Abstract
In the setting of increasing restrictions to legal abortion in the United States, reports have emerged of self-induced termination of pregnancies with misoprostol, obtained without a prescription or provider. This study seeks to describe the prevalence of women seeking or employing misoprostol for self-induced abortion, and how they access information. In a cross-sectional study of women immediately following their abortion at three reproductive health clinics in the Midwestern United States, an anonymous survey queried gestational age, barriers, online investigation about self-induction and opinions concerning the availability of medical abortion. From June to September 2016, 276 women participated out of 437 presenting to the clinics during the study period. One hundred and ninety-one (74.6%) women had investigated abortion options online, and of those, 58 (30.9%) investigated misoprostol online, for home use. Women who investigated online options were less likely to have had a prior abortion than those who did not investigate online (29.3% vs. 63.1%, p < .01). They were also more likely to report prior home attempts to end this pregnancy (8.6% vs. 0%, p = .05). Overall, four (1.6%) of the respondents purchased misoprostol and three (1.2%) used it. A majority of women seeking an abortion sought online information prior to their clinic appointment, and almost a third of those had investigated misoprostol for home use. Women are accessing information regarding misoprostol for self-induction of abortion on the Internet. As barriers to legal abortion increase, women may be more likely to self-induce abortion.
Resumé
Dans le contexte d’une multiplication des restrictions à l’avortement légal aux États-Unis, des interruptions de grossesse provoquées par les femmes elles-mêmes avec le misoprostol, obtenu sans ordonnance ou prestataire, ont été signalées. Cette étude souhaite décrire la prévalence des femmes recherchant ou employant le misoprostol pour un avortement autoprovoqué et montrer comment elles ont obtenu les informations. Dans une étude transversale auprès de femmes immédiatement après leur avortement dans trois dispensaires de santé reproductive dans le Midwest aux États-Unis, une enquête anonyme a interrogé sur l’âge gestationnel, les obstacles rencontrés, les recherches en ligne sur le déclenchement de l’avortement et les opinions concernant la disponibilité de l’avortement médicamenteux. De juin à septembre 2016, 276 femmes y ont participé, sur 437 s’étant présentées dans les dispensaires pendant la période de l’étude. Cent quatre-vingt-onze femmes (74,6%) s’étaient informées en ligne sur les options d’avortement, dont 58 (30,9%) avaient enquêté sur le misoprostol en ligne, pour une utilisation à domicile. Les femmes qui avaient recherché les options en ligne avaient moins de probabilités d’avoir eu un avortement précédemment que celles qui n’avaient pas fait de recherches en ligne (29,3% contre 63,1%, p < 0,01). Elles avaient aussi plus de probabilités de notifier des tentatives antérieures d’interruption de grossesse à domicile (8,6% contre 0%, p = 0,05). Dans l’ensemble, quatre (1,6%) des répondantes ont acheté du misoprostol et trois (1,2%) l’ont utilisé. Une majorité des femmes souhaitant avorter ont recherché des informations en ligne avant leur rendez-vous au dispensaire, et près d’un tiers d’entre elles ont enquêté sur le misoprostol utilisé à domicile. Les femmes accèdent sur internet à des informations sur le misoprostol pour interrompre elles-mêmes leur grossesse. À mesure que les obstacles à l’avortement se multiplient, il est probable que les femmes seront plus nombreuses à provoquer elles-mêmes leur avortement.
Resumen
En el contexto de crecientes restricciones al aborto legal en Estados Unidos, han surgido informes de interrupciones del embarazo autoinducidas con misoprostol, obtenido sin receta y sin prestador de servicios. Este estudio procura describir la prevalencia de mujeres que buscan o emplean misoprostol para autoinducir el aborto, y cómo acceden a la información. En un estudio transversal de mujeres inmediatamente después de su aborto en tres clínicas de salud reproductiva en el medio oeste de Estados Unidos, una encuesta anónima preguntó acerca de la edad gestacional, barreras, investigación en línea sobre autoinducción y opiniones sobre la disponibilidad del método de aborto con medicamentos. Desde junio a septiembre de 2016, de las 437 mujeres que se presentaron en las clínicas durante el período del estudio, 276 participaron. Ciento noventa y un mujeres (74.6%) habían investigado las opciones de aborto en línea y, de esas, 58 (30.9%) investigaron el misoprostol en línea, para uso domiciliario. Las mujeres que investigaron las opciones en línea eran menos propensas a haber tenido un aborto anterior que aquéllas que no lo investigaron en línea (29.3% vs 63.1%, p < 0.01). Asimismo, eran más propensas a informar intentos domicilarios anteriores de interrumpir ese embarazo (8.6% vs 0%, p = 0.05). En general, cuatro (1.6%) de las encuestadas compraron misoprostol y tres (1.2%) lo usaron. La mayoría de las mujeres en busca de un aborto buscaron información en línea antes de acudir a su cita en la clínica, y casi una tercera parte de ellas había investigado el misoprostol para uso domiciliario. Las mujeres están usando el internet para acceder a la información sobre el misoprostol para la autoinducción del aborto. A medida que aumentan las barreras al aborto legal, es posible que las mujeres sean más propensas a autoinducir el aborto.
