Abstract
Phenomenon: Ultrasound skills are becoming increasingly important in clinical practice but are resource-intensive to teach. Near-peer tutors often alleviate faculty teaching burden, but little is known about what teaching methods near-peer and faculty tutors use. Using the lens of cognitive apprenticeship, this study describes how much time faculty and near-peer tutors spend on different teaching methods during abdominal ultrasound skills training. Approach: Sixteen near-peer and 16 faculty tutors were videotaped during one 55-min practical ultrasound lesson with randomly assigned students. Videos were directly coded using Cognitive Apprenticeship teaching methods and activities. Segment durations were summed up and compared quantitatively. Findings: All 32 tutors spent most of the time on observing and helping students (Coaching, Median 29:14 minutes), followed by asking open and stimulating questions (Articulation, 12:04 minutes and demonstrating and giving explanations (Modeling, 04:50 minutes). Overall, distributions of teaching methods used were similar between faculty and near-peer tutors. However, faculty tutors spent more time on helping students manually, whereas near-peer tutors spent more time on exploring students’ learning gaps and establishing a safe learning climate. Cognitive Apprenticeship was well suited as observational framework to describe ultrasound skills. Insights: Ultrasound train-the-tutor programs should particularly focus on coaching and articulation. Near-peers’ similar use of teaching methods adds to the evidence that supports the use of near-peer teaching in ultrasound skills education.
Introduction
In recent years, diagnostic ultrasound has become an important tool for everyday clinical decision-making and is used by physicians in many different specialties.Citation1 As a result, many medical schools have added modules on learning ultrasound skills to their curricula.Citation2 Ultrasound is a complex skill that involves probe navigation, communication, and image interpretation.Citation3 Typically, ultrasound skills are taught in small groups of 3–4 studentsCitation4 and are thus highly resource-intensive. Numerous medical schools resolve the resulting shortage in teaching staff by involving more advanced students to teach their peers,Citation5 an educational arrangement called near-peer teaching.Citation6 Despite the growing attention to ultrasound education, little attention has been paid to methods used in ultrasound skills teaching.Citation7 Furthermore, there is little research on how near-peer tutors approach this type of trainingCitation8 and whether they use similar teaching methods to faculty tutors. Both of these topics require further investigation in order to optimize train-the-trainer programs.
Teaching ultrasound is complex and involves a variety of teaching methods.Citation9 Crofts et al. observed and interviewed learners in a postgraduate ultrasound programme and identified three dominant learning processes that support ultrasound skills acquisition: Observation of expert practice, feedback on performance, and deliberate practice.Citation3 An Australian group went one step further and asked 528 ultrasound tutors to self-report the teaching strategies that they used when teaching ultrasound skills. On a three-point scale of “do,” “sometimes do” and “do not,” a majority of tutors reported to use coaching (92%), verbalized demonstration (86%), concluding feedback (83%), identification of learning gaps (81%), and immediate error-correction (79%). Less often, tutors reported to identify areas for further learning (68%), use physical guidance (65%) or verbalization by the learner (48%).Citation10 In summary, ultrasound teaching appears to be a combination of demonstration by experts, deliberate practice guided by helping and just-in-time feedback and exploration of gaps and further learning goals; however a clear description of ultrasound teaching methods and their use is still lacking.
To deal with the high volume of small group learning sessions, near-peer teaching has been implemented in many areas of undergraduate curricula.Citation11,Citation12 Studies conducted so far demonstrate favorable student learning outcomes especially in practical skills teaching and no difference when compared to faculty teaching: A recent meta-analysis reviewed 27 studies that compared near-peer teaching with a variety of control interventions and found superior learning outcomes for near-peer teaching of practical skills (SMD = 0.69) but no difference for knowledge outcomes.Citation12 A second meta-analysis focused on ten studies that compared near-peer to faculty teaching in clinical skills, anatomy, and ultrasound training in undergraduate medical programs and found no difference in skills and knowledge outcomes.Citation13 In conclusion, near-peer tutors seem to be non-inferior to faculty tutors when teaching practical procedures such as ultrasound skills. However, there is no information on whether they approach ultrasound teaching in a similar way.
