Abstract
The psychological, behavioral and psychosocial implications of self-control are well established, but relatively little is known about its implications for physical health. This study examined the association between self-control and two important indicators of cardiovascular risk: morning blood pressure surge (MBPS) and maximum oxygen consumption (VO2max). Undergraduate students (N = 78) completed a measure of dispositional self-control (Brief Self-Control Scale), participated in a 24-h ambulatory assessment of heart rate (HR) and blood pressure (BP), and completed the YMCA Cycle Ergometer Submaximal Test. Regression analyzes yielded a significant positive relationship between self-control and VO2max. Results also indicated a significant negative association between self-control and MBPS, independent of average 24-h blood pressure and VO2max scores. These findings expand our understanding of the relationship between dispositional self-control and MBPS. Study limitations and directions for future research are discussed.
Introduction
The personal and social implications of self-control, or the capacity to override immediate impulsive thoughts, emotions, or behaviors for a delayed and more desirable outcome, are well established (Baumeister & Heatherton, Citation1996; de Ridder et al., Citation2012). For example, individuals with high dispositional self-control experience a range of benefits including improved interpersonal functioning, affect regulation, and overall psychological well-being (Finkel & Campbel, Citation2001; Tangney et al., Citation2004). Conversely, those with low dispositional self-control are at a higher risk for obesity (Lili, Citation2014) and more likely to engage in deleterious health behaviors such as substance use and problem drinking (Moffitt et al., Citation2011). As research has focused on behavioral and psychosocial outcomes of self-control relatively little is known regarding its impact on physiological functioning and physical health.
One response to the deficit just noted is the emergence of research on self-control and cardiovascular functioning. Specifically, high dispositional self-control has been related to lower laboratory heart rate (HR) and improved ambulatory HR variability (HRV) (Beute & de Kort, Citation2014; Daly et al., Citation2014; Segerstrom & Nes, Citation2007). However, lack of ambulatory hemodynamic assessments and issues of replication cast doubt on some of the findings (for replication failure see Reynard et al., Citation2011). Given that cardiovascular disease is the leading cause of death in the US and globally (Miniño et al., Citation2007), continued examination of self-control and cardiovascular functioning is critical.
Independent of average 24-h blood pressure (BP), morning variation in BP has been linked to the occurrence of cardiovascular events (Gosse & Schumacher, Citation2006; Kario, Citation2010; Manfredini et al., Citation2003). As an indicator of the natural morning diurnal peak in BP, morning BP surge (MBPS) has been suspected to play an important role in the pathophysiologic relationship between hemodynamic alterations and various indicators of cardiovascular risk and damage (Kario & White, Citation2008; Kario, Citation2007; Kario, Citation2010; Kario, Citation2015; Kario, Citation2016; Sheppard et al., Citation2015; White, Citation2010). For example, research indicates that circadian variation characterized by MBPS predicts occurrence of ischemic and hemorrhagic stroke in both hypertensive and normotensive patients (Casetta et al., Citation2002a,Citationb). Thus as the majority of acute adverse cardiac events occur in the morning hours; a greater understanding of factors associated with MBPS will have important clinical implications in the development of therapeutic targets for preventing cardiovascular complications (Morris et al., Citation2016; Sheppard et al., Citation2015). Despite the demonstrated link between self-control and improved cardiovascular functioning in laboratory settings, few studies assess ambulatory BP or demonstrate a relationship to diurnal variation in hemodynamic functioning.
Considering the link between self-control and exercise effort, planning and decision-making (Martin Ginis & Bray, Citation2010) as well as the established relationship between exercise and cardiovascular health, research is also needed to understand the connection between self-control and cardiovascular health via fitness indicators. One common indicator of cardiorespiratory fitness and a key measurement in predicting all-cause mortality is maximal oxygen consumption (VO2max) (Myers et al., Citation2000; Wei et al., Citation1999). Despite clear evidence demonstrating the importance of VO2max and MBPS as indicators of cardiovascular risk, their relationship in the context of self-control have yet to be examined.
Therefore, the present study seeks to examine the link between self-control and indicators of cardiovascular health (VO2max, MBPS). It is hypothesized that self-control is related negatively to ambulatory measures of HR, BP, and MBPS and positively to VO2max. Specifically, those with high dispositional self-control will demonstrate lower HR and BP values, fewer exaggerated MBPS peaks, and greater cardiorespiratory fitness. Furthermore, in a supplemental analysis, the role of cardiovascular fitness (VO2max) in accounting for (mediating) the relationship between self-control and morning surge was explored.
