor one, being listened to and feeling understood is an important element of a trusting, supportive relationship (#24, +3; #7, +2; #11, +1). Respondents who align with this factor strongly believe that stroke survivors should have more power and control of decision-making than professionals (#3, −2; #6, −1; #1, −4). It was also important to tailor support to the individual, as well as support to manage the emotional over the physical impact of stroke (22, +2; #10, +3; #5, −1) as illustrated here:
“…in my eyes stroke was physical but [the] emotional side affected me more than physical’ (stroke survivor).
There were also some items rated of lower importance to respondents in this factor including online support (#12, −4) since stroke survivors either reported that they had no pre-stroke online experience, or had difficulty accessing online support because of their stroke impairment(s). Some respondents also commented that they preferred human contact to check that they were being understood due to fear of misinterpretation online:
“one of the things I’m struggling with doing is things I could do normally [before stroke]. Online like typing wrong things, better to talk to someone rather than online – because [I am] brain damaged, in the way it’s damaged I get confused.” (stroke survivor).
Respondents in this factor gave lower priority to the need for additional resources, such as training or additional support from local or community organisations to make SSM work (#27, −1; #8, −2; #14, −2), as summarised in this quote:
“We’ve done this [developed SSM in service] in [site] with no additional resources – reworked the way the team deliver the care they deliver, reduce home visits especially while attending SSM course; no extra staff and allow people to self-refer back into the service” (manager).
Factor 2: feeling heard, understood, and supported by everybody
Factor 2 is an account that emphasises the importance of listening to the stroke survivor and the provision of support that offers a sense of feeling cared for and supported (#19, +4; #24, +4). Here, support is seen as coming from a wide network including spouse, family, friends, health care professionals, and local community organisations (#26, +2; #8, +2):
“…my husband is not one for saying ‘I’ll do everything for you’ but he’ll support if needed” (stroke survivor).
The emotional and physical impacts of stroke are considered equally important in factor two as is the importance of understanding the needs of the person to know what and how to target support (#5, #7,#10, all +3). Factor 2 also emphasised the importance of a holistic approach to the provision of SSM because respondents perceived that SSM should address multiple health problems alongside the impact of the person’s stroke (#2, +1).
Respondents in factor 2 perceived that when working with clinicians, power and decision-making should be shared equally between clinicians and stroke survivors (#3, +1). Respondents in this factor reported that it was important that stroke survivors had the freedom and flexibility to decide what works best for them (#28, +2) but that there were also times when it was suitable and appropriate for professionals to decide what is best (#21, −2) in the context of a trusting, supportive relationship (#11, 0):
[in relation to professionals decide] “A wee bit maybe but it’s up to the person and what they think is best for them – it’s going back to being listened to and if I can’t communicate and professionals deciding won’t necessarily be the right thing” (Stroke survivor).
Goals and hope were viewed as less important in this factor than in the other three factors (#9, 0; #4, −4). Elements of SSM that involved reflection were rated as less important in this factor: seeing how others in the same boat are doing; sharing and learning about SSM from each other, and having a safe space to learn and practice what works and does not work in relation to self-management (#1, −3; #15, −2; #13, −2; #20, −1). Like the other factors, online support was viewed as least important (#12, −4) either because stroke survivors did not use online pre-stroke, preferred human contact, or don’t see the merit as it represents their pre-stroke role, as indicated in the following quote:
“When I was at work I needed online but now I don’t give a toss, it’s irrelevant – don’t have the interest” (stroke survivor).
Factor 3: preparation, appropriate resources, and training
Factor 3 is an account that emphasises the importance of embedding and delivering SSM within routine stroke care (#29, +4) and the requirements for making this happen. Respondents prioritised the need for service-wide scaffolding of practical resources to be in place, such as dedicated time, preparation, and training for self-management (#14, +3; #17, +3; #27, +2) as illustrated here:
“Staff are time limited – need best resources and professional [sic] adept at supporting patients with self-management” (manager).
Provision of support for self-management from a wide range of local and community organisations is also seen as important for successful SSM (#8, +4). Respondents in factor 3 felt it was important that power for decision-making around SSM is shared equally between stroke survivors and clinicians (#3, +2). Reflection for both stroke survivors and clinicians on what does and does not work well was also important as was a safe space to learn and practice self-management strategies; both of which were ranked higher in this factor than in others (#1, +3; #15, +1). One of the comments from a respondent in this factor summarises why a safe space to connect and share experiences, and to learn with and from each other is so important for making community-based SSM work:
“…in community, staff can feel isolated – staff get together and if something going well share it – all the same problems come out and it’s reassuring and gives a boost – allow staff time together to see how to do things differently- consistency across health board regardless of what teams they are in” (manager).
