Abstract
Phenomenon: Chronic disease is a leading cause of death and disability in the United States. With an increase in the demand for healthcare and rising costs related to chronic care, physicians need to be better trained to address chronic disease at various stages of illness in a collaborative and cost-effective manner. Specific and measurable learning objectives are key to the design and evaluation of effective training, but there has been no consensus on chronic disease learning objectives appropriate to medical student education. Approach: Wagner’s Chronic Care Model (CCM) was selected as a theoretical framework to guide development of an enhanced chronic disease prevention and management (CDPM) curriculum. Findings of a literature review of CDPM competencies, objectives, and topical statements were mapped to each of the six domains of the CCM to understand the breadth of existing learning topics within each domain. At an in-person meeting, medical educators prepared a survey for the modified Delphi approach. Attendees identified 51 possible learning objectives from the literature review mapping, rephrased the CCM domains as competencies, constructed possible CDPM learning objectives for each competency with the goal of reaching multi-institutional consensus on a limited number of CDPM learning objectives that would be feasible for institutions to use to guide enhancement of medical student curricula related to CDPM. After the meeting, the group developed a survey which included 39 learning objectives. In the study phase of the modified Delphi approach, 32 physician CDPM experts and educators completed an online survey to prioritize the top 20 objectives. The next step occurred at a CDPM interest group in-person meeting with the goal of identifying the top 10 objectives. Findings: The CCM domains were reframed as the following competencies for medical student education: patient self-care management, decision support, clinical information systems, community resources, delivery systems and teams, and health system practice and improvement. Eleven CDPM learning objectives were identified within the six competencies that were most important in developing curriculum for medical students. Insights: These learning objectives cut across education on the prevention and management of individual chronic diseases and frame chronic disease care as requiring the health system science competencies identified in the CCM. They are intended to be used in combination with traditional disease-specific pathophysiology and treatment objectives. Additional efforts are needed to identify specific curricular strategies and assessment tools for each learning objective.
Introduction
Chronic disease is a leading cause of death and disability in the United States.Citation1 With an increase in the demand for health care and rising costs related to chronic care, physicians need to be better trained to address chronic disease by drawing on the entire health care delivery system.Citation2,Citation3 Wagner’s Chronic Care Model (CCM) has been well-studied as an effective framework to understand the impact of patient-provider relationships and systems-level design features that, in combination, lead to high quality chronic care outcomes in primary care practice.Citation4,Citation5 Elements of the CCM model include health system organization, community resources and policies, patient self-management support, delivery system design, decision support strategies, and clinical information systems.Citation4 These elements can be found across all of the Accreditation Council for Graduate Medical Education’s (ACGME) core competencies, with each element specifically related to an aspect of systems-based practice.Citation6 The CCM is also related to domains within the emerging health system science framework, such as health care delivery processes, clinical informatics, evidence-based practice, and population health. This health systems science framework is used to identify and develop curricula related to the principles and methods of improving care of patients and populations.Citation3
While the pathophysiology and treatment of specific chronic diseases are included in most medical school curricula as part of the competencies in medical knowledge and patient care, the inclusion of chronic disease prevention and management (CDPM) from a systems-based practice perspective has seldom been studied in the education literature. In a 2015 systematic review of educational interventions in chronic care in the medical, nursing, and pharmacy literature, Bogetz and colleagues identified only 22 studies that met their inclusion criteria.Citation2 The authors mapped these studies onto Wagner’s CCM to better represent the degree to which curricular interventions included an evidence-based systems perspective in the approach to increasing chronic care education. The majority of these studies addressed only one CCM element, only seven included more than one element, and none included all six elements. This suggests that education in CDPM is not approached from a health systems science perspective with systems-based practice in mind.
