ABSTRACT
Research has found that vaccine-promoting messages can elicit state reactance (i.e., negative emotions in response to a perceived threat to behavioral freedom), especially among individuals with high trait reactance (i.e., proneness to experiencing reactance). This can result in a lower willingness to accept vaccines. We investigated whether inoculation against reactance – that is, forewarning individuals about potentially experiencing reactance – can reduce the effects of trait reactance on vaccination willingness. Participants (N = 710) recruited through Facebook were randomly allocated to be either inoculated or not. They were then shown a message promoting a fictitious vaccine, which included either a low, medium, or high threat to freedom. Contrary to research on other health topics, inoculation was ineffective at reducing state reactance toward the vaccination message. Inoculation also did not mitigate the effects of trait reactance on vaccination willingness, and was even counterproductive in some cases. High-reactant individuals were less willing to get vaccinated than low-reactant ones, especially at high freedom threat. Conversely, high freedom threat resulted in increased vaccination willingness among low-reactant individuals. Further research is needed to understand why inoculation against reactance produces different results with vaccination, and to develop communication strategies that mitigate reactance to vaccination campaigns without compromising the positive effects of vaccine recommendations for low-reactant individuals.
Introduction
Vaccine hesitancy poses a significant threat to global health by increasing the risk of outbreaks of severe vaccine-preventable diseases (WHO, Citation2019). Because of this, vaccine communicators devote considerable effort to informing the public about the benefits and safety of vaccines to encourage vaccine-hesitant people to get vaccinated. However, such communication can fail because of psychological reactance. Psychological reactance is a motivational arousal that people can experience when they perceive that their freedom to make decisions is limited or threatened (Brehm & Brehm, Citation1981; Rosenberg & Siegel, Citation2018; Steindl et al., Citation2015). This can happen as a response to recommendations, persuasion, rules, and regulations. Reactance involves emotions (e.g., anger and frustration) and cognitions (e.g., negative thoughts about the freedom threat) that motivate people to regain their freedom, which can manifest as noncompliance or opposing behaviors or attitudes. Reactance can be considered both a state (i.e., a situational experience of arousal in response to a perceived threat) and a trait (i.e., propensity to experience state reactance; Rosenberg & Siegel, Citation2018; Steindl et al., Citation2015).
Vaccine-promoting communication can be perceived by some as infringing upon their autonomy to decide whether to vaccinate, possibly leading to the formation of negative attitudes toward vaccines and eventual vaccination refusal. In fact, individuals with high trait reactance have been found to have more negative vaccine attitudes, lower vaccination intentions, and a higher likelihood of having rejected vaccination in both cross-sectional (Drążkowski & Trepanowski, Citation2022; Finkelstein et al., Citation2020; Hornsey et al., Citation2018; Soveri et al., Citation2020, Citation2023) and longitudinal studies (Soveri et al., Citation2023). They have also been found less willing than low-reactant individuals to change their position on getting vaccinated when given information about the safety and benefits of the vaccine (Soveri et al., Citation2023).
The negative consequences of reactance on the effectiveness of health communication have stimulated research on ways to mitigate it. For example, avoiding freedom-threatening language, providing behavioral alternatives to choose between, and formulating health messages as narratives have been found to reduce state reactance toward health-promoting messages on topics such as physical exercise, healthy diet, alcohol consumption, and smoking (Reynolds-Tylus, Citation2019; Rosenberg & Siegel, Citation2018). However, less is known about decreasing reactance toward vaccine-promoting messages. The existing research has primarily compared levels of state reactance between voluntary and mandatory vaccination. These studies indicate that presenting vaccination as mandatory – thus restricting individuals’ freedom to choose to get vaccinated or not – results in more state reactance than framing it as voluntary (Betsch & Böhm, Citation2016; Sprengholz & Betsch, Citation2020; Sprengholz et al., Citation2021, Citation2022). The more state reactance a vaccine mandate triggers, the less willing the individual has been found to accept the mandated vaccine (Sprengholz et al., Citation2021). While examining how mandating vaccination affects state reactance is informative for policy-making, communicators also need to know how best to design vaccine-promoting messages within the framework of established policies. In a recent study, Soveri et al. (Citation2023) found that emphasizing that vaccination is voluntary (vs. no mention of voluntariness) failed to mitigate the negative effects of trait reactance on vaccination willingness.