Two recent randomized studies with near-peer vs. faculty tutors in ultrasound teaching found similar skills outcomes measured in OSCE exams for musculoskeletalCitation14 and abdominal ultrasound skillsCitation15 and even superior outcomes for the near-peer group in a cardiac ultrasound course.Citation16 Other studies underlined the long-term retention of skills in near-peer-led ultrasound training for medical studentsCitation17 and the favorable effects on the learning of the peer-tutors themselves.Citation18,Citation19 From a psychological perspective, near-peers are better able to communicate informally and empathically with fellow students because of similar roles (social congruence). Also, the nature of near-peers’ semantic networks of learning more closely resembles that of the learners (cognitive congruence).Citation6,Citation20 It is not known whether and how these psychological differences may influence the way in which near-peers choose and apply different teaching methods in ultrasound skills training.
In this study, we set out to expand our knowledge of the teaching methods that near-peer and faculty tutors use to teach ultrasound skills. To capture the various facets of practical ultrasound skills training, we adopted Collin’s Cognitive Apprenticeship theory (CA).Citation21 We chose CA because it is a common framework for characterizing teaching formats and interactions in medical education and its use has been found to have positive effects on student satisfaction and learning outcomes.Citation22 Also, ultrasound learning often takes place within a master-apprentice learning setting—a setting for which CA provides a more targeted approach compared to other instructional frameworks.Citation7 CA builds on principles of traditional apprenticeship-style learning but takes it to a higher level because it teaches and makes explicit the often tacit processes involved in experts’ handling of complex cognitive tasks.Citation23 It is a theory-based approach to teaching and learning that operationalizes four interconnected dimensions of learning environments: Content, method, sequence, and sociology, though the “method” dimension has received most of the attention in health science education.Citation22
CA teaching methods encourage tutors and students to make “thinking” visible.Citation21 It underlines the importance of modeling by an expert; that is, an expert performs a task and explains how to do it and why. CA also emphasizes the importance of an expert observing the novice who is performing and giving explanations and feedback and helping verbally and manually, which is called coaching. Furthermore, CA underlines the importance of an expert or tutor asking open and stimulating questions to stimulate reasoning (articulation). Finally, an expert should stimulate a novice to set own tasks and goals. In other words, CA, emphasizes modeling, coaching, articulation, and exploration,Citation24 which we chose as the basis of our framework to observe ultrasound skills teaching.
Given the lack of a clear description of ultrasound teaching methods and their use and a lack of understanding on the extent to which near-peer and faculty tutors differ in their approach to teaching ultrasound skills, we sought to answer the following research questions:
How much time do near-peer tutors and faculty tutors spend on the different cognitive apprenticeship teaching methods during ultrasound skills teaching?
What are the similarities and differences in amount of time spent by near-peer and faculty tutors on teaching methods and other activities from cognitive apprenticeship during ultrasound skills training?
A better understanding of which ultrasound teaching activities are used to what extent will be beneficial for the design of targeted “train-the-tutor” programs.
Methods
This was an observational study that counted and quantitatively analyzed the overall duration of teaching methods and activities in 16 near-peer and 16 faculty ultrasound lessons using a framework derived from cognitive apprenticeship.
Context
The setting for this study was the practical part of a blended learning beginner course on abdominal ultrasound at the University of Bern between October 2020 and March 2021. The course focuses on abdominal ultrasound but includes short lessons on thoracic, neck, and musculo-skeletal ultrasound. This course is an elective for third-year medical students within the 6-year curriculum. The course comprises 16-hour long small-group (N = 4) practical ultrasound training sessions dispersed over three months, accompanied by five hours of online self-study on anatomy and principles of ultrasound examination. Students who pass this course and the subsequent summative objective structured clinical exam (OSCE) earn an internationally recognized certificate in abdominal ultrasound.Citation25
Participants
The study participants were 16 near-peer tutors, 16 faculty tutors, and 64 participating students. Near-peer tutors teaching in this course were recruited in their fourth to sixth year of medical school from an existing pool of near-peer ultrasound tutors who taught different courses at the University of Bern. All near-peer ultrasound tutors at the University of Bern must take a three day basic and a three day advanced ultrasound training course. These courses briefly cover group dynamics and giving feedback, but not within the context of CA. All near-peer tutors finished this mandatory training before the study. Faculty tutors were recruited from an existing pool of medical doctors who teach ultrasound courses at the University of Bern. All faculty tutors were formally educated in ultrasound and were experienced tutors at different levels of didactic training.