Introduction
Increasing numbers of laws restricting abortion access, aimed at distancing women from the right to abortion, have been passed in the United States, including 334 restrictions from 2010 to 2016.Citation1 Currently, nearly half of all states are hostile to abortion rights (with greater than four major abortion restrictions in place) and only 20% of women live in a state supportive of abortion rights.Citation1 These abortion restrictions have driven some women to engage in unsafe, self-induced abortions similar to what occurred prior to legalisation of abortion in the United States in 1973.Citation2,Citation3
Misoprostol has been studied as a single agent for a medical abortion but is less efficacious than the combination of misoprostol and mifepristone when compared for use for medical abortion prior to 63 days gestation.Citation4,Citation5 The current standard, and the Food and Drug Administration approved regimen for medical abortion, is 200 mg mifepristone followed in 24–48 hours by 800 mcg misoprostol.Citation6 Even prior to the availability of medical abortion in the US, an urban study demonstrated that 37% of women were aware of misoprostol and its use as an abortifacient.Citation7 Due to its efficacy and over-the-counter availability in many countries, misoprostol used alone has become a common agent for self-induction worldwide.Citation8–10
In a 2009 US national survey of women at abortion clinics, 1.7% of women reported attempting self-induction by ingesting herbs or medications, and another 1.2% of women used misoprostol to self-induce abortion.Citation11 A study in Texas noted that 1–4% of women attempted self-induction.Citation8 Rates reach 7.4% in countries where abortion is legally restricted, such as in Brazil, where abortion is restricted to cases of rape or threat to maternal life, and in Saudi Arabia, where parental or spousal consent is required.Citation9,Citation12 The data also suggest that immigrants from countries with heavily restricted abortion access know more about misoprostol and its use as an abortifacient.Citation13
There is good evidence on the safety of using misoprostol and mifepristone for medical abortion with established telemedicine models, including video conferencing, demonstrated by the success of Planned Parenthood in Iowa, as well as online telemedicine use by Women on Web in Ireland. Both demonstrate similar rates in complications of medical abortion in a clinic setting.Citation14,Citation15 Additionally, in Australia, where mifepristone is now available by prescription in pharmacies, but where medical abortion has been uncommon, a foundation provides the medications to patients by mail after verifying the pregnancy and performing counselling over the phone.Citation16 However, safety is not ensured when the source of the medication and instructions provided are questionable.
Given the volume of anti-abortion legislation that has been successfully enacted in the US within recent years, including waiting periods, gestational age limits, building requirements that current clinics cannot support and physician admitting privileges, all of which have caused numerous clinics to close, we suspect that women are left in a position where abortion with a physician is becoming inaccessible. However, there is no specific data in the Midwest US on this phenomenon despite it being an area with increasing restrictions, but with fewer immigrants and less access to medications from other countries, such as were present in the studies above. Overall, self-sourced abortion is an area with many research gaps, including regarding women’s experiences and desires surrounding this practice.Citation10 Our objective was to identify if there is a trend in increasing women’s investigation of, or actual, self-termination; and if so, how women obtain this information. In addition, we investigated how women would react to the potential availability of medical abortion without a provider, especially with misoprostol since it is inexpensive and has been found to be readily available globally. We particularly focused on the availability of information online, since the dissemination of information via the Internet is common and relieves women of many of the barriers they face accessing typical care. Awareness of a practice taking place outside the traditional realm, with associated potential medical implications, is necessary for women’s healthcare providers and for policymakers.
Materials and methods
We developed a survey to investigate age, race, marital status, educational status, income, gravidity, parity, maternal estimation of gestational age and actual gestational age measured by ultrasound, money spent to obtain an abortion excluding medical fees, and distance travelled. The survey asked questions on women’s position on abortion rights, familiarity with misoprostol as an abortifacient, how information about abortion care and misoprostol was obtained, and barriers to care. The first 16 questions were about demographics and pregnancy history, followed by seven questions about the investigation of misoprostol online and use of misoprostol in past and present pregnancies, and six questions about barriers to care and whether a hypothetical alternative of over the counter misoprostol would be acceptable. The survey was comprised of multiple choice questions, some of which allowed multiple responses. There were also a few options to write in responses if the multiple choices did not include their response. Questions were developed by the study authors as no validated study about self-induced abortion was available. The survey was available in English and validated for readability and easy language level by a third party in the College of Public Health with expertise in survey design.