Another technique that has been tested to prevent reactance toward health-promoting messages is psychological inoculation. Psychological inoculation involves warning individuals about future attacks on their attitudes and beliefs to protect them from persuasion (Compton, Citation2013). The technique is commonly used in misinformation research and has been found to be successful in making individuals more resistant to persuasion and misinformation (Banas & Rains, Citation2010; Lewandowsky & van der Linden, Citation2021). Inoculations have two central aspects: a warning about future persuasion or misinformation and a rebuttal explaining why the information is misleading or false (Lewandowsky & van der Linden, Citation2021). Inoculation activates cognitive processes, such as the formation of counterarguments, that motivate the individual to protect their beliefs prior to encountering persuasive attempts or misinformation.
The concept of threat is at the core of both psychological inoculation theory and psychological reactance theory, as both inoculation and reactance are thought to elicit resistance to persuasion by increasing the perceived threat of an external persuasive message (Compton, Citation2021; Richards et al., Citation2017). However, instead of building resistance toward external messages, inoculation against reactance involves making individuals resistant to their own internal reactions, thereby decreasing their resistance toward the external persuasive message (Richards & Banas, Citation2015; Richards et al., Citation2017). More specifically, the inoculation is expected to elicit the perception that the individuals’ own reactance poses a threat to them. This perception can help people create resistance toward reactance, ultimately preventing the reactance from increasing the perceived threat of the subsequent persuasive message. Thus, an inoculation against reactance involves a warning that what follows might cause reactance and an explanation of why not to become reactant (Richards & Banas, Citation2015).
Experimental studies have shown that inoculation is effective in decreasing state reactance toward messages that promote reduced consumption of alcohol (Richards & Banas, Citation2015; Richards et al., Citation2017), soft drinks (Richards et al., Citation2017), and e-cigarettes (Clayton et al., Citation2023) by reducing the perceived threat of the messages. However, results are more mixed concerning whether the reduced state reactance translates into higher intentions to engage in the promoted behaviors. In the studies by Richards et al. (Citation2017) and Richards and Banas (Citation2015), inoculation led to lower intentions to drink alcohol and soft drinks. In contrast, the inoculation in the study by Clayton et al. (Citation2023) did not affect intentions to use e-cigarettes, although it successfully reduced state reactance and the perceived threat of the health message. Furthermore, comparing messages with low and high freedom threat, Richards et al. (Citation2017) found that inoculation was successful only when freedom threat was low. They also demonstrated that inoculation against reactance can backfire and cause increased reactance if the inoculation elaborates on the threat of reactance and therefore is perceived as a freedom threat itself.
To the best of our knowledge, only one study has investigated inoculation in relation to trait reactance. This study showed that individuals with high trait reactance perceived a message that encouraged safe-sex behaviors as a threat to their freedom, regardless of whether the message was formulated to pose a low or high freedom threat (Richards et al., Citation2021). Inoculation successfully reduced the perceived threat of the low-threat message for these individuals, but was ineffective for the high-threat message. In contrast, individuals with low trait reactance perceived the low-threat message to pose a small threat even without inoculation, and inoculation successfully reduced the perceived threat of the high-threat message. Trait reactance thus predicts the perceived threat of health-promoting messages and seems to moderate the effectiveness of inoculations.
The present study
The novel contribution of the present study is to extend the research on inoculation against reactance to the field of vaccination. Drawing on psychological reactance theory and psychological inoculation theory, we investigated whether inoculation against reactance can reduce state reactance to vaccine communication among individuals with high trait reactance and increase their vaccination willingness and receptiveness to information about vaccines. We examined this at three different levels of threat (low, medium, and high) to participants’ freedom to choose whether to accept a vaccine in a fictitious vaccination campaign. The study, including the research hypotheses, was preregistered at the Open Science Framework (OSF; https://osf.io/wka5c). We expected that high-reactant individuals would report more state reactance and lower willingness to get vaccinated (H1) and that the effect of trait reactance on state reactance and vaccination willingness would be larger when the threat to freedom in the leaflet was larger (H2). We hypothesized that inoculation would mitigate the effect of trait reactance (H3). Lastly, we expected that high-reactant individuals would change their vaccination willingness less after receiving information about the vaccine compared to low-reactant individuals (H4).
Materials and methods
Participants
Participants were recruited through a Facebook post marketed to adult (18-year-olds and older) Facebook users in Finland. The post contained a link to the online survey and was marketed between September 18th and 20th, 2023. The post reached 33,986 individuals, of whom 1100 (3.2%) clicked the link. The final sample consisted of the 710 (64.5%) individuals who completed the whole survey and answered the attention-check questions correctly. Of these, 615 (86.6%) were women, 85 (12.0%) were men, and 10 (1.4%) reported their gender as other than male or female or did not want to report their gender. The mean age of the sample was 49.84 (SD = 13.38, range = 18–84). Most participants had a bachelor’s (n = 235, 33.1%) or master’s (n = 234, 33.0%) degree as their highest level of education.