Tutor characteristics are described in . All participants were purposefully selected to represent a range of experiences and to include men and women. Near-peer tutors were younger (median: 23 years old vs. 41), less experienced, and more likely to be female than faculty tutors. Near-peer tutors also said they spent more time teaching per month (4 hours vs. 2, p = 0.25). We did not discuss CA methods with either faculty or near-peer tutors. Near-peers received their initial didactic training by faculty tutors who did not participate in this study.
Table 1. Tutor characteristics, continuous variables denoted as median [25th percentile, 75th percentile].
The 64 participating third-year medical students were randomly allocated to 16 groups of four by an external partner (Clinical Trials Unit Bern) using centralized computed randomization. Students remained in the same group for the whole course.
Ethical approval
We submitted an ethics request (BASEC number Req-2020-01087) to the cantonal ethics committee of Bern, Switzerland, which declared this study was not subject to the Swiss Human Research Act. All study participants signed an informed consent form and were informed that the teaching sessions would be videotaped to compare teaching behavior, but did not know what behaviors were subject to the study. Because unexpected pathological findings are frequent in ultrasound courses, we set up a reporting system in which a senior staff member would contact participants with incidental findings within 24 hours. The University of Bern paid an expert in ultrasound to reassess the findings if necessary.
Teaching sessions and group allocation
Thirty-two practical ultrasound lessons were recorded, taught by 16 different near-peer and 16 faculty tutors (n = 32). Because teaching activities depend both on the tutor and on participants, several measures were taken to level out differences in participant groups. The course size was set to 16 student groups of four. For each of these groups, one lesson with a near-peer and one lesson with a faculty tutor was videotaped and analyzed. The order in which the lessons were organized was deliberately chosen to ensure that near-peer and faculty tutors were analyzed in trainings with the same number of beginner (4 lessons), intermediate (8 lessons) and advanced (4 lessons) groups. The sample size was limited by the number of available tutors, but we determined that including 16 groups would power our study to detect quantitative differences between near-peer and faculty tutors if the effect size was large (≥1SD, alpha: 5%, power: 80%).
Data collection
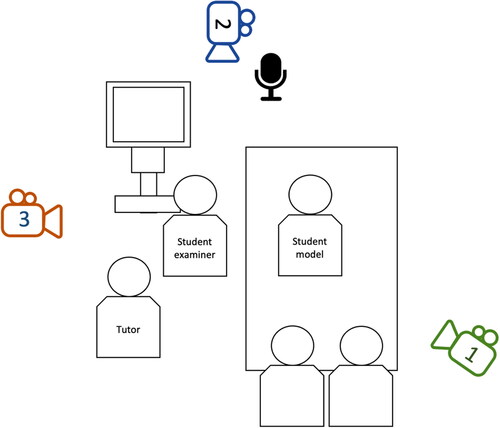
All participating tutors filled in an online questionnaire about demographics, ultrasound, and teaching experience. Three immobile video cameras and an additional microphone () were used to record the sessions. Camera 1 focused on tutor–student interactions and tutors and students handling the ultrasound machine. Camera 2 captured the faces of the tutor and the four participating students, who were looking toward the screen. Camera 3 focused on the probe and the hands guiding the probe and operating the ultrasound machine. For the analysis, all 3 video tracks were merged into a 3-perspective video and synchronized it with the audio track from the added microphone.
Data analysis
All the videos were analyzed in real time in MAXQDA software (version 2020, Release 20.3.0) using an observational framework derived from Cognitive Apprenticeship (CA).Citation24 The CA methods adapted for clinical teaching are divided into modeling, coaching, articulation, and exploration. Three categories “Creating a Safe Learning Climate,”Citation26 “Procedural Information,” and “Off-task”Citation27 were added to code the time not spent on CA methods (detailed description in Appendix 1).