Compared to the other factors, respondents in factor three placed more importance on the need for a leader or a champion (#25, 0) who could provide direction, advice, and support to practitioners, as illustrated here:
“…having someone that can pick up the phone and ask advice from (staff) and someone that’s enthusiastic – don’t like change in NHS as it can be difficult, and leaders can help” (manager).
Interestingly, online provision of SSM was seen as more important in factor three than in other factors (#12, −1). It is also seen as less important for stroke survivors to have flexibility and freedom to decide what works best for them (#28, −3), but also less important that professionals are in charge of deciding what’s right for people and their self-management (#21, −4) or for everyone to have a clear role in SSM (#23, −4;). In comparison to the other three factors, the following statements were ranked lower in factor three: being listened to (#24, 0); understanding the person (#7,-1); and SSM being valued and understood by everyone (#30, −3).
Factor 4: right thing, right place, right time for the individual
Factor four is an account that emphasises the importance of timing in providing the right kind of support when stroke survivors need it (#18, +4). Respondents highlighted the importance of understanding the needs of the individual so that support can be tailored accordingly (#7, +3; #22, +3):
“Clinicians tend to lose sight that it’s an individual; different humans have different requirements – tailor [input] and supplier and receiver are happy it’s bespoke” (clinician).
Adequate training for professionals to deliver SSM is viewed as particularly important (#27, +4) for successful SSM, as is the view that SSM should be valued and understood by everyone (#30, +3). Respondents also perceive that a focus on personally meaningful goals and building self-worth, self-belief, and confidence in stroke survivors’ abilities to self-manage is also important (#9, +2; #16, +2; #32, +1). Personally meaningful goals are seen to foster engagement in person-centred self-management:
“…person more likely to engage if the service provided is meaningful” (clinician).
In relation to the statements viewed as less important, respondents in this factor perceived that seeing how others in the same boat are doing with their self-management was less important than in the other three factors (#20, −3). Similar to factors 1 and 2, online support was less important (#12, −4) because it was perceived it was not tailored, or lack of computer literacy pre-stroke, or because stroke survivors feared being misunderstood if there was no face to face interaction, as illustrated in this quote:
“[online support not suitable because]…personally I like to know that I’m being understood” (stroke survivor).
Discussion
Our findings highlight that there are different interpretations of what is important for successful SSM in stroke. By unearthing the hidden viewpoints about the nuance of how SSM is understood we present some insight into what is required for successful SSM and how SSM might best be implemented in practice.
Participants loading onto factors 1 and 2 prioritised the person-centred elements of SSM, such as building confidence and self-worth, as well as understanding, listening to, and helping stroke survivors feel supported and cared for as the important aspects of successful SSM. In contrast, participants loading onto factor 3 prioritised having the necessary resources and infrastructure in place to deliver tailored self-management support; strategies, such as having adequate dedicated time, preparation, resources, and training were perceived as essential for successful SSM. The role of a leader or champion, in addition to resources for self-management, was viewed as particularly important in factor 3. Our findings suggest that participants prioritising statements around resources, such as training may have felt either less confident, or more constrained, to access or deliver self-management support due to the absence of local strategic, organisational investment, and support. Not all participants in resource restrained contexts necessarily loaded onto factor 3 nor are these findings generalisable to all people working in resource restrained areas. However, these findings highlight that people’s priorities and perspectives may be influenced by the contexts in which they access or deliver SSM, providing a valuable direction for further research and the development of context-specific guidance for implementing SSM in practice. Factor 4 straddled the priorities of all other factors, identifying the important elements in factors 1, 2, and 3 that need to be appropriately timed to make SSM work.