Following the University of Iowa Institutional Review Board approval, survey administration commenced at three non-profit independent reproductive health clinics, identifying all women presenting for medical or surgical abortion procedures. The maximum gestational age for procedures was 21 weeks, confirmed by ultrasound. Women presenting for induced abortions were included. Women under the age of 18 years, currently incarcerated, or not proficient in English, were excluded. A letter containing elements of consent was provided to women by a research assistant prior to or following their abortion procedure, while in the recovery room. Subjects completed the survey either on paper or computer tablet. Surveys were returned to a secure box with the research assistant whether completed or not, in order to maintain confidentiality. No compensation was provided.
Study data were collected and managed using REDCap (Research Electronic Data Capture) secure, web-based, electronic data capture tools hosted by the University of Iowa Institute of Clinical and Translational Science,Citation17 supported by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) programme, grant U54TR001356. Statistical analysis was done using SAS version 9.3 (SAS Institute Inc. Base SAS®, Cary, NC, USA). Descriptive statistics included means and percentages. Test of symmetry was used to assess change for the variables with ≥3 nominal response categories. A statistically significant result was defined as p-value <.05. Comparisons between subject groups utilized Pearson-Chi square tests for categorical variables and Wilcoxon-Rank Sum for ordinal data.
Results
From June through September 2016, 437 women obtained abortions and 276 (63.2%) completed the questionnaire. Demographic data is included in , with 228 (90.1%) at less than 14 weeks gestation. Response rates to individual questions varied and denominators are therefore noted. Gestational age averaged 8.4 weeks by patient estimate and 8.7 weeks by ultrasound dating (p = .12) with a median of 8 weeks gestation for both groups. However, the mean difference in a single participant’s estimate was 0.91 weeks. Most respondents (191 of 256 [74.6%]) investigated misoprostol and other abortion options online. Of the 188 women who specified how they investigated online, 58 (30.9%) reported investigating misoprostol self-sourced online for home use. Women who investigated misoprostol online were less likely to have had a prior abortion (29.3% vs. 63.1%, p < .01) and more likely to report prior home attempts to end this pregnancy (8.6% vs. 0%, p = .049) (). Over one-third of women (97 [36.2%]) had had a prior abortion. Overall, four (1.6%) respondents purchased misoprostol, one from a store, one from a clinic, and two who had purchased it from outside the United States.
Table 1. Demographic data of women presenting to abortion clinics in the Midwest participating in a survey on self-sourcing abortion (N = 276)
Table 2. Comparison of those that did not investigate online prior to appointment versus each of the two groups that investigated online in terms of abortion experiences and preferences for an over the counter option for abortion (OTC = over the counter, DIY = do it yourself)
Prior to coming to the clinic, 11 of 252 women (4.4%) tried to end their pregnancy, 3 (1.2%) with a medication. There were 17 instances reported of trying to end a pregnancy in the current pregnancy, or in a prior pregnancy with a variety of means, including Vitamin C, black cohosh (an herbal remedy), dong quai (a medicinal herb), and other herbal remedies, although these may include overlap of a single woman trying multiple methods. Nine of 258 women (3.5%) reported that they had a friend who used misoprostol for abortion at home.
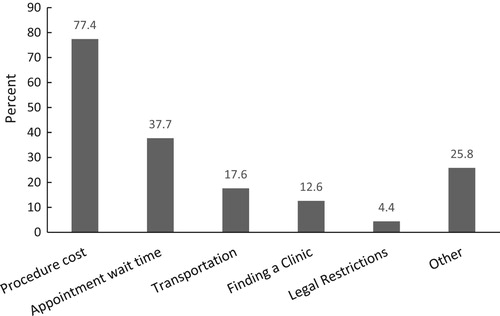
In total, 163 of 251 (64%) women reported barriers to care including those in , as well as considerations including childcare and time off work. If these barriers were removed, 110 of 152 (72.4%) respondents reported that they could have presented to care more than one week earlier. This is further demonstrated as women who reported barriers to care presented at a mean gestational age of 8.6 weeks and those without barriers presented at a mean of 7.6 weeks (p = .03). Women who reported barriers to care had higher out of pocket expenses ($412 vs. $260, p = .01) but were similar in terms of race, income, highest level of education, parity, and history of prior abortion. There was also no difference in numbers of women who looked online or found information on misoprostol between those who did and did not report barriers to care.