As part of the Accelerating Change in Medical Education (ACE) initiative, the American Medical Association (AMA) convened a meeting in June 2016 of national experts in CDPM. Key stakeholders responsible for CDPM curriculum at each ACE consortium school were invited for a focused discussion. The goal was to discuss CDPM from a systems-based practice perspective in medical student education and to identify gaps in the CDPM curriculum at their own institutions as well as strategies to address these gaps. Participants agreed on the need for a set of medical student level CDPM learning objectives that could serve as a foundation for the systematic development of curriculum, assessment tools, and multi-institutional educational intervention studies.Citation7 This study reports on a multi-step process utilizing a modified Delphi technique to develop learning objectives that medical students should accomplish prior to graduation to prepare them to deliver evidence-based chronic care within a health systems science lens.Citation8
Methods
In 2013, the AMA formed the ACE Consortium and funded an expansion from 11 to 32 schools in 2016. As a result of strong interest from within the consortium to improve chronic disease curricula, the AMA convened an invitational meeting in June 2016 to explore current gaps, barriers, and needs associated with curricula focused on CDPM, discuss current best practices for preparing medical students to prevent and manage chronic diseases, define achievable goals for medical students related to CDPM and explore potential methods of achieving these goals, develop an action plan to work toward the established goals, and discuss how attendees could collaborate with and support consortium schools in their efforts. A co-investigator with expertise in curriculum development facilitated small group sessions to identify achievable goals (L.W.). By the conclusion of the meeting, attendees agreed that the next step was to identify a core set of learning objectives utilizing a modified Delphi technique. A CDPM interest group was formed to continue the work of this invitational meeting, including defining fundamental principles of CDPM for teaching and assessment.
Justification
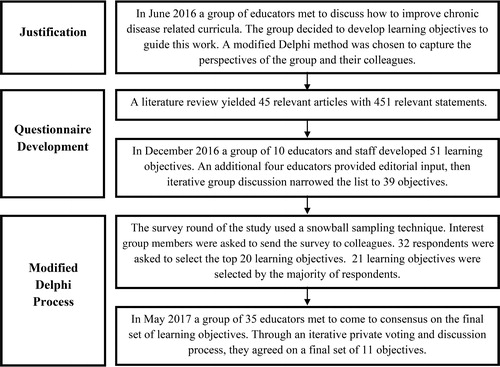
A modified Delphi technique was selected to develop a set of learning objectives to guide the interest group’s work. This technique was chosen to systematically collate the opinions and expertise of group members based on their own experiences teaching and integrating this content within their individual institutions. As the goal was to develop new curricula and enhance existing curricula within participating institutions, we believed that the constructivist nature of this technique would reflect the collective needs of group members. The main steps of the modified Delphi process are depicted in .
Planning and design
First, the CDPM interest group members created a working definition of chronic disease. Through multiple conversations, chronic disease was defined as an illness or medical condition lasting more than three months, generally not self-limited, with an impact on patient quality of life and function. Chronic disease is “broadly inclusive of health issues that require a life course approach to health promotion, risk factor reduction, disease prevention, treatment and management of illness, and systems-level, multi-sectorial approaches for population health.”Citation9 (p. Citation1) The group chose Wagner’s Chronic Care Model as a framework because of the body of research on primary care outcomes, their own experiences using the CCM within their curricula, and previous use of this model within education research.Citation2,Citation5 Additionally, the CCM is applicable across multiple specialties (including and beyond primary care), and it aligns well to both ACGME core competencies and the health systems science framework while still being specific to CDPM. In this context, elements of the CCM were operationalized as competency domains at a level of description appropriate for medical student education: patient self-care management, decision support, clinical information systems, community resources, delivery systems and teams, and health system practice and improvement.
In order to generate a questionnaire for the Delphi process, the interest group conducted a literature search to develop a master list of existing learning objectives or competency statements relating to CDPM that are associated with teaching chronic care to all health professionals at all levels of education. That list served as the basis of a facilitated discussion among a smaller group who then prepared a first draft set of learning objectives. That first draft was subsequently edited by an additional small group of interest group members.
The literature search was conducted by one of the authors (M.D.) with the support of a medical librarian. Search terms were modeled after the literature search described by Bogetz et al. and included variations of Wagner’s CCM, as well as a mixture of the name of each domain of Wagner’s CCM with the words “learning objectives” or “competencies” (e.g., decision support learning objectives; decision support competencies). A PubMed and Google Scholar search of articles related to the CCM yielded 45 relevant articles. Articles were included from across the continuum of medical education if they included at least some variation of competencies, objectives, and statements articulating attitudes, knowledge, or behaviors for preventing or managing chronic disease related to CCM. To supplement the literature search, the ACGME milestones related to these CCM competencies were identified from each specialty. The resulting set of articles and their associated competency statements were mapped to the six CCM-derived educational competencies. A physician-investigator (K.K.) reviewed and confirmed the mapping, and removed objectives and ACGME specialty milestones related to CDPM that were disease specific. describes the number of sources and the number of statements that were mapped to each educational competency.
