Abstract
Purpose
To ascertain the feasibility and acceptability of delivering a job retention vocational rehabilitation intervention [MSVR] for people with multiple sclerosis (pwMS) in a community setting. Secondary objectives included determining whether MSVR was associated with changes in quality of life, fatigue, mood, cognition, workplace accommodations, work instability, work self-efficacy, and goal attainment.
Methods
Single-centre mixed-methods feasibility case series.
Results
15 pwMS and three employers received 8.36 (SD = 4.48) and 1.94 (SD = 0.38) hours of MSVR respectively over three months. The intervention predominantly addressed managing cognition, fatigue, and negotiating reasonable accommodations. Four healthcare professionals were recruited to clarify clinical information.
The intervention was feasible to deliver, and there was a significant positive impact on goal attainment immediately following MSVR (t(14) = 7.44, p = .0001, d = 1.9), and at months 3 (t(13) = 4.81, p = .0001, d = 1.28), 6 (t(11) = 4.45, p = .001, d = 1.28), and 12 (t(9) = 5.15, p = .001, d = −2.56). There was no impact on quality of life, fatigue, mood, cognition, workplace accommodations, work instability, and work self-efficacy. In post-intervention interviews, participants reported that MSVR was acceptable. Four themes were derived regarding the context, employer engagement, empowerment through knowledge, and intervention components and attributes.
Conclusion
It was feasible and acceptable to deliver MSVR. Participants better understood their MS, became more confident managing problems at work and attained their work-related goals.
People with multiple sclerosis (MS) experience problems at work because of the interaction between symptoms and environmental factors (e.g., co-workers’ attitudes).
Vocational rehabilitation for people with MS and their employers should be tailored in terms of content and intensity.
People with MS can be empowered at work by learning about MS and how their symptoms fluctuate over time.
Understanding legal responsibilities and examples of accommodations at work can be beneficial for employers.
IMPLICATIONS FOR REHABILITATION
Introduction
Multiple sclerosis (MS) affects approximately 700,000 people in Europe and 130,000 people in the United Kingdom (UK) [Citation1,Citation2]. People are usually still employed when they are diagnosed with MS; however, they leave the workforce prematurely [Citation3]. There is extensive evidence that employment is good for physical and mental health, economic reasons, and social status [Citation4].
Current healthcare services for people with MS recommend the need to support the person with MS with employment from the point of diagnosis. However, there is little to no information about the support needed and the attributes for this support.
Vocational rehabilitation (VR) aims to support those with illness or disability at work [Citation5]. VR is considered a quality requirement of the National Service Framework (NSF) for people with long-term health conditions such as MS [Citation6], and an outcome of UK National Health Service interventions (NHS) [Citation7].
To date, there is inconclusive information about the effectiveness of these interventions for people with MS [Citation8]. Few VR interventions for people with MS have been developed, implemented, and evaluated. The most recent interventions have focused on developing job-seeking skills [Citation9] or addressing the impact of cognition at work [Citation10]. Unfortunately, these interventions do not address all factors that affect job retention (e.g., fatigue levels, accessibility issues, etc.).
Previous research exploring the VR needs of people with MS at work suggests that people with MS need holistic support in understanding and managing their condition, support in identifying workplace accommodations and managing employers’ expectations through education [Citation11,Citation12].
Because of the limitations of the previously identified interventions, we developed a job retention VR intervention to support employed people with MS at work based on extensive literature and stakeholder engagement [Citation11,Citation13]. The intervention is called MSVR and is designed to be delivered to both the person with MS and their employer (including line managers, human resources, or occupational health).
This study presents the experiences of delivering MSVR and further insight into what VR for people with MS looks like. This study aimed to understand the feasibility of delivering MSVR and its acceptability for people with MS, employers and healthcare professionals. Secondary objectives explored whether MSVR was associated with changes in outcomes such as fatigue, cognition, work self-efficacy, work instability, and goal attainment for people with MS at four different time points.
Methods
Design and setting
This is a feasibility mixed-methods single-case series study design with an embedded qualitative study. Participants with MS and employers were involved in a three-month intervention and an interview three months post-intervention. The participants with MS were also asked to complete a questionnaire at the end of the intervention, and at 3-,6-, and 12 months post-intervention.
