Abstract
Context
Wearable cameras have great potential for producing novel outcome measures of upper limb (UL) function and guiding care in individuals with cervical spinal cord injury (cSCI) living in the community. However, little is known about the perspectives of individuals with cSCI on the potential adoption of this technology.
Objective
To analyze feedback from individuals with cSCI regarding the use of wearable cameras to record daily activities at home, in order to define guidelines for improving the design of this technology and fostering its implementation to optimize UL rehabilitation.
Design
Mixed-methods study.
Participants
Thirteen adults with cSCI C3-C8 AIS A-D impairment.
Measures
Interview including survey and semi-structured questions.
Results
Participants felt that this technology can provide naturalistic information regarding hand use to clinicians and researchers, which in turn can lead to better assessments of UL function and optimized therapies. Participants described the technology as easy-to-use but often reported discomfort that prevented them from conducting long recordings of fully natural activities. Privacy concerns included the possibility to capture household members and personal information displayed on objects (e.g. smartphones).
Conclusion
We provide the first set of guidelines to help researchers and therapists understand which steps need to be taken to translate wearable cameras into outpatient care and community-based research for UL rehabilitation. These guidelines include miniaturized and easy-to-wear cameras, as well as multiple measures for preventing privacy concerns such as avoiding public spaces and providing control over the recordings (e.g. start and stop the recordings at any time, keep or delete a recording).
Introduction
Cervical spinal cord injury (cSCI) causes paralysis of the upper limbs, trunk and lower limbs, and varying degrees of autonomic dysfunction which significantly reduce an individual’s quality of life and community participation.Citation1,Citation2 Regaining functional use of the upper limbs (ULs) is the top recovery priority for most individuals with cSCI,Citation3,Citation4 as this would allow them to be independent with their activities of daily living (ADLs) and instrumental ADLs (iADLs).Citation5
Several challenges prevent the optimal recovery of UL function. Due to healthcare system pressures, patients are often discharged from inpatient rehabilitation to home prior to attaining optimal neurological and functional ability.Citation6–8 As well, improvements in UL motor functions observed in the clinic have been shown not to necessarily translate into an increased functional use of ULs during ADLs.Citation9 It would therefore be highly beneficial if UL condition could be monitored in the community to better understand how people with cSCI perform their day-to-day tasks in the home. This information could lead to the development of optimal rehabilitation strategies through personalized insights into the challenges encountered in the home and the strategies used to address them. Unfortunately, the distances between patient homes and rehabilitation centers,Citation10 which are often distant from one another, constitute an additional barrier to tracking the UL recovery in the home environment. A possible solution is to capitalize on the increased interest in technologies for monitoring function in the home environment when distances are too great and/or access to outpatient services is limited.Citation11–13
Wearable devices have been used to describe activity or produce outcomes reflecting UL function during ADLs and iADLs in individuals with SCI and post-stroke.Citation14–19 Several authors proposed the use of accelerometers or inertial measurement units which are comfortable and can be used for several hours in free-living conditions.Citation14,Citation16,Citation19 Although advantageous for studying global kinematics of ULs, these devices fail to provide detailed information regarding hand and finger movements, as well as the context of functional use of the hands. Technologies such as sensorized gloves,Citation18 which capture hand movements in greater detail, may instead be cumbersome and inconvenient for people whose hand function and sensation are impaired.