Figure 1. Barriers to accessing abortion care cited by women undergoing abortions in the Midwest between May to September 2016. 159 (64.9%) of all women reported barriers to care, denoted below. Women were able to choose all applicable categories
Respondents were of the opinion that an over-the-counter option would have improved access to care in 128/240 (53.3%) of respondents’ opinions. If a safe, over-the-counter abortion option were available, 80/242 (33.0%) reported they would be comfortable trying it and 82/240 (34.2%) would likely use it with a future unwanted pregnancy. Those who had looked online for misoprostol tended towards being more comfortable with a theoretical safe over-the-counter abortion option than those not looking online (42.6% vs. 28.1%, p = .19).
Discussion
The public health successes of abortion legalisation in the US remain tenuous in the current political and healthcare environment where self-induction is re-emerging.Citation18 With barriers that eliminate access to standard abortion providers and procedures, the use of misoprostol self-administration without a provider has proven to be a safe and efficacious alternative.Citation15,Citation19
Our study shows that women in a rural Midwestern state are aware of and investigate these options. The rate of 1.6% of women who bought misoprostol before the presentation is similar to rates reported previously.Citation8,Citation11 However, at the time the survey was administered, state law was fairly permissive regarding abortion access. Follow-up studies are needed to determine if increasing restrictions and closure of several clinics will increase self-induction rates. The use of misoprostol is likely to be more widespread than our study and similar previous studies suggest, given that it only encompasses women accessing abortion services. Those who obtained misoprostol illicitly and succeeded in self-termination would not likely access clinic care. Given the efficacy of single-agent misoprostol regimens of 76%,Citation4,Citation5 the four patients who obtained misoprostol prior to coming in may represent a much larger group who obtained misoprostol and never presented to care or had used misoprostol solely because they could not access an in-clinic abortion. The inability to capture the full number of those using misoprostol is a major limitation of our study and other studies which are limited to an abortion clinic setting, introducing participation bias. Another limitation is that we only surveyed English-speaking patients; it is estimated that less than 10% of those who did not participate were because of a language barrier, consistent with the typical patient population at the study clinics. Anecdotally, lower response rates were noted on days when study personnel were unavailable, and the survey was given by clinic staff only.
Women who sought information about misoprostol online were less likely to have had a previous abortion than those who had not looked online and were also more interested in the potential for the availability of over-the-counter options for abortion. This indicates those with a prior termination possess knowledge about the abortion clinic process and are less likely to seek out other options.
This study demonstrates that women investigate and are knowledgeable of means to end pregnancies other than physician supervised abortions. As women gain knowledge of self-induction, demand for self-sourced abortion medication as well as high-quality information, such as what is provided by the Plan C organisation (http://plancpills.org), Women on Web (https://www.womenonweb.org/), or Safe2Choose (https://safe2choose.org/), will likely increase. Given the studied safety and efficacy of medical abortion regimens, this is an opportunity to increase access to safe abortion, but it also raises questions about the safety of taking medications that may not be from regulated sources, the ability of women to estimate gestational age, and the complications that could arise without proper instructions. Studies on online instructions, label comprehension, complication rates, and actual use are needed to guide women who are unable or unwilling to seek traditional abortion services to provide the care they need in a safe environment with legitimate medications and evidence-based protocols.Citation20 In addition, ensuring that information necessary to find a clinic with abortion services is readily available online is necessary, since that is a primary source where women get their information. While maintaining access to family planning services is essential to ensure women’s safety, this study demonstrates that non-traditional methods of abortion cannot be ignored as part of women’s reproductive health care.
Acknowledgements
The authors would like to thank Bridget Zimmerman, PhD for assistance with data analysis. The authors also wish to thank the Emma Goldman Clinic and Planned Parenthood of the Heartland for allowing us to conduct this survey at their clinical sites. This work was presented at the National Abortion Federation 41st Annual Meeting; Montréal, Québec, 24 April, 2017.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Courtney Kerestes http://orcid.org/0000-0002-2243-8068
Colleen K Stockdale http://orcid.org/0000-0003-0074-3261
Abbey J Hardy-Fairbanks http://orcid.org/0000-0003-4041-3937
Additional information
Funding
References
- Nash E, Gold RB, Ansari-Thomas Z, et al. Policy Trends in the States:2016: Guttmacher Institute; 2017 [updated 2017 Jan 3; cited 2017 Mar 16]. Available from: https://www.guttmacher.org/article/2017/01/policy-trends-states-2016.