Despite the different views identified in this study, there were elements important to the success of SSM for all respondents: a trusting supportive relationship, working in partnership, sharing power and decision making for SSM, a focus on meaningful goals, and support that builds stroke survivors’ sense of self-worth and confidence in their own abilities. Self-confidence and self-worth are central aspects of successful SSM in stroke and their importance in this study was expected given the existing evidence of the link of self-efficacy as a mediator or outcome to successful SSM [Citation9]. Our findings expand on Bright and Reeves [Citation33] meta-synthesis that explored communication and therapeutic relationships in stroke survivors with aphasia; they found that the relationship between clinicians and stroke survivors is the key part of rehabilitation. A trusting supportive relationship where stroke survivors’ needs are understood can foster hope, relieve emotional distress, and improve satisfaction with services, ultimately helping to support the reconstruction of life after stroke [Citation33]. This emphasis on person-centredness resonates with contemporary notions that SSM is a relationship-based approach, characterised by mutual respect for each other’s knowledge, experience, and capabilities [Citation34,Citation35], rather than simply compliance with professional advice [Citation16]. This Q study found a partnership approach was important, where collaboration enables stroke survivors and clinicians to co-create self-management plans and goals that align with stroke survivors’ priorities [Citation34,Citation35]. Thus, developing a trusting supportive relationship between stroke survivors and clinicians builds the foundation for successful SSM.
Of note, online support was consistently low ranking across factors with respondents often indicating access or communication issues could prevent them from engaging in online forms of SSM. Many also commented that they preferred the human contact of face-to-face interactions. The study was conducted before the COVID-19 pandemic and an increase in the use of remote consultations [Citation36] may have shifted perceptions on its role in SSM. The role of online support for self-management in stroke would make an interesting topic for future research as technology-enabled support and rehabilitation take on greater prominence in our post-Covid world. Research on how trusting and supportive relationships for SSM can be developed, enhanced, and sustained in this new environment will also be important.
The factors in this study each have a subtle emphasis on different components of SSM which highlights how its delivery could be framed to best support the stroke survivor and their needs. Indeed, members of the same clinical team and managers may have differing viewpoints about SSM, and our findings indicate that teams should consider these viewpoints when they develop their SSM practice; individuals should be aware of their own viewpoints and consider others’ perspectives when working to support self-management. For example, exploring how respondents may approach a strategy, such as a goal setting, for people sharing the views expressed in factor one, SSM might involve working together to break down larger, aspirational goals into more achievable, smaller goals. Attempting and achieving smaller goals while working towards larger aspirations helps build self-confidence and self-worth [Citation37], while aspirations help maintain hope for the future [Citation38]. For people sharing the views expressed in factor two, the process of goal setting can open up a conversation about what matters most to the stroke survivor which would help clinicians to understand the individual stroke survivor, demonstrate their support for the stroke survivor as they work towards their goals, and share decision making and action planning with the stroke survivor. For those sharing views in factor three, clinicians may need time to train and prepare themselves for delivering SSM and for engaging in meaningful conversations with stroke survivors around their goals. For people sharing the views expressed in factor four, the conversation to set goals may provide an understanding of the person and their needs to help to tailor appropriate and timely support. This finding corroborates existing research highlighting the importance of listening to stroke survivors, understanding the context of the person and their lives, and encouraging them to think about their own priorities, using these personal priorities to ground the provision of SSM [Citation10,39].
As part of our overall study design, the Q-study was helpful for informing the next stage of programme theory development around how SSM works and why. Realist evaluation approaches explore the influence of context on mechanisms of action. This Q-study helped to offer a sense of the potential mechanisms by which SSM works, as well as suggestions for possible contexts that may influence how successful SSM can become embedded in routine stroke care. For example, the views represented in factor three suggest that in resource-stretched settings where SSM is neither understood nor valued, then clinicians may prioritise the elements that will support them to first develop an understanding of what SSM is and how it can be delivered. This includes training and preparation for delivering SSM but also dedicated time to learn about, share and practice strategies for delivering SSM. Our findings suggest that successful implementation of SSM in practice may differ depending on the context in which community stroke teams work, in turn influencing how staff learns and gain confidence to embed SSM in practice. Further research is needed to understand how context influences SSM in practice. Programme theories, informed by the Q-study, that identify different context-mechanism-outcome configurations on how SSM works and why will be fully explored and tested in the subsequent phases of the realist evaluation study [Citation19].
There are some limitations of this study. We conducted the Q study in a population from Scotland, UK and thus, although offering some valuable insights, the findings are set in the context of Scotland. Secondly, the study was undertaken before the Covid-19 pandemic. The changing landscape resulting from the pandemic has implications for the structure and delivery of community stroke rehabilitation. As such, the way stroke survivors, clinicians, and managers would prioritise the statements from the Q study may differ if repeated post-pandemic. This limitation could not be predicted and mitigated but provides an interesting context for the study. Finally, the stroke survivors involved in this study were from an older age group (median age of 65.6 years old) although an effort was made to recruit a variety of ages with participants ranging from the youngest at 34 years old, this could mean that views of younger stroke survivors may be different. This provides an opportunity for future research to explore the varying viewpoints of stroke survivors of different ages and backgrounds.