The study was approved by the Ethics Committee for Human Sciences at the University of Turku (reference: 29/2023). All participants provided their electronic informed consent before participating in the study. They did not receive any compensation for their participation.
Procedure
The procedure is shown in . After giving informed consent, participants were asked to provide demographic information (i.e., gender, age, and level of education). They were then presented with a short text asking them to imagine that a novel (fictitious) virus causing “green fever” is spreading across the world and that the disease can be serious to those infected. After this, participants randomly received either an inoculation text or no text. They were then randomly presented with one of three leaflets including information about a fictitious vaccination campaign with different levels of threat to participants’ freedom to choose to vaccinate or not (low, medium, or high). After this, participants received an attention check question (see, Supplementary Material) as well as questions about their emotional response to the leaflet (state reactance) and their willingness to get vaccinated with the vaccine in question. Following this, participants received information about the vaccine that was created to mimic that of real vaccines, and they were presented another attention check question. Participants were then again asked about their willingness to get vaccinated. Trait reactance and vaccine attitudes were randomly measured either directly after the demographic questions or at the end of the survey. The median time to complete the study was 5.90 minutes.
Figure 1. Experiment flow demonstrating the procedure and allocation of experimental conditions.
Materials
Inoculation
The inoculation text presented to half of the sample included the two key elements of inoculations against reactance – a warning about reactance and an explanation of why not to become reactant – and was based on an inoculation used in previous research (Richards et al. (Citation2017); Experiment 2). The inoculation read as follows: “The following texts may contain strong language. Some may feel that the text is an attempt to limit their freedom to make their own decisions. Try not to let this affect your judgment. The message of the text may be good and contain important information, although it is presented in a way that may arouse negative feelings, such as anger.”
Threat to freedom
The three leaflets about the fictitious vaccination campaign were formulated with three different levels of threat to participants’ freedom to choose to get vaccinated or not: low, medium, and high (). Prior to the actual data collection, we conducted a pilot study that showed that the leaflets elicited different levels of perceived threat in the expected direction (see, Supplementary Material).
Table 1. Presented information about the vaccination campaign in leaflets with low, medium, and high threat to freedom.
Vaccine information
All participants were provided with the same fictitious information on the safety and efficacy of the vaccine and the severity of the vaccine-preventable disease (see, Supplementary Material). The information described the benefits of the vaccine to outweigh the risks.
Measures
Trait reactance
Trait reactance was measured with the Hong Psychological Reactance Scale (HPRS; Hong & Page, Citation1989). Of the 14 items that are included in the scale, we presented nine that have been shown to result in a satisfactory one-factor solution in Finnish samples (Waris et al., Citation2021). Participants responded to the items on a scale from 1 (completely disagree) to 5 (completely agree). We assessed the fit of the one-factor solution using confirmatory factor analysis (CFA; see, the Results section). Factor scores were retrieved from the CFA and used as the measure of trait reactance in subsequent analyses. A higher HPRS score indicates higher trait reactance.
State reactance
To measure how much state reactance the leaflet elicited, we used the question and the item “frustrated” from the Epistemic Emotions Scale (Pekrun et al., Citation2017) along with two additional items: “angry” and “irritated.” Participants were asked to indicate the strength with which they experienced each emotion when reading the leaflet. Responses were provided on a 5-point scale (1 = not at all; 5 = very strong). The responses to the three items were averaged for the analyses (Cronbach’s alpha = .90).
Vaccination willingness
Willingness to get vaccinated with the fictitious vaccine was measured with the question “How willing would you be to get the vaccine mentioned in the leaflet if it were real?.” Response alternatives ranged from 1 (not at all willing) to 5 (very willing). Participants completed this question at two time points; once after the leaflet (T1) and once after the information about the vaccine and the disease (T2). A change score was calculated by subtracting vaccination willingness at T1 from that at T2 (i.e., a positive score indicates increased willingness).
Vaccine attitudes
Vaccine attitudes were measured with the 5C scale (Betsch et al., Citation2018), which consists of five statements measuring vaccine confidence, convenience, complacency, calculation, and collective responsibility. Participants indicated their agreement with the statements on a scale ranging from 1 (strongly disagree) to 7 (strongly agree).