To fill the above gaps, wearable cameras (i.e. cameras mounted on the head) have been used to capture the functional use of the hands during ADLs and iADLs in people with cSCI.Citation20–23 A salient feature of the first-person vision paradigm (a.k.a. egocentric vision) is that the camera movements are driven by the user’s attention, which results in video recordings focused on the hands and manipulated objects.Citation20,Citation24 Moreover, the possibility to obtain rich observational data of functional use of the hands is another advantage for implementing this technology in clinical decision making.Citation25
Recent work demonstrated the ability of computer vision to track the user’s hands,Citation22 detect functional hand-object interactions,Citation23,Citation26,Citation27 and identify the presence of tenodesis grasp.Citation21 These approaches constitute the basis for producing new strategies to monitor rehabilitation progress in people with cSCI living in the community and reporting novel outcome measures of UL function.Citation23
Although wearable video-based technology yielded promising results in the context of UL rehabilitation, we still have sparse information about its acceptability among individuals with cSCI, as well as feedback and concerns regarding its potential adoption during daily life. These aspects are of critical importance for integrating novel technologies into everyday life, especially in this case, where privacy concerns may arise from recording video at home.Citation28,Citation29 A previous study, in which video recordings were conducted in a home simulation laboratory following standardized protocols,Citation30 collected views of individuals with cSCI on the use of wearable cameras for monitoring UL function and reported concerns related to privacy and comfort. Regardless, the participants strongly believed that this technology could provide useful information for clinical and research applications. However, those video recordings were not subject to the challenges of the built environment, family members, or caregivers in the environment.Citation30
Given the potential contributions of wearable technology for optimizing UL rehabilitation in cSCI, there is a need to further explore its applicability in naturalistic settings. To date, information about the experiences of individuals with cSCI using wearable cameras at home has been limited to a pilot study of three individuals.Citation31 Thus, our aim was to obtain feedback from individuals with cSCI who used wearable cameras in their homes to record unscripted activities, and to extrapolate key findings into a set of guidelines for improving how this technology can be designed and implemented to optimize UL rehabilitation. These guidelines are intended for clinicians working in outpatient SCI clinics and researchers developing wearable technologies for monitoring UL function remotely.
Materials and methods
Participants
Inclusion criteria are reported in . Eligible participants were contacted over the phone based on the research volunteer pool information provided by the centralized recruitment department at UHN – Toronto Rehabilitation Institute. Individuals interested in participating in this study were invited to the rehabilitation center for a first meeting where they were assessed using the Spinal Cord Independence Measure III (SCIM)Citation32 and the Graded Redefined Assessment of Strength, Sensibility and Prehension (GRASSP).Citation33 The International Standards for Neurological Classification of SCI (ISNCSCI)Citation34 were extracted from clinical charts when available or self-reported. Thirteen individuals with cSCI were recruited. A summary of clinical and demographic information is reported in . The study was approved by the Research Ethics Boards at the UHN – Toronto Rehabilitation Institute. All participants signed informed consent according to the requirements of the Declaration of Helsinki. Any household members or caregivers who appeared in the videos also provided signed informed consent.
Table 1 Inclusion and exclusion criteria for this study.
Table 2 Demographic and clinical information of the participants (UEMS = Upper Extremity Motor Score; T/NT: Traumatic/Non-Traumatic).
Study design
A detailed description of the acquisition protocol is described in Tsai et al.Citation35 Briefly, participants agreed to record their normal daily routine at home using a head-mounted camera (GoPro® Hero5 Black). Specifically, they were asked to record three videos of approximately 1.5 h each, over a two-week period, that would include them performing ADLs or iADLs that involved the use of hands. The content of the recordings was chosen collaboratively between the participants and researchers.Citation35 Participants were also trained to use a tablet (ASUS® ZenPad™ 8″ 16GB) with pre-installed GoPro® application, which allowed them to start and stop the recordings at any time, make sure their hands were visible, and review and edit the recordings before returning the equipment. Examples of activities collected in this study included: feeding, brushing teeth, washing hands, doing the laundry, cleaning, and preparing meals.
Upon returning the equipment, participants were interviewed using a survey and semi-structured questions. The interview outline was designed to explore participants’ opinions about privacy considerations and concerns surrounding the use of wearable cameras in the home, the perceptions of usefulness of this approach, and usability aspects related to wearing an egocentric camera during ADLs and iADLs.
Interview guide and data collection
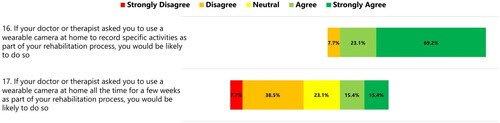
The interview outline is shown in the Appendix. The survey was composed of 17 statements to which participants responded by indicating the level of agreement on a five-point Likert scale (1-strongly disagree, 2-disagree, 3-neutral, 4-agree, and 5-strongly agree). The statements explored different aspects regarding the use of wearable cameras for monitoring UL function at home, for example: concerns about the use of recorded videos by clinicians and researchers (statements 1-4); comfort wearing a first-person camera at home or in public (statements 5-6); usefulness of letting researchers and clinicians access video data (statements 7-9); importance and difficulties of collecting and reviewing the videos (statements 10-13); interference with routine and household members (statements 14-15); and intended use of the technology if prescribed by doctors or therapists (statements 16-17).