Methods
Participants
Seventy-eight undergraduate students (85% female, Mage = 20.56 years, SD = 2.53, Mheight = 161.84 cm, SD = 6.45, Mweight = 62.14 kg, SD = 9.21, 87% Caucasian) qualified for study inclusion. To exclude confounds related to cardiovascular functioning, participants were excluded from study participation through an online health-screening assessment if they smoked, exercised regularly (>120 min per week) in the previous 6 months (as cardiorespiratory fitness is an independent predictor of cardiovascular mortality and hence a confounder of cardiac functioning (Blair et al., Citation1996; Denham et al., Citation2016; Ramos et al., Citation2016) and (May et al., Citation2016a,Citationb), were hypertensive (BP >140/90 mmHg), had chronic diseases, or were taking β-blockers, antidepressants or stimulants. The participants were asked to abstain from caffeine, alcohol and strenuous physical activity 24 h prior to the testing period and during the assessment period. The female participants were tested in the early follicular phase of the menstrual cycle to avoid potential variations in pressure wave morphology and cardiac reactivity (Lustyk et al., Citation2012). The participants were recruited from undergraduate classrooms as an option for voluntary class credit and all the data were collected in the middle (weeks 3–9) of the semester. All the participants gave their written consent prior to study participation as approved by The Florida State University Institutional Review Board.
Measures
Self-control
The Brief Self-Control Scale, an abbreviated measure of the Self-Control Scale (BSCS; Tangney et al., Citation2004) was used to measure dispositional self-control. The BSCS consists of 13-items which assess self-control in five domains: controlling thoughts, controlling emotions, controlling impulses, regulating behavior and/or performance, and habit breaking. Scores on each item ranging from 1 (not at all like me) to 5 (very much like me) with higher scores indicating greater dispositional self-control. In the present sample coefficient α was .91.
YMCA cycle ergometer submaximal test
This submaximal cardiorespiratory fitness test makes use of the temporal linear relationship between cardiac output and oxygen consumption to calculate maximum oxygen consumption (VO2max; Garatachea et al., Citation2007). Briefly, participants start off at a specific bike resistance (828E Monark Cycle Ergomedic Test Cycle; Vansbro, Sweden) determined by their resting HR. HR was obtained by means of a validated wireless monitor (Polar 800CX; Polar Electro OY, Kempele, Finland) with a strap placed around the thoracic area at the level of the xyphoid process of the sternum (Nunan et al., Citation2009). The resistance is increased in stages in accordance with the participants rising HR. Prior to the increase of resistance, a steady state HR is ensured to maintain the relationship between cardiac output and oxygen consumption. When the participant’s HR reached 85% of their age predicted max HR the test was terminated. VO2max calculations were derived based on equations provided by the Canadian Society for Exercise Physiology (Canadian Society for Exercise Physiology, Citation2010).
Ambulatory monitoring
Ambulatory HR and BP measurements were collected using validated oscillometric 90217A SpaceLabs (Spacelabs; Wokingham, Berkshire, UK) recorders as described in prior studies from our laboratories (see May et al., Citation2014a,Citationb). Devices were calibrated to take four measurements per hour for 24 h. Waking and sleeping times were defined by self-report. Following Kario (Citation2010), MBPS was defined as a sleep-trough surge and calculated as morning BP (2 h BP average composed of 8 BP readings conducted immediately after wake-up time) minus the lowest nocturnal BP (1 h BP average composed of 4 BP readings centered around the lowest nighttime reading).
Procedure
The participants first completed measurement scales (BSCS and exclusion criteria questions) online. The qualifying participants were then scheduled for a laboratory appointment to complete a 24 h ambulatory HR and BP measurement. During the laboratory appointment, anthropometric measurements (including height and weight) were taken and participants were fitted with an ambulatory BP monitoring device. Ambulatory monitoring began between 0800 and 1000 h and concluded when the device was returned to the laboratory the following day. Directly following the ambulatory monitoring device return, participants completed the YMCA sub max ergometer test via a bike task. Following this test, the participants were thanked, debriefed and dismissed.
