Abstract
Purpose
This study aims to explore the meaningful contributions of rehabilitation for participants living with persistent pain.
Materials and methods
A phenomenological methodology was used. Thirteen purposefully selected participants, who self-identified as substantially improved from persistent pain due to rehabilitation, were interviewed in-depth. Data were analyzed using reflexive thematic analyses.
Results
Participants included three men and ten women, age ranging from 22–69 years, pain duration was 2–30 years. Seven interconnected themes were developed: 1) indication of negative pain and health care experiences, 2) supporting working alliance with healthcare professionals, 3) Pain Dialogue, 4) improved self-awareness and self-regulation, 5) different view on pain, 6) autonomy and personal growth and 7) hope and new perspective. Integration of these themes provided a framework for understanding meaningful contributions of rehabilitation from the participants’ perspective.
Conclusions
The study identified seven interconnected themes enhancing meaningful contributions of rehabilitation for participants who have substantially improved from persistent pain. These findings provide a novel conceptual understanding of how rehabilitation can foster recovery. The themes strongly support person-centred care, an understanding of Pain Dialogue and personal growth through the lens of the lived experience. The quality of the therapeutic relationship is considered a central vehicle for improved health outcomes.
IMPLICATIONS FOR REHABILITATION
A rehabilitation participant perspective can contribute to better outcomes in pain rehabilitation.
A shift from a pain-centred to a person-centred approach should be considered to enhance meaningful contributions of rehabilitation.
Pain Education should be reconceptualized into Pain Dialogue.
The quality of the therapeutic relationship can be regarded as a key driver for the effectiveness of person-centred care and Pain Dialogue.
Introduction
Persistent musculoskeletal (MSK) pain is a leading cause of disability worldwide, placing unsustainable strain on health systems [Citation1] and imposing a significant burden on those affected by persistent MSK pain [Citation2–5]. This burden demonstrates the need for effective person-centred care in pain rehabilitation. Although the International Association for the Study of Pain (IASP) defines pain as a complex health condition and acknowledges its personal nature [Citation6], many health care professionals (HCPs) find it challenging to integrate personal aspects in the management of persons with persistent pain [Citation7–14]. In pain rehabilitation, self-management support is an overall approach to managing persistent musculoskeletal pain [Citation15,Citation16], which is seen as essential to providing person-centred care [Citation17,Citation18]. Self-management support is defined as “supporting the individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition” [Citation15]. Pain Education (PE) is a common component of self-management support, that has been associated with clinically relevant benefits [Citation19–23]. Patients’ unhelpful beliefs regarding MSK pain have been associated with higher levels of pain-related fear and avoidance behaviours [Citation24–27]. Identifying patients’ beliefs is relevant due to their influence on reconceptualizing pain as safe and non-threatening [Citation28]. PE generally aims to align an individual’s pain experience and knowledge with modern pain science, thereby developing and strengthening their own biopsychosocial understanding of pain, which contributes to the conceptual change [Citation22,Citation23,Citation29]. Conceptual change refers to an integral process of restructuring of existing knowledge and acknowledges the relevance of cognitive, behavioural, and emotional aspects of pain [Citation30].
PE has been developed top-down by clinicians and researchers, relying largely on conceptual models that lack empirical foundation [Citation31,Citation32]. This top-down approach may not accurately address a person’s core problems or views on successful treatment outcomes [Citation33–35]. The current perspective is shifting towards increased awareness of participants’ view on PE and embracing (inter)active learning frameworks [Citation36]. However, based on the available evidence, it is impossible to make clear clinical recommendations for PE related to participants’ perspective on content and delivery [Citation29, Citation37]. The revised definition of pain by the IASP acknowledges that pain is a personal experience shaped by the unique life experiences of the person with pain [Citation6]. Despite the revised definition of pain and the promotion of person-centred care in rehabilitation guidelines, integrating the lived experience of pain remains a blind spot in PE and pain rehabilitation [Citation29,Citation38–42]. As a result, it remains unknown which aspects of PE and pain rehabilitation patients experience as the main valuable contributions. Including participants’ engagement in pain research [Citation43–45] and education is therefore essential, as they are best positioned to provide context for PE based on their experiences [Citation41,Citation42,Citation46,Citation47].
Qualitative research is the most suitable method to understand the meaningful contributions of rehabilitation in those who live with persistent pain [Citation47–51]. This study used the theory of “living well with chronic pain” [Citation48] and the conceptual model of the healing journey [Citation52] as a starting point. However, while these models describe processes for recovery from persistent pain, they do not provide insight into the meaningful contributions of rehabilitation for participants who experienced improvement. Previous qualitative studies have explored the experiences of rehabilitation participants undergoing a transdisciplinary PE program [Citation53] and pain reconceptualization following PE in a single centre. In these studies patients were commonly consulted by the same clinician, which may limit the transferability of the findings [Citation29,Citation54–57]. As such, the experiences have not yet been explored in a mix of primary, secondary, or tertiary care. The current study focuses on providing insights into a wide palette of meaningful contributions of rehabilitation in participants with persistent pain, independent of a specific program, clinic, clinician, or centre. Moreover, focusing on experiences in improvement may lead to a new conceptual comprehension of how rehabilitation may facilitate participants’ healing journey. In addition, this understanding has the potential to improve counselling as well as providing an opportunity to revisit HPC educational curricula through the lens of lived experience [Citation58]. The research question guiding this study is: “What are the meaningful contributions of rehabilitation for people who have substantially improved in living with persistent pain?” Understanding these contributions is important for improving person-centred care and facilitating better rehabilitation outcomes for those living with persistent pain.
Materials and methods
Design
The study design was based on principles of the “constructionist paradigm,” which involves exploring underlying ideas, assumptions, and conceptualizations, that are fluid and context dependent [Citation59–61]. The design involved iterative data collection and analysis of semi-structured in-depth interviews, focussing on facilitating meaning-making, interpreting and theme development [Citation62]. The findings were co-constructed by participant and researcher, with the researcher acting as a “subjective instrument.” Additionally, an interpretive phenomenological approach was used to gain a deeper understanding of the meaningful contributions in pain rehabilitation [Citation60,Citation63–65]. The Standards for Reporting Qualitative Research guided the reporting of this study [Citation66].
Participants
Between June 2021 to December 2022, participants were purposefully selected to encompass a wide range of characteristics [Citation65]. Eligibility criteria included self-identification as substantially improved from persistent pain (defined as pain persisting for more than three months) [Citation67] a history of treatment or currently treated for persistent pain in primary, secondary, and/or tertiary care settings, PE was part of pain management program or treatment, age of at least 18 years, proficiency in Dutch communication and writing, living independently in their own home. Participants were excluded if they had comorbid conditions (severe medical or psychiatric complaints) significantly interfering with their pain, functioning, or quality of life. Recruitment was conducted in collaboration with the Dutch patient organization “Pijnpatienten naar 1 stem,” a collaboration of 11 pain patient’s organizations, and through the researchers’ network. Those who considered themselves substantially improved were selected and invited to participate and provided written informed consent. Approval for this study was obtained from the local ethics committees committee at the University Medical Center Groningen (M21.267098).
