ABSTRACT
Objectives
It has been hypothesized that dietary fiber intake has a beneficial impact on prevention of dementia, but the epidemiological evidence is scant. We sought to examine whether dietary fiber intake is inversely associated with risk of dementia requiring care under the national insurance (disabling dementia).
Methods
The study setting was the Circulatory Risk in Communities Study, involving 3739 Japanese individuals aged 40–64 years at the dietary surveys (1985–99). Dietary fiber intake was estimated using the 24-hour dietary recall method. Incident disabling dementia was followed up from 1999 through 2020. Disabling dementia was further classified into that with or without a history of stroke. Hazard ratios of disabling dementia according to quartiles of total, soluble, and insoluble fiber intake were calculated using the Cox proportional hazards model.
Results
During a median 19.7-year follow-up, a total of 670 cases of disabling dementia developed. Dietary fiber intake was inversely associated with risk of dementia: the multivariate hazards ratios (95% confidence intervals) were 0.83 (0.67–1.04), 0.81 (0.65–1.02), and 0.74 (0.57–0.96) for individuals with the second, third, and highest quartiles of dietary fiber intake, respectively, as compared with the lowest quartile (P for trend = 0.03). The inverse association was more evident for soluble fiber intake and was confined to dementia without a history of stroke. As for fiber-containing foods, potatoes, but not vegetables or fruits, showed a similar association.
Conclusions
Dietary fiber intake, especially soluble fiber, was inversely associated with risk of disabling dementia in a general Japanese population.
Introduction
Dietary fiber is a component that reaches the large intestine without being affected by digestive enzymes in the small intestine but is thought to affect the bacterial flora in the large intestine [Citation1] and may lead to health benefits [Citation2]. Recently, brain-gut interaction has received attention in terms of the development of dementia [Citation3]. The concept of brain-gut interaction emerged from the idea that the central nervous system communicates bidirectionally with the gastrointestinal tract, suggesting that the gut microbiome may influence brain plasticity and cognitive function [Citation4]. For example, a cross-sectional study of 128 Japanese patients who visited a memory clinic showed that the number of Bacteroides species was lower among patients with dementia than among those without it [Citation5].
A soluble high-fiber food or diet enhanced the abundance of the Bacteroides species in mice [Citation6]. Another mice study showed that a soluble high-fiber diet attenuated neuroinflammation associated with ageing via butyrate-induced gut bacteria [Citation7], whilst insoluble fiber was not reported to have such a neuroprotective effect. Most insoluble fibers have not been recognized as prebiotics [Citation1], but some animal studies have suggested that insoluble fibers were involved in the regulation of the gut microbiome [Citation8].
In this context, we sought to test the hypothesis that dietary intake of fiber, especially soluble fiber, is associated with a reduced risk of dementia. As secondary analyses, we classified dementia into that with a history of stroke and that without it and hypothesized an inverse association between fiber intake and risks of both types of dementia via the antiatherosclerotic and neuroprotective effects of dietary fiber. We previously reported an inverse association between intake of beans, a fiber-containing food, and risk of disabling dementia [Citation9]. We here extended the analyses to dietary intakes of total, soluble, and insoluble fibers and other fiber-containing foods (i.e. potatoes, vegetables, and fruits) in relation to risk of disabling dementia. We distinguished potatoes from vegetables because the composition of starch in potatoes and vegetables is quite different, potatoes are considered as a different category from vegetables in Japanese food culture, and potatoes are classified separately from vegetables in the Standard Tables of Food Composition in Japan.
Methods
Study cohort
The Circulatory Risk in Communities Study (CIRCS) is an ongoing dynamic community cohort study involving five communities in Japan. Details of the CIRCS protocol have been described elsewhere [Citation10]. In the present study, we included three communities, Ikawa, Yao, and Kyowa, where disabling dementia surveillance is being conducted.