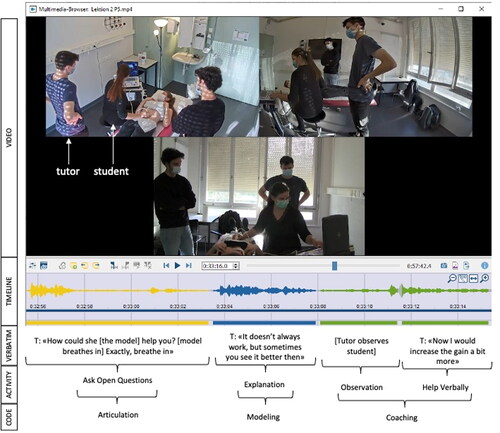
To operationalize the four CA methods, the teaching methods were further divided into 15 teaching activities based on the Maastricht Clinical Teaching QuestionnaireCitation26 (see ). The following types of interactions in ultrasound teaching were investigated (operationalized activities are in parentheses): modeling (demonstration, explanation); coaching (observation, feedback, set tasks, help verbally, help manually); articulation (ask open/closed questions, stimulate questions, think about gaps); exploration (set own tasks/goals); create safe learning climate; procedural information; and off-task interactions. gives verbatim examples for all types of interactions.
Table 2. Verbatim examples for methods and other activities from cognitive apprenticeship.
The full timeline was split into segments in MAXQDA and attributed to one of the teaching interactions according to the codebook. Segment duration was defined from the moment an activity began to the moment a different activity dominated. The length of one unit of analysis could therefore vary from a few seconds (e.g. a tutor interrupting observation by setting a new task) to about a minute (e.g. longer period of uninterrupted demonstration by tutor). Mean code length was 4.3 s; 12,158 segments were coded. If several activities overlapped, the dominant activity was chosen for the analysis. For example, in the beginning of the scene depicted in , the tutor observes the student but the main teaching activity is that the tutor encourages the student to reflect on how to optimize the image (“Ask open Question”). Coding only one activity at a time enabled us to attribute the full time of the lesson to one activity and to give percentages of “time spent per activity.” shows direct coding of videos within MAXQDA. Verbatim transcripts are presented in this figure for illustration purposes only; we did not routinely transcribe videos for this study but coded directly in the videos.
The first two videos were analyzed by three researchers (RH, RC, SR) who met to discuss their coding and come to consensus after every video. During consensus meetings, researchers used MAXQDA’s merge function to compare their coded timelines and discussed discordant segments. At these meetings, they also discussed general difficulties in coding like missing or ambiguous categories. The initial codebook was updated when necessary, for example, to add sub-categories for spontaneous student actions or to divide the activity “Helping” (method: Coaching) into “Help Verbally” and “Help Manually” (e.g., taking the probe). All these changes were documented in the updated codebook (for the final version, see Appendix 1). Reasons for changes were documented in a separate decision sheet. In addition to the consensus meetings, there were monthly meetings with the other members of the research team (RH, SH, DD, RS) to discuss the coding and analysis process and to reach consensus on the final codebook. Pairs of researchers (amongst RH, RC, SR) analyzed the next eight videos, coming to consensus on classification and time notations after every second video. In the first videos, all three researchers coded, inter-rater reliability was low and resolving to consensus required discussion after every video and major changes to the codebook. Reliability increased over time, reaching an intra-class correlation coefficient (ICC) between researchers of 0.96 ± 0.15 for duration of teaching methods for the last four videos (#6-10) that researchers coded in pairs. This level of reliability was sufficient to justify coding by a single researcher for the remaining 22 videos (14 by RC, 6 by SR, 2 by RH) discussed in continuing consensus meetings. In this phase of coding, researchers highlighted unclear sections of the lessons and discussed parts of the videos with the research team. We did not calculate inter-rater reliability for individual segments due to the nature of the coding process. Because every rater not only rated the activity, but also set the start and end point of the activity, the rate of exact overlap for every segment and activity was heavily impaired by the chosen segment length (and boundary, which could differ between raters by as small as a second) and did not reflect the actual inter-rater reliability. Instead, coding was discussed to reach consensus.