In conclusion, our study identified four different viewpoints, as well as key shared elements, on what is most important in supporting self-management after stroke from the perspective of stroke survivors, community stroke clinicians, and managers in four Scottish health boards. By describing and exploring these viewpoints our study affords clinicians and managers the opportunity to reflect on their own viewpoints and how others in their teams, and the stroke survivors that they work with, might see SSM differently. The findings could be used to inform more targeted quality improvement strategies to support the delivery of consistent and sustainable SSM that considers the preferences of stroke survivors and their families/friends. Having an awareness of these viewpoints offers an opportunity to appreciate where others are coming from and thus a potential to improve how clinicians work together and support stroke survivors to self-manage effectively. Our findings suggest that different things are needed at different times during the stroke survivor-clinician interaction, as well as from the team and health board context to make SSM work effectively. More research is needed to understand what makes SSM work for whom and why to guide clinicians about how best to work with stroke survivors to support their self-management to live a fulfilled life after stroke.
Supplementary_material.docx
Download MS Word (1.6 MB)Acknowledgements
We wish to acknowledge and thank our Patient and Public Involvement group members: Ms. Betty Gilmour; Mr. Colin Fraser; Ms. Pat Mooty; and Ms. Audrey Taggart for their help with the design, piloting, and reporting of the Q study. Thanks to Ms. Brenda Bain, Prof. Mark Barber, and Mr. Mark Smith for their help in piloting the Q sort. We also wish to thank our project team members: Dr. Rebecca Fisher; Dr. Katie Gallacher; Prof. Fiona Jones; Dr. Terry Quinn; Prof. Mark Barber; Mr. Mark Smith; Ms. Katrina Brennan; and Ms. Therese Lebedis for contributing to the design and conduct of the IMPETUS project and for commenting on the factor arrays and statements in the Q sort. Thanks to our advisory group members: Ms. Anne Armstrong; Prof. Jo Booth; Prof. Audrey Bowen; Mr. Phil Colis; Ms. Sara Redmond; and Prof. Frederike van Wijck (Chair) for their support and advice throughout the conduct of the IMPETUS study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Consent was not obtained to share anonymised data for this project.
Additional information
Funding
References
- Stroke Association. Stroke recoveries at risk. London: Stroke Association; 2021.
- Global Burden of Disease 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18:459–480.
- The Stroke Association. State of the nation. London: Stroke Association; 2018.
- Gallacher KI, Batty GD, McLean G, et al. Stroke, multimorbidity and polypharmacy in a nationally representative sample of 1,424,378 patients in Scotland: implications for treatment burden. BMC Med. 2014;12(1):151.
- Averbe L, Avis S, Chrichton S, et al. The long-term outcomes of depression up to 10 years after stroke; the South London stroke register. J Neurol Neurosurg Psychiatry. 2014;85:514–521.
- Rudd AG, Bowen A, Young G, et al. National clinical guideline for stroke. London: Royal College of Physicians; 2017.
- Scottish Government. Scottish stroke improvement plan. Edinburgh: Scottish Government; 2014.
- World Health Organisation. Rehabilitation competency framework. Geneva: World Health Organisation; 2020.
- Lennon S, McKenna S, Jones F. Self-management programmes for people post stroke: a systematic review. Clin Rehabil. 2013;27(10):867–878.
- Fu V, Weatherall M, McPherson K, et al. Taking charge after stroke: a randomized controlled trial of a person-centered, self-directed rehabilitation intervention. Int J Stroke. 2020;15(9):954–964.
- Fryer CE, Luker JA, McDonnell MN, et al. Self-management programmes for quality of life in people with stroke. Cochrane Database Syst Rev. 2016;2016(8):CD010442.
- NHS National Services Scotland. Scottish stroke improvement programme report. Edinburgh: NHS; 2016.
- Gallacher K, Morrison D, Jani B, et al. Uncovering treatment burden as a key concept for stroke care: a systematic review of qualitative research. PLOS Med. 2013;10(6):e1001473.