Statistical analyses
The data that support the findings of this study, as well as R code for analyses, are openly available at OSF (https://osf.io/ybh8c/). R version 4.2.2 (R Core Team, Citation2022) was used for all analyses. The lavaan package version 0.6.15 (Rosseel, Citation2012) was used for the CFA.
Results
Descriptive information
Participants’ mean trait reactance (averaged over the nine items) was 2.48 (SD = 0.81; scale range 1–5; Figure S3). The mean state reactance that the leaflets elicited was 1.77 (SD = 0.98; scale range 1–5; Figure S4). Participants’ mean vaccination willingness was 3.51 (SD = 1.39; scale range 1–5) at T1 and 3.75 (SD = 1.38) at T2. A paired samples t test showed that the increase in vaccination willingness was statistically significant, t(709) = 9.45, p < .001, Cohen’s d = 0.36. Vaccination willingness at T1 and T2 is presented by level of trait reactance, inoculation, and threat to freedom in . Response distributions for all items are presented in Tables S3 and S4.
Figure 2. Mean vaccination willingness and standard error at T1 and T2 by level of trait reactance (dichotomized as high [average HPRS raw score ≥ 3; n = 199, 28.0%] and low [average HPRS raw score < 3; n = 511, 72.0%]), inoculation (no; yes), and threat to freedom (low; medium; high). The figure includes the total sample, and therefore, ceiling effects suppress the change in vaccination willingness, especially among low-reactant individuals. Change in willingness is better visualized in figure S5, from which individuals with the highest possible willingness at T1 have been removed.
![Figure 2. Mean vaccination willingness and standard error at T1 and T2 by level of trait reactance (dichotomized as high [average HPRS raw score ≥ 3; n = 199, 28.0%] and low [average HPRS raw score < 3; n = 511, 72.0%]), inoculation (no; yes), and threat to freedom (low; medium; high). The figure includes the total sample, and therefore, ceiling effects suppress the change in vaccination willingness, especially among low-reactant individuals. Change in willingness is better visualized in figure S5, from which individuals with the highest possible willingness at T1 have been removed.](/cms/asset/923f705b-b0d8-4651-b7ed-decbf3c5dc19/hhth_a_2325185_f0002_oc.jpg)
Preliminary analyses
The CFA showed that the one-factor solution for the HPRS scale suggested by Waris et al. (Citation2021) fit the data well when including two residual correlations between indicators, χ2(25) = 150.89, CFI = .977, TLI = .967, RMSEA = .084; 90% CI[.072, .097], SRMR = .046 (Table S5). One-way ANOVAs with group (six levels; 2 [inoculation] x 3 [threat to freedom]) as independent variable and the HPRS and the 5C variables as dependent measures did not show any statistically significant differences between groups, indicating that the groups were balanced on trait reactance and vaccine attitude (Table S6).
Main analyses
To investigate our hypotheses, we ran three linear regression analyses with state reactance, vaccination willingness at T1, and change in vaccination willingness between T1 and T2 as outcomes, respectively. All analyses included trait reactance, inoculation (no; yes), and threat to freedom (low; medium; high) as predictors, including their interaction terms. For threat to freedom, the contrasts were coded so that each level of threat was compared to the preceding level (i.e., medium vs. low, high vs. medium). VIF and tolerance values suggested no multicollinearity between predictors.
H1 received support, as participants with higher trait reactance reported significantly more state reactance and lower willingness to get vaccinated at T1 compared to those with lower trait reactance (). In line with H2, statistically significant interactions showed that the effect of trait reactance on state reactance and T1 vaccination willingness was stronger in the group that had received the high-threat leaflet compared to the group that had received the medium-threat leaflet. For state reactance, the high-threat leaflet resulted in a significantly higher state reactance compared to the medium-threat leaflet, and the difference between the leaflets increased as trait reactance increased (; Panel A). For T1 vaccination willingness, the high-threat leaflet resulted in lower vaccination willingness than the medium-threat leaflet among participants with higher trait reactance, but higher vaccination willingness among participants with lower trait reactance (; Panel B). There were no significant differences between the low- and medium-threat leaflets. Contrary to H3, inoculation was not a statistically significant predictor in any of the analyses.
Figure 3. Effects of trait reactance and threat to freedom on state reactance (Panel A; N = 710), T1 vaccination willingness (Panel B; N = 710), and change in vaccination willingness between T1 and T2 (Panel C; n = 515). Higher numbers indicate higher trait reactance, higher state reactance, larger vaccination willingness, and larger increase in vaccination willingness. Responses have been vertically jittered to facilitate interpretation.