Statistical analysis
The codes and duration of coded segments were exported to a table. Since the length of training sessions varied somewhat, segment lengths were divided by total video duration and multiplied by 55 minutes to standardize duration to 55 minute per lesson.
For the analysis, teaching methods and other activities were summed up per tutor. Percentage of every teaching method was calculated for all 32 lessons. To compare near-peer and faculty tutors, median time spent on each teaching method and other activities during the 16 near-peer and 16 faculty lessons was calculated, using median values to increase robustness because of the small number of groups.Citation28Differences in groups were calculated using Mann-Whitney U test.
Results
Overall, 32 videos of full ultrasound lessons by 32 different tutors were analyzed with a mean duration of 57 minutes, 40 seconds (min/max 49:09/63:34) per lesson. In the analysis, all numbers were standardized to a lesson length of 55 minutes for better comparability.
Description of ultrasound lessons within the framework of cognitive apprenticeship
shows the median time spent on each teaching method by faculty and peer-tutors. Within the CA teaching activities, the 32 tutors spent most of their time on coaching (median: 29:14 minutes) and articulation (12:04 minutes). Modeling was less frequent (04:50 minutes). In many sessions, tutors induced little or no Exploration (00:38 minutes). CA teaching activities accounted for 87.7% of the time (46:46 minutes) with minimal time spent on off-task activities (04:22 minutes), providing procedural information (01:28 minutes) and creating a safe learning environment (00:45 min). Across the individual tutors, the distribution of CA teaching methods was similar, though the time spent on modeling and articulation varied the most (see Appendix 2).
Table 3. Summary of time used for cognitive apprenticeship methods and other activities, denoted as median [25th percentile, 75th percentile], n = 32.
When dividing CA methods into specific teaching activities () we found tutors spent most of their time on observation (coaching) with explanations (09:46 min) or without explanation (08:25 minutes) and on asking open questions (articulation, 04:41 minutes). Feedback (coaching) took less time (02:36 minutes) and feedback incidents were typically short (00:04 minutes).
Comparing near-peer and faculty tutors
compares median time spent by near-peer and faculty tutors on all teaching activities. The overall distribution was very similar between near-peer and faculty tutors with a high share of CA teaching activities, particularly coaching and articulation. There were no statistically significant differences in the time spent for the aggregated categories modeling, coaching, articulation, and exploration.
Figure 3. Teaching activities within cognitive apprenticeship methods (median values). *Statistically significant differences.
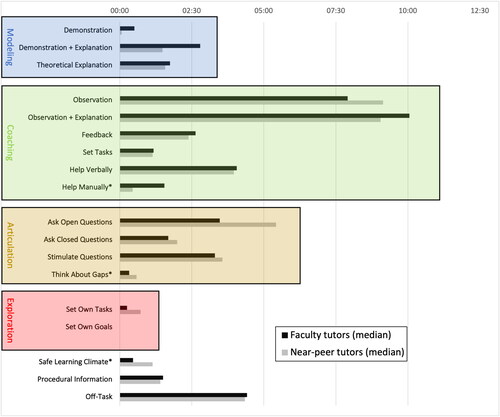
When looking at the activities that were used per CA method in more detail, three differences were statistically significant: faculty tutors spent more time on “Help Manually” (01:33 minutes vs. 00:27 min, p = 0.05), and spent less time stimulating “Thinking About Gaps” (00:20 minutes vs. 00:35 minutes (p = 0.046)) and establishing a Safe Learning Climate (00:28 minutes vs. 01:08 minutes, p = 0.009). The absolute time difference for all these activities was small (max. 01:06 minutes over 55:00 utes) (see Appendix 1 for details).