- Gallacher KI, May CR, Langhorne P, et al. A conceptual model of treatment burden and patient capacity in stroke. BMC Fam Pract. 2018;19(1):9.
- Morgan HM, Entwistle VA, Cribb A, et al. We need to talk about purpose: a critical interpretive synthesis of health and social care professionals' approaches to self-management support for people with long-term conditions. Health Expect. 2017;20(2):243–259.
- Kidd L, Booth J, Lawrence M, et al. Implementing supported self-management in community based stroke care: a secondary analysis of nurses’ perspectives. JCM. 2020;9(4):e985.
- Kidd L, Lawrence M, Booth J, et al. Development and evaluation of a nurse-led, tailored stroke self-management intervention. BMC Health Serv Res. 2015;15:359.
- Hancock N, Houghton J. People 1st: bridges training and improvement programme executive summary. UK: University of East Anglia; 2020. Available from: https://www.hee.nhs.uk/sites/default/files/documents/People%201st%20executive%20summary_0.pdf
- Kidd L, Duncan Millar J, Mason H, et al. Supported self-management in community stroke rehabilitation: what is it and how does it work? A protocol for a realist evaluation study. BMJ Open. 12(1):e055491.
- Pawson R, Tilley Pawson R, Tilley N. Realistic evaluation. UK: SAGE Publications; 1997.
- Wong G, Westhorp G, Manzano A, et al. RAMESES II reporting standards for realist evaluations. BMC Med. 2016;14(1):96.
- Westhorp G. Realist impact evaluation: an introduction. London: Overseas Development Institute; 2014.
- Greenhalgh J, Pawson R, Wright J, et al. Functionality and feedback: a protocol for a realist synthesis of the collation, interpretation and utilisation of PROMs data to improve patient care. BMJ Open. 2014;4(7):e005601.
- Watts S, Stenner P. Doing Q methodological research: theory, method and interpretation. London: Sage; 2012.
- Brown S. Political subjectivity: applications of Q methodology in political science. New Haven (CT): Yale University Press; 1980.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation. 2016;22(3):342–360.
- Baker R, Thompson C, Mannion R. Q methodology in health economics. J Health Serv Res Policy. 2006;11(1):38–45.
- Emmel N. Sampling and choosing cases in qualitative research: a realist approach. London: Sage; 2013.
- PQMETHOD [Internet]. Munich; Peter Schmolck; 2021 [cited 2021 Nov]. Available from: http://schmolck.org/qmethod/
- Banasick S. Ken-Q analysis (version 1.0.6) [Software]. Available from: https://shawnbanasick.github.io/ken-q-analysis/
- Brown SR. A primer on Q methodology. Oper Subject. 1993;16:91–138.
- Watts S, Stenner P. Doing Q methodology: theory method and interpretation. Qual Res Psychol. 2005;2(1):67–69.
- Bright FAS, Reeves B. Creating therapeutic relationships through communication: a qualitative metasynthesis from the perspectives of people with communication impairment after stroke. Disabil Rehabil. 2020. DOI:10.1080/09638288.2020.1849419.
- Tomaselli G, Buttigieg SC, Rosano A, et al. Person-centered care from a relational ethics perspective for the delivery of high quality and safe healthcare: a scoping review. Front Public Health. 2020;8:44.
- Jones F, Gage H, Drummond A, et al. Feasibility study of an integrated stroke self-management programme: a cluster-randomised controlled trial. BMJ Open. 2016;6(1):e008900.
- Wherton J, Greenhalgh T, Shaw S. Expanding video consultation services at pace and scale in Scotland during the COVID-19 pandemic: national mixed methods case study. J Med Internet Res. 2021;23(10):e31374.
- Levack WMM, Dean SG, Siegert RJ, et al. Navigating patient-centered goal setting in inpatient stroke rehabilitation: how clinicians control the process to meet perceived professional responsibilities. Patient Educ Couns. 2011;85(2):206–213.
- Scobbie L, Brady MC, Duncan EAS, et al. Goal attainment, adjustment and disengagement in the first year after stroke: a qualitative study. Neuropsychol Rehabil. 2021;31(5):691–709.
- Jones F, McKevitt C, Riazi A, et al. How is rehabilitation with and without an integrated self-management approach perceived by UK community-dwelling stroke survivors? A qualitative process evaluation to explore implementation and contextual variations. BMJ Open. 2017;7(4):e014109.