Table 1. Results of a literature review mapping articles to the chronic care model.Citation4
Seven interest group members with both educational and chronic disease expertise representing six medical schools and five specialties (internal medicine, family medicine, obstetrics and gynecology, geriatrics, and endocrinology) along with three AMA staff members convened in December 2016 to discuss the findings of the literature review and decide on topics for which to draft learning objectives. Meeting attendees worked in pairs on each one of the six CCM-derived educational competencies to draft initial learning objectives based on the statements from the literature review mapped to the competency that they had been assigned. Attendees created 51 learning objectives, agreed that the list was fluid and that objectives may be altered, added, or removed based on subsequent discussion. As such, four members of the interest group who were not present at the in-person meeting volunteered to provide input during two conference calls on the thoroughness of objectives included and the feasibility of incorporating them within an undergraduate medical education curriculum. As a result of this exercise, the 51 learning objectives were narrowed down to 39 based on consensus on these calls. Consensus was reached when all opposing views were discussed and no dissenting opinions were given about the chosen learning objectives.
Study conduct
The survey round of the modified-Delphi approach was the first of a two-step study design. A snowball sampling approach was utilized in which interest group members were asked to complete an online survey to select 20 objectives based on importance for medical student education. Participants were told that their responses would help develop a curricular framework for CDPM. Interest group members were asked to recruit one or more colleagues with expertise in CDPM and/or medical education to also complete the online survey. We mitigated the potential of biasing participants by providing space for them to comment on the survey and inform us of any content areas that were missing from this set of objectives. Learning objectives were retained for the next step if they were selected by the majority of respondents.
The second step of the study design was conducted at an in-person CDPM thematic consortium meeting in May 2017 with attendees from 14 schools. An investigator with curriculum development expertise (L.W.) facilitated a discussion of the objectives identified in the previous step of the study design with a focus on relevance, importance, feasibility, and uniqueness. The final list of learning objectives was intended to be unique to CDPM and not duplicated elsewhere in medical school curricula. During these discussions, the learning objectives were slightly edited for clarity. Following the discussion, a private vote was held. Each objective was written out on a large flip board, and each participant independently placed a marker next to an objective to indicate the most important. Attendees reached complete consensus on a final set of learning objectives based on subsequent discussion and reflection of their votes. In this process, objectives were revised during the discussion to reflect the conversation. Collective agreement on consensus was reached when all participants agreed that their perspectives did not conflict with the final set of objectives. Results were reported to the group and confirmed through subsequent discussion. After this meeting, a physician-investigator with expertise in chronic disease (E.J.) further revised the learning objectives for clarity and consistency of language throughout the framework.
The University of Illinois at Chicago institutional review board, the central review board for the AMA, determined that this study was exempt as part of the AMA’s protocol of evaluation and research related to regular education practices for the Accelerating Change in Medical Education initiative.
Results
The survey portion of the modified Delphi process was completed by 32 chronic disease educators and resulted in 21 proposed learning objectives. A majority of participants in this process included primary care physicians and held academic appointments as either faculty, course directors, residency program directors, and/or deans. The number of objectives chosen by each respondent ranged from six to 21, and all objectives that were chosen by the majority were included in the next step of the study design. This step involved 35 attendees at a face-to-face CDPM thematic meeting in May 2017 and resulted in a final set of 11 learning objectives. describes each educational competency and lists the final learning objectives for each. Overall, critiques of objectives that were not selected included ambiguity, implementation that would require major changes to curricula, material that was covered elsewhere in the medical student curricula, or objectives that were beyond the scope of undergraduate medical education. The selected learning objectives were inclusive of all six elements of Wagner’s CCM, were important in increasing attention to chronic disease care, could be easily integrated into existing medical student curricula, and were measurable.
Table 2. Chronic disease prevention and management competencies, descriptions, and learning objectives.
Patient self-care management
The learning objectives selected for the patient self-care management competency ensure that students can elicit and articulate patient identified barriers to and strategies for health promoting behaviors, as well as demonstrate communication strategies (e.g., motivational interviewing) to engage patients in self-care management. These two behaviors are central to a person-centered approach to care that incorporates patients and their support system (e.g., family, friends) preferences with recommendations of their health care team. Patients living with chronic disease face many challenges in their everyday lives and often make informed and uninformed decisions about their own care. Physicians should be able to engage patients in sharing what they have tried and to negotiate a shared treatment plan that recognizes the patient’s priorities, as well as any patient and system barriers to ensure this plan is feasible and optimal. This approach requires an ongoing dialogue that considers important patient comorbidities including social needs that may evolve over time, as well as important communication tools to help patients achieve their self-defined health goals utilizing shared-decision making strategies.