Discussion
From the perspective of cognitive apprenticeship, ultrasound teaching mainly consists of coaching and articulation, more specifically of observation (coaching), verbal and manual help (coaching), and asking and stimulating questions (articulation). Near-peer and faculty tutors both included a large variety of CA teaching activities and a high percentage of on-task-activities. When students were struggling to achieve a task, faculty tutors more often took over the probe (“Help manually”) while near-peer tutors helped instead by giving verbal cues. Near-peer tutors spent more time establishing a safe learning climate and talking about gaps in students’ knowledge and skills.
We found both near-peer and faculty tutors spent little time on modeling and some tutors almost did not use modeling at all (<1 minute). This is in contrast to the interview/observation study by Crofts, who suggested “observation of expert practice” (modeling) as one of two dominant themes associated with ultrasound skills learning.Citation3 The e-learning that was used in this blended learning course already contained some modeling of expert practice, namely short videos that show experts perform a standardized exam on a healthy volunteer. This may have reduced the need for modeling in the practical training of this course. Modeling may also not be as important in ultrasound teaching because ultrasound is an innocuous, painless procedure,Citation29 which may lower the barrier to experiment. Furthermore, the immediate and visible impact of probe manipulation on the produced image may also facilitate self-learning in ultrasound skills teaching and reduce the need for modeling.
The importance of the second theme by Crofts, “feedback on performance” (coaching),Citation3 was only partially supported by our study: Feedback was common, but very short (around 5% of overall time; mean duration 4 s). Other aspects of coaching such as observation with or without explanation were much more common. The ultrasound images directly provide students with visual feedback, often allowing them to identify specific structures. Therefore, it may often be self-evident to the student whether or not he or she succeeded in the task, likely reducing the need for the tutor to provide structured feedback. In our study, tutors often supported this visual feedback by explaining what was visible on the image while observing.
We found near-peer and faculty tutors use similar teaching strategies when seen through the lens of cognitive apprenticeship. The similarity of teaching strategies and the low percentage of off-task activity in near-peer teaching is reassuring for curriculum planners who think about deploying near-peer tutors in small-group ultrasound skills training. While it is known from experimental studies that the learning outcomes of near-peer and faculty teaching are similar,Citation13 the current study suggests that the means by which both groups facilitated learning may also be similar.Citation6
In our study, near-peer tutors were less likely to manually correct students’ positioning of the probe and more likely to silently observe students perform. This somewhat more passive role may be explained by near-peer tutors’ awareness of their limited content expertise.Citation8 Near-peer tutors spent more time creating a safe learning environment, for example, by introducing themselves, and there was more “talking about gaps” in groups led by near-peer tutors. This aligns with a study by Lockspeiser, where near-peer tutors demonstrated social and cognitive congruence by sharing their own learning difficulties and solutions.Citation20 Overall, we found that there was more variance in facilitation practices within tutor type than across them—a finding that resonates well with a previous video-analysis study that described teaching behaviors in PBL sessions by 3 near-peer and 3 faculty tutors.Citation30
Strengths and limitations
This is the first study to observe and quantify teaching activities in ultrasound teaching by both faculty and near-peer tutors. Careful measures were taken to level out differences in the observed lessons such as randomization of participants, standard size of all groups, and stratification of videotaped lessons with regard to the previous experience of participants. Cognitive Apprenticeship appeared to be a well-suited framework to describe all observable methods that tutors used to instill ultrasound skills in students. One limitation of this study is the lack of a golden standard for how much time is ideally spent on the different methods and activities that are described. This might be a topic for future studies. A second limitation concerns the single setting of this study within practical ultrasound teaching.
Suggestions for further research
Further studies should dive deeper into potential quality markers of the teaching methods observed in this study. Also, more evidence is needed on the educational impact of individual teaching activities described in this study across different contexts and gender. Focal areas could be manual probe correction or passive observation or the combination of them both with regards to participant perception and learning outcomes. This would allow the formulation of a golden standard on the use of teaching methods in practical ultrasound training based on empirical evidence. Qualitative exploration of both the participants’ as well as the tutors’ experiences in practical ultrasound teaching would allow exploration of how and why near peers may apply some CA teaching methods differently from faculty teachers. It would also allow exploration of differences and similarities within the other learning dimensions of CA (content, sequencing, sociology).