The semi-structured questions were designed based on the Consolidated Framework for Implementation Research (CFIR).Citation36 This framework identifies factors that might influence the successful implementation of an intervention and allows us to interpret how the systematic uptake of research can be implemented into daily practice to improve quality and effectiveness of health services. Details elicited by the questions were in line with four main categories of the CFIR: outer settings – patient needs and resources (question 1); intervention characteristics (question 2); characteristics of individuals – knowledge and beliefs about the intervention (questions 3 and 4); and process (question 5). A sixth question was included to gather feedback not covered by the previous ones. Probes were used to explore the items into greater detail and to verify the interviewer’s understanding of the collected information. Each interview lasted approximately 30 min and was conducted in person at the participant’s home by the team member who trained the participants to use the technology (AB, whose background is in biomedical engineering). All interviews were audio-recorded and transcribed verbatim.
Data analysis
Mixed-methods analysisCitation37 was chosen to obtain a quantitative understanding of participants’ perceptions of using the wearable camera and to depict their overall satisfaction with the experience. Qualitative interviews were used to better elucidate the survey responses as well as to gain an in-depth understanding of the full experience. From this analysis we extrapolated key findings into a set of guidelines for improving how this technology can be designed and implemented to optimize UL rehabilitation.
Two members of the research team (AB, SLH) conducted a qualitative content analysisCitation38,Citation39 of the transcripts to identify the major themes of the interviews. First, the researchers independently read three transcripts to obtain an overview of the data and identify emerging and recurrent aspects pertaining the study.Citation39 Afterwards, these transcripts were thoroughly reviewed, sections of interest within the text were highlighted, and descriptive code was assigned to them. The two coders met to identify an initial coding framework, which was then used to independently code another three transcripts. Subsequent meetings and coding exercises produced a final version of the coding framework after three iterations. The final coding framework was re-applied to all the transcripts. Agreement between the two coders was consistently high and discrepancies were easily resolved. Themes were identified as a recurring category or connection made between the categories.Citation38 Investigator triangulation was used at each stage of the analysis process to ensure the trustworthiness of the data.Citation39
Results
Survey results
Summaries of the survey results are reported in . Most of the participants (61.5–69.3%) expressed little concern about having data of their daily life used by clinicians and researchers for monitoring hand function, regardless of the type of information being accessed (i.e. raw videos or summary measures of hand function, ). Moreover, participants would be more comfortable wearing a first-person camera at home than in public ().
Figure 1 Distribution of responses to statements 1 to 4 (concerns about the use of recorded videos by clinicians and researchers).
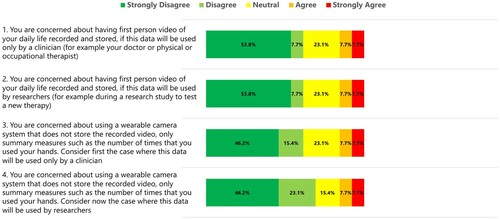
Figure 2 Distribution of responses to statements 5 and 6 (comfort wearing a first-person camera at home and in public).
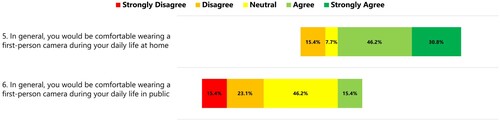
Figure 3 Distribution of responses to statements 7 to 9 (usefulness of letting researchers and clinicians access video data).
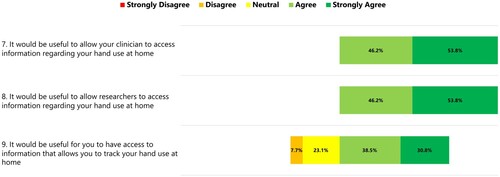
Figure 4 Distribution of responses to statements 10 to 13 (importance and difficulties of collecting and reviewing the videos).

Figure 5 Distribution of responses to statements 14 and 15 (interference with ADLs and household members).