Data collection
Participants’ demographic information, including sex, age, family status, type of pain problem, education level (primary, secondary, tertiary), duration of pain, level of healthcare (primary, secondary, and/or tertiary care settings: care provided respectively in a private practice or health centre, hospital and/or rehabilitation centre) and employment status, were obtained directly from the participants. Before the interviews, participants were informed about the research project, and the interviewer’s (AJB) professional background, role, and training. Semi-structured in-depth interviews were conducted using theoretical frameworks related to improvement in persistent pain [Citation48,Citation52]. The primary questions were: (a) "Could you share with me the most difficult moment in your life when dealing with persistent pain?”; b) What was the main impact on your life at that time and how is it now?"; (c) "How do you define improving from persistent pain?"; (d)” What were learnings from rehabilitation that significantly contributed to your improvement?" Additionally, participants were asked to reflect on a series of opposing statements regarding pain (e.g., suffering or challenge?; movement or rest?; exercise or pain medication?; and the significance or futility of understanding pain). Furthermore, questions were asked about learning strategies; “What was the best way for you to learn about pain?” During the interviews, the interviewer was responsive to the participants’ narrative, asking open-ended questions and follow-up probes to elicit in-depth information. The interview questions were developed by the research team, reviewed by an external pain expert (LM), and the Dutch Patient Association, and pilot-tested with three participants. Feedback from the pilot interviews and the interview skills of the primary researcher (AJB) was provided by two experienced health psychologists [Citation65]. All interviews were conducted by the same interviewer (AJB) at a convenient location for the participant.
Following the initial interviews, the interview’s focus was changed to better capture participants’ broader perspectives on meaningful contributions, with Pain Education (PE) playing an integral role in this framework. Our initial conceptualization centred on PE, with individuals actively engaging in learning about pain neurophysiology to enhance their condition. During the process, we observed that PE alone did not effectively facilitate a shift in participants’ perspectives on pain. Interestingly, PE was not at the centre of participants’ concerns reflecting on their rehabilitation benefits. Participants held explicit and implicit attitudes toward their pain, contributing to ambivalence and inconsistencies in their interpretation of pain experiences and willingness to adopt rehabilitation strategies. It became evident that PE did not address the primary needs of rehabilitation participants seeking improvement.
We incorporated peer-debriefing from the outset of the interviews. The interviewer (AJB) engaged in discussions and reflections on her experiences, impressions, and findings regarding the interviews with the second author (DP) [Citation60, Citation68]. Additionally, reflective notes were maintained to ensure ongoing reflexivity regarding the theoretical framework, interview guide, research team meetings, peer debriefing sessions, and data analysis.
Data analysis
All interviews were audio-recorded and transcribed verbatim by the primary researcher (AJB). Transcripts were analyzed using qualitative software (Atlas-ti 9) [Citation69]. Reflexive thematic analysis (RTA) was employed for data analysis [Citation62]. This approach underscores the researcher’s subjectivity as an analytic resource and their reflexive engagement with theory, data, and interpretation [Citation70]. The coding process was integral to theme development, encompassing inductive and theoretical/deductive coding approaches [Citation70,Citation71]. Themes represent patterns of shared meaning, underpinned by central concepts that provide a coherent narrative related to the research question [Citation62,Citation70,Citation71]. Themes are assumed to be the final outcomes of data coding and iterative theme development.
Researcher characteristics and reflexivity
RTA captures an approach that fully embraces qualitative research principles and acknowledge the subjective expertise the researcher contributes to the process [Citation70]. The study involved interviews conducted by a researcher (AJB) with a background in physiotherapy and human movement science, pursuing a PhD related to improving pain-related knowledge, attitudes, and beliefs of HCP’s. The researcher had no prior relationship with the participants. The second author (DP), an experienced researcher, lecturer, and clinician in physiotherapy and pain, collaborated closely with the primary author through peer debriefing. The third author (GP), an experienced health and clinical psychologist with expertise in qualitative research, provided psychological reflections on the development of themes as interdisciplinary surplus. The remaining members of the research team, along with a rehabilitation participant (EdR) serving as a “partner in research,” retained a somewhat distant position to enable a richer reflection on the research process and its outcomes.
Triangulation
The coding process was collaborative, with two researchers (AJB, DP) coding ten transcripts and three additional interviews used for refinement. Discussion and reflection on accuracy of codes took place, with the aim of developing a rich and nuanced reading of the data. For RTA, a six-phase process for data engagement, coding and theme development took place, consisting of 1) data familiarisation, 2) systematic data coding, 3) generating initial themes from coded and collated data, 4) developing and reviewing themes, 5) refining, defining and naming themes, and 6) writing the report [Citation70]. After eight interviews, an authors’ group meeting was held to determine the relevance of codes, and the relationships between codes in relation to the overall research question. A rehabilitation participant (EdR) participated in the authors’ group meeting and collaborated with the primary researcher during consultations [Citation43]. The results of this meeting provided input for follow-up interviews. In RTA, codes are dynamic, subject to evolution, expansion, rephrasing, merging, or deletion [Citation62,Citation71]. During meetings of GH, DP and AJB, themes were discussed on relevance and quality (information power) [Citation64,Citation72]. Conceptual depth was achieved when themes reached richness and diversity for refinement [Citation71]. Quotations from various participants were selected and translated into English to support theme reporting.
Results
Participants
Sixteen eligible participants were invited for an interview, of whom three declined due to either excessive time commitments or unspecified reasons. In total, 13 participants were interviewed (three men, ten women). The age range was 22–69 years. The range of duration of pain was 2–30 years (). The interviews lasted 90–120 min.
Table 1. Characteristics of participants N = 13.
Meaningful contributions – an overview of themes
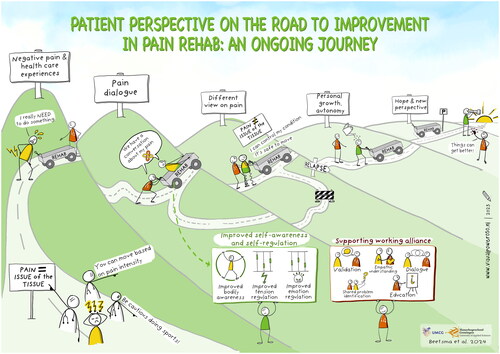
In total seven themes were generated. The integration of the seven themes () provides a comprehensive framework for understanding meaningful contributions of rehabilitation in participants who have experienced a substantial improvement in living with persistent pain. For readability, numerical identifiers have been assigned to the themes. In practice however, the themes are interconnected and without a ranking. The first theme focuses on the indication of negative experiences related to HCPs by rehabilitation participants, which has led to a state of earlier hopelessness and sets the foundation for the generation of themes that contributed to the process of improvement. Participants reported feeling distressed due to their past negative experiences, which ultimately led them to seek help in rehabilitation. The second theme focuses on the supporting working alliance with the HCP, in which the validation of the experience of pain was a prerequisite, as well as an acceptable and meaningful explanation for pain. The third theme involves deepening the interaction between the participant and the HCP, by using the supportive and meaningful role of education and communication in Pain Dialogue. Improved self-awareness and self-regulation (fourth theme) relate to the processes contributing to the development of a different view on pain and a helpful adaptive mindset about their body in pain (fifth theme). This ongoing process led to improved self-esteem, autonomy, and personal growth (sixth theme), which in turn facilitated an improved connection with others. The seventh theme concerns experiencing hope and new prospects for change. The processes underlying experienced improvement should be viewed as an ongoing journey of healing, rather than an endpoint of rehabilitation. This journey seemed to require a transition from a pain-centred approach to a more person-centred approach in rehabilitation.
Figure 1. Meaningful contributions of rehabilitation for participants living with persistent pain.
Theme 1: Indication of negative pain and health care experiences
Earlier negative experiences in healthcare and with HCPs were reported by almost all participants, causing distress, negative expectations, and a loss of motivation to seek help and to explore new pain coping strategies (again). The participant’s desire for healing and renewed help-seeking was primarily motivated by the accumulation of suffering. The pain itself was also identified as an important negative experience for many participants. For example, participants pushed themselves beyond their limits, ignored bodily signals, or suppressed the pain until it became unbearable. Participants often interpreted the pain as tissue damage and potentially harmful and would return to old thoughts and habits consistent with the biomedical model.