A total of 9992 people aged 40–69 years living in these three communities participated in the annual health checkups between 1985 and 1999. Of these, 38% of the participants, usually systematically sampled, underwent the dietary surveys. We determined the risk set as 3750 people who first participated in the dietary surveys from 1985 to 1999. They were followed up to confirm incident dementia from 1999 through 2020 (except for from April 2005 to April 2008, for which period the data were unavailable) in Kyowa; from 1999 through 2019 in Ikawa; and from 2006 through 2019 in Yao ().
Figure 1. Dietary surveys were conducted from 1985 to 1999. They were followed up to confirm incident dementia from 1999 through 2020 (except for from April 2005 to April 2008, for which period the data were unavailable) in Kyowa; from 1999 through 2019 in Ikawa; and from 2006 through 2019 in Yao. Persons who participated in the dietary survey within 5 years before receiving a dementia diagnosis were excluded.
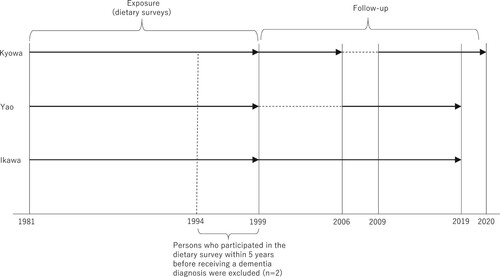
The participants were primarily healthy at the time of the dietary surveys, and we did not ask about history of dementia in the dietary surveys. Instead, we excluded persons who participated in the dietary survey at least five years before receiving a dementia diagnosis (n = 2 excluded) to minimize the possibility of reverse causation. We further excluded nine persons with invalid dietary data. In the end, a total of 3739 participants were involved in this study.
Disabling dementia
From the perspective of preventing dementia that requires care, we determined the outcome of this study as dementia that required care (disabling dementia) under the National Long-Term Care Insurance System, which is a national compulsory insurance for all individuals aged 40 years or older in Japan. The criteria for disabling dementia were the same as those of our previous study [Citation11]; that is, onset of disabling dementia was defined as the first time the following two conditions were met: (1) ‘the level of care require’ being ≥1 (requiring assistance with some or all daily activities for six months or more owing to physical or mental disabilities) and (2) ‘the grade of activities of daily living related to dementia’ being ≥ II (grade II is equivalent to moderate dementia-related behavioral disturbance and cognitive impairment with slight dependence) diagnosed by attending physicians under the National Long-Term Care Insurance System. The validation of the criteria was previously confirmed by comparison with the clinical diagnoses of neuropsychiatrists with high specificity (96%) and with moderate sensitivity (73%) [Citation12]. For the subtype analyses, we further classified the dementia cases into those with or without a history of stroke on the basis of a systematic stroke registration described in our previous study [Citation13], as well as of self-reports provided at the time of the dietary surveys. For the subtype analyses, the follow-up ended on 31 December 2015 for Kyowa and on 31 December 2018 for Ikawa and Yao owing to the availability of the stroke registry data.
Dietary surveys
An interview to administer the 24-hour dietary recall for one day was conducted by trained dietitians, who asked what and how much the participants had eaten during the 24 hours before the interview. In the interview, actualized food models, pictures of food materials and dishes, and/or real foods and dishes such as rice and miso soup were shown to the participant to help him/her with recall of food intake. On the basis of the interview, the foods consumed and their amount were coded, and the intake of each nutrient (including total, soluble, and insoluble fibers) as well as intake of each food group were calculated by using the Standard Tables of Food Composition in Japan (Seventh Revised Version).
Standard multivariate methods were applied for energy adjustment. Reproducibility of the 24-hour recall data was tested by comparison of the fiber intakes of the two studies conducted one year apart in 126 subsamples; the Spearman correlation coefficient was 0.28 for total fiber intake, 0.29 for soluble fiber intake, and 0.32 for insoluble fiber intake.