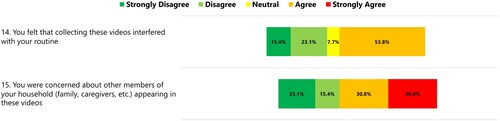
Figure 6 Distribution of responses to statements 16 and 17 (intended use of the technology if prescribed by a doctor or therapist).
All participants agreed that it would be useful to let researchers and clinicians access information regarding hand use at home. However, participants reported lower agreement when asked if they would find it useful to access this information ().
Regarding the importance and difficulties of collecting and reviewing videos, 69.3% of participants considered this technology easy-to-use (statement 10, ). The percentage of disagreement and neutral responses was higher when participants were asked if it was easy or important to review the videos before sharing them with researchers (statements 11 and 13, ). Instead, all participants agreed that it was important to start and stop the recordings at any time (statement 12, ).
Conflicting responses were obtained when exploring the interference of technology with routine (statements 14, ). In fact, 53.8% of participants felt that collecting videos interfered with their routine, whereas the rest of them either disagreed or gave neutral response. Most of participants (61.6%) expressed concern for the presence of household members in the video (statements 15, ).
Regarding the potential use of the technology if prescribed by a doctor or therapist, there was an overall agreement by the participants that they would use this technology if it were prescribed for recording specific activities at home. Conversely, participants showed less willingness to use it at home all the time for a few weeks as part of the rehabilitation process ().
Semi-structured interview results
The qualitative analysis of the interviews identified four themes related to the design and use of wearable cameras for capturing functional use of the hands at home: (1) Comfort and technical aspects (with 3 sub-themes – likes, dislikes, suggestions for improvement); (2) Privacy; (3) Impact on routine; and (4) Added value of the technology. For each theme, selected illustrative quotes are reported in .
Table 3 Illustrative quotes for Theme 1 – comfort and technical aspects.
Table 4 Illustrative quotes for Theme 2 – privacy.
Table 5 Illustrative quotes for Theme 3 – impact on routine.
Table 6 Illustrative quotes for Theme 4 – added value of technology.
Theme 1 – comfort and technical aspects
This area focused on the practical aspects related to the use of this technology, physical comfort in wearing the camera during data collection at home, and consideration on its design. One of the main aspects was the support needed for using the wearable camera. It emerged that participants with poor hand function often needed help from caregivers or household members to don and doff the camera (, quote 1).
Three sub-themes were identified: (1) Likes (i.e. what did participants like of the technology?); (2) Dislikes (i.e. what did participants not like of the technology?); and (3) Suggestions for improvement. When talking about the positive aspects of the technology, there was almost a complete agreement by participants that the technology was easy to use or that its use got easier over time.
Several participants found the camera uncomfortable for periods longer than 30 min, mostly because of its weight and overheating on the forehead. Other negative aspects were the limited battery life (approximately 1.5–2 h) and the awareness that sound was also being recorded (, quotes 2–4).
Suggestions for improvement focused on potential strategies to alleviate some of the above issues, such as having lighter and less intrusive cameras that would be easier to don and doff, and that could conduct longer recordings to capture more natural behaviors. Extending battery life and avoiding the recording of sounds were also noted (, quotes 5–7).
Theme 2 – privacy
This theme explored privacy-related issues that may arise from recording videos of daily routine at home. Participants identified several positive aspects that helped prevent privacy concerns and alleviated the worries of collecting video during daily routines at home, for example: the egocentric point of view of the camera, which did not show the user’s face; the possibility to start and stop the recording at any time; and detailed orientation and instructions from the research team (e.g. avoiding or stop recording during certain activities or in public places) (, quotes 1–2).
Despite these aspects, major privacy concerns emerged from the interviews. The possibility to record other people’s faces, especially if they did not consent to be part of the study, was concerning. Moreover, the possibility to capture objects that carry any sort of personal information (identity documents, phone numbers, etc.), and recording the audio were flagged as worrisome (, quotes 2–5).
Theme 3 – impact on routine
This theme focused on how the technology influenced the way activities were conducted at home during the data collection. Although one of the instructions given to participants before data collection was to conduct a normal routine without doing anything out of the ordinary,Citation35 it emerged that participants often planned their activities beforehand or conducted a higher than usual number of activities consecutively to fit the recording schedule ().