- Coles MS, Koenigs LP. Self-induced medical abortion in an adolescent. J Pediatr Adolesc Gynecol. 2007 Apr;20(2):93–5. PubMed PMID: 17418393 doi: 10.1016/j.jpag.2006.10.015
- Kerestes C, Sheets K, Stockdale C, et al. Prevalence, attitudes and knowledge of misoprostol for self-induction of abortion in women presenting for abortion at reproductive health clinics. Contraception. 2017;95(5):517–518. doi: 10.1016/j.contraception.2017.02.012
- Ngoc NT, Blum J, Raghavan S, et al. Comparing two early medical abortion regimens: mifepristone + misoprostol vs. misoprostol alone. Contraception. 2011 May;83(5):410–417. PubMed PMID: 21477682. doi: 10.1016/j.contraception.2010.09.002
- Jain JK, Dutton C, Harwood B, et al. A prospective randomized, double-blinded, placebo-controlled trial comparing mifepristone and vaginal misoprostol to vaginal misoprostol alone for elective termination of early pregnancy. Hum Reprod. 2002 Jun;17(6):1477–1482. PubMed PMID: 12042265. doi: 10.1093/humrep/17.6.1477
- FDA. Mifeprex® (mifepristone) tablets [drug insert]. New York (NY): Danco Laboratories; 2016.
- Rosing MA, Archbald CD. The knowledge, acceptability, and use of misoprostol for self-induced medical abortion in an urban US population. JAMWA. 2000;55(S)(3 Suppl):S183–S185. PubMed PMID: 10846334.
- Fuentes L, Grossman D. Knowledge, opinion, and experience related to abortion self-induction in Texas. Texas Policy Evaluation Project Research Brief. 2015.
- Costa SH. Commercial availability of misoprostol and induced abortion in Brazil. Int J Gynaecol Obstet. 1998 Dec;63(Suppl 1):S131–S139. PubMed PMID: 10075223. doi: 10.1016/S0020-7292(98)00195-7
- Kapp N, Blanchard K, Coast E, et al. Developing a forward-looking agenda and methodologies for research of self-use of medical abortion. Contraception. 2018/02/01/;97(2):184–188. doi: 10.1016/j.contraception.2017.09.007
- Jones RK. How commonly do US abortion patients report attempts to self-induce? Am J Obstet Gynecol. 2011 Jan;204(1):23.e1–23.e4. PubMed PMID: 20863478. doi: 10.1016/j.ajog.2010.08.019
- Alsibiani SA. Use of misoprostol for self-induced medical abortions among Saudi women: a call for attention. Gynecol Obstet Invest. 2014;78(2):88–93. PubMed PMID: 24993350. doi: 10.1159/000363238
- Grossman D, Holt K, Pena M, et al. Self-induction of abortion among women in the United States. Reprod Health Matters. 2010 Nov;18(36):136–146. PubMed PMID: 21111358. doi: 10.1016/S0968-8080(10)36534-7
- Grossman D, Grindlay K. Safety of medical abortion provided through telemedicine compared with in person. Obstet Gynecol. 2017 Oct;130(4):778–782. PubMed PMID: 28885427; eng. doi: 10.1097/AOG.0000000000002212
- Aiken ARA, Digol I, Trussell J, et al. Self reported outcomes and adverse events after medical abortion through online telemedicine: population based study in the Republic of Ireland and Northern Ireland. Br Med J. 2017 May;357:j2011. PubMed PMID: 28512085. doi: 10.1136/bmj.j2011
- Hyland P, Raymond EG, Chong E. A direct-to-patient telemedicine abortion service in Australia: Retrospective analysis of the first 18 months. Aust N Z J Obstet Gynaecol. 2018 Mar. PubMed PMID: 29603139; eng.
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–381. PubMed PMID: 18929686; PubMed Central PMCID: PMCPMC2700030. doi: 10.1016/j.jbi.2008.08.010
- Kelly M. Legalized abortion: a public health success story. Reprod Freedom News. 1999 Jun;8(6):7. PubMed PMID: 12295140.
- Briozzo L, Vidiella G, Rodriguez F, et al. A risk reduction strategy to prevent maternal deaths associated with unsafe abortion. Int J Gynaecol Obstet. 2006 Nov;95(2):221–226. PubMed PMID: 17010348. doi: 10.1016/j.ijgo.2006.07.013
- Kapp N, Grossman D, Jackson E, et al. A research agenda for moving early medical pregnancy termination over the counter. BJOG. 2017 Oct;124(11):1646–1652. PubMed PMID: 28317327; eng. doi: 10.1111/1471-0528.14646