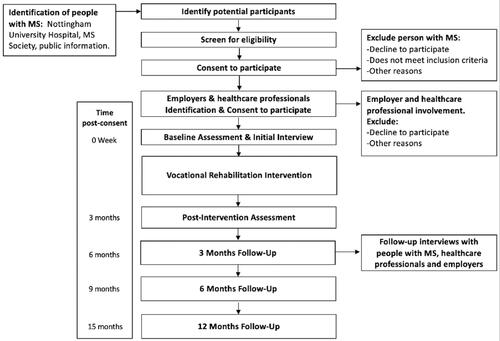
Healthcare professionals were recruited to understand the clinical characteristics of the participants with MS and to request additional support for people with MS if needed. They completed the initial interview and an interview at 3-months post-intervention to explore the acceptability of the intervention and barriers to participating in the support. presents the study participants’ pathway.
Figure 1. Participant’s recruitment pathway.
Eligibility and recruitment
Participants were recruited over five months and received the intervention remotely. The inclusion criteria for participants with MS were: diagnosis of MS, aged between 18–65 years, currently employed, can give informed consent, and can communicate in English. The only exclusion criterion was: planning to retire due to age or take early retirement within the next six months. Employers and healthcare professionals were recruited if they: consented to participate in the study, and were over the age of 18 years. There were no exclusion criteria for employers and healthcare professionals.
We recruited participants with MS from three sources: The MS Clinic at Nottingham University Hospitals (NUH) NHS Trust, local charities working with people with MS (e.g., UK MS Society), and publicly available information on social media (e.g., Twitter). Once a participant with MS was recruited, the assistant psychologist (BDP) informed the participant of the possibility of including their employer/line manager in the intervention. Those participants with MS interested in involving their employer were provided with a Participant Information Sheet (PIS) to share with their employer. Employers were only contacted by their employees or assistant psychologist if the employee agreed to employer involvement in the intervention. Participants were also asked if they wanted to designate a healthcare professional involved in their usual MS care to gather further information about the characteristics of their MS and further support if needed. Agreeing to include an employer or healthcare professional in the intervention was not an inclusion criterion for the participant with MS.
This study was granted ethical approval by the Division of Psychiatry and Applied Psychology at the University of Nottingham, reference number 1582 (April 2019). Ethical approval was also granted by the NRES Committee East Midlands Nottingham 2, reference number 20/EM/0113, and the Research and Development (R&D) department of NUH NHS Trust. All participants completed a consent form before data collection.
Intervention description
MSVR aims to support people with MS to remain at work by providing support both in managing MS symptoms and reducing environmental barriers [Citation13]. MSVR was underpinned by a biopsychosocial approach that takes into account the chronic and progressive character of MS and environmental factors [Citation14], paradigms of work disability prevention [Citation15], and anti-discrimination legislation (e.g., UK Equality Act 2010) [Citation16] to ensure the person with MS is adequately supported in the workplace. The full description of the intervention following the template for intervention description and replication (TIDieR) [Citation17] is presented in Supplementary Material A.
The first step of the intervention consisted of an initial interview (i.e., a workability assessment). The aim was to understand the demographic, clinical and professional characteristics of the person with MS, barriers to job retention, and set intervention work-related goals.
Participants then received up to 10 h of individually tailored VR in 1:1 meetings over three months with the assistant psychologist. The intervention was tailored for each participant from a menu of components presented in .
Table 1. Menu of intervention components.
Participants with MS had the opportunity to include their employer in the intervention. The employers’ intervention involved an initial interview to understand their role and experience in supporting the person with MS at work and up to 4 h of support addressing topics such as understanding MS, legal responsibilities, and identifying reasonable accommodations.
The intervention was delivered by an assistant psychologist (BDP) with experience working with people with MS, who was involved in the intervention development. The assistant psychologist received mentoring from an Occupational Therapist with extensive experience in delivering VR to people with long-term neurological conditions.
The intervention was designed to be delivered in person or remotely according to the preference and availability of the participant.
To record the support provided to each participant, we adapted a proforma previously used to measure the delivery of VR interventions for people with stroke and traumatic brain injury [Citation18,Citation19]. The proforma allowed recording of intervention intensity and components delivered. The proforma was used to record both face-to-face contact (direct contact) which refers to the topics discussed during each session with the person with MS (or employer); and indirect contact, which includes all the activities conducted outside of the session such as liaison with other professionals and communications. Supplementary material A presents the methods used to measure intervention content.
Feasibility measures
To ascertain the feasibility of delivering MSVR the assistant psychologist recorded on a proforma data regarding:
Feasibility of recruiting participants using the recruitment strategy for the study.
Time to recruit the target sample (15 people with MS, 10 employers, 10 healthcare professionals).