Conclusion
Near-peer and faculty tutors used similar teaching strategies with only minor differences while teaching ultrasound skills. Near-peer and faculty tutors both included a large variety of CA teaching activities and a high percentage of on-task-activities. Our results may help to design targeted, ultrasound train-the-tutor programs that sufficiently prepare tutors for the most used teaching activities in this setting. Further, our finding that near-peer and faculty tutors use similar teaching methods and activities adds to the evidence that supports use of near-peer teaching in ultrasound skills education.
HTLM-2022-0200_Appendix_2_SUPPLENTAL.CONENT.ONLINE.ONLY.pdf
Download PDF (68.3 KB)HTLM-2022-0200.R1_Appendix_1_-_SUPPLEMENTAL.CONTENT.ONLINE.ONLY.pdf
Download PDF (78.1 KB)Acknowledgements
The authors are grateful to the tutors and medical students who volunteered to participate in this study and allowed us to record and analyze their ultrasound sessions. We also thank Kali Tal for her editorial suggestions.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- Ma IWY, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: Consensus Recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32(9):1052–1057. doi:10.1007/s11606-017-4071-5.
- Cantisani V, Dietrich CF, Badea R, et al. EFSUMB statement on medical student education in ultrasound [long version]. Ultrasound Int Open. 2016;2(1):E2–7. doi:10.1055/s-0035-1569413.
- Crofts G. A framework for guiding learning in ultrasound scanning. Ultrasound. 2015;23(1):6–10. doi:10.1177/1742271X14562228.
- Dietrich CF, Hoffmann B, Abramowicz J, et al. Medical student ultrasound education: a WFUMB Position Paper, Part I. Ultrasound Med Biol. 2019;45(2):271–281. doi:10.1016/j.ultrasmedbio.2018.09.017.
- Kaymak D, Räschle N, Serra A, Hari R. Introduction of an ultrasound course based on peer-tutoring - an update on the blended learning basic course sonography. Praxis (Bern 1994). 2020;109(8):577–582. doi:10.1024/1661-8157/a003494.
- Ten Cate O, Durning S. Dimensions and psychology of peer teaching in medical education. Med Teach. 2007;29(6):546–552. doi:10.1080/01421590701583816.
- Nicholls D, Sweet L, Muller A, Hyett J, Ullah S. Continuing development and initial validation of a questionnaire to measure sonographer skill-teaching perceptions in clinical practice. J Med Ultrasound. 2017;25(2):82–89. doi:10.1016/j.jmu.2017.01.001.
- Knobe M, Munker R, Sellei RM, et al. Peer teaching: a randomised controlled trial using student-teachers to teach musculoskeletal ultrasound. Med Educ. 2010;44(2):148–155. doi:10.1111/j.1365-2923.2009.03557.x.
- Nicholls D. The Pedagogical Approaches Used by Australian Sonographers to Teach Psychomotor Scanning Skills. Diss. Flinders University, College of Nursing and Health Sciences; 2020.
- Nicholls D, Sweet L, Hyett J, Müller A. A survey of Australian sonographer psychomotor teaching practices. Australas J Ultrasound Med. 2020;23(4):227–237. doi:10.1002/ajum.12223.
- Yang MM, Golden BP, Cameron KA, et al. Learning through teaching: peer teaching and mentoring experiences among third-year medical students. Teach Learn Med. 2022;34(4):360–367.
- Brierley C, Ellis L, Reid ER. Peer-assisted learning in medical education: a systematic review and meta-analysis. Med Educ. 2022;56(4):365–373. Published online September 30 doi:10.1111/medu.14672.
- Rees EL, Quinn PJ, Davies B, Fotheringham V. How does peer teaching compare to faculty teaching? A systematic review and meta-analysis (.). Med Teach. 2016;38(8):829–837. doi:10.3109/0142159X.2015.1112888.
- Cremerius C, Gradl-Dietsch G, Beeres FJP, et al. Team-based learning for teaching musculoskeletal ultrasound skills: a prospective randomised trial. Eur J Trauma Emerg Surg. 2021;47(4):1189–1199. doi:10.1007/s00068-019-01298-9.