To determine whether associations would be observed in fiber-containing foods, we also examined the associations of potatoes, vegetables, and fruits (by which the partial R2 for the proportion of the variance in total fiber intake explained was ≥0.05) with risk of disabling dementia. Grains and beans, although they yielded a high R2, were not tested here because the findings for these are supposed to be published elsewhere.
Other risk factors
Potential risk factors for disabling dementia were measured at the time of the dietary surveys. Well-trained study physicians or nurses measured the arterial systolic and fifth-phase diastolic blood pressures by using standard mercury sphygmomanometers on the right arm of the participants, who were quietly seated after having rested for at least 5 minutes. If the first systolic blood pressure reading was ≥140 mmHg and/or the diastolic blood pressure was ≥90 mmHg, the physicians or nurses repeated the measurement. For these cases, the second reading was used in the analysis; otherwise, the first reading was used. Height without shoes and weight in light clothing were measured, and body mass index was calculated as weight in kilograms divided by height in meters squared. Face-to-face interviews were conducted to determine drinking (never, ex, or current) and smoking (never, ex, or current) statuses, amount of alcohol, number of cigarettes, antihypertensive medication, cholesterol-lowering medication, medication for diabetes, and a history of stroke. Serum glucose and total cholesterol were measured without a fasting requirement. Diabetes mellitus was defined as fasting serum glucose ≥126 mg/dL or nonfasting serum glucose ≥200 mg/dL, or being under medication for diabetes.
Statistical analysis
The age-adjusted means and proportions of the characteristics of the study participants at the dietary surveys were compared according to the quartiles of total fiber intake yielded by analyses of covariance. We conducted proportional hazards regression analyses to calculate the hazards ratios and 95% confidence intervals across the quartiles of total, soluble, and insoluble fiber intake and fiber-containing foods (potatoes, vegetables, and fruits) nested by the study communities and adjusted for age, sex, smoking status (never, ex, or current smokers of ≤20 or >20 cigarettes/day), alcohol drinking (never, ex, or current drinkers of <46 or ≥46 g ethanol/day), total energy intake (continuous), and fish, meat, and sodium consumptions (continuous), as potential confounders. For missing values for these variables (<5% of each variable), we set dummy variables and included them in the models. The linear trend for the hazard ratios across the categories was tested using the median value of each independent variable. Because we did not observe significant interactions among sex and any exposures in relation to risk of disabling dementia (P > .05), sex-specific analyses were not performed. All probability values for the statistical tests were two-tailed, and probability values below 0.05 were considered significant. All statistical tests were performed using SAS 9.4 software (SAS Institute, Cary, NC, U.S.A.).
Ethical consideration
Informed consent was obtained from community representatives. Individual consent was not required for the analysis of this study because it was conducted as a secondary use of data obtained for public health practice on cardiovascular disease prevention in the local community at that time. In accordance with relevant guidelines and regulations afterwards, the participants were retrospectively given the opportunity to withdraw their data from analysis. The study was approved by the institutional review boards of the relevant institutions (Osaka Center of Cancer and Cardiovascular Disease Prevention, University of Tsukuba, and Osaka University).
Results
As shown in , men consumed less total fiber than did women. Systolic and diastolic blood pressures were inversely associated with total fiber intake. All food items, including fiber-containing foods (potatoes, vegetables, and fruits), and sodium were positively associated with total fiber intake.
Table 1. Characteristics of participants according to quartiles of total fiber intake at dietary surveys, CIRCS, aged 40–64 years, 1981–99.
During the follow-up (median, 19.7 years; maximum, 21.3 years), we observed a total of 670 cases of disabling dementia. Total fiber intake was inversely and linearly associated with risk of incident dementia (). The multivariate hazard ratios (95% confidence intervals) were 0.83 (0.67–1.04), 0.81 (0.65–1.02), and 0.74 (0.57–0.96) for individuals with the second, third, and highest quartiles of total fiber intake, respectively, compared with those with the lowest quartile (P for trend = .03). Of note, the association was not altered after further adjustment for potential mediators (body mass index, systolic blood pressure, antihypertensive medication use, serum total cholesterol, cholesterol-lowering medication, and diabetes): the respective hazard ratios were 0.81 (0.65–1.02), 0.80 (0.64–1.01), and 0.75 (0.58–0.98) (P for trend = .05) (not shown in ). The association of total fiber intake with disabling dementia was confined to dementia without a history of stroke.