Feasibility of delivering up to 10 hours of MSVR to people with MS and 4 hours for employers.
Practical attrition and dropout reasons (if provided).
Appropriateness of study methods and procedures.
Quantitative measures
The assistant psychologist collected demographic information from the participants during the initial interview. Participants with MS were asked to complete a booklet of questionnaires at baseline, at the end of the intervention, and at 3-,6-, and 12 months post-intervention. The measures collected were (): Perceived difficulties questionnaire (PDQ) [Citation20] to measure the presence of cognitive difficulties; Work Productivity and Activity Impairment Questionnaire [Citation21] to assess the impact of MS at work; MS Work Instability Scale (MS-WIS) [Citation22] to assess levels of work instability; Hospital Anxiety and Depression Scale (HADS) [Citation23] to assess levels of anxiety and depression; Modified Fatigue Impact Scale −5 Items version [Citation24] to assess fatigue levels; EQ-5D (Euro-QOL) [Citation25] to assess health-related quality of life; Work Self-efficacy Scale (WSES) [Citation26] to assess work self-efficacy; Workplace Adjustments questions [Citation27] to measure the work adjustments received; Goal Attainment Scaling [Citation28] to ascertain the level of goal attainment.
Table 2. Summary of assessments and time-points.
Qualitative measures
At three months post-intervention, all the participants included in the study (persons with MS, employers, and healthcare professionals) were invited via email to complete an online semi-structured interview with the assistant psychologist who delivered the intervention. The characteristics of the assistant psychologist are presented in . The assistant psychologist did not know the participants prior to the intervention delivery. The interviews, conducted using a topic guide, focussed on understanding the intervention’s acceptability and potential barriers to future implementation.
Table 3. Interviewer characteristics.
Data analysis
We present descriptive statistics mean and standard deviation (SD) to present the demographic, clinical and employment characteristics of the participants. Quantitative data were analysed using Statistical Package for Social Sciences (SPSS) version 24.0. To compare the performance of the participants as a group at different time points, we conducted paired T-tests and Wilcoxon signed-rank test (for parametric and non-parametric data, respectively).
Interviews were audio-recorded, transcribed verbatim and handled using NVivo v.12. The analysis was informed by the framework method [Citation29]. The framework method involves five steps, which have been summarised in . Topic guides were informed by the Behaviour Change Wheel (BCW) [Citation30], the International Classification of Functioning Disability and Health (ICF) [Citation14], and the Consolidated Framework for Implementation Research (CFIR) [Citation31]. A Patient and Public Involvement (PPI) representative reviewed the topic guides to ensure the questions could capture the experiences of receiving the intervention and were easy to understand. We present the topic guides used and how they map to the theoretical frameworks in Supplementary Material B.
Table 4. Description of framework analysis.
The main domains of the theoretical frameworks were used to inform the coding of the interviews, and the main themes were agreed upon between the study authors through discussion. We used Yardley’s framework about quality of the data collection and analysis [Citation32] to improve the quality of our study. The Consolidated Criteria for Reporting Qualitative Research checklist was used to ensure comprehensive reporting of the interviews study (Supplementary Material C).
Data synthesis
The data from the qualitative and quantitative findings were synthesised following the convergence coding matrix strategy [Citation33]. This method allows for identifying areas of agreement and disagreement between the two types of data.
Results
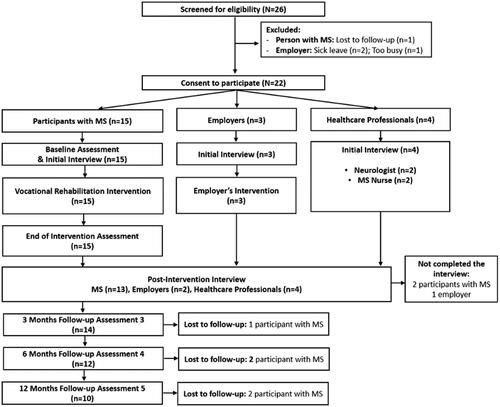
represents the pathway the participants followed through the study. In total, 26 people were screened and 22 consented to participate. The participants with MS were recruited from NHS (n = 3), and self-referral from publicly available information (e.g., social media advertisement) (n = 12).
Figure 2. Screening and recruitment flow.
Participant characteristics
Fifteen participants with MS were included in the study. At the time of recruitment three participants were furloughed as a result of the Covid-19 pandemic. The combined employment and demographic characteristics of the participants with MS are presented in .