Decision support
Two of the learning objectives selected for the decision support competency relate to data collection. Relevant data include personalized subjective data reported by the patient, objective data collected by the provider, and information that supports clinical decision-making, such as the evidence base or clinical guidelines relevant to a given condition. These objectives ensure that learners utilize appropriate tools (e.g., expanded social history, chronic disease history, and physical examination) to obtain patient-centered values, goals, and socio-behavioral-economic factors that influence CDPM decision-making, as well as evidence-based clinical practice guidelines or tools (e.g., rubrics, calculators, and risk screeners) for patient-centric and population-based risk assessment screening. The objective related to collection of patient data emphasizes the importance of including psychosocial determinants of health and person-centered information such as personal values and goals as part of the standard history for a person with a chronic disease. The objective focused on evidence-based guidelines emphasizes the use of practical tools rather than extensive critical appraisal of the primary literature. The third objective involves synthesizing all relevant information, both subjective and objective, ensuring that learners apply the information gathered to co-create a comprehensive CDPM plan with the patient. The group discussed that this objective could also engage students in addressing the discomfort that occurs when guidelines and patient preferences do not align. These objectives build on traditional data collection and decision-making skills. Specifically, they highlight the importance of collecting nontraditional data in a biomedical context (e.g., social needs), eliciting person-centered information, and developing and documenting a long-term plan that addresses biomedical and psychosocial needs using a shared decision-making approach.
Clinical information systems
The first learning objective in the clinical information systems competency ensures that learners appropriately utilize the electronic health record to review, guide, and document person-centered CDPM information. This strategy is a key component to understanding the big picture of how information systems add value to the management of chronic diseases over time. The ability to conduct this task for individual patients over time is a different skill than the ability to use the record to address an acute medical concern. After learning how to use the information systems at the individual level, learners should be able to utilize electronic health record tools to identify population level burden, disparities, trends, and outcomes in CDPM. Essential skills include understanding how a variety of information systems can inform individual patient care and extrapolating results to population level actions. Information systems have enhanced the ability to track outcomes over time, identify patients who need additional interventions, and develop registries to longitudinally follow patients to understand the development and trajectories of their chronic conditions.
Community resources
The essential learning objective that emerged for this competency ensures that learners will be able to recognize community resource availability for CDPM. Community resources in the CCM refer to community programs and linkages with community organizations that fill gaps or extend the delivery of care. These resources, such as exercise programs, senior centers and departments of health, have the potential to expand the health system’s capacity to care for chronic illness and improve outcomes, and may be particularly useful for practices with limited resources. In a broader context, community resources would include need-based programs offered by federal, state, and other regional nonprofit organizations. This objective requires students to learn about their community and helps bridge the gap between the health care system's services and the community’s unmet needs, emphasizing that the relationship between the health care system and the community must be bi-directional.
Delivery systems and teams
The learning objective selected for the delivery systems and teams domain ensures that students are able to describe the advantages and functions of interprofessional teams in chronic disease care delivery, care coordination, and transitions of care. Successful interventions for CDPM rely on multidisciplinary care teams to ensure that patients receive comprehensive clinical and self-management support services. The group discussed that effective interprofessional care may also help prevent physician burnout.
Health care practice and improvement
Two learning objectives selected for the health care practice and improvement competency ensure that learners will be able to describe the role of health care finance systems in influencing chronic disease care delivery and identify local and national public policies and practices that affect CDPM. This competency encompasses issues related to access to care as well as to the quality of care delivery. It has implications for patients and providers in terms of a wide range of socioeconomic concerns, cultural considerations, as well as geographic implications. Limited political representation and influence are noteworthy factors with potentially serious consequences for health system practices, improvements, and substantive reforms. Policies can restrict access, particularly for patients already struggling with financial and other resource challenges, affecting both patients and providers, respectively and in partnership. As such, the group discussed that understanding the importance of policy and its implications on health will help learners appreciate the effect of public policy on access to care, and that health care costs and finance may be drivers of the other competencies as well, specifically funding for team-based care.