Statistical analysis
Pearson correlations evaluated measurement scale and physiological associations. Hierarchical multiple regression (HMR) analyses were conducted to test the association between self-control scores, fitness scores (VO2max), average 24 h HR and BP scores, and MBPS scores. HMR analyses are also able to demonstrate any incremental contribution of self-control scores above fitness scores and average 24-h BP scores in accounting for variance in MBPS scores. Model 1 of the HMR contained the VO2max and the average 24-h BP predictors and Model 2 introduced self-control as a predictor. Two separate HMR analyses were conducted, one for each surge outcome (systolic MBPS and diastolic MBPS). Follow-up analyses categorized participants into surge quartiles and utilized univariate analysis of variance (ANOVA) to examine differences in self-control scores between surge quartiles. All regression and ANOVA statistical analyses were performed using IBM SPSS version 20 (Chicago, IL). Mediation modeling was performed using Mplus Version 7.3 (Los Angeles, CA: Muthén & Muthén) to test the indirect effects (bootstrapped with 5000 samples) between self-control and outcome variables (systolic MBPS and diastolic MBPS) via VO2max.
Results
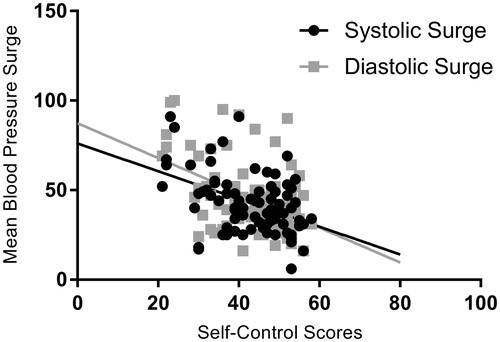
Pearson correlations demonstrated significant negative associations (p < .05) between self-control scores and average 24-h ambulatory HR (r = −.27), systolic MBPS (r = −.43), and diastolic MBPS (r = −.45) values. Additionally, V02max was positively related to self-control scores (r = .20) and negatively related to average 24 hour ambulatory HR (r = −.20), average 24-h ambulatory systolic BP (r = −.24) and diastolic BP (r = −.22) scores. Of note, average 24-h ambulatory systolic BP (r = −.04) and diastolic BP (r = −.09) scores were not statistically related to self-control scores. See for descriptive statistics and correlation matrix.
Table 1. Means, standard deviations and correlations among study variables.
After controlling for average 24-h BP and VO2max, the HMR analyses showed that self-control was significantly negatively related to systolic MBPS (B = −.98) and diastolic MBPS (B = −1.23, see for the HMR analyses). Specifically, self-control independently predicted an additional 24% of variance in systolic MBPS scores, ΔF(1, 73) = 11.89, p < .001, and 25% in diastolic MBPS scores, ΔF(1, 73) = 12.23, p < .001 (). The exploratory mediation analyses yielded null findings: VO2max did not account for the relationship between self-control and surge values, with non-significant indirect effects on systolic MBPS (β = −.12, p = .707) and diastolic MBPS (β = −.16, p = .534).
Table 2. Hierarchical multiple regression analyses of morning blood pressure surge indices.
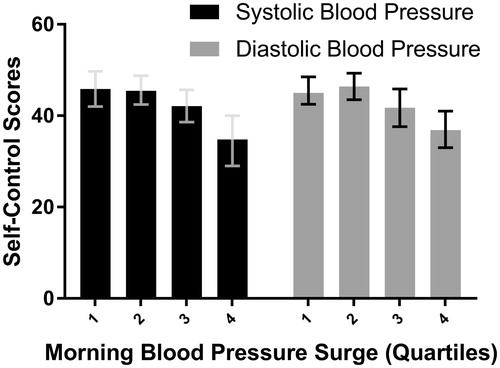
For the follow-up quartile analyses, the division points for the four quartiles for systolic MBPS were 31.00, 41.00, and 51.75. The division points for the four quartiles for diastolic MBPS were 30.25, 42.00, and 52.00. Univariate ANOVA analyses indicated significant differences in self-control scores between systolic MBPS quartiles, F(3, 74) = 5.16, p = .003, partial η2 = .169, as well as between the diastolic MBPS quartiles, F(3, 74) = 4.49, p = .006, partial η2 = .151. Post-hoc comparisons with Bonferroni alpha corrections indicated quartiles 1 and 2 to be significantly different (p < .05) in self-control scores from quartile 4 for both systolic and diastolic MBPS quartiles (see for post-hoc MBPS quartile comparisons).