Table 5. Demographic and employment characteristics of participants with multiple sclerosis.
The participants with MS were on average aged 46.13 (SD: 9.58) years and were relatively well educated (). They had MS for a mean of 5.87 (4.83) years. Regarding the level of physical disability, their Expanded Disability Severity Score (EDSS) ranged from 0 (no disability) to 7.5 (severe disability), with an average score of 4.57 (2.10).
Three employers (line managers) were included in the study (1 woman, and 2 men). All self-identified as White British and had high educational levels, including degrees (n = 2) and postgraduate qualifications (n = 1). The employers had been supervising the person with MS for a relatively short time, ranging between two months to three years.
Four healthcare professionals (2 women, and 2 men) were included. The healthcare professionals included three neurologists and one MS nurse with an average of 14.25 (6.65) years of experience working with people with MS. The demographic characteristics of the employers and healthcare professionals are presented in .
Table 6. Demographic and employment characteristics employers and healthcare professionals.
Feasibility results
The recruitment methods selected were suitable for the study. However, only 20% (n = 3) and 26% (n = 4) of participants with MS agreed to include their employers and designated healthcare professional in the intervention. The recruitment time had to be extended by two months to reach the recruitment target of participants with MS.
It was feasible to deliver up to 10 h of support for people with MS and 4 for their employers. However, as reported below (MSVR Delivery), not all participants needed all the support. All participants who started the intervention completed it, and there were no dropouts.
The questionnaire return rates for the participants with MS were 100% (n = 15) at post-intervention, 93.33% (n = 14) at three-months, 80% (n = 12) six, and 66.67% (n = 10) at 12 months. Data completeness was excellent (100%); all questionnaires returned were fully completed.
MSVR delivery
The intervention was delivered between June 2020 and January 2021. On average, the participants with MS received 8.36 (4.48) hours of MSVR. The initial interview lasted on average 60 (16.9) minutes, and participants received on average 4.74 h (SD = 2.33) of direct support and 2.61 (2.2) hours of indirect support. Because the intervention was delivered only remotely, no time was spent travelling.
Five participants with MS (33.3%) received more support than that initially proposed (10 h). These participants required lengthier discussions addressing a wider range of topics. The main intervention components addressed and the percentage of the direct time spent addressing these topics are presented in .
Figure 3. MSVR content per component for participants with MS.
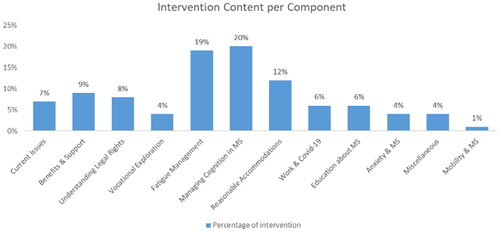
The most common topics addressed for participants with MS were managing cognitive problems, fatigue management, and identifying and requesting reasonable accommodations. To address the needs of the participants recruited, three new intervention components were incorporated into the intervention. These were supported by providing support identifying and requesting benefits (i.e., economic support), information about working during Covid-19, and mobility in MS.
The employers received on average 1.94 (0.38) hours of support. All completed the initial interview plus one intervention session. The employer’s intervention addressed two main concerns: (1) the impact of MS symptoms at work, and (2) how to deal with the impact at the group level of the reduced productivity of an employee with MS.
Quantitative Results
All measures, except for the HADS depression subscale, met the criteria for analysis using a paired t-test. The HADS depression subscale was analysed using the Wilcoxon signed-rank test because the distribution of the difference between the baseline and the following time points was not normally distributed.
There was a significant positive impact on goal attainment immediately following MSVR at 3, 6, and 12 months (). However, there was not a statistically significant difference in the PDQ, MS-WIS, HADS anxiety, EQ-5D-5L, WSES, and MFIS-5 at any time point (). The Wilcoxon signed-rank test showed no significant difference in the HADS depression scores at post-intervention (Z = −158, p < 0.874, r = 0.04), three (Z = −224, p < 0.823, r = 0.06), six (Z = −1.65, p < 0.098, r = .47), and 12 (Z = 1.42, p < 0.153, r = 0.44) months.
Table 7. Paired T-Test quantitative measures.
Qualitative results
The interviews lasted for 37 min on average (SD = 16.26). Two participants with MS and one employer were lost to follow-up and therefore, did not participate in the interview. The demographic characteristics of the participants who completed the interviews are presented in (employers and healthcare professionals) and (participants with MS).
Table 8. Summary of demographic characteristics of interview participants.