I push myself twice as hard when things get difficult…when I push myself twice as hard, I don’t feel the pain anymore. (P1)
Many participants reported struggling with their pain over extended periods and developed a dysfunctional relationship with their condition. Their pain was viewed as an external adversary, which posed a constant threat. As multiple participants reported receiving advice from their HCP based on a biomedical (i.e., tissue damage) model and provided conflicting advice, contributing to uncertainty, fear, and distress and for some participants, intensified the search for a medical diagnosis. Common negative learning experiences included beliefs such as “exertion or exercise is detrimental to me,” “I need to move based on the pain intensity” and “I am responsible for causing my own pain.” Participants reported also protective advice received from their HCPs related to physical activities and sports, suggesting individuals to become more cautious in loading their bodies and potentially developing dysfunctional behaviour patterns and bodily protective behaviours.
I started living according to my pelvic and hip trauma… That means I became more careful; I won’t go running because my pelvis and hips are not strong enough, or I won’t get pregnant again because my pelvis and hips probably can’t handle it. (P6)
Participants consistently highlighted a lack of alignment and agreement in problem identification and problem approach between themselves and their HCPs. They yearned for a holistic and person-centred approach that was often absent. Participants indicated that fragmentation of healthcare contributed to this problem.
The biomedical explanation for their symptoms, and a lack of acknowledgement and comprehension of their conditions left some participants feeling rejected and abandoned, leading to feelings of hopelessness and loneliness.
The rheumatologist basically only said, You’re overweight, you need to lose weight, and then fibromyalgia will disappear on its own. That didn’t really help. (P3)
Theme 2: Supporting working alliance with HCP
A recurring and pivotal concern in the context of experiencing improvement in living with pain is a positive working alliance with their HCPs. This alliance was experienced as essential for effective treatment. Participants consistently indicated that when they felt understood and attentively listened to by their HCPs, they were more likely to actively engage in rehabilitation and embrace novel behaviours.
HCP took me very seriously because she said: ‘If you have boundaries, you should respect them. If I can help you with that, you should say so, then we can look together at what you need’…that was the first time I thought, I also have something to say here…that you can learn to set your boundaries in a safe setting. (P3)
Validation by their HCPs included empathetic understanding, clear explanations about symptoms (e.g., the concept of pain without tissue damage), a safe treatment environment, an individualized assessment of needs, a positive working alliance, and reassurance against abandonment.
Most participants valued a person-centred approach, where HCPs attentively listened to their pain experiences, displayed empathy, and engaged in collaborative problem identification. This approach built trust in both the healthcare provider and the treatment. Some participants felt more secure and understood when their complex needs were addressed by a multidisciplinary team of HCPs, emphasizing the importance of supportive messages conveying a realistic perspective. These messages regulated tension and emotions, offering hope for improvement.
HCPs said: we don’t have all the answers, but we can help you discover the solution together. (P1)
I think information is important because otherwise, you’re really a victim of your own life. That’s also the case with pain; you lose control, the body you always relied on suddenly doesn’t work anymore…what you need is someone who thinks along with you…The most important thing about the HCP is to give someone the experience that they are not alone. (P9)
Participants also mentioned less successful working alliances. They mentioned that they relied heavily on the HCPs explanations and did not feel ownership of their own health concerns. They faced difficulties in managing their own health and achieving sustainable positive changes. These feelings of dependency towards the HCP prevented them from taking an active role in self-management and hindered their ability to develop the necessary skills and knowledge for long-term self-care.
I notice that I am too dependent on the explanations of the PT. If I have pains in my diaphragm region, I confuse it with heart problems and immediately experience a hypochondriacal attack. (P6)
Theme 3: Pain Dialogue
This theme underscores a pivotal lesson in rehabilitation, PE effectiveness hinges on acknowledging the role and influences of the other themes and meeting implicit needs. We found that participants’ selection of education and communication strategies is shaped by heightened self-awareness and self-regulation, external influences, and past negative experiences. Participants were able to listen, learn, and explore new strategies, when HCPs adopt a person-centred approach, recognizing participants’ expertise and experiences as valuable sources of knowledge. This approach, the so called ‘Pain Dialogue’ fosters respect, empowerment in self-care, and learning aligned with individual strengths and needs. Much of the learning process was not explicitly programmed, but arises from experiential reception of reassuring, and supportive HCP messages.
What I really appreciated is that the HCPs assumed that we were the experts and that allowed us to learn from our own foundation. (P3)
One notable positive outcome of Pain Dialogue was the alteration of participants’ emotional perception of their illness. They no longer perceived their pain as imaginary or self-inflicted. Moreover, when a message such as "you do not have a pelvic and hip trauma; your pelvic and hip area is strong,” was nested in a larger narrative conveying the message, this appears to enhance the strength and credibility of the message.
All participants highlighted the significance of active learning, which involves learning through reflection on personal experiences, supported and facilitated by the HCP.
PT provided an explanation that made me think, ‘actually, I’m still doing very well…a lot depends on how he approaches things and how calm he was and listened…he has so much knowledge about pain experiences. (P6)
The experience of some participants underscored the importance of integrating theoretical knowledge with their own personal pain encounters, a process further facilitated by real-life events. For instance, when confronted with a novel pain experience, one participant encountered difficulties in applying their explicit knowledge about pain to comprehend it. This scenario underscored the participant’s need for guidance and support from the HCP to effectively adapt to and attribute meaning to this newfound experience of pain.
Actually, the penny only really dropped when things went wrong. The theory was there, but in practice I got more and more symptoms and then I got stuck, and the PT pointed out to me: look at what’s going on in your life, and then I thought and felt, suddenly: aha! That’s how it works in practice. (P5)
One participant reported that explicit PE combined with personal experiences yielded positive learning outcomes. Through reflection on these processes, the participant gained insights into both unhelpful and beneficial thoughts and behavioural patterns. He perceived these learning processes as instrumental in enhancing their capacity to “manage pain in a better way.” Furthermore, some participants acknowledged that their negative thoughts had been impeding their progress and this realization emerged through confrontational dialogues with their HCPs. Such constructive interactions allowed space for doubt, catalyzed change, and ultimately contributed significantly to their recovery.
PT: You go to bed three times a day and you sleep? Did you do that before you got pain? It’s not logical that you sleep 12 hours every day. I had never thought about it that way. (P8)
HCP-guided education, as Pain Dialogue, empowered participants to structure their daily and weekly routines, employ active coping strategies, and engage in activities with reduced bodily protective behaviours. Many participants discovered satisfaction and relaxation in time-structured training or movement, characterized by clear progression, fostering a sense of achievement, and bolstering self-efficacy. These experiences enhanced their ability to regulate physical exertion and symptom management, reducing fear and nurturing confidence in their physical capabilities. Consequently, participants embraced a more adaptable and diversified approach to managing their pain.
My brain sends the wrong signals, and you can train that…I can be very disciplined…and that gives me a lot of satisfaction…I did the exercises on a time schedule (time contingent), and that’s how I set boundaries. (P10)
My PT said: I see no reason why you can’t run. That gave me a feeling that I can just do something, while I thought I shouldn’t do it, that makes such a difference in your self-confidence. (P6)
Positioning of Pain Education (PE) as explaining pain neurophysiology
Finally, it was noteworthy that most participants struggled to articulate and reproduce what they learned about pain neurophysiology, including aspects such as the involvement of the central nervous system and the brain. The position of PE, as learning about pain neurophysiology, evolved during the research process, emerging as a subtheme.