Theme 4 – added value of technology
There was wide consensus among participants on the fact that recording videos while conducting activities at home was the benefit of this technology. Participants believed that hand use information captured within a natural context would allow clinicians and therapists to improve their understanding of hand function in real world conditions, conduct better assessments, and optimize interventions (, quotes 1–3). Moreover, the possibility to quantify hand use over time was seen by some participants as another benefit for individuals with cSCI, who could use this technology as an incentive for pursuing hand rehabilitation, by checking their improvements over time (, quote 4).
Discussion
This mixed-methods study has provided important insights on the acceptability and potential use of wearable cameras to observe UL function in persons with cSCI in their home environments.
Regarding the technology itself, most of the participants felt it was quite easy to use. A salient issue that arose, however, was that participants required assistance to wear the headband, especially those with reduced hand function. This aspect was anticipated by the research team, which provided training (when necessary) to family members and/or caregivers through a preliminary meeting or phone calls.Citation35 Tactile and thermal discomfort often arose after wearing the camera over time. Several participants suggested that smaller and easier-to-wear cameras would improve independence in using the device as well as its usability for longer recordings.
In line with previous studies,Citation28–30 privacy arose as a major concern when collecting videos of ADLs and iADLs at home. However, concerns were not primarily related to their own personal privacy, as participants were willing to share videos of themselves for research and clinical purposes. They felt that the collected information could help clinicians conduct better assessments of UL function, thereby optimizing therapies. Participants also felt that the egocentric point of view of the camera and the possibility to control the recordings protected them from personal privacy issues. The major concerns, instead, were directed towards their surrounding environment, such as invading the privacy of household members, capturing objects with personal information (e.g. computer’s and smartphone’s screens), and recording audio of conversations. These issues can be partially alleviated if recordings are limited to within domestic environments (as suggested by responses to statements 5–6, ) and audio is disabled during data collection. More sophisticated pre-processing would be required to alleviate concerns related to other people and personal information, for example by automatically detecting and blurring faces and specific objects in the video via computer vision algorithms.Citation40,Citation41
In addition to the presence of other people, discomfort in wearing the camera was the main factor that influenced the natural execution of ADLs and iADLs. Several participants felt that collecting videos interfered with their routine (responses to statement 14, ). This fact was further accounted by the qualitative interviews where most participants expressed that camera’s weight and overheating were constant reminders that a device was on their heads. Moreover, battery constraints pushed participants to plan and concentrate more activities within a restricted amount of time (). Nevertheless, participants confirmed that activities collected in the video reflected parts of their normal routine, and that planning might have caused only alterations in the timing of these activities rather than the type. We believe that less intrusive and easier to wear cameras, along with longer battery life, will facilitate the recording of natural activities in addition to solve problems related to discomfort.
Although planning might have been a drawback for recording natural behaviors, in some cases it might have helped alleviate some privacy concerns, as participants were aware of what they recorded. As a result, more than 30% of them felt there was no need to review the videos before sharing them with researchers, as indicated by the neutral and negative responses to statements 11 and 13 (). This point raises an interesting fact: smaller and less intrusive cameras might not be the panacea for all problems. While with smaller cameras it will certainly be easier to slip into more naturalistic behaviors, it will also be easier to forget them on while recording, increasing the chances of inadvertent privacy incidents. A trade-off must be found, for example equipping smaller cameras with cues that remind the user about ongoing recordings. However, given the preference of most participants to record shorter chunks, and avoid using the camera all the time as part of the rehabilitation (see prevalence of disagreement to statement 17, ), we also believe that freedom in starting and stopping the recordings should be maintained for the user, after agreeing with therapists on which activities require more attention.
In terms of added value of this technology, wide consensus was found on the fact that this technology can provide more naturalistic information regarding hand use to clinicians or researchers, which in turn can lead to better assessments and optimized therapies. Some participants also felt that this technology could provide direct advantage for patients, as the visualization of the patterns of hand function over time, especially in case of improvements during rehabilitation, can help them feel a sense of achievement to further incentivize rehabilitation participation.
Given the above findings, we have proposed a set of guidelines on how to integrate egocentric cameras into outpatient care and research for monitoring UL function in individuals with cSCI living in the community (see ).