The themes identified in the post-intervention interviews were categorised as barriers and facilitators to the acceptability of the intervention (see coding Tree in ). Four main themes were drawn: (1) context, (2) employer engagement, (3) empowerment through knowledge, and (4) intervention components and attributes.
Table 9. Interviews coding tree.
Context
Most participants with MS did not understand what impact MS can have in the workplace or how to manage the impact of their MS symptoms. The content and structure of MSVR were seen as acceptable by the participants. One participant felt the need to have meetings in person:
If you are struggling emotionally, it would be good to have that human contact. (MS_09)
Interviewer: Was there anything that did not work well with you?
Participant: Covid-19…haha that is all I can say, Covid-19 got in the way. I mean because it stopped the participation of the intervention with the school; the only thing I can say that got in the way, nothing else did. Environmental surroundings did. (MS_04)
Before [the intervention] I used to sit for hours and just be there. Now I pace myself, you taught me that and I do feel better. (MS_12)
As doctors, I think it would be very tricky for us to also have that expertise, and be confident enough to deliver those interventions, when it is outside our area of expertise. (HCP_03)
I mean I don’t work full-time so that made it [participate in the intervention] easier. It might be a little bit more difficult for somebody who works 5–9 Monday to Friday. (MS_08)
Employer engagement
The most common issues at work usually arose from difficulties managing relationships with the employer. Thus, there were mixed views about whether to include the employer in the intervention:
I was a bit concerned in the early stages about including my employer. Because I feel like I have a supportive employer anyway, I kind of felt that it might be a little bit of a slur on them, that I wanted them included on it. (MS_10)
At the start [of the intervention] it needs to be only the person [with MS] and the person [therapist] doing the intervention so that you get to know the person and issues before the employer pops in. (MS_08)
I think it’s been very insightful. I think that the explanation that you [assistant psychologist] gave me about the condition and background of what is involved in the condition and by extension things to be aware of, as an employer was very useful. (EMP_03)
I had my yearly review from my manager, and he said since November or December last year he has seen that my output has improved, and I am doing more, I have more energy to give or put into my work, so yes, it is all flying colours from every direction. (MS_11)
Empowerment through knowledge
Empowerment was a recurring topic throughout the interviews. Understanding their legal rights and learning what made their symptoms worse or fluctuate over the day was seen as crucial to requesting support. The knowledge acquired helped the participants with MS structure their requests and address the employer’s questions:
I feel empowered and capable. I have had some conversations with my new line manager, and she is very supportive. Whenever I need it, I would be able to speak up for myself. Because I think a lot of the things with the understanding the MS, now I feel in a better position because I understand how it affects me in work, I can ask for relevant things. (MS_05)
Before we started talking, the cognitive side worried me, it scared me, because that is the side of me that I use all the time at work, that’s the side that pays my wages, keeps food on the table. (MS_01)
I think it has been useful because as you know, [name] has issues of coming to terms with her condition, and I think this has helped her face up to it and therefore has been more open to all of us at work. (EMP_01)
Intervention components and attributes
Three main sub-themes were drawn from this theme referring to the support received, tailoring of the intervention, and the therapist’s attributes.
Support received
The participants with MS highlighted the importance of conducting a detailed assessment of needs at work to think about barriers at work. In particular, participants found it beneficial to discuss ideas to manage the challenges at work:
I think it was the practical tips really, and talking through them with somebody, it is nice when somebody understands what is going on or says that these things happen, and they are real. It is Ok to feel like that. (MS_12)
You [assistant psychologist] used to send us an email summarizing what we covered [in the session] and any information with it. You would always then re-cover what we did in the previous session, so it jogged my memory of what we were going to cover today. (MS_04)
Intervention tailoring
Receiving an individually-tailored intervention in terms of hours of support, content, and goals was seen as a valued feature of MSVR by employers and people with MS:
I think because it [the intervention] was based around me and my outcomes, I felt it was all valuable because it was all specific to what I was saying. (MS_05)
With some things like “Access to Work,” the sort of length of time for the study might need to be more flexible so that you start and if things like that have to go back to Government or HR, you can have a sort of a number of hours in one month, and then come back to it. (MS_08)
Therapist’s attributes
The participants with MS believed that it was essential for the success of the intervention to have a therapist (i.e., the person delivering the intervention) who has extensive knowledge about MS and employment law. They also commented on the need for the therapist to collaborate with other professionals (e.g., human resources, legal representatives) to complement the support:
The person that is leading it [the intervention], is quite important as well. Because you [assistant psychologist] have done a lot of research, you have really good natural knowledge on the topics that I wanted advice about, but then also, you supplemented your natural knowledge with seeking advice from other professionals that would be more knowledgeable in a particular knowledge as well. (MS_14)
I think it was you [assistant psychologist]…you made me feel more confident. It is all of that, I think the whole thing has been very beneficial. (MS_12)
Convergence matrix
The combined findings from both methodologies and levels of agreement are presented in . There was convergence on only one measure (fatigue). We found complementary data from the anxiety, depression, and goal attainment measures. For most measures, there was a disagreement between the quantitative and qualitative data about cognition, work self-efficacy, and work instability. Two measures (relationship with line manager and empowerment) were not covered by the quantitative findings and were only identified in the qualitative data.