Table 2. Age- and sex-adjusted and multivariate hazard ratios and 95% confidence intervals of incident dementia according to quartiles of fiber intake.
The inverse association with incident disabling dementia was more evident for soluble fiber intake and for potatoes, but not for vegetables or fruits (). The inverse association of soluble fiber was confined to dementia without a history of stroke (Supplementary Table 1). The inverse association of potatoes was observed similarly for dementia with or without a history of stroke, but neither reached statistical significance.
Table 3. Age- and sex-adjusted and multivariate hazard ratios and 95% confidence intervals of incident dementia according to quartiles of intakes of soluble and insoluble fibers, and fiber-containing food groups.
Since the dementia registry data were unavailable between 2005 and 2008 in one community we studied, we conducted a sensitivity analysis starting follow-up from 2009. The associations did not change essentially: the multivariate hazard ratios (95% confidence intervals) of disabling dementia were 0.92 (0.72–1.17), 0.87 (0.68–1.12), and 0.75 (0.57–1.00) for individuals with the second, third, and highest quartiles of total fiber intake, respectively, as compared with those with the lowest quartile (P for trend = .04). The respective hazard ratios of disabling dementia without a history of stroke were 0.89 (0.66–1.19), 0.75 (0.55–1.03), and 0.59 (0.41–0.85) (P for trend = .003) (not shown in tables).
Discussion
We found an inverse association between dietary fiber intake, especially soluble fiber intake, and risk of disabling dementia in the Japanese population. The association was confined to disabling dementia cases without a history of stroke. This is the first prospective study to find an inverse association between dietary fiber intake and risk of dementia in a general population.
The mechanism explaining how dietary fiber reduces the risk of dementia warrants discussion. Fibers were reported to have beneficial effects on body weight, systolic blood pressure, serum lipids, and fasting glucose, and risks of stroke and diabetes [Citation14], which could partly explain the association between fibers and dementia, especially vascular-type dementia. Another mechanism is that dietary soluble fiber regulates the composition of intestinal bacteria [Citation1], and this composition was associated with the prevalence of dementia [Citation3]. Animal studies have shown that dietary soluble fiber improved neuroinflammation [Citation7] that is responsible for Alzheimer disease pathology [Citation15] and that the gut-brain axis may have a role in the cerebral accumulation of amyloid protein such as amyloid-β [Citation16], which is in line with the result of our study. However, another cross-sectional study found no significant correlation between fiber intake and plasma or brain amyloid-β [Citation17]. We also need to note that having a high-fiber diet may reflect a diversity of dietary intake and that socioeconomic status may influence the risk of dementia. A systematic review reported a lower risk of dementia in persons with healthy dietary patterns and Mediterranean diets, i.e. containing high dietary fiber [Citation18], which is partially in line with our result.
We used the data of the compulsory national insurance to register dementia cases, which was a strength of this study. In this system, all individuals with disabling dementia who had applied for long-term care insurance in the communities were identified. The criteria for ‘the level of care required’ are uniformly determined throughout the country, and thus objectivity is guaranteed. On the other hand, using the data based on this system has several inevitable limitations, as previously discussed [Citation19]. The diagnosis of ‘the grade of activities of daily living related to dementia’ was made by attending physicians, not psychiatrists. However, we previously did validate the diagnosis [Citation12], as stated in the Methods. Further, we did not discriminate dementia into Alzheimer and vascular types. Instead, we used information on dementia with or without a history of stroke, assuming that dementia with a history of stroke is likely vascular-type dementia and that dementia without a history of stroke is likely Alzheimer-type dementia.