Table 7 Guidelines for integration of egocentric cameras into outpatient rehabilitation and research for monitoring UL function of individuals with cSCI.
Limitations and future work
The main limitation of this study was the inclusion of only one female participant, which did not allow us to carry out any sex-based analysis. The reduced sample size, the limited age range (44–63 years old), and the prevalence of individuals with AIS grade D were additional limitations. With larger samples it will be interesting to investigate potential relationships between participant’s responses, age, level of injury, and AIS grade.
Conclusion
We analyzed feedback from individuals with cSCI who used a wearable camera for recording ADLs and iADLs at home in the context of UL rehabilitation. The perceived potential of the approach was high, and the privacy considerations tractable, supporting earlier findings. Although egocentric vision has great potential for extracting novel outcome measures of UL function, several steps still need to be taken to translate the technology into outpatient care and community-based research. From this study, we provide the first set of guidelines to help researchers understand what these steps are. We are confident that with constant developments in hardware miniaturization and artificial intelligence, it will soon be easy to fulfill the suggested requirements to develop wearable video-based technology for remote monitoring of UL function in people with cSCI living in the community.
Disclaimer statements
Contributors None.
Funding This work was supported by the Craig H. Neilsen Foundation [grant number 542675].
Conflicts of interest SKR is the CEO of Neural Outcomes Consulting Inc. which is the manufacturer of GRASSP products. The other authors report no conflicts of interest.
Acknowledgements
The authors would like to thank Matt Heffernan for his valuable assistance in transcribing the interviews, and all the participants and their families involved in the study.
References
- Fougeyrollas P, Noreau L. Long-term consequences of spinal cord injury on social participation: the occurrence of handicap situations. Disabil Rehabil. 2000;22(4):170–80.
- Carpenter C, Forwell SJ, Jongbloed LE, Backman CL. Community participation after spinal cord injury. Arch Phys Med Rehabil 2007;88(4):427–33.
- Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004;21(10):1371–83.
- Snoek GJ, Ijzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F. Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004;42(9):526–32.
- American Occupational Therapy Association. Framework: domain & process. Am J Occup Ther 2014.
- Munce SEP, Wodchis WP, Guilcher SJT, Couris CM, Verrier M, Fung K, et al. Direct costs of adult traumatic spinal cord injury in ontario. Spinal Cord 2013;51(1):64–9.
- Burns AS, Yee J, Flett HM, Guy K, Cournoyea N. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord 2013;51(2):165–9.
- Burns AS, Ditunno JF. Establishing prognosis and maximizing functional outcomes after spinal cord injury: A review of current and future directions in rehabilitation management. Spine 2001;26(24S):S137–45.
- Waddell KJ, Strube MJ, Bailey RR, Klaesner JW, Birkenmeier RL, Dromerick AW, et al. Does task-specific training improve upper limb performance in daily life poststroke? Neurorehabil Neural Repair 2017;31(3):290–300.
- Craven C, Verrier M, Balioussis C, Wolfe D, Hsieh J, Noonan V, et al. Rehabilitation environmental scan atlas: capturing capacity in Canadian SCI rehabilitation. Rick Hansen Inst 2012.
- Bell A, Grampurohit N, Marino RJ, Duff S, Kaplan G, Calhoun Thielen C, et al. Home activity-based interventions for the neurologically impaired upper extremity: a scoping review. Home Health Care Manage Practice 2020:1084822320953836.
- Patel S, Hughes R, Hester T, Stein J, Akay M, Dy JG, et al. A novel approach to monitor rehabilitation outcomes in stroke survivors using wearable technology. Proc IEEE 2010;98(3):450–61.
- Singh H, Musselman K, Colella TJF, McGilton KS, Iaboni A, Bayley M, et al. Exploring the perspectives of outpatient rehabilitation clinicians on the challenges with monitoring patient health, function and activity in the community. Disabil Rehabil 2020:1–10.
- Noorkõiv M, Rodgers H, Price CI. Accelerometer measurement of upper extremity movement after stroke: A systematic review of clinical studies. J Neuroeng Rehabil 2014;11(1):1–1.
- Brogioli M, Schneider S, Popp WL, Albisser U, Brust AK, Velstra IM, et al. Monitoring upper limb recovery after cervical spinal cord injury: insights beyond assessment scores. Front Neurol 2016;7:142.