- Hofer M, Kamper L, Heussen N, Martin O, Heverhagen J. Influence of clinical expertise between clinician-instructors versus student-instructors on the effectiveness of ultrasound courses. Ultraschall Med. 2022;43(01):58–63. doi:10.1055/a-1176-0622.
- Ben-Sasson A, Lior Y, Krispel J, et al. Peer-teaching cardiac ultrasound among medical students: A real option. PLoS One. 2019;14(3):e0212794. doi:10.1371/journal.pone.0212794.
- Nourkami-Tutdibi N, Tutdibi E, Schmidt S, Zemlin M, Abdul-Khaliq H, Hofer M. Long-term knowledge retention after peer-assisted abdominal ultrasound teaching: is PAL a successful model for achieving knowledge retention? Ultraschall Med. 2020;41(1):36–43. doi:10.1055/a-1034-7749.
- Hoffmann B, Blaivas M, Abramowicz J, et al. Medical student ultrasound education, a WFUMB Position Paper, Part II. A consensus statement of ultrasound societies. Med Ultrason. 2020;22(2):220–229. doi:10.11152/mu-2599.
- Birrane J, Misran H, Creaney M, Shorten G, Nix CM. A scoping review of ultrasound teaching in undergraduate medical education. MedSciEduc. 2018;28(1):45–56. doi:10.1007/s40670-017-0491-4.
- Lockspeiser TM, O’Sullivan P, Teherani A, Muller J. Understanding the experience of being taught by peers: the value of social and cognitive congruence. Adv Health Sci Educ Theory Pract. 2008;13(3):361–372. doi:10.1007/s10459-006-9049-8.
- Collins A Brown JS, Holum A. Cognitive apprenticeship: Making thinking visible. Am Educ. 1991;15(3):6–11.
- Lyons K, McLaughlin JE, Khanova J, Roth MT. Cognitive apprenticeship in health sciences education: a qualitative review. Adv Health Sci Educ Theory Pract. 2017;22(3):723–739. doi:10.1007/s10459-016-9707-4.
- Stalmeijer RE. When I say … cognitive apprenticeship. Med Educ. 2015;49(4):355–356. doi:10.1111/medu.12630.
- Stalmeijer RE, Dolmans DH, Snellen-Balendong HA, van Santen-Hoeufft M, Wolfhagen IH, Scherpbier AJ. Clinical teaching based on principles of cognitive apprenticeship: views of experienced clinical teachers. Acad Med. 2013;88(6):861–865. doi:10.1097/ACM.0b013e31828fff12.
- Raschle N, Hari R. Blended learning basic course sonography - A SGUM accredited ultrasound course based on peer-tutoring. Praxis (Bern 1994). 2018;107(23):1255–1259. doi:10.1024/1661-8157/a003116.
- Stalmeijer RE, Dolmans DH, Wolfhagen IH, Muijtjens AM, Scherpbier AJ. The Maastricht Clinical Teaching Questionnaire (MCTQ) as a valid and reliable instrument for the evaluation of clinical teachers. Acad Med. 2010;85(11):1732–1738. doi:10.1097/ACM.0b013e3181f554d6.
- Visschers‐Pleijers AJ, Dolmans DH, De Leng BA, Wolfhagen IH, Van Der Vleuten CP. Analysis of verbal interactions in tutorial groups: a process study. Med Educ. 2006;40(2):129–137. doi:10.1111/j.1365-2929.2005.02368.x.
- Tavakol M, Wilcox RR. Medical education research: the application of robust statistical methods. Int J Med Educ. 2013;4:93–95. doi:10.5116/ijme.5181.5fe8.
- Devey GB, Wells PN. Ultrasound in medical diagnosis. Sci Am. 1978;238(5):98–112. doi:10.1038/scientificamerican0578-98.
- Cianciolo AT, Kidd B, Murray S. Observational analysis of near-peer and faculty tutoring in problem-based learning groups. Med Educ. 2016;50(7):757–767. doi:10.1111/medu.12969.