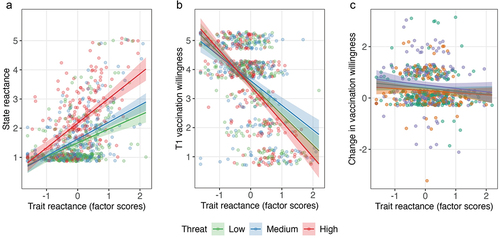
Table 2. Results from regression analyses.
In the regression analysis with change in vaccination willingness as outcome (i.e., the difference between T1 and T2), we excluded those participants who reported their T1 vaccination willingness to be 5 (the maximum score possible; n = 195, 27.5%). This decision was preregistered and made to avoid ceiling effects, as we expected a positive change in vaccination willingness due to the vaccine information being framed to promote vaccination. In support of H4, participants with higher trait reactance changed their vaccination willingness significantly less between T1 and T2 than those with lower trait reactance. Furthermore, participants who had received the high-threat leaflet reported a larger positive change than those who had received the medium-threat leaflet (; Panel C).
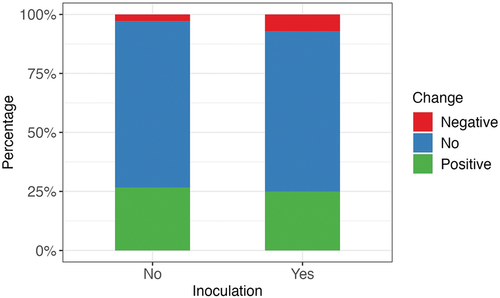
Post-hoc analyses
Although the vaccine information presented to the participants promoted vaccination, some individuals changed their willingness to get vaccinated in the negative direction after having read it. To explore whether inoculation was related to the direction of the change in vaccination willingness, we coded a variable with the categories positive (vaccination willingness higher at T2 than T1), negative (vaccination willingness lower at T2 than T1), and no change (vaccination willingness same at both T1 and T2). We conducted a chi-square test of independence including this categorical variable and inoculation (no; yes). The relationship between the variables was statistically significant, χ2 (2) = 6.96, p = .030. A negative change was significantly more common among participants who received the inoculation (7.2%) compared to those who did not (2.9%; ). The inoculated participants who changed their vaccination willingness in the negative direction did not significantly differ from the rest of the inoculated ones with regard to demographic variables (gender, age, and education), trait reactance, and vaccine attitudes (see, Supplementary Material for statistical information about these analyses).
Figure 4. Percentage of individuals who changed their vaccination willingness between T1 and T2 in the negative or positive direction, or who did not change their willingness, by inoculation (no; yes).
Discussion
In the present study, we investigated whether inoculation against reactance can reduce state reactance to vaccine-promoting messages among high-reactant individuals and increase their vaccination willingness and receptiveness to vaccine information. We examined this at different levels of threat to freedom by presenting participants with a leaflet about a fictitious vaccination campaign with a low, medium, or high level of freedom threat. The results showed that inoculation against reactance was ineffective in reducing state reactance to the message and preventing the negative effects that trait reactance had on vaccination willingness and receptiveness to vaccine information. Although all vaccine messages were formulated to mimic real vaccines and diseases, a limitation of the present study is that the vaccination campaign was fictitious, and the reactions to the campaign may therefore differ from those in real life. Furthermore, the study did not include a measure of inoculation threat, making it difficult to determine whether the inoculation message failed to create the intended perception of reactance as a threat, or if the message successfully induced this perception, but that this did not reduce resistance toward the vaccine-promoting message. When generalizing the results, it should be kept in mind that the data collection was conducted on Facebook and thus only included social media users Also, women and highly educated individuals were overrepresented in the sample (87% women, 33% bachelor’s degree, 33% master’s degree; corresponding percentages in the Finnish population are 51%, 13%, and 11%, respectively; Statistics Finland, Citation2024a, Citation2024b). However, demographics such as gender and education have been found not to influence the effectiveness of inoculation (Roozenbeek et al., Citation2020).
In line with previous studies that have linked trait reactance to more negative vaccine attitudes, lower vaccination intentions, and past vaccine rejection (Drążkowski & Trepanowski, Citation2022; Finkelstein et al., Citation2020; Hornsey et al., Citation2018; Soveri et al., Citation2020, Citation2023), participants with high trait reactance reported higher state reactance to the vaccine-promoting message and lower willingness to receive the vaccine than low-reactant participants at all levels of message threat. The relationship between trait reactance and vaccination willingness was strong (standardized b = −.52) even when controlling for other variables. We also replicated the results by Soveri et al. (Citation2023), who found that high-reactant individuals changed their stance on vaccination less than low-reactant individuals after learning about the benefits and safety of the vaccine. The results thus suggest that trait reactance can have a considerable negative impact on how vaccination campaigns are received.