Discussion
Extant research on self-control shows that it is implicated in a multitude of personal and social behaviors (Baumeister et al., Citation1994; de Ridder et al., Citation2012; Tangney et al., Citation2004). However, relatively little is known about how self-control is related to physiology and physical health. The present study therefore examined the relationship between dispositional self-control, cardiovascular functioning, and fitness as measured by ambulatory HR, BP, MBPS and VO2max. The novel findings of the present study are consistent with our hypotheses; individuals with high dispositional self-control exhibited higher VO2max during an exercise task as well as lower MBPS over a 24-h ambulatory assessment, independent of average 24-h BP and VO2max. Conversely, those with low-dispositional self-control displayed higher averages of MBPS and poorer VO2max. Mediation analyses, however, failed to indicate that VO2max accounts for the relationship between self-control and surge values.
The current study also identified a novel relationship between ambulatory HR and self-control scores (as opposed to the null ambulatory HR to self-control relationship reported in Daly et al. (Citation2014)). Unfortunately, Daly et al. (Citation2014) do not report ambulatory BP correlations with self-control indices. This precludes a comparison with the current study’s result which were unable to establish a relationship between self-control and average 24-h BP.
The study is also relevant to the debate concerning the analysis of surge data in the MBPS literature. Although the current data fit a linear model and demonstrate a linear relationship between self-control scores and MBPS values, they also provide some support for use of thresholds (cutoff limits or endpoints) for potentially problematic MBPS values, at least for psychosocial (i.e. self-control) risk factors. For both systolic and diastolic MBPS, self-control scores in the fourth quartile were markedly lower. There appears to be active disagreement as to whether predetermined thresholds of MBPS are appropriate for reliable prediction of cardiovascular events. For example, Sheppard et al. (Citation2015) demonstrate via meta-analytic methods, that only through measurement and analysis as a continuous variable were increased levels of MBPS associated with increased risk of stroke (as no relationship was demonstrated between MBPS and cardiovascular events when MBPS was defined and analyzed using predetermined thresholds). Sheppard et al. (Citation2015) note the dangers of attenuated relationships and the loss of statistical power through use of predetermined thresholds. In contrast, Kario (Citation2015, p. 8) provides evidence and argues that both extremes (the absence of MBPS or/negative MBPS values as well as exaggerated MBPS values) may be pathological and “identification of pathological thresholds of MBPS is clinically important”. Continued refinement of the operational definition of MBPS (seven different definitions of MBPS were identified in Sheppard et al. (Citation2015)) as well as further examination of MBPS distributions in relation to specific outcomes (both psychosocial and physical) in future work may help clarify the aforementioned issue of threshold utility.
In regards to theoretical expansion, the conceptual link between self-control and MBPS potentially lies in their relationships with stress; high levels of psychological stress have been associated with exaggerated MBPS (Kario et al., Citation2002) and self-control is conceptualized as the capacity to manage stress via the inhibition of impulsive responses (Baumeister & Heatherton, Citation1996; Tangney et al., Citation2004). Under the self-regulatory strength model of self-control, the strength to inhibit immediate impulsive thoughts, behaviors and emotions is contingent upon a finite cognitive resource. Such resources diminish as self-control is employed, reducing the strength or capacity to manage stress in subsequent situations (Baumeister & Heatherton, Citation1996; Baumeister et al., Citation1998; Cheung et al., Citation2014). Thus, low levels of self-control make it more likely that an individual will accrue greater stress which can potentially lead to increases in MBPS.
In a complementary manner, the relationship between self-control and MBPS can also potentially be understood via their link to the autonomic nervous system (ANS). Self-regulatory processes, such as inhibiting impulsive behaviors, are said to share neural networks in the prefrontal cortex that are analogous to the central autonomic network which directly influences parasympathetic input to the HR (Ahern et al., Citation2001; Segerstrom & Nes, Citation2007). Moreover, in a rare study examining self-control and HRV, a measure of ANS activity, HRV was suggested to serve as an index of self-regulatory strength and effort (Segerstrom & Nes, Citation2007). While HRV can reflect aspects of sympathetic activity, MBPS serves as one outcome of activity in the sympathetic nervous system (Lambert et al., Citation2014) and is an independent predictor of cardiovascular risk (Kario et al., Citation2003; Kario, Citation2010). Specifically, the increase in vascular tone within the arteries as a result of increased sympathetic activity potentially influences surges in morning BP (Kario, Citation2010; Panza et al., Citation1991). Although sympathetic activity is well established as a mechanism of change in BP (Grassi et al., Citation2010), factors such as vascular disease (i.e., arterial stiffness) as well as determinants of total peripheral resistance (e.g. blood vessel diameter, blood viscosity, coagulation) have also been shown to influence BP (Guyton & Hall, Citation1996; Kario, Citation2010). Future research examining the relationship between self-control and BP should take into account such confounds (e.g. vascular disease and determinates of total peripheral resistance).