Discussion
Medical education must continue to evolve in order to prepare students to meet the needs of populations with an increasing prevalence of chronic disease and participate in changing models of health care delivery to better meet those needs.Citation2,Citation3,Citation6 Medical schools and licensing examinations have traditionally focused on acute clinical conditions, initial diagnosis, or treatment of specific chronic conditions (e.g., diabetes, hypertension) as it is easier to develop teaching and assessment scenarios around such clinical presentations. Prior reports have suggested the need for improving education on preventive medicine and have highlighted the substantial differences between education on acute and chronic diseases.Citation10,Citation11
This study used an expert consensus process with a modified Delphi technique to identify 11 learning objectives that focus on the prevention and management of chronic disease from a systems perspective, reflecting the increasing attention to health systems science nationally.Citation3 Using Wagner’s CCM as a conceptual and contextual framework, faculty members can use these learning objectives to guide the development and enhancement of CDPM medical student curricula.Citation4,Citation10 The goal of these learning objectives is to teach CDPM in a manner that encompasses the range of strategies necessary for managing chronic disease that goes beyond the learning of the pathophysiology and treatment of individual chronic conditions during the organ system sections of the curriculum. The objectives focus on systems-level issues that affect the context in which individual care is being delivered. With the increasing prevalence of chronic disease, it is important that students recognize the important role of health systems science in the management of individuals and populations with multiple comorbidities.Citation3 Thus, these objectives reflect knowledge, skills, and behaviors needed for CDPM that can be applied across the specific chronic diseases included in a typical organ-system and specialty-oriented medical student curriculum.
In reaching consensus on the objectives, the CDPM interest group spent a considerable amount of time discussing patient engagement and care delivery in the context of family, community, and population, all of which influence patients’ perceptions of wellness and their disease experience. This intricate interplay of forces requires an important set of skills grounded in a redefinition of the traditional relationship between patients and providers in which care is currently delivered. As such, these objectives are strongly related to health systems science and emphasize both the clinical and systems knowledge required for a foundational understanding of the skills and behaviors necessary to practice in the collaborative environment required for effective chronic disease management.Citation3,Citation5
In real-world management of chronic disease, the vast majority of physicians’ time is spent with patients who will not be cured. Instead, the physician’s goal is to help the patient maintain functionality and experience less distress.Citation1,Citation4 During the development of these CDPM learning objectives, the interest group repeatedly discussed the role that the chronic disease burden plays in physician and student burnout. Studies over the last few decades have demonstrated a trend in students becoming more cynical toward patients with chronic disease as they progress through their education.Citation10,Citation12–15 Ultimately, the group elected to remove learning objectives related to student wellness because they are typically captured elsewhere in the curriculum. But, it is interesting to consider whether the implementation of these CDPM learning objectives could promote the development of skills and attitudes to counteract this tendency toward cynicism. Additionally, these learning objectives include those that focus on developing students as patient advocates, recognizing the role of students as change agents in adding value to the health system through their educational pursuits.Citation16–18
Results of this modified Delphi study should be taken into consideration with the study’s limitations. First, the sample used for the modified Delphi approach was a convenience sample of chronic disease interest group members that attended in-person meetings or completed a survey. Though all were experts in medical education and CDPM, all were drawn from the schools in an education consortium that received funding from the AMA to accelerate change through innovations in medical education, and the purpose of the work was to address their collective needs. These results may not reflect the experiences and perspectives of chronic disease faculty at non-consortium member schools. Second, these ideas were captured at a specific point in time during which the health care system is under pressure to reduce costs. As perceptions and experiences in the health care system change over time, so may opinions about what is important to teach related to CDPM. Third, these results include the perspectives of mostly physicians. Although the planning phase of this process did not exclude any content from non-physician health care professions education, the explicit perspectives of other members of the health care team were not included in this study. Future work validating the use of these learning objectives should include a purposive interprofessional expert panel to understand their expectations of medical students and their perspectives of the physician role in working with chronically ill patients within their health care teams. Finally, issues of wellness and lifelong learning are not addressed within this framework but may be important to include when addressing the cynicism some students feel toward caring for chronically ill patients.
Conclusion
Eleven learning objectives were identified through a modified Delphi process to help guide the development or enhancement of CDPM curricula in undergraduate medical education. The next step for this CDPM interest group is the identification of best practices for teaching these objectives and the development of assessment tools for determining the degree to which students have accomplished them.
Funders
The project was performed with financial support from the American Medical Association as part of the Accelerating Change in Medical Education Initiative.
Prior presentations
These learning objectives were presented as a poster presentation at the annual American Board of Medical Specialties meeting in September 2017 in Chicago, IL, and at the annual Association of American Medical Colleges meeting in November 2018 in Austin, TX. These learning objectives were also presented as an oral paper presentation at the annual American Educational Research Association meeting in April 2019 in Toronto, Canada.