Contrary to our prediction and previous research (Clayton et al., Citation2023; Richards & Banas, Citation2015; Richards et al., Citation2017, Citation2021), we did not find inoculation against reactance to be effective at reducing state reactance or increasing willingness to engage in the promoted health behavior, although our inoculation text was nearly identical to one that has been employed successfully in previous studies (Richards et al., Citation2017, Citation2021). In contrast to prior research, the health topic in the present study was hypothetical, which may account for the discrepancies between the findings. Furthermore, the present study is the first to test inoculation against reactance toward vaccine-promoting messages. It has been shown that vaccination is a challenging topic for “conventional” inoculation research (i.e., inoculation against external messages). In a recent study in a sample of predominantly vaccine-positive individuals, Banas et al. (Citation2023) showed that inoculation successfully protected individuals from anti-vaccination propaganda, but not by increasing motivation to protect already held beliefs, as individuals were highly motivated to protect their beliefs regardless of inoculation. In other words, the inoculation proved to be effective, but not through the expected mechanism, potentially due to the polarized nature of the vaccination topic. Concerning inoculation against reactance, Richards et al. (Citation2017) speculated that some health topics might inherently be perceived as more freedom-threatening than others, and that this can increase the risk that reactance inoculations themselves are perceived as freedom-threatening. Inoculation interventions have also been found to be perceived as more manipulative than debunking interventions presented after misinformation or persuasion attempts (Bruns et al., Citation2023). Considering the polarized and politicized debate on vaccination, and the existence of vaccine mandates, it is possible that vaccination is perceived as a freedom-threatening topic. This could increase the risk that reactance inoculations are perceived as manipulative and render them less effective. Our post-hoc analysis even suggested that the inoculation backfired for some participants, as the inoculated participants were more likely than the uninoculated ones to lower their vaccination willingness after receiving information about the vaccine. Future research should investigate the relevance of the inherent threat of different health topics for inoculation against reactance, as well as examine the conditions under which inoculation could be effectively applied within the vaccination context. For example, Amazeen et al. (Citation2022) have shown that generic inoculations (including only a warning) can be more effective than specific inoculations (including both a warning and a refutation) when preexisting attitudes are negative. It has also been shown that inoculation against reactance triggers both affective (i.e., fear) and cognitive (i.e., the formation of counterarguments) responses to threat and that these have opposing mediating effects on how the subsequent health message is perceived (Richards & Banas, Citation2018). A greater affective response can lead to more negative perceptions of the message, whereas a greater cognitive response can result in more favorable ones. Future research could therefore examine generic inoculations against reactance and formulate inoculation messages to inhibit affective and promote cognitive responses. This might be particularly important for high-threat health topics.
In the present study, high-reactant participants reacted especially negatively when the vaccination campaign message was framed to pose a large threat to freedom. For low-reactant individuals, the differences in vaccination willingness between the threat framings were smaller, and the high-threat message even resulted in a higher willingness to vaccinate than the medium-threat framing. Similar results were obtained in a previous study with a similar design (Soveri et al., Citation2023). Low-reactant participants in that study became more willing to get vaccinated after receiving vaccine information when the vaccination was framed as mandatory, whereas high-reactant participants did not change their stance on vaccination. Taken together, these two studies suggest that mandatory vaccination, or messaging that poses a high threat to freedom, can have positive effects for low-reactant individuals, but negative for high-reactant ones.
Contrary to expectations, the low-threat message did not mitigate the effects of trait reactance compared to the medium-threat message. This is also in line with the study by Soveri et al. (Citation2023). Highlighting voluntariness does thus not seem superior in mitigating reactance compared to recommending vaccines. This may be due to the fact that both studies were conducted in a context where no vaccines are mandatory for the general population, thereby leading to vaccine recommendations being interpreted as voluntary by default. The effectiveness of messages of this type might depend on the vaccine policies in place.