Another indicator of cardiovascular functioning relatively unexplored in the self-control literature is VO2max. VO2max, or maximum oxygen consumption during aerobic activity, is considered the gold-standard measure of cardiorespiratory fitness and is a vital measure in predicting heart failure (Hyde & Gengenbach, Citation2007; Myers et al., Citation2000). Findings from the present study demonstrate a significant positive association between levels of dispositional self-control and VO2max. Their link can be explained by self-control’s relationship to physical exercise. Specifically, higher VO2max is indicative of greater physical fitness which can be achieved via exercise training (Bouchard et al., Citation1999) and previous research has established that adherence to training requires a substantial amount of self-control effort (Bandura, Citation2005). Therefore, it is possible that individuals with low levels of dispositional self-control lack the resources needed to adhere to an exercise training regimen (Martin Ginis & Bray, Citation2010), further leading to poorer cardiovascular health. Although a significant relationship was found between self-control scores and VO2max, mediation analyses failed to indicate VO2max as a statistically significant mediator. It is possible that the exercise exclusion criterion in this study (i.e. exercised more than 120 min per week in the previous 6 months) reduced variability in self-control and VO2max scores (as self-control may impact aerobic capacity through adherence to exercise regimens) reducing the indirect effect. While the mediation analysis in this research was supplementary and not the main focus of this research, future research directly testing hypothesized mediational relationships with less restrictive exercise criteria may be of interest.
Overall findings from the current study linking self-control to indicators of cardiovascular functioning (MBPS, VO2max) have potentially profound clinical implications as physiological indicators are vital in providing us an understanding of biological processes, risk prediction and disease progression (Mayeux, Citation2008). In the self-regulatory strength model of self-control, self-control functions like a muscle such that our capacity to inhibit impulsive thoughts, behaviors and emotions can be strengthened through self-control exercises (Baumeister & Heatherton, Citation1996). For example, Muraven (Citation2010) demonstrated that practicing inhibition for two weeks, via squeezing a hand-grip exercise and using the non-dominant hand to complete everyday tasks (i.e. opening doors, brushing teeth), led to significant improvements in laboratory self-control assessments. In fact, self-control interventions have been effective at improving psychosocial (Finkel et al., Citation2009; Houben et al., Citation2011; Oaten & Cheng, Citation2006) and some physiological outcomes (Beute & de Kort, Citation2014; Bray et al., Citation2008; Daly et al., Citation2014). Thus extant research, along with the current findings, suggests that prospective research aimed at improving cardiovascular functioning via self-control interventions may be practical and effective. Self-control may then serve as a viable point of intervention for improving biological processes and disease progression associated with cardiovascular functioning.
It should be noted that the current study is not without limitations. First, use of a cross-sectional design restricts our ability to infer causality. Future studies are needed to examine the exact nature of the casual relationship between self-control and cardiovascular indicators as well as the effects of self-control exercises on cardiovascular functioning. Experimental research aimed at manipulating self-control (for example, either by decreasing self-control through the mechanism of ego depletion or through increasing self-control via training mechanisms such as hand-grip exercises) are promising methodologies for evaluation of causal inferences. In addition, our ability to extend our findings in regards to sex, age and cultural differences is limited by the use of a sample predominately made up of young adult Caucasian females. Previous research examining self-control, VO2max, and MBPS have all shown gender and age effects (Bouchard et al., Citation1999; de Ridder et al., Citation2012; Hyde & Gengenbach, Citation2007; Sun et al., Citation2009), emphasizing the importance of controlling (or modeling) for such factors in future research examining self-control and cardiovascular indicators.
Another potential study limitation is that only healthy (normotensive) subjects were used and hence the results of this study cannot be generalized to clinical (hypertensive) populations. More restrictive study eligibility requirements were adopted to preclude the complications of interpreting data that included some diseased or medicated subjects. However, morning surge is predictive of cardiovascular events even in normotensive populations (Casetta et al., Citation2002a,Citationb; Li et al., Citation2010; Metoki et al., Citation2006). The identification of a relationship between self-control and surge in a young, healthy (normotensive) sample suggests the relationship between self-control, surge and more serious cardiovascular endpoints may be more pronounced in an older, less healthy population. Thus as stated in Manfredini et al. (Citation2003), detection of pathological MBPS might be useful as MBPS may be harmful for normotensive subjects.