- Popp WL, Brogioli M, Leuenberger K, Albisser U, Frotzler A, Curt A, et al. A novel algorithm for detecting active propulsion in wheelchair users following spinal cord injury. Med Eng Phys 2016;38(3):267–74.
- Friedman N, Rowe JB, Reinkensmeyer DJ, Bachman M. The manumeter: a wearable device for monitoring daily use of the wrist and fingers. IEEE J Biomed Heal Informatics 2014;18(6):1804–12.
- Oess NP, Wanek J, Curt A. Design and evaluation of a low-cost instrumented glove for hand function assessment. J Neuroeng Rehabil 2012;9(1):1–1.
- Lum PS, Shu L, Bochniewicz EM, Tran T, Chang LC, Barth J, et al. Improving accelerometry-based measurement of functional use of the upper extremity after stroke: machine learning versus counts threshold method. Neurorehabil Neural Repair 2020;34(12):1078–87.
- Bandini A, Zariffa J. Analysis of the hands in egocentric vision: a survey. IEEE Trans Pattern Anal Mach Intell [Internet] 2020: 1–1. Available from: https://ieeexplore.ieee.org/document/9064606/.
- Dousty M, Zariffa J. Tenodesis grasp detection in egocentric video. IEEE J Biomed Heal Informatics 2020.
- Visee RJ, Likitlersuang J, Zariffa J. An effective and efficient method for detecting hands in egocentric videos for rehabilitation applications. IEEE Trans Neural Syst Rehabil Eng 2020;28(3):748–55.
- Likitlersuang J, Sumitro ER, Cao T, Visée RJ, Kalsi-Ryan S, Zariffa J. Egocentric video: a new tool for capturing hand use of individuals with spinal cord injury at home. J Neuroeng Rehabil 2019;16(1):1–1.
- Nguyen THC, Nebel JC, Florez-Revuelta F. Recognition of activities of daily living with egocentric vision: a review. Sensors (Switzerland) 2016;16(1):72.
- McGinnis PQ, Hack LM, Nixon-Cave K, Michlovitz SL. Factors that influence the clinical decision making of physical therapists in choosing a balance assessment approach. Phys Ther 2009;89(3):233–47.
- Likitlersuang J, Zariffa J. Interaction detection in egocentric video: toward a novel outcome measure for upper extremity function. IEEE J Biomed Heal Informat 2018;22(2):561–69.
- Bandini A, Dousty M, Zariffa J. A wearable vision-based system for detecting hand-object interactions in individuals with cervical spinal cord injury: first results in the home environment. In: Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS; 2020 (pp. 2159–2162).
- Gelonch O, Ribera M, Codern-Bové N, Ramos S, Quintana M, Chico G, et al. Acceptability of a lifelogging wearable camera in older adults with mild cognitive impairment: a mixed-method study. BMC Geriatr 2019;19(1):1–10.
- Gupta R, Crane M, Gurrin C. Considerations on privacy in the era of digitally logged lives. Online Inf Rev 2021;45(2):278–296.
- Likitlersuang J, Sumitro ER, Theventhiran P, Kalsi-Ryan S, Zariffa J. Views of individuals with spinal cord injury on the use of wearable cameras to monitor upper limb function in the home and community. J Spinal Cord Med 2017;40(6):706–14.
- Likitlersuang J, Visée RJ, Kalsi-Ryan S, Zariffa J. Capturing hand use of individuals with spinal cord injury at home using egocentric video: A feasibility study. Spinal Cord Series and Cases. 2021;7(1):1–9.
- Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the spinal cord independence measure, version III: rasch psychometric validation. Spinal Cord 2007;45(4):275–91.
- Kalsi-Ryan S, Beaton D, Curt A, Duff S, Popovic MR, Rudhe C, et al. The graded redefined assessment of strength sensibility and prehension: reliability and validity. J Neurotrauma 2012;29(5):905–14.
- Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the International Standards for Neurological Classification of spinal cord injury. J Spinal Cord Medi 2011;34(6):547–54.
- Tsai M-F, Bandini A, Wang RH, Zariffa J. Capturing representative hand Use at home using egocentric video in individuals with upper limb impairment. J Vis Exp 2020;166:e61898.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci 2009;4(1):1–5.