Theme 4: Improved self-awareness and self-regulation
During rehabilitation, some participants gained heightened self-awareness and body perception, boosting their confidence, self-efficacy, and the ability to view their pain differently. These improvements led to increased freedom, self-control, and the capacity to prioritize their values, ultimately enhancing self-esteem. Previously, limited self-regulation hindered their ability to adopt new perspectives on their pain problem. For instance, one participant, fearing her neck might detach, demonstrated a profound sense of insecurity within her own body. Trusted HCP-led Pain Dialogue emphasizing that pain does not necessarily indicate tissue damage could alleviate uncertainty and anxiety.
Physiotherapy has had an impact on ‘making peace again with my body’, ‘taking ownership of that entire upper back and neck’ and thinking again; this is a part of me. (P9)
As participants underwent a shift in their self-regulation, their engagement within the rehabilitation program increased. Certain individuals adopted attitudes encompassing respecting their own boundaries, a heightened acknowledgement of pain’s significance, increased body awareness, pain acceptance, and the allowance of emotions, resulting in more effective tension regulation.
I have learned that I am allowed to have and show emotions, and I notice that this does me a lot of good physically. It had caused a lot of tension in my body, and I notice that I can relax better now. (P3)
For some participants, receiving a diagnosis or explanation engendered a sense of security, further reinforced by a trusted HCP. Additionally, Pain Dialogue itself enhanced confidence and contributed to tension regulation, facilitating an improved connection with their inner selves.
The key to success is that it is in my consciousness, that I know what is going on, together with my positive mindset and returning to my own normal as soon as possible, that made the difference. (P8)
Theme 5: Different view on pain
Our study unveiled intricate and individualized shifts in participants’ views on pain. Prior to rehabilitation, many participants believed their persistent pain was caused by physical issues and tissue damage. However, their core beliefs evolved through interactions with their HCP and improved self-awareness and self-regulation. They learned that movement is safe, and pain does not necessarily indicate tissue damage. These new beliefs contrasted starkly with their previous beliefs, which centred on the idea that pain signalled a severe bodily problem.
What truly altered my perspective was when my physiotherapist (PT) said, you can just move… understanding central sensitization and knowing what’s going on in my life right now, there’s no cancer or anything were pivotal. (P5)
For some participants, understanding pain as originating from bodily signals and an overactive nervous system (such as the concept of central sensitization) helped to reduce their perception that “pain is happening to me.” In some cases, learning about the multifaceted nature of persistent pain empowered them to identify factors they could control or manage.
My brain is completely unaccustomed to it, so it sounds the alarm. My brain wants to protect me very well. Understanding this was very liberating, enabling better recovery. (P10)
Participants also recognized the significance of their own behavioural patterns. Our findings showed that understanding the benefits of exercise and physical activity, even in the presence of pain, helped recognize the importance of adopting healthy habits and maintaining a daily structure.
I had long attributed my pain to pelvic and hip trauma, but my PT said; your pelvis is strong, you can go running, that made a significant impact. (P6)
Talking about his rehabilitation process: My back had only grown stiffer over the past 1.5 years due to excessive rest. I needed to break that pattern. Instead of lying down, a walk in the forest was more beneficial. (P8)
Several participants emphasized comprehending the adverse effects of persistent dysfunctional behaviour patterns and reported heightened awareness of their unhealthy dysfunctional relationship with pain. Some HCPs encouraged them to cease battling pain and view their situation differently, empowering participants to take ownership of their recovery and experience positive physical and mental changes.
I gained insight into my relationship with my pain… which was predominantly adversarial further perpetuated by a diagnosis of pelvic and hip trauma. My PT altered my perspective; from being physically unfit to realizing that I did not have a healthy relationship with my pain and that I do have control over it, steering me away from fear and victimization. (P6)
In conclusion, participants’ evolving perspectives on pain, shaped by rehabilitation, HCP guidance, and improved self-awareness, encompassed a transition from viewing pain as an external affliction to recognizing their agency in managing and improving their condition. These shifts underscore the complex and individualized nature of pain perception and management.
Theme 6: Autonomy and personal growth
Our findings indicate that, during rehabilitation, a heightened sense of ownership over their pain, increased autonomy, personal growth, and enhanced empowerment are pivotal experiences, although these were usually not explicitly stated as treatment goals. A more positive attitude towards their inner selves correlated with a more positive attitude towards pain, as participants recognized their active role and autonomy in the improvement process. Some also identified the detrimental impact of a victimhood mindset, contributing to this transformative change.
‘I used to think that the pain wasn’t real, I shouldn’t make a fuss, there was nothing physically broken, but now I take that pain very seriously. That was a real eye-opener (P10)
Furthermore, some participants emphasized significant shifts in their work situations and environments, along with their ability to work without worsening symptoms. These changes held great importance for improved self-esteem, self-efficacy, and identity. For achieving these transformations, gaining insights, and exploring new work strategies such as pacing and adapting tasks or environments, was necessary.
I can even derive satisfaction from work on bad days, because there are still things I can do, and I no longer have to protect myself constantly. (P1)
That was a real eye-opener that you can work actively all day without overloading and getting physical complaints. (P2)
Theme 7: Hope and new perspective
Participants gained confidence in their capacity for positive change and improvement of their condition in rehabilitation. They expressed hope and optimism as they developed a different view on pain and a stronger sense of ownership for their recovery. This transformation was particularly pronounced when participants received encouragement and confidence from their HCPs, validating the possibility of improvement. Experiencing validation and maintaining optimistic recovery expectations, enhanced confidence in the future. Participants valued realistic perspectives and appreciated HCPs explicitly promoting a "growth mindset,” emphasizing the potential for learning and change. This shift towards a more positive perspective and increased psychological flexibility, facilitated acceptance of their situation. Additionally, the realization of self-efficacy and improved functioning empowered participants, providing a profound sense of liberation.
I was examined the entire day by a multidisciplinary team and when I got home, tears rolled down my cheeks. Finally, there was a story, which gives an enormous feeling of relief and perspective. This is super relevant for your recovery, and you have a goal together. (P6)
It was the first time someone said to me, ‘You have this, and it can get better.’ If she has so much confidence in it, it gives confidence in yourself. (P7)
Discussion
Our aim was to understand the meaningful contributions of rehabilitation for participants who have substantially improved in living with persistent pain. The interconnectedness of the themes and framing them within the process of meaningful contributions of rehabilitation, provides a novel conceptual understanding of how rehabilitation can enhance recovery. We argue that pain is a personal experience, as such, a person’s pain cannot be understood without the lived experience. Consequently, emphasis in pain rehabilitation varies depending on evolving personal needs. These are primarily unconscious and diverse aspects that contribute to individuals’ improvement in persistent pain. The themes illustrate the challenges encountered by the participants, as well as the paths they discovered and pursued to transform their perspectives on pain, self-awareness, trust in HCPs, and the necessary steps for their own journey of development. The processes underlying experienced improvement should be viewed as an ongoing journey of healing, rather than an endpoint of rehabilitation.