Furthermore, it should also be noted that while the current study reports both systolic and diastolic MBPS values in an effort to provide evidence of the robust association between BP values and self-control scores, the clinical importance of diastolic MBPS remains unclear with future research needed to identify the utility (or not) of diastolic surge values. Finally, using the self-regulatory strength model of self-control to conceptualize the relationship between self-control and cardiovascular indicators can be seen as limiting as the model recently has been subject to criticism. Previous research has suggested that self-control is a measure of motivation and attention and that the notion of a depletable resource is fictitious (Inzlicht & Schmeichel, Citation2012; Job et al., Citation2010). However, despite model revisions in response to such criticism (Beedie & Lane, Citation2012), the underlying assumption of depletion has yet to falter (Baumeister & Vohs, Citation2016).
In conclusion, the present study found dispositional self-control to be significantly associated with MBPS and VO2max. These findings make an original contribution to the literature by establishing a link between self-control and two important, well-established indicators of cardiovascular risk. Although the exact nature of their relationship is still to be determined, the current results help to further expand our understanding of the relationship between self-control and physiological biomarkers, specifically MBPS. Future research can further expand the conceptual and mechanistic conceptualizations of the relationship between self-control and cardiovascular indicators. This research can then highlight the potential benefits of self-control as a point of intervention for improving cardiovascular functioning. Thus the potential impact of interventions aimed at improving self-control in the service of improved health outcomes warrants further investigations.
Disclosure statement
The current study was unaccompanied by external funding. The authors are solely responsible for the content of the paper. All authors assert no conflict of interest.
References
- Ahern GL, Sollers JJ, Lane RD, Labiner DM, Herring AM, Weinand ME, Hutzler R, et al. (2001). Heart rate and heart rate variability changes in the intracarotid sodium amobarbital test. Epilepsia 42:912–21.
- Bandura A. (2005). The primacy of self-regulation in health promotion. Appl Psychol 54:245–54.
- Baumeister RF, Bratslavsky E, Muraven M, Tice DM. (1998). Ego depletion: Is the active self a limited resource? J Pers Soc Psychol 74:1252–65.
- Baumeister RF, Heatherton TF. (1996). Self-regulation failure: an overview. Psychol Inq 7:1–15.
- Baumeister RF, Heatherton TF, Tice DM. (1994). Losing control: how and why people fail at self-regulation. San Diego, CA: Academic Press, Inc.
- Baumeister RF, Vohs KD. (2016). Strength model of self-regulation as limited resource: assessment, controversies, update. Adv Exp Soc Psychol 54:67–127.
- Beedie CJ, Lane AM. (2012). The role of glucose in self-control: another look at the evidence and analternative conceptualization. Personal Social Psychol Rev 16:143–53.
- Beute F, de Kort YA. (2014). Natural resistance: exposure to nature and self-regulation, mood, and physiology after ego-depletion. J Environ Psychol 40:167–78.
- Blair SN, Kampert JB, Kohl HW, Barlow CE, Macera CA, Paffenbarger RS, Gibbons LW. (1996). Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA 276:205–10.
- Bouchard C, An P, Rice T, Skinner JS, Wilmore JH, Gagnon J, Pérusse L, et al. (1999). Familial aggregation of VO(2max) response to exercise training: results from the HERITAGE Family Study. J Appl Physiol 87:1003–8.
- Bray SR, Ginis KA, Hicks AL, Woodgate J. (2008). Effects of self-regulatory strength depletion on muscular performance and EMG activation. Psychophysiology 45:337–43.
- Canadian Society for Exercise Physiology. (2010). The Canadian Physical Activity, Fitness and Lifestyle Approach (CPAFLA). 3rd ed. Ottawa, CAN: Canadian Society for Exercise Physiology.
- Casetta I, Granieri E, Fallica E, la Cecilia O, Paolino E, Manfredini R. (2002a). Patient demographic and clinical features and circadian variation in onset of ischemic stroke. Arch Neurol 59:48–53.
- Casetta I, Granieri E, Portaluppi F, Manfredini R. (2002b). Circadian variability in hemorrhagic stroke. JAMA 287:1266–7.
- Cheung T, Gillebaart M, Kroese F, De Ridder D. (2014). Why are people with high self-control happier? The effect of trait self-control on happiness as mediated by regulatory focus. Front Psychol 5:722.