The other limitations of this study should be noted. First, the dietary surveys asked about meals taken in the last 24 hours. Thus, this survey method was inevitably affected by the foods that the participants happened to have eaten on the previous day or the day of the survey. Nevertheless, the probability of coincidentally eating something that the participant did not usually eat on the specific day of the survey should be small: the 1-year reproducibility of the survey methods was moderate (r ≈ 0.3). Second, the dietary habits must have changed during the long follow-up. Especially in this study, the median time between the dietary survey (1985–99) and the start of follow-up (1999 or 2006) was 9 years. It should be noted that this study focused on the association between dietary fiber intake when the participants were aged 40–64 years before the start of follow-up and probably before the development of most dementia cases. Third, we did not have information on socioeconomic factors, which might be potential residual confounding factors [Citation20]. The national surveys of Japanese representative samples showed a small positive association between household expenditure and total fiber intake (7.2 vs. 6.9 g/1000 kcal in men and 8.8 vs. 8.3 g/1000 kcal in women for the highest vs. lowest quartiles of household expenditure in 2003–7) [Citation21], but no association between household income and potato intake, a main contributor of fiber intake in this study [Citation22]. Last, we did not survey dementia at baseline, although we excluded participants who developed dementia within 5 years of the dietary survey, and the median time from the dietary survey to dementia onset for cases was long (24 years). In addition, data on the dementia registry were unavailable in 1 community between 2005 and 2008. However, the sensitivity analyses following up all the participants from 2009 did not change the results materially. Therefore, the possibility of reverse causation and the impact of unavailable data should be small.
Conclusions
Dietary intake of fiber, especially soluble fiber, was inversely associated with risk of disabling dementia in a general Japanese population. This study should provide new insights into dietary factors that prevent dementia, which needs to be confirmed by further observational and/or intervention studies.
Supplemental Material
Download MS Word (33.2 KB)Acknowledgments
We thank F. Miyamasu, Medical English Communications Center, University of Tsukuba, for language revision.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request and with the permission of the CIRCS committee.
Additional information
Funding
References
- Rezende ESV, Lima GC, Naves MMV. Dietary fibers as beneficial microbiota modulators: A proposal classification by prebiotic categories. Nutrition. 2021;89(111217). doi:10.1016/j.nut.2021.111217.
- Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. Br Med J. 2018;361(k2179). doi:10.1136/bmj.k2179.
- Saji N, Hisada T, Tsuduki T, Niida S, Toba K, Sakurai T. Proportional changes in the gut microbiome: a risk factor for cardiovascular disease and dementia? Hypertens Res. 2019;42(7):1090–1. doi:10.1038/s41440-019-0218-6.
- Solas M, Milagro FI, Ramirez MJ, Martinez JA. Inflammation and gut-brain axis link obesity to cognitive dysfunction: plausible pharmacological interventions. Curr Opin Pharmacol. 2017;37:87–92. doi:10.1016/j.coph.2017.10.005.
- Saji N, Niida S, Murotani K, Hisada T, Tsuduki T, Sugimoto T, et al. Analysis of the relationship between the gut microbiome and dementia: a cross-sectional study conducted in Japan. Sci Rep. 2019;9(1):1008, doi:10.1038/s41598-018-38218-7.
- Nakajima A, Sasaki T, Itoh K, Kitahara T, Takema, Y, Hiramatsu, K, Ishikawa, D, et al. A soluble fiber diet increases Bacteroides fragilis group abundance and immunoglobulin A production in the gut. Appl Environ Microbiol. 2020;86(13). doi:10.1128/AEM.00405-20.
- Matt SM, Allen JM, Lawson MA, Mailing LJ, Woods JA, Johnson RW. Butyrate and dietary soluble fiber improve neuroinflammation associated with aging in mice. Front Immunol. 2018;9(1832). doi:10.3389/fimmu.2018.01832.