Regarding meaningful contributions of rehabilitation, it appeared that this process required a shift from a pain-centred approach to a person-centred approach. Many participants experienced a shift in their perspective on pain and personal mindset after enduring prolonged negative healthcare experiences. This shift was facilitated by establishing a trustworthy and validating working relationship with their HCP, alongside enhanced self-awareness, and self-regulation. Within the alliance, Pain Dialogue played a vital role. It served to validate the participants’ perception that their thoughts and feelings were understandable and legitimate, while also contributing to alleviate negative emotions, increased expression of feelings, and facilitated shared decision making and sense of autonomy [Citation58,Citation73–76]. Effective reception of safe and credible messages depended on the HCP’s ability to explain the participant’s condition in an understandable manner and the participant’s trust in the HCP to provide reassurance. Key elements of successful Pain Dialogue included a focus on the persons’ unique circumstances, including perceptions and emotions, the provision of a safe environment, and the contextual relevance of information to the individual’s specific situation, rather than the exclusive emphasis on neurophysiological content. Rehabilitation could promote autonomy and personal growth and fostered hope and resilience in participants, empowering them to approach and perceive their own body-mind-processes in a more positive and adaptive manner. Consequently, this growth in capacity for self-regulation [Citation76], positive self-perception, self-esteem, and autonomy in pain management can meaningfully impact their well-being.
In this study, effective pain management found its foundation in the personal journey of development, where addressing needs was pivotal. Participants reported that when they felt understood and heard by their HCPs, they were more likely to actively engage in rehabilitation and be receptive to confronting the meaning of pain and their way of coping. The existing literature assist the idea that a supportive partnership encourages participants to actively participate in rehabilitation [Citation39,Citation77] and promotes self-management [Citation16]. An HCP who is understanding, empathetic, and acknowledges the unique needs, values, and goals of their rehabilitation participants is considered essential for a person-centred approach in PE and pain management. This approach also involves facilitating Pain Dialogue and supporting and empowering the rehabilitation participant through the development of appropriate person-centred skills. These results appear to be consistent with other research on the topic [Citation18,Citation38,Citation45,Citation76, Citation78–81]. It is within an adequate context, where distrust and anxiety are addressed and overcome, that Pain Dialogue, exploration, and exercise can truly find their grounds. Thus, the quality of the therapeutic relationship is considered a central component for the effectiveness of person-centred care and Pain Dialogue [Citation82,Citation83]. Furthermore, we learned from the participants that previous health care experiences, based on a more biomedical model often lacked alignment and agreement on problem identification, treatment strategies, resulting in negative expectations, feelings of unsafety and invalidation. In previous research, many of the rehabilitation participants reported that they did not receive what they felt they needed in previous health care settings [Citation84].
For improvement in self-empowerment and autonomy, a deep conceptual change in understanding their experiences of pain is required [Citation85,Citation86]. For this, HCPs should provide space and opportunity for critical, guided reflection to encourage rehabilitation participants to re-examine their beliefs and attitudes. While participants wished the encounters to be empathetic and individualized, these aspects were often not sufficient to achieve sense of ownership and autonomic agency. A person-centred working alliance led to trust and productive, reciprocal discussions on critical issues that emerged during the rehabilitation process. Previous qualitative research has, similarly, highlighted the importance of a strong working alliance and active involvement of the participants in their own rehabilitation [Citation87,Citation88].
Many clinicians “explain pain” or “apply PE” in a pain-monologue matter focusing on educating modern pain beliefs, not aligned with a person-centred approach. Important limitations of conventional PE have become clear [Citation36]. The learning objectives of PE are only achieved in about 50% of the patients [Citation23,Citation29]. Pain and disability did not improve in those patients who did not undergo conceptual change [Citation36]. This finding is corroborated by qualitative appraisal of patient responses to PE [Citation54,Citation55]. In this study, most participants could not articulate and reproduce what they actually learned about pain neurophysiology in PE. This outcome diverges from our initial expectations of what was perceived important in pain rehabilitation. Rehabilitation participants learn to adopt a different perspective on their pain enabling them to progress, with less emphasis on their ability to articulate the neurophysiological mechanisms behind it. These outcomes align with recent findings of participants who experienced a change in their pain beliefs after PE, which were enhanced by a strong therapeutic relationship [Citation89]. The working alliance with the HCP, the diverse nature of pain conditions, and various factors impacting individual’s pain experiences present challenges in participating in rehabilitation and adopting PE. Also, some participants lacked resilience or access to supportive environments, hindering their ability to adopt a helpful perspective towards pain. Even those with extensive knowledge of pain and understanding its victimization aspect reported difficulties managing flare-ups. The existing literature supports the notion that for behaviour change, an understanding of capability, opportunity, and motivation constitutes three fundamental conditions for behaviour (COM-B model) [Citation90]. Participants held explicit and implicit attitudes towards their pain, which can contribute to ambivalence and inconsistencies in their interpretation of pain and what is adopted from rehabilitation. Target concepts taught in PE(28) could modify core beliefs, however, superficial changes with low learning yields can lead to a relapse into old biomedical thoughts and habits [Citation29,Citation30]. While individuals may experience a perceived overall effect of PE, their sense of ownership over the problem, autonomy and personal growth, functioning, and quality of life may not improve. Conversely, the favourable results of PE may manifest differently, involving a focus on person-centredness and supporting a robust working alliance during PE. This means allocating enough time, attentive listening, delivering a clear explanation, and gaining insight into the patient’s symptoms and body awareness. The ultimate goal is to help people to attain self-control [Citation76] and find inner peace [Citation47, Citation53].
This study introduced a novel concept, termed Pain Dialogue, which integrates personalized PE, as opposed to the conventional HCPs’ pain-monologue approach, focusing on educating patients about pain neurophysiology. To enhance the effectiveness of PE, it should go beyond educating about pain neurophysiology and consider participant’s broader needs and perspectives [Citation91–93]. Participants conveyed that their inclination to actively participate in Pain Dialogue and adopt new behaviours was heightened when they perceived that their HCPs comprehended and attentively attended to their concerns. When HCPs adhered to a person-centred approach, explicitly conveying, "I might be able to help you, if we collaborate to clarify your pain” and recognizing the participants’ expertise and experiences as valuable reservoirs of knowledge, this further facilitated the establishment of a productive Pain Dialogue. Recognizing the influence of pain’s threat value on individuals understanding and coping, allowing rehabilitation participants to share their stories can promote readiness for PE [Citation29, Citation76]. In Pain Dialogue, viewing pain as adaptive processes and understanding the biopsychosocial aspects can develop greater resilience to cope with flare-ups [Citation28]. These aspects in Pain Dialogue enhances rehabilitation participants’ ability to cope with their condition, leading to active interventions like exercise, pursuing valued life goals, and promoting recovery [Citation29].
Strengths and limitations
Conceptual analyses of qualitative data, such as reflexive thematic analysis are interpretations of qualitative data. This interpretive process can be considered a strength because analyses rely on a rigorous approach to the data combined with reflexive and creative processes. Through an iterative and inductive approach to theme development, we were able to achieve conceptual depth and refine themes. To strengthen the rigor of our study, we implemented several measures such as extensive peer debriefing, researchers’ group meeting and a rehabilitation participant as a partner in research was included. We also consulted with an experienced clinical health psychologist to prevent researchers from leaning towards certain codes and themes. Additionally, the eligibility criteria were purposely broad to increase the transferability of our findings. We also paid significant attention to elaborating on the experiences of participants to ensure the credibility of the study. Our interviews lasted an average of two hours, which is longer than the typical one-hour duration of such interviews. Despite the researcher who conducted the interviews receiving interview training from an experienced clinical health psychologist and completing a course on qualitative research and analysis during the study, she had no prior experience in interviewing or conducting qualitative research. Despite efforts, individuals with low health literacy are underrepresented in the present study, limiting transferability to this relevant subgroup. It might even be reflective of the worrying observation that fewer people with low literacy benefit from healthcare interventions [Citation94,Citation95]. There are only 3 men included in the study. This could be seen as a limitation although the goal was not to be representative, but rather to have a rich sample. Also, the literature and our data do not suggest that there are differences between men and women regarding this subject. For improvement, we have relied on self-reported progress from a patient’s perspective aligned with a person-centred approach and the lived experience. If an appropriate objective measure were available, it could be beneficial to integrate this instrument into our study alongside self-reporting.