- Wisdom J, Creswell JW. Integrating quantitative and qualitative data collection and analysis while studying patient-centered medical home models. Agency Healthc Res Qual 2013:13–0028.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004;24(2):105–12.
- Creswell JW, Creswell JD. Research design: Qualitative, quantitative, and mixed methods approaches. Sage publications; 2017 Nov 27.
- Uittenbogaard R, Sebastian C, Vijverberg J, Boom B, Gavrila DM, De With PHN. Privacy protection in street-view panoramas using depth and multi-view imagery. In: Proceedings of the IEEE Computer Society Conference on Computer Vision and Pattern Recognition; 2019 (pp. 10581–10590).
- Fan L. Practical image obfuscation with provable privacy. In: Proceedings – IEEE International Conference on Multimedia and Expo; 2019 (pp. 784–789).
Appendix
INTERVIEW GUIDE FOR PARTICIPANTS WITH SCI
Structured interview questions
How strongly do you agree or disagree with the following statements? [Strongly Disagree, Disagree, Neutral, Agree, Strongly Agree]
You are concerned about having first person video of your daily life recorded and stored, if this data will be used only by a clinician (for example your doctor or physical or occupational therapist).
You are concerned about having first person video of your daily life recorded and stored, if this data will be used by researchers (for example during a research study to test a new therapy).
You are concerned about using a wearable camera system that does not store the recorded video, only summary measures such as the number of times that you used your hands. Consider first the case where this data will be used only by a clinician.
You are concerned about using a wearable camera system that does not store the recorded video, only summary measures such as the number of times that you used your hands. Consider now the case where this data will be used by researchers.
In general, you would be comfortable wearing a first person camera during your daily life at home.
In general, you would be comfortable wearing a first person camera during your daily life in public.
It would be useful to allow your clinician to access information regarding your hand use at home.
It would be useful to allow researchers to access information regarding your hand use at home.
It would be useful for you to have access to information that allows you to track your hand use at home.
It was easy to use the wearable camera to record the videos at home (putting on the camera, controlling the recordings, etc.).
It was easy to review the videos before sharing them with the researchers.
It was important to you to be able to start and stop the recordings at any time.
It was important to you to be able to review the videos before sharing them with the researchers.
You felt that collecting these videos interfered with your routine.
You were concerned about other members of your household (family, caregivers, etc.) appearing in these videos.
If your doctor or therapist asked you to use a wearable camera at home to record specific activities as part of your rehabilitation process, you would be likely to do so.
If your doctor or therapist asked you to use a wearable camera at home all the time for a few weeks as part of your rehabilitation process, you would be likely to do so.
Before starting the study, what were your expectations about wearing a camera and letting researchers and clinicians observe your daily activities? PROMPTS: What did you hope to gain from it, if anything? What concerns, if any, did you have?
After participating in this study, what was it like using the wearable camera in your home? PROMPTS: Were your expectations met or did they change? What did you think about the overall design of the system? How easy was it to use? What supports, if any, did you need to use the technology (i.e. putting it on, taking it off, etc.)? Did it get easier over time? What was convenient? What was inconvenient?
What were your thoughts about issues of personal privacy while using the wearable camera? PROMPTS: Did wearing the camera change the way you would do things? Were there certain activities that you would use the camera and others where you would not? How did others living with you react/respond to the camera? What concerns, if any, do you have about how the data would be shared and used?
What aspects of using the wearable camera for capturing how you use your hands do you feel could be beneficial for helping clinicians and researchers to better understand what it means to have hand impairment? PROMPTS: Why or how do you think the information collected could be helpful to clinicians? How do you think researchers might be able to use the information? How do you think it might help others with hand impairments? How would you compare it to your experiences with traditional rehabilitation?
If there were not limits on money or the technology, what would be the ideal way to use wearable technology to help do assessments of your hand function in your natural environment (i.e. home, work, etc.)? PROMPTS: What kind of supports would you need, if any, to use it? What would the devices look like? How would you like them to be used? Where do you think they would be the most useful for helping clinicians better understand your needs?
Is there anything else about your experiences of participating in our wearable camera study that you would like to share but we didn’t touch upon?