- Martinez-Lopez LM, Pepper A, Pilla R, Woodward AP, Suchodolski JS, Mansfield C. Effect of sequentially fed high protein, hydrolyzed protein, and high fiber diets on the fecal microbiota of healthy dogs: a cross-over study. Anim Microbiome. 2021;3(1):42), doi:10.1186/s42523-021-00101-8.
- Kishida R, Yamagishi K, Muraki I, et al. Dietary intake of beans and risk of disabling dementia. The 55th Scientific Meeting of the Japanese Society of Cardiovascular Disease Prevention [abstract]. 2019.
- Yamagishi K, Muraki I, Kubota Y, Hayama-Terada M, Imano H, Cui R, et al. The Circulatory risk in Communities Study (CIRCS): A long-term epidemiological study for lifestyle-related disease among Japanese men and women living in communities. J Epidemiol. 2019;29(3):83–91. doi:10.2188/jea.JE20180196.
- Ikeda A, Yamagishi K, Tanigawa T, Cui R, Yao M, Noda H, et al. Cigarette smoking and risk of disabling dementia in a Japanese rural community: a nested case-control study. Cerebrovasc Dis. 2008;25(4):324–31. doi:10.1159/000118377.
- Noda H, Yamagishi K, Ikeda A, Asada T, Iso H. Identification of dementia using standard clinical assessments by primary care physicians in Japan. Geriatr Gerontol Int. 2018;18(5):738–44. doi:10.1111/ggi.13243.
- Imano H, Kitamura A, Sato S, Kiyama M, Ohira T, Yamagishi K, et al. Trends for blood pressure and its contribution to stroke incidence in the middle-aged Japanese population: the Circulatory Risk in Communities Study (CIRCS). Stroke. 2009;40(5):1571–7. doi:10.1161/STROKEAHA.108.538629.
- Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393(10170):434–45. doi:10.1016/S0140-6736(18)31809-9.
- Giau VV, Wu SY, Jamerlan A, An SSA, Kim SY, Hulme J. Gut microbiota and their neuroinflammatory implications in Alzheimer's disease. Nutrients. 2018;10(11). doi:10.3390/nu10111765.
- Pistollato F, Sumalla Cano S, Elio I, Masias Vergara M, Giampieri F, Battino M. Role of gut microbiota and nutrients in amyloid formation and pathogenesis of Alzheimer disease. Nutr Rev. 2016;74(10):624–34. doi:10.1093/nutrit/nuw023.
- Fernando W, Rainey-Smith SR, Gardener SL, Villemagne VL, Burnham SC, Macaulay SL, et al. Associations of dietary protein and fiber intake with brain and blood amyloid-b. J Alzheimers Dis. 2018;61(4):1589–98. doi:10.3233/JAD-170742.
- Cao L, Tan L, Wang HF, Jiang T, Zhu X-C, Lu H, et al. Dietary patterns and risk of dementia: a systematic review and meta-analysis of cohort studies. Mol Neurobiol. 2016;53(9):6144–54. doi:10.1007/s12035-015-9516-4.
- Yamagishi K, Iso H. Reply to the letter “alpha-linolenic acid levels and risk of dementia; but which type of dementia”. Clin Nutr. 2017;36(2):612), doi:10.1016/j.clnu.2017.01.015.
- Sattler C, Toro P, Schonknecht P, Schroder J. Cognitive activity, education and socioeconomic status as preventive factors for mild cognitive impairment and Alzheimer's disease. Psychiatry Res. 2012;196(1):90–5. doi:10.1016/j.psychres.2011.11.012.
- Fukuda Y, Hiyoshi A. High quality nutrient intake is associated with higher household expenditures by Japanese adults. Biosci Trends. 2012;6(4):176–82. doi:10.5582/bst.2012.v6.4.176.
- Ministry of Health Labour and Welfare. The National Health and Nutrition Survey in Japan. 2016. Available from: https://www.mhlw.go.jp/bunya/kenkou/eiyou/h26-houkoku.html. Accessed 2021/9/5. 2014.