Table 10. Convergence matrix case series.
Discussion
It was feasible and acceptable to deliver MSVR for employed people with MS and their employers in a community setting. MSVR was associated with improved goal attainment, but the intervention had no impact on measures of quality of life, fatigue, mood, cognition, workplace accommodations, work instability, and work self-efficacy. All participants recruited completed the intervention.
On average, participants with MS needed fewer than the originally planned 10 h of support. A third of participants with MS did, however, need additional hours, but these were still provided within the intervention timeline (3 months). Because the intervention was highly individualised, those participants who were experiencing issues with their employers or had greater difficulty managing their symptoms at work and required further support to address their needs. This heterogeneity in the intensity of support needed has been discussed in the literature that suggests that all people with MS should be informed about where to look for support with employment; those who are concerned about work should be supported to self-manage their condition, and a smaller group of people with MS who are in a work crisis (e.g., attending an employment tribunal) require specialist VR support [Citation35]. However, it is not yet clear what factors (employment, clinical, personal) led to people needing these different levels of support or indeed the content of the specialist support.
The most commonly requested support was related to managing cognitive problems and fatigue at work. These findings are in line with other studies that suggest fatigue is a commonly reported factor for leaving the workforce [Citation36] and cognitive problems negatively affect work performance [Citation37].
Additionally, most participants requested support in identifying reasonable accommodations and understanding legal rights. Unfortunately, the experiences of delivering the intervention and interviews highlighted that not all employers provided the accommodations requested. This was also found in research about disability equality in the workplace, suggesting that up to 67% of workers with disabilities in the UK have had all or some of their accommodations requests refused [Citation38].
For this reason, participants with MS requested information about their legal rights. Under the UK Equality Act (2010) employers have a legal responsibility to implement reasonable accommodations for employees with MS [Citation16]. However, some employers still fail to provide these accommodations [Citation11]. Therefore, professionals involved in the delivery of VR for people with MS should know disability legislation and discrimination, as well as the ability to negotiate support with employers.
Delivering the intervention during the pandemic helped us identify areas of support that were not originally intended to be addressed by the intervention, such as support with benefits and support understanding Covid-19 regulations and what they meant for the working arrangements of the participants with MS. The intervention was developed pre-Covid-19; thus, we could not have foreseen the need for this support during the development stages. However, because the intervention was still in the modelling phase of its development, we had room to incorporate additional support as needed.
Participants recognised that receiving individually-tailored support was the most important attribute of the intervention. The intervention was designed to adopt a flexible approach to provide tailored support in terms of content, goals, hours of support, modality of delivery, and frequency of sessions. The benefits of individually-tailored support have been widely acknowledged in the literature [Citation6,Citation8].
One of the main limitations of the study is that we only recruited three employers for the intervention. Thus, we were unable to provide detailed information about their needs. This finding is interesting in itself and aligns with previous research in VR for people with long-term neurological conditions reporting challenges with employer recruitment [Citation39]. Employers are a key factor in work stability [Citation35]. Unfortunately, many participants with MS were uncomfortable with involving their employers because they had poor relationships with their line managers. To compensate for the lack of employer engagement, the intervention empowered the participants with MS to request additional support from their line managers and advised them on how to talk about the impact of their MS at work. Future research should aim to explore the benefits for employers of supporting employees with disabilities at work, to enhance their engagement in VR interventions. Examples of strategies could be disability confident schemes, developing accredited training opportunities for employers or implementing policies that require organisations to demonstrate that they can support employees with disabilities at work.