- Daly M, Baumeister RF, Delaney L, MacLachlan M. (2014). Self-control and its relation to emotions and psychobiology: evidence from a day reconstruction method study. J Behav Med 37:81–93.
- Denham J, Brown NJ, Tomaszewski M, Williams B, O’Brien BJ, Charchar FJ. (2016). Aortic augmentation index in endurance athletes: a role for cardiorespiratory fitness. Eur J Appl Physiol 116:1537–44.
- De Ridder DT, Lensvelt-Mulders G, Finkenauer C, Stok FM, Baumeister RF. (2012). Taking stock of self-control: a meta-analysis of how trait self-control relates to a wide range of behaviors. Personal Soc Psychol Rev 16:76–99.
- Finkel E, Campbel W. (2001). Self-control and accommodation in close relationships: an interdependence analysis. J Pers Soc Psychol 81:263–77.
- Finkel EJ, DeWall CN, Slotter EB, Oaten M, Foshee VA. (2009). Self-regulatory failure and intimate partner violence perpetration. J Pers Soc Psychol 97:483–99.
- Garatachea N, Cavalcanti E, García-López D, González-Gallego J, de Paz JA. (2007). Estimation of energy expenditure in healthy adults from the YMCA submaximal cycle ergometer test. Eval Health Prof 30:138–49.
- Gosse P, Schumacher H. (2006). Early morning blood pressure surge. J Clin Hypertens (Greenwich) 8:584–9.
- Grassi G, Bombelli M, Seravalle G, Dell’Oro R, Quarti-Trevano F. (2010). Diurnal blood pressure variation and sympathetic activity. Hypertens Res 33:381–5.
- Guyton AC, Hall JE. (1996). Textbook of medical physiology. Philadelphia, PA: W.B. Saunders Company.
- Houben K, Wiers RW, Jansen A. (2011). Getting a grip on drinking behavior: training working memory to reduce alcohol abuse. Psychol Sci 22:968–75.
- Hyde T, Gengenbach MS. (2007). Conservative management of sports injuries. 2nd ed. Sudbury, MA: Jones & Bartlett.
- Inzlicht M, Schmeichel BJ. (2012). What is ego depletion? Toward a mechanistic revision of the resource model of self-control. Perspect Psychol Sci 7:450–63.
- Job V, Dweck CS, Walton GM. (2010). Ego depletion-is it all in your head? Implicit theories about willpower affect self-regulation. Psychol Sci 21:1686–93.
- Kario K. (2016). New insight of morning blood pressure surge into the triggers of cardiovascular disease-synergistic resonance of blood pressure variability. Am J Hypertens 29:14–16.
- Kario K. (2015). Morning surge in blood pressure: a phenotype of systemic hemodynamic atherothrombotic syndrome. Am J Hypertens 28:7–9.
- Kario K. (2010). Morning surge in blood pressure and cardiovascular risk: evidence and perspectives. Hypertens 56:765–73.
- Kario K. (2007). Vascular damage in exaggerated morning surge in blood pressure. Hypertension 49:771–2.
- Kario K, Eguchi K, Hoshide S, Hoshide Y, Umeda Y, Mitsuhashi T, Shimada K. (2002). U-curve relationship between orthostatic blood pressure change and silent cerebrovascular disease in elderly hypertensives: orthostatic hypertension as a new cardiovascular risk factor. J Am Coll Cardiol 40:133–41.
- Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, et al. (2003). Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circ 107:1401–6.
- Kario K, White WB. (2008). Early morning hypertension: what does it contribute to overall cardiovascular risk assessment? J Am Soc Hypertens 2:397–402.
- Lambert EA, Chatzivlastou K, Schlaich M, Lambert G, Head GA. (2014). Morning surge in blood pressure is associated with reactivity of the sympathetic nervous system. Am J Hypertens 27:783–92.
- Li Y, Thijs L, Hansen TW, Kikuya M, Boggia J, Richart T, Metoki H, et al. (2010). International database on ambulatory blood pressure monitoring in relation to cardiovascular outcomes investigators. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertens 55:1040–8.
- Lili W. (2014). Body mass index, obesity, and self-control: a comparison of chronotypes. Soc Behav Personal 42:313–20.
- Lustyk MK, Douglas HA, Shilling EA, Woods NF. (2012). Hemodynamic and psychological responses to laboratory stressors in women: assessing the roles of menstrual cycle phase, premenstrual symptomatology, and sleep characteristics. Int J Psychophysiol 86:283–90.