Conflict of interest
Mr. Dekhtyar, Dr. Kirley, and Mrs. Barkowski are paid employees of the American Medical Association. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the American Medical Association.
Acknowledgements
The authors would like to thank Grace Berry, MD; Ruth Crowe, MD, PhD; Darwin Deen, MD, MS; Richard Hawkins, MD; Kenneth Lazarus, MD; Karen McDonough, MD; Eric Walford, MD; Kate Whelihan, MPH; and Jody Gerome Zuchowski, DO, for attending and participating at an in-person meeting and for helping develop and revise the learning objectives used during the modified Delphi process.
References
- Bauer UE, Briss PA, Goodman RA, et al. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. doi:10.1016/S0140-6736(14)60648-6.
- Bogetz JF, Rassbach CE, Bereknyei S, et al. Training health care professionals for 21st-century practice: A systematic review of educational interventions on chronic care. Acad Med. 2015;90(11):1561–1572. doi:10.1097/ACM.0000000000000773.
- Gonzalo JD, Dekhtyar M, Starr SR, et al. Health systems science curricula in undergraduate medical education. Acad Med. 2017;92(1):123–131. doi:10.1097/ACM.0000000000001177.
- Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4.
- Coleman K, Austin BT, Brach C, et al. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009;28(1):75–85. doi:10.1377/hlthaff.28.1.75.
- Kirsh SR, Aron DC. Integrating the chronic-care model and the ACGME competencies: Using shared medical appointments to focus on systems-based practice. Qual Saf Heal Care. 2008;17(1):15–19. doi:10.1136/qshc.2006.020925.
- Bzowyckyj AS, Dow A, Knab MS. Evaluating the impact of educational interventions on patients and communities. Acad Med. 2017;92(11):1531–1535. doi:10.1097/ACM.0000000000001718.
- Junger S, Payne SA, Brine J, et al. Guidance on conducting and reporting delphi studies (CREDES) in palliative care: recommendations based on a methodlogical systematic review. Palliat Med. 2017;31(8):684–706. doi:10.1177/0269216317690685.
- Sciences NA of Chronic Disease Prevention and Control. Global chronic disease prevention and control. http://nationalacademies.org/hmd/Activities/Global/PublicPrivatePartnershipsForum/innovation-collaboratives/Global-Chronic-Disease-Prevention-and-Control.aspx. Published 2015.
- Holman H. Chronic disease – The need for a new clinical education. JAMA. 2004;292(9):1057–1059. doi:10.1001/jama.292.9.1057.
- Garr DR, Lackland DT, Wilson DB. Prevention education and evaluation in US medical schools: A status report. Acad Med. 2000;75(Supplement):S14–S21. doi:10.1097/00001888-200007001-00003.
- Davis BE, Nelson DB, Sahler OJZ, et al. Do clerkship experiences affect medical students’ attitudes toward chronically ill patients? Acad Med. 2001;76(8):815–820. doi:10.1097/00001888-200108000-00015.
- Turner J, Pugh J, Budiani D. It’s always continuing”: First-year medical students’ perspectives on chronic illness and the care of chronically ill patients. Acad Med. 2005;80(2):183–188. doi:10.1097/00001888-200502000-00017.
- Arenson CA, Rattner S, Borden C, et al. Cross-sectional assessment of medical and nursing students’ attitudes toward chronic illness at matriculation and graduation. Acad Med. 2008;83(Supplement):S93–S96. doi:10.1097/ACM.0b013e318183c945.
- Whitcomb ME, Cohen JJ. The future of primary care medicine. N Engl J Med. 2004;351(7):710–712. doi:10.1056/NEJMsb045003.
- Matson CC, Stephens MB, Davis AK, Tallia A, Wilke A. Engaging learners to achieve escape velocity in transformational education and practice. Ann Fam Med. 2016;14(2):184–185. doi:10.1370/afm.1920.
- Gonzalo JD, Graaf D, Johannes B, et al. Adding value to the health care system: Identifying value-added systems roles for medical students. Am J Med Qual. 2017;32(3):261–270. doi:10.1177/1062860616645401.
- Gonzalo JD, Dekhtyar M, Hawkins RE, Wolpaw DR. How can medical students add value? Identifying roles, barriers, and strategies to advance the value of undergraduate medical education to patient care and the health system. Acad Med. 2017;92(9):1294–1301. doi:10.1097/ACM.0000000000001662.