While strong recommendations and mandatory vaccination might increase vaccination willingness among those less prone to experience reactance, finding ways to mitigate reactance is important for ensuring successful vaccination campaigns and high vaccine uptake. Reactance can have consequences that extend beyond willingness to accept the targeted vaccine, as experimental research has found that vaccine-promoting messages that induce state reactance lower intentions to accept other (unmentioned) vaccines and decrease willingness to engage in other health-protecting behaviors (Sprengholz et al., Citation2021). Future research should investigate how to balance messaging to maximize vaccine uptake. In particular, solutions are needed to mitigate the negative effects of high trait reactance on the effectiveness of vaccination campaigns without sacrificing the positive effects that vaccine recommendations have for low-reactant individuals.
Supplementary Material.docx
Download MS Word (596.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are openly available at the Open Science Framework at https://osf.io/ybh8c/.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10410236.2024.2325185
Additional information
Funding
References
- Amazeen, M. A., Krishna, A., & Eschmann, R. (2022). Cutting the bunk: Comparing the solo and aggregate effects of prebunking and debunking COVID-19 vaccine misinformation. Science Communication, 44(4), 387–417. https://doi.org/10.1177/10755470221111558
- Banas, J. A., Bessarabova, E., Penkauskas, M. C., & Talbert, N. (2023). Inoculating against anti-vaccination conspiracies. Health Communication, 1–9. https://doi.org/10.1080/10410236.2023.2235733
- Banas, J. A., & Rains, S. A. (2010). A meta-analysis of research on inoculation theory. Communication Monographs, 77(3), 281–311. https://doi.org/10.1080/03637751003758193
- Betsch, C., & Böhm, R. (2016). Detrimental effects of introducing partial compulsory vaccination: Experimental evidence. The European Journal of Public Health, 26(3), 378–381. https://doi.org/10.1093/eurpub/ckv154
- Betsch, C., Schmid, P., Heinemeier, D., Korn, L., Holtmann, C., Böhm, R., & Angelillo, I. F. (2018). Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. Public Library of Science One, 13(12), 1–32. https://doi.org/10.1371/journal.pone.0208601
- Brehm, S. S., & Brehm, J. W. (1981). Psychological reactance: A theory of freedom and control. Academic Press.
- Bruns, H., Dessart, F. J., Krawczyk, M., Lewandowsky, S., Pantazi, M., Pennycook, G., Schmid, P., & Smillie, L. (2023). The role of (trust in) the source of prebunks and debunks of misinformation. Evidence from online experiments in four EU countries. OSF Preprints. https://doi.org/10.31219/osf.io/vd5qt
- Clayton, R. B., Compton, J., Reynolds-Tylus, T., Neumann, D., & Park, J. (2023). Revisiting the effects of an inoculation treatment on psychological reactance: A conceptual replication and extension with self-report and psychophysiological measures. Human Communication Research, 49(1), 104–111. https://doi.org/10.1093/hcr/hqac026
- Compton, J. (2013). Inoculation theory. In J. P. Dillard & L. Shen (Eds.), The SAGE handbook of persuasion: Developments in theory and practice (2nd ed., pp. 220–236). SAGE Publications, Incorporated.
- Compton, J. (2021). Threat and/in inoculation theory. International Journal of Communication, 15, 4294–4306. http://ijoc.org
- Drążkowski, D., & Trepanowski, R. (2022). Reactance and perceived disease severity as determinants of COVID-19 vaccination intention: An application of the theory of planned behavior. Psychology, Health & Medicine, 27(10), 2171–2178. https://doi.org/10.1080/13548506.2021.2014060
- Finkelstein, S. R., Boland, W. A., Vallen, B., Connell, P. M., Sherman, G. D., & Feemster, K. A. (2020). Psychological reactance impacts ratings of pediatrician vaccine-related communication quality, perceived vaccine safety, and vaccination priority among U.S. parents. Human Vaccines and Immunotherapeutics, 16(5), 1024–1029. https://doi.org/10.1080/21645515.2019.1694815
- Hong, S.-M., & Page, S. (1989). A psychological reactance scale: Development, factor structure and reliability. Psychological Reports, 64(3_suppl), 1323–1326. https://doi.org/10.2466/pr0.1989.64.3c.1323
- Hornsey, M. J., Harris, E. A., & Fielding, K. S. (2018). The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychology, 37(4), 304–315. https://doi.org/10.1037/hea0000586