- Manfredini R, Boari B, Portaluppi F. (2003). Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives. Circ 108:1401–6.
- Martin Ginis KA, Bray SR. (2010). Application of the limited strength model of self-regulation to understanding exercise effort, planning and adherence. Psychol Health 25:1147–60.
- May RW, Bamber M, Seibert GS, Sanchez-Gonzalez MA, Leonard JT, Salsbury RA, Fincham FD. (2016a). Understanding the physiology of mindfulness: aortic hemodynamics and heart rate variability. Stress 19:168–74.
- May RW, Sanchez-Gonzalez MA, Fincham FD. (2014a). School burnout: Increased sympathetic vasomotor tone and attenuated ambulatory diurnal blood pressure variability in young adult women. Stress 18:11–19.
- May RW, Sanchez-Gonzalez MA, Hawkins KA, Batchelor WB, Fincham FD. (2014b). Effect of anger and trait forgiveness on cardiovascular risk in young adult females. Am J Cardiol 114:47–52.
- May RW, Sanchez-Gonzalez MA, Seibert GS, Samaan JS, Fincham FD. (2016b). Impact of a motivated performance task on autonomic and hemodynamic cardiovascular reactivity. Stress 19:280–6.
- Mayeux R. (2008). Biomarkers: potential uses and limitations. NeuroRx 1:182–8.
- Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, Totsune K, et al. (2006). Prognostic significance for stroke of a morning pressor surge and a nocturnal blood. Hypertens 47:149–54.
- Miniño AM, Heron MP, Murphy SL, Kochanek KD. (2007). Deaths: final data for 2004. Natl Vital Stat Rep 55:1–119.
- Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, Houts R, et al. (2011). A gradient of childhood self-control predicts health, wealth, and public safety. Proc Natl Acad Sci USA 108:2693–8.
- Morris CJ, Purvis TE, Hu K, Scheer FA. (2016). Circadian misalignment increases cardiovascular disease risk factors in humans. Proc Natl Acad Sci USA 113:E1402–11.
- Muraven M. (2010). Building self-control strength: practicing self-control leads to improved self-control performance. J Exp Soc Psychol 46:465–8.
- Myers J, Gullestad L, Vagelos R, Do D, Bellin D, Ross H, Fowler MB. (2000). Cardiopulmonary exercise testing and prognosis in severe heart failure: 14 mL/kg/min revisited. Am Heart J 139:78–84.
- Nunan D, Donovan G, Jakovljevic DG, Hodges L, Sandercock G, Brodie D. (2009). Validity and reliability of short-term heart-rate variability from the Polar S810. Med Sci Sports Exerc 41:243–50.
- Oaten M, Cheng K. (2006). Longitudinal gains in self-regulation from regular physical exercise. Br J Health Psychol 11:717–33.
- Panza JA, Epstein SE, Quyyumi AA. (1991). Circadian variation in vascular tone and its relation to alpha-sympathetic vasoconstrictor activity. N Engl J Med 325:986–90.
- Ramos JS, Ramos MV, Dalleck LC, Borrani F, Walker KB, Fassett RG, Sharman JE, et al. (2016). Fitness is independently associated with central hemodynamics in metabolic syndrome. Med Sci Sports Exerc 48:1539–47.
- Reynard A, Gevirtz R, Berlow R, Milton B, Kerri B. (2011). Heart rate variability as a marker of self-regulation. Appl Psychophysiol Biofeedback 36:209–15.
- Segerstrom SC, Nes LS. (2007). Heart rate variability reflects self-regulatory strength, effort, and fatigue. Psychol Sci 18:275–81.
- Sheppard JP, Hodgkinson J, Riley R, Martin U, Bayliss S, McManus RJ. (2015). Prognostic significance of the morning blood pressure surge in clinical practice: a systematic review. Am J Hypertens 28:30–41.
- Sun N, Xi Y, Jing S, Lu X. (2009). Morning blood pressure surge varies with age and gender in hypertensive individuals. Int J Cardiol 135:272–3.
- Tangney JP, Baumeister RF, Boone AL. (2004). High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. J Personal 72:271–324.
- Wei M, Kampert JB, Barlow CE, Nichaman MZ, Gibbons LW, Paffenbarger RS Jr, Blair SN. (1999). Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA 282:1547–53.
- White WB. (2010). The risk of waking-up: impact of the morning surge in blood pressure. Hypertens 55:835–37.