One of the main strengths of this study was the diversity of methods used to collect data about the intervention delivered. We collected both quantitative and qualitative data to address the study’s aims. Data from a proforma and notes were taken by the assistant psychologist during intervention delivery and were combined to measure the intervention content and timing. This provided rich data to describe what VR interventions for people with MS could include, and to illustrate the nature of individual tailoring in terms of content, dose, and measure the intensity of hours of support needed according to the person with MS and their employment circumstances.
We also used multiple quantitative measures to obtain rich data about the impact of the VR intervention on aspects that were addressed with the intervention, such as fatigue and cognition. We selected questionnaires that had been validated with people with MS (where possible) and were simple and quick to complete, to reduce participant burden. We felt that including a lengthy assessment might lead to participants getting tired or not completing all the questions. Unfortunately, we did not find any effect of the MSVR on the measures of quality of life, fatigue, mood, cognition, work instability, and work self-efficacy. This could be because they were insufficiently sensitive to changes resulting from the intervention, which were mostly identified by the qualitative findings. This discrepancy may be explained by heterogeneity in the sample in terms of disability levels, support received at work and the impact of MS at work. Additionally, not all the benefits of the intervention could be captured using the quantitative measures selected. There are no measures specific enough to capture gradual changes in relationships with their line managers or gain a better understanding of the support that may be beneficial for the person with MS in the future. For this reason, it is important to include vocational goal setting as a key outcome of VR interventions. Finally, the impact of the Covid-19 pandemic led to people with disabilities experiencing high levels of isolation, poor access to other healthcare services, and uncertainty at work [Citation40]. These issues were recorded in the interviews and participants attributed increased fatigue and lower mood to the Covid-19 restrictions.
Future studies should explore other tools that may be more suitable to measure the impact of VR interventions. For example, it may be beneficial to include tools to measure empowerment and understand relationships with line managers. In this study, participants suggested having become more empowered at work, however, this was only captured in the post-intervention interviews. There is also a need to include outcome measures for the employers to capture changes in their knowledge about MS, confidence in managing the person with a health condition at work, and attitudes towards disabilities.
Because of the diversity in employment, clinical, and personal characteristics, there is a need to further understand the support (in terms of content and intensity) that people with MS need according to their circumstances; as well as the mechanisms underlying of VR for people with MS, so that there is a clear understanding of what aspects of the support provided led to successful goal achievement for most participants, and why others did not benefit from the support.
In conclusion, VR interventions have the potential to help people with MS achieve their employment goals. There is a need to support healthcare professionals involved in the care of people with MS to identify those experiencing employment concerns and develop services that integrate employment and healthcare services to provide comprehensive care to people with MS.
Supplemental Material
Download Zip (573.1 KB)Acknowledgements
The authors thank the participants included in this research for their time and Dr. Jain Holmes for providing support and mentoring during the delivery of the intervention.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Cardone A. Having the conversation about work with people with multiple sclerosis: a guide for healthcare professionals. Neurodegener Dis Manag. 2017;7(6s):41–44.
- MS Society. MS Prevalence Report. 2020. Available from: https://www.mssociety.org.uk/what-we-do/our-work/our-evidence/ms-in-the-uk
- Rumrill PD, Koch LC, Wohlford S. Job retention strategies for individuals with multiple sclerosis. J Vocat Rehabil. 2013;39:127–135.
- Waddell G, Kim Burton A. Is work good for your health and well-being? 2006;57:229.
- British Society of Rehabilitation Medicine. Vocational rehabilitation-the way forward. 2nd ed. BSRM Working Party Report; London: BSRM 2003.
- Department of Health. The National Service Framework for long term conditions. London; Department of Health (2005).
- Department of Health. The NHS outcomes framework 2015/16. 2013. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/385749/NHS_Outcomes_Framework.pdf
- Khan F, Ng L, Turner-Stokes L. Effectiveness of vocational rehabilitation intervention on the return to work and employment of persons with multiple sclerosis. Cochrane Database Syst Rev. 2009;2009(1):CD007256.
- Dorstyn D, Roberts R, Murphy G, et al. Online resource to promote vocational interests among job seekers with multiple sclerosis: a randomized controlled trial in Australia. Arch Phys Med Rehabil. 2018;99(2):272–280.
- Stimmel MB, Cohen JN, Schneider SJ, et al. A neuropsychologically-based intervention with increased follow-up support for employed women with multiple sclerosis: a pilot randomized controlled trial. Clin Rehabil. 2020;34(10):1292–1302.
- de Dios Pérez B, Radford K, das Nair R. Experiences of people with multiple sclerosis at work: towards the understanding of the needs for a job retention vocational rehabilitation intervention. Work. 2022;72(1):303–313.