- Lewandowsky, S., & van der Linden, S. (2021). Countering misinformation and fake news through inoculation and prebunking. European Review of Social Psychology, 32(2), 348–384. https://doi.org/10.1080/10463283.2021.1876983
- Pekrun, R., Vogl, E., Muis, K. R., & Sinatra, G. M. (2017). Measuring emotions during epistemic activities: The epistemically-related emotion scales. Cognition and Emotion, 31(6), 1268–1276. https://doi.org/10.1080/02699931.2016.1204989
- R Core Team. (2022). R: A language and environment for statistical computing. https://www.R-project.org/
- Reynolds-Tylus, T. (2019). Psychological reactance and persuasive health communication: A review of the literature. Frontiers in Communication, 4. https://doi.org/10.3389/fcomm.2019.00056
- Richards, A. S., & Banas, J. A. (2015). Inoculating against reactance to persuasive health messages. Health Communication, 30(5), 451–460. https://doi.org/10.1080/10410236.2013.867005
- Richards, A. S., & Banas, J. A. (2018). The opposing mediational effects of apprehensive threat and motivational threat when inoculating against reactance to health promotion. Southern Communication Journal, 83(4), 245–255. https://doi.org/10.1080/1041794X.2018.1498909
- Richards, A. S., Banas, J. A., & Magid, Y. (2017). More on inoculating against reactance to persuasive health messages: The paradox of threat. Health Communication, 32(7), 890–902. https://doi.org/10.1080/10410236.2016.1196410
- Richards, A. S., Bessarabova, E., Banas, J. A., & Larsen, M. (2021). Freedom-prompting reactance mitigation strategies function differently across levels of trait reactance. Communication Quarterly, 69(3), 238–258. https://doi.org/10.1080/01463373.2021.1920443
- Roozenbeek, J., Van Der Linden, S., & Nygren, T. (2020). Prebunking interventions based on “Inoculation” theory can reduce susceptibility to misinformation across cultures. Harvard Kennedy School Misinformation Review. https://doi.org/10.37016//mr-2020-008
- Rosenberg, B. D., & Siegel, J. T. (2018). A 50-year review of psychological reactance theory: Do not read this article. Motivation Science, 4(4), 281–300. https://doi.org/10.1037/mot0000091
- Rosseel, Y. (2012). Lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(2), 1–36. https://doi.org/10.18637/jss.v048.i02
- Soveri, A., Karlsson, L. C., Mäki, K. O., Holford, D., Fasce, A., Schmid, P., Antfolk, J., Karlsson, L., Karlsson, H., Nolvi, S., Karukivi, M., Lindfelt, M., & Lewandowsky, S. (2023). Trait reactance as psychological motivation to reject vaccination: Two longitudinal studies and one experimental study. Applied Psychology: Health and Well-Being. https://doi.org/10.1111/aphw.12506
- Soveri, A., Karlsson, L. C., Mäki, O., Antfolk, J., Waris, O., Karlsson, H., Karlsson, L., Lindfelt, M., Lewandowsky, S., & Jonason, P. K. (2020). Trait reactance and trust in doctors as predictors of vaccination behavior, vaccine attitudes, and use of complementary and alternative medicine in parents of young children. Public Library of Science One, 15(7), 1–16. https://doi.org/10.1371/journal.pone.0236527
- Sprengholz, P., & Betsch, C. (2020). Herd immunity communication counters detrimental effects of selective vaccination mandates: Experimental evidence. EClinicalMedicine, 22, 22. https://doi.org/10.1016/j.eclinm.2020.100352
- Sprengholz, P., Betsch, C., & Böhm, R. (2021). Reactance revisited: Consequences of mandatory and scarce vaccination in the case of COVID-19. Applied Psychology: Health and Well-Being, 13(4), 986–995. https://doi.org/10.1111/aphw.12285
- Sprengholz, P., Felgendreff, L., Böhm, R., & Betsch, C. (2022). Vaccination policy reactance: Predictors, consequences, and countermeasures. Journal of Health Psychology, 27(6), 1394–1407. https://doi.org/10.1177/13591053211044535
- Statistics Finland. (2024a). Educational structure of population. https://stat.fi/en/statistics/vkour
- Statistics Finland. (2024b). Population and society. https://www.tilastokeskus.fi/tup/suoluk/suoluk_vaesto_en.html
- Steindl, C., Jonas, E., Sittenthaler, S., Traut-Mattausch, E., & Greenberg, J. (2015). Understanding psychological reactance: New developments and findings. Zeitschrift für Psychologie, 223(4), 205–2014. https://doi.org/10.1027/2151-2604/a000222
- Waris, O., Karlsson, L., Antfolk, J., Karlsson, L., Karlsson, H., & Soveri, A. (2021). The factorial structure of the Hong Psychological Reactance Scale in two Finnish samples. Nordic Psychology, 73(1), 68–90. https://doi.org/10.1080/19012276.2020.1800508
- WHO. (2019). Ten Threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