Recommendations
The effectiveness of PE is dependent on the presence of a supportive working alliance between the person and the HCP, as well as the fulfilment of the participants’ implicit needs. To enhance the effectiveness of PE, a shift from a pain-centred approach to a person-centred one should be considered, thus giving rise to the concept of Pain Dialogue. The themes derived from this study support person-centred care in pain rehabilitation and the pivotal role of Pain Dialogue, viewed through the lens of the lived experience. Consequently, we need to assess the outcomes of rehabilitation in a manner that more accurately aligns with a person-centred approach [Citation95,Citation96]. The quality of the therapeutic relationship is considered a central vehicle for the effectiveness of person-centred care and Pain Dialogue. Insight in the processes leading to new conceptual understanding of participants’ meanings, holds an educational potential in HCP training. Providing HCPs with opportunities to listen to participants narratives, creates the opportunity for transformative learning beyond the biomedical to a biopsychosocial, person-centred approach to health care. From this study, it seems very important to explicitly state goals related to a sense of ownership, personal growth, and autonomy in rehabilitation. These aspects in rehabilitation can provide direction and guidance for conversations with people with persistent pain.
Based on the findings of this study, the question arises whether the field of research into persistent pain learns enough from the perspective of the patient, who is an expert by experience. We would recommend learning from individuals with lived experience and incorporating patients as partners in research [Citation43]. Going beyond mere participation in research, individuals with lived experience provide invaluable insights. Their knowledge enriches our understanding of the treatments being studied, facilitates the translation of knowledge into practice, and contributes to achieving more favourable outcomes. For face and content validity of patient reported research instruments, the standard should be to see patients as experts [Citation97]. Future research is warranted to evaluate the impact of pain treatment approaches, incorporating person-centred care, Pain Dialogue, and a supportive working alliance to assess how these changes influence pain rehabilitation. Also, future research is needed in patients with low health literacy and in patients with low socioeconomic status. This patient population may require a different approach with a tailored recruitment method. Perhaps different themes are at play compared to those observed in the current study. Qualitative research can guide the development of educational strategies by examining how patients’ values inform treatment and advice.
In conclusion, this study demonstrates seven interconnected themes contributing to meaningful contributions of rehabilitation for participants who have substantially improved in living with persistent pain. These findings provide a novel conceptual understanding of how rehabilitation fosters recovery. The themes strongly support person-centred care, an understanding of Pain Dialogue and personal growth through the lens of the lived experience. The quality of the therapeutic relationship is considered a central vehicle for improved health outcomes.
Acknowledgments
We thank the interviewed participants for their valuable contributions to this study. We thank Lorimer Moseley (LM) for his contribution to the interview topics. During the preparation of this work the author(s) used ChatCPT (https://chat.openai.com) to formulate more concisely in the results section of this article.
Disclosure statement
No potential competing interest was reported by the authors.
Additional information
Funding
References
- Blyth FM, Briggs AM, Schneider CH, et al. The global burden of musculoskeletal pain—where to from here? Am J Public Health. 2019;109(1):35–40. doi: 10.2105/AJPH.2018.304747.[PMC]
- Goldberg DS, McGee SJ. Pain as a global public health priority. BMC Public Health. 2011;11(1):770. doi: 10.1186/1471-2458-11-770.
- Jackson T, Thomas S, Stabile V, et al. Prevalence of chronic pain in low-income and middle-income countries: a systematic review and meta-analysis. Lancet. 2015;385 Suppl 2: s 10. doi: 10.1016/S0140-6736(15)60805-4.
- Rice ASC, Smith BH, Blyth FM. Pain and the global burden of disease. Pain. 2016;157(4):791–796. doi: 10.1097/j.pain.0000000000000454.
- Breivik H, Eisenberg E, O’Brien T. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013;13(1):1229. doi: 10.1186/1471-2458-13-1229.
- Raja SN, Carr DB, Cohen M, et al. The Revised IASP definition of pain: concepts, challenges, and compromises. 2021;161(9):1976–82. doi: 10.1097/j.pain.0000000000001939.
- Alexanders J, Anderson A, Henderson S. Musculoskeletal physiotherapists’ use of psychological interventions: a systematic review of therapists’ perceptions and practice. Physiotherapy. 2015;101(2):95–102. doi: 10.1016/j.physio.2014.03.008.
- Singla M, Jones M, Edwards I, et al. Physiotherapists’ assessment of patients’ psychosocial status: are we standing on thin ice? A qualitative descriptive study. Man Ther. 2015;20(2):328–334. doi: 10.1016/j.math.2014.10.004.
- Verwoerd MJ, Wittink H, Goossens MEJB, et al. Physiotherapists’ knowledge, attitude and practice behaviour to prevent chronification in patients with non-specific, non-traumatic, acute- and subacute neck pain: a qualitative study. Musculoskelet Sci Pract. 2022;57(vember 2021):102493. doi: 10.1016/j.msksp.2021.102493.
- Cowell I, O’Sullivan P, O’Sullivan K, et al. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: a qualitative study. Musculoskelet Sci Pract. 2018;38(May):113–119. doi: 10.1016/j.msksp.2018.10.006.
- Synnott A, O’Keeffe M, Bunzli S, et al. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiother. 2015;61(2):68–76. doi: 10.1016/j.jphys.2015.02.016.
- Van Dijk J, Elbers S, Mollema J, et al. Physiotherapists using the biopsychosocial model: barriers and facilitators. A scoping review. Pain Practice. 2022;22:61–62.
- Simpson P, Holopainen R, Schütze R, et al. Becoming confidently competent: a qualitative investigation of training in cognitive functional therapy for persistent low back pain. Physiother Theor Pract. 2022;40(4):804–816. doi: 10.1080/09593985.2022.2151333.
- Simpson P, Holopainen R, Schütze R, et al. Training of physical therapists to deliver individualized biopsychosocial interventions to treat musculoskeletal pain conditions: a scoping review. Phys Ther. 2021;101(10):1–12. doi: 10.1093/ptj/pzab188.
- Barlow J, Wright C, Sheasby J, et al. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–187. doi: 10.1016/s0738-3991(02)00032-0.
- Hutting N, Johnston V, Staal JB, et al. Promoting the use of self-management strategies for people with persistent musculoskeletal disorders: the role of physical therapists. J Orthop Sports Phys Ther. 2019;49(4):212–215. doi: 10.2519/jospt.2019.0605.
- Hutting N, Caneiro JP, Ong’wen OM, et al. Patient-centered care in musculoskeletal practice: key elements to support clinicians to focus on the person. Musculoskelet Sci Pract. 2022;57(July 2021):102434. doi: 10.1016/j.msksp.2021.102434.
- Hutting N, Caneiro JP, Ong’wen OM, et al. Person-centered care for musculoskeletal pain: putting principles into practice. Musculoskelet Sci Pract. 2022;62(September):102663. doi: 10.1016/j.msksp.2022.102663.
- Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain: a systematic review and meta-analysis. Man Ther. 2011;16(6):544–549. doi: 10.1016/j.math.2011.05.003.
- Louw A, Zimney K, Puentedura EJ, et al. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theor Pract. 2016;32(5):332–355. doi: 10.1080/09593985.2016.1194646.
- Siddall B, Ram A, Jones MD, et al. The short-term impact of combining pain neuroscience education with exercise for chronic musculoskeletal pain: a systematic review and meta-analysis. PAIN. 2021;163(1):e20–e30. Articles i. doi: 10.1097/j.pain.0000000000002308.
- Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. J Pain. 2015;16(9):807–813. doi: 10.1016/j.jpain.2015.05.005.
- Wood L, Hendrick PA. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: short-and long-term outcomes of pain and disability. Eur. J. Pain. 2019;23(2):234–249. doi: 10.1002/ejp.1314.
- Darlow B. Beliefs about back pain: the confluence of client, clinician and community. Int. J. Osteopat. Med. 2016;20:53–61. doi: 10.1016/j.ijosm.2016.01.005.
- Kragting M, Pool-Goudzwaard AL, Coppieters MW, et al. Illness perceptions in people with chronic and disabling non-specific neck pain seeking primary healthcare: a qualitative study. BMC Musculoskelet Disord. 2024;25(1):179. doi: 10.1186/s12891-024-07302-7.
- Briggs AM, Jordan JE, Buchbinder R, et al. Health literacy and beliefs among a community cohort with and without chronic low back pain. Pain. 2010;150(2):275–283. doi: 10.1016/j.pain.2010.04.031.
- Bunzli S, Smith A, Schütze R, et al. Beliefs underlying pain-related fear and how they evolve: a qualitative investigation in people with chronic back pain and high pain-related fear. BMJ Open. 2015;5(10):e008847. doi: 10.1136/bmjopen-2015-008847.
- Moseley G. Lorimer and DSB. Explain Pain Supercharged, The Clinician’s Manual. South Australia: Noigroup Publications; 2017.
- Watson JA, Ryan CG, Cooper L, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. J Pain. 2019;20(10):1140.e1-1140–e22. doi: 10.1016/j.jpain.2019.02.011.
- Nadelson LS, Heddy BC, Jones S, et al. Conceptual change in science teaching and learning: introducing the dynamic model of conceptual change. IJEP. 2018;7(2):151–195. doi: 10.17583/ijep.2018.3349.
- Leake HB, Heathcote LC, Simons LE, et al. Talking to teens about pain: a modified delphi study of adolescent pain science education. Canadian J. Pain. 2019;3(1):200–208. doi: 10.1080/24740527.2019.1682934.
- Stanton TR, Karran EL, Butler DS, et al. A pain science education and walking program to increase physical activity in people with symptomatic knee osteoarthritis: a feasibility study. Pain Rep. 2020;5(5):e830. doi: 10.1097/PR9.0000000000000830.
- Fischer D, Stewart AL, Bloch DA, et al. Capturing the patient’s view of change as a clinical outcome measure. J. Am. Med. Assoc. 1999;282(12):1157–1162.
- O’Brien EM, Staud RM, Hassinger AD, et al. Patient-centered perspective on treatment outcomes in chronic pain. Pain Med. 2010;11(1):6–15. doi: 10.1111/j.1526-4637.2009.00685.x.
- van Rysewyk S, Blomkvist R, Crighton R, et al. Understanding the lived experience of chronic pain: a systematic review and synthesis of qualitative evidence syntheses. 2023.
- Lorimer Moseley G, Leake HB, Beetsma AJ, et al. Teaching patients about pain: the emergence of pain science education, its learning frameworks and delivery strategies. J Pain. 2024;25(5):104425. doi: 10.1016/j.jpain.2023.11.008.
- Martinez-Calderon J, Ho EKY, Ferreira PH, et al. A call for improving research on pain neuroscience education and chronic pain: an overview of systematic reviews. J Orthop Sports Phys Ther. 2023;53(6):353–368–368. doi: 10.2519/jospt.2023.11833.
- O’Hagan ET, Cashin AG, Traeger AC, et al. Person-centred education and advice for people with low back pain: Making the best of what we know. Braz J Phys Ther. 2011;1(2178–5317):1–13.
- Miciak M, Mayan M, Brown C, et al. The necessary conditions of engagement for the therapeutic relationship in physiotherapy: an interpretive description study. Arch Physiother. 2018;8(1):3. doi: 10.1186/s40945-018-0044-1.
- Nicholls DA, Ahlsen B, Bjorbækmo W, et al. Critical physiotherapy: a ten-year retrospective. Physiother Theor Pract. 2023;00(00):1–13.
- Helme D. Trust me, I’m a patient: pain education for professionals from a lay perspective. Br J Pain. 2012;6(2):79–80.
- Tellier PP, Bélanger E, Rodríguez C, et al. Improving undergraduate medical education about pain assessment and management: a qualitative descriptive study of stakeholders’ perceptions. Pain Res Manag. 2013;18(5):259–265. doi: 10.1155/2013/920961.
- Belton J, Hoens A, Scott A, et al. Patients as partners in research: it’s the right thing to do. J Orthop Sports Phys Ther. 2019;49(9):623–626. doi: 10.2519/jospt.2019.0106.
- Duffett L. Patient engagement: what partnering with patient in research is all about. Thromb Res. 2017;150:113–120. doi: 10.1016/j.thromres.2016.10.029.
- Belton J, Birkinshaw H, Pincus T. Patient-centered consultations for persons with musculoskeletal conditions. Chiropr Man Therap. 2022;30(1):53. doi: 10.1186/s12998-022-00466-w.
- Hasenbring MI, Pincus T. Effective reassurance in primary care of low back pain: what messages from clinicians are most beneficial at early stages? Clin. J. Pain. 2015;31(2):133–136. doi: 10.1097/AJP.0000000000000097.
- Thompson K, Johnson MI, Milligan J, et al. Rethinking pain education from the perspectives of people experiencing pain: a meta-ethnography to inform physiotherapy training. BMJ Open. 2022;12(1):e046363. doi: 10.1136/bmjopen-2020-046363.
- Lennox Thompson B, Gage J, Kirk R. Living well with chronic pain: a classical grounded theory. Disabil Rehabil. 2018;42(8):1141–1152. doi: 10.1080/09638288.2018.1517195.
- Toye F, Seers K, Hannink E, et al. A mega-ethnography of eleven qualitative evidence syntheses exploring the experience of living with chronic non-malignant pain. BMC Med Res Methodol. 2017;17(1):116. doi: 10.1186/s12874-017-0392-7.
- Kitson A, Marshall A, Bassett K, et al. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs. 2013;69(1):4–15. doi: 10.1111/j.1365-2648.2012.06064.x.
- Thompson K, Johnson MI, Milligan J, et al. Twenty-five years of pain education research-what have we learned? Findings from a comprehensive scoping review of research into pre-registration pain education for health professionals. Pain. 2018;159(11):2146–2158. doi: 10.1097/j.pain.0000000000001352.
- Toye F, Belton J, Hannink E, et al. A healing journey with chronic pain: a meta-ethnography synthesizing 195 qualitative studies. Pain Med. 2021;22(6):1333–1344. doi: 10.1093/pm/pnaa373.
- Wijma AJ, Speksnijder CM, Crom-Ottens AF, et al. What is important in transdisciplinary pain neuroscience education? A qualitative study. Disabil Rehabil. 2018;40(18):2181–2191. doi: 10.1080/09638288.2017.1327990.
- Robinson V, King R, Ryan CG, et al. A qualitative exploration of people’s experiences of pain neurophysiological education for chronic pain: the importance of relevance for the individual. Man Ther. 2016;22:56–61. doi: 10.1016/j.math.2015.10.001.
- King R, Robinson V, Elliott-Button HL, et al. Pain reconceptualisation after pain neurophysiology education in adults with chronic low back pain: a qualitative study. Pain Res Manag. 2018;2018:3745651–3745610. doi: 10.1155/2018/3745651.
- Pate JW, Tran E, Radhakrishnan S, et al. The importance of perceived relevance: a qualitative evaluation of patient’s perceptions of value and impact following a low-intensity group-based pain management program. Medicina (Lithuania). 2021;57(1):46. doi: 10.3390/medicina57010046.