- Sweetland J, Riazi A, Cano SJ, et al. Vocational rehabilitation services for people with multiple sclerosis: what patients want from clinicians and employers. Mult Scler. 2007;13(9):1183–1189.
- de Dios Pérez B. Preventing job loss for people with multiple sclerosis [PhD Thesis]. Embargo: University of Nottingham; 2022.
- World Health Organisation. International classification of functioning, disability and health: ICF. Geneva: World Health Organization: 2001.
- Loisel P, Buchbinder R, Hazard R, et al. Prevention of work disability due to musculoskeletal disorders: the challenge of implementing evidence. J Occup Rehabil. 2005;15(4):507–524.
- Legislation.gov.uk. 2010. Equality Act 2010. [online] Available from: https://www.legislation.gov.uk/ukpga/2010/15/contents
- Hoffmann T, Glasziou P, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Br Med J. 2014;348:g1687.
- Phillips J, Drummond A, Radford K, et al. Return to work after traumatic brain injury: recording, measuring, and describing occupational therapy intervention. Br J Occupational Therapy. 2010;73:422–430.
- Grant M, Radford K, Sinclair E, et al. Return to work after stroke: recording, measuring, and describing occupational therapy intervention. Br J Occup Therapy. 2014;77:457–465.
- Sullivan MJL, Edgley K, Dehoux E. A survey of multiple sclerosis: perceived cognitive problems and compensatory strategy use. Can J Rehabil. 1990;4:99–105.
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–365.
- McFadden E, Horton MC, Ford HL, et al. Screening for the risk of job loss in multiple sclerosis (MS): development of an MS-specific work instability scale (MS-WIS). Mult Scler. 2012;18(6):862–870.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Fisk JD, Ritvo PG, Ross L, et al. Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis. 1994;18: s 79–83.
- Van Reenen M, Janssen B. EQ-5D-5L user guide basic information on how to use the EQ-5D-5L instrument. Rotterdam: EuroQol Research Foundation (2015): 9.
- Silvia P, Maria Luisa F, Francesco A, et al. Work Self-Efficacy Scale and search for Work Self-Efficacy Scale: a validation study in Spanish and Italian cultural contexts. Revista de Psicología Del Trabajo y de Las Organizaciones. 2010;26:201–210.
- Watkin C, Phillips J, Radford K. Brain injury what is a “return to work” following traumatic brain injury? Analysis of work outcomes 12 months post TBI what is a “return to work” following traumatic brain injury? 2019;34:68–77.
- Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil. 2009;23(4):362–370.
- Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. Brit. Med. J. 320,7227(2000):114.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions Michie et al. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42–11.
- Keith RE, Crosson JC, O'Malley AS, et al. Using the consolidated framework for implementation research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci. 2017;12(1):15.
- Yardley L. Dilemmas in qualitative health research. Psychol Health. 2000;15:215–228.
- O’Cathain A, Knowles E, Turner J. et al. Phase 3 integration of regression and case studies. Explaining variation in emergency admissions: a mixed-methods study of emergency and urgent care systems. NIHR Journals Library, 2014.
- Department for Work and Pension. Access to work: get support if you have a disability or health condition: what access to work is - GOV UK. Available from: https://www.gov.uk/access-to-work.
- Doogan C, Playford ED. Supporting work for people with multiple sclerosis. Mult Scler. 2014;20(6):646–650.
- Krupp LB, Alvarez LA, LaRocca NG, et al. Fatigue in multiple sclerosis. Arch Neurol. 1988;45(4):435–437.
- Clemens L, Langdon D. How does cognition relate to employment in multiple sclerosis? A systematic review. Mult Scler Relat Disord. 2018;26:183–191.
- Unison. Let's be reasonable: disability equality in the workplace; 2019. Available from: https://www.unison.org.uk/content/uploads/2019/11/Lets-Be-Reasonable-disability-equality-in-the-workplace.docx
- Radford K, Phillips J, Drummond A, et al. Return to work after traumatic brain injury: cohort comparison and economic evaluation. Brain Inj. 2013;27(5):507–520.
- Shakespeare T, Watson N, Brunner R, et al. Disabled people in Britain and the impact of the COVID-19 pandemic. Soc Policy Adm. 2022;56(1):103–117.
- ONS. Standard occupational classification (SOC) – Office for national statistics. ONS; 2020. Available from: https://www.ons.gov.uk/methodology/classificationsandstandards/standardoccupationalclassificationsoc/soc2020