- Leake HB, Moseley GL, Stanton TR, et al. What do patients value learning about pain? A mixed-methods survey on the relevance of target concepts after pain science education. Pain. 2021;162(10):2558–2568. doi: 10.1097/j.pain.0000000000002244.
- Slater H, Jordan JE, O’Sullivan PB, et al. ‘Listen to me, learn from me’: a priority setting partnership for shaping interdisciplinary pain training to strengthen chronic pain care. Pain. 2022;163(11):e1145–e1163. doi: 10.1097/j.pain.0000000000002647.
- Hutter I, Hennink M, Bailey A. Qualitative research methods. London SAGE Publications; 2011.
- Pope C, Mays N. Qualitative research in health care, 4th ed. London Wiley Blackwell; 2020.
- Reeves S, Albert M, Kuper A, et al. Qualitative research: why use theories in qualitative research? BMJ. 2008;337(aug07 3):a949–a949. doi: 10.1136/bmj.a949.
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exer. Health. 2019;11(4):589–597. doi: 10.1080/2159676X.2019.1628806.
- Creswell JW. Qualitative inquiry & research Design: choosing among five approaches. 2nd ed. Thousand Oaks (CA): Sage; 2007, 57–62.
- Braun V, Clarke V. Qualitative research in psychology using thematic analysis in psychology using thematic analysis in psychology. Qual. Res. Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa.
- Kelly A, Tymms K, Fallon K, et al. Qualitative research in rheumatology: an overview of methods and contributions to practice and policy. J. Rheumatol. 2021;48(1):6–15.
- O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388.
- Finnerup NB, Scholz J, First MB, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11) rolf-detlef. Pain. 2018;160(1):19–27.
- McMahon SA, Winch PJ. Systematic debriefing after qualitative encounters: an essential analysis step in applied qualitative research. BMJ Glob Health. 2018;3(5):e000837. doi: 10.1136/bmjgh-2018-000837.
- ATLAS.ti GmbH. atlas.ti.7. Berlin: Cincom Systems, Inc; 1993.
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual. Res. Psychol. 2021;18(3):328–352. doi: 10.1080/14780887.2020.1769238.
- Braun V, Clarke V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qual. Res. Sport Exer. Health. 2021;13(2):201–216. doi: 10.1080/2159676X.2019.1704846.
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–1760. doi: 10.1177/1049732315617444.
- Linton SJ. Intricacies of good communication in the context of pain: does validation reinforce disclosure? Pain. 2015;156(2):199–200. doi: 10.1097/01.j.pain.0000460297.25831.67.
- Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain. 2016;156(2):215–219. doi: 10.1097/01.j.pain.0000460301.18207.c2.
- Linton SJ, Boersma K, Vangronsveld K, et al. Painfully reassuring? The effects of validation on emotions and adherence in a pain test. Eur. J. Pain. 2012;16(4):592–599. doi: 10.1016/j.ejpain.2011.07.011.
- Mol TI, van Bennekom CAM, Scholten EWM, et al. Self-regulation as rehabilitation outcome: what is important according to former patients? Disabil Rehabil. 2022;44(24):7484–7490. doi: 10.1080/09638288.2021.1998663.
- Higgins T, Larson E, Schnall R. Unraveling the meaning of patient engagement: a concept analysis. Patient Educ Couns. 2017;100(1):30–36. doi: 10.1016/j.pec.2016.09.002.
- Howarth M, Warne T, Haigh C. Pain from the inside: understanding the theoretical underpinning of person-centered care delivered by pain teams. Pain Manage Nurs. 2014;15(1):340–348. doi: 10.1016/j.pmn.2012.12.008.
- Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79–86. doi: 10.1136/bjsports-2018-099878.
- Ringold S, Angeles-Han ST, Beukelman T, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for non-systemic polyarthritis, sacroiliitis, and enthesitis. Arthritis Care Res (Hoboken). 2019;71(6):717–734. doi: 10.1002/acr.23870.
- Wijma AJ, Bletterman AN, Clark JR, et al. Patient-centeredness in physiotherapy: what does it entail? A systematic review of qualitative studies. Physiother Theor Pract. 2017;33(11):825–840. doi: 10.1080/09593985.2017.1357151.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc. Sci. Med. 2000;51(7):1087–1110. doi: 10.1016/S0277-9536(00)00098-8.
- MacLeod R, McPherson KM. Care and compassion: part of person-centred rehabilitation, inappropriate response or a forgotten art? Disabil Rehabil. 2007;29(20-21):1589–1595. doi: 10.1080/09638280701618729.
- Bunzli S, Watkins R, Smith A, et al. Lives on hold: a qualitative synthesis exploring the experience of chronic low-back pain. Clin. J. Pain. 2013;29(10):907–916. doi: 10.1097/AJP.0b013e31827a6dd8.
- Hoggan C. Transformative learning theory: where we are after 45 years. 2023, 5–11.
- Mezirow J. Transformative learning: theory to practice. In Transformative learning theory, Vol. 7. Wiley Online Library; 1997,5–12.
- Holopainen R, Piirainen A, Heinonen A, et al. From “non-encounters” to autonomic agency. Conceptions of patients with low back pain about their encounters in the health care system. Musculoskelet Care. 2018;16(2):269–277. doi: 10.1002/msc.1230.
- Paap D, Krops LA, Preuper HRS, et al. Participants’ unspoken thoughts and feelings negatively influence the therapeutic alliance, a qualitative study in a multidisciplinary pain rehabilitation setting. Disabil. Rehabil. 2021;0(0):1–11.
- Acker R, Swain N, Perry M, et al. ‘Thinking about pain in a different way’: patient perspectives of a neuroscience-informed physiotherapy programme for rotator cuff-related shoulder pain. Musculoskelet Sci Pract. 2023;63(December 2022):102691. doi: 10.1016/j.msksp.2022.102691.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:42.doi: 10.1186/1748-5908-6-42.
- Louw A, Sluka KA, Nijs J, et al. Revisiting the provision of pain neuroscience education: an adjunct intervention for patients, but a primary focus for clinician education. J Orthop Sports Phys Ther. 2020;51(2):57–59. doi: 10.2519/jospt.2021.9804.
- Zimney K, Van Bogaert W, Louw A. The biology of chronic pain and its implications for pain neuroscience education: state of the art. J Clin Med. 2023;12(13):4199. doi: 10.3390/jcm12134199.
- Correia JC, Waqas A, Aujoulat I, et al. Evolution of therapeutic patient education: a systematic scoping review and scientometric analysis. Int J Environ Res Public Health. 2022;19(10):6128. doi: 10.3390/ijerph19106128.
- van der Scheer-Horst E, Rutten G, Stortenbeker I, et al. Limited health literacy in primary care physiotherapy: does a physiotherapist use techniques to improve communication? Patient Educ Couns. 2023;109(May 2022):107624. doi: 10.1016/j.pec.2023.107624.
- Reneman MF, Medicine R, Schrier E, et al. Patients first: toward a patient-centered instrument to measure impact of chronic pain. Phys Ther. 2018;98(7):616–625.
- Borghuis EMC, Reneman MF, Schiphorst Preuper HR. Assessing discrepancies in outcomes of pain rehabilitation: “these questionnaires don’t measure results that are relevant to me. Disabil Rehabil. 2020;42(16):2374–2380. doi: 10.1080/09638288.2018.1561956.
- Vet Hcw d, Terwee CB, Mokkink LB, et al. Measurement in medicine: a practical guide. Quality of Life Research. Cambridge University Press; 2011. doi: 10.1017/CBO9780511996214.
