 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
The study objective was to assess the feasibility of stimulating the lower trapezius (LT), the upper trapezius (UT) and serratus anterior (SA) muscles along with anterior or middle deltoid, using surface functional electrical stimulation (FES). The secondary aim was to understand the effects of LT, UT, and SA stimulation on maximum arm reach achieved in shoulder flexion and abduction.
Design
Single arm interventional study.
Setting
Inpatient Rehabilitation Hospital.
Participants
Ten healthy volunteers.
Intervention
Participants completed 10 trials for each of the 3 conditions in flexion and abduction, i.e. (1) Active voluntary flexion or abduction, (2) FES for anterior deltoid for flexion or middle deltoid for abduction, and (3) FES for LT, UT, and SA along with anterior deltoid for flexion or middle deltoid for abduction.
Outcome Measures
Maximum arm reach and percent angle relative to the voluntary movement were computed from motion capture data for each condition. Wilcoxon signed-rank test was used to compare the maximum reach between two FES conditions.
Results
The study results showed that all three interscapular muscles can be stimulated using surface FES. Maximum reach in abduction was greater for FES of middle deltoid along with the interscapular muscles (51.77° ± 17.54°) compared to FES for middle deltoid alone (43.76° ± 15.32°; Z = −2.701, P = 0.007). Maximum reach in flexion for FES of anterior deltoid, along with interscapular muscles, was similar to that during FES of anterior deltoid alone.
Conclusion
Interscapular muscles can be stimulated using surface FES devices and should be engaged during rehabilitation as appropriate.
Introduction
Functional Electrical Stimulation (FES) for the rehabilitation of the upper extremity function was first proposed in 1963 by Long and Masciarelli,Citation1 to help compensate for the lost function. In the last 2–3 decades FES has been revolutionized with a shift of focus toward retraining the lost function. Examples of transcutaneous FES upper extremity systems include the (a) Neuromuscular Electrical Stimulation System (NESS) H200 or the NESS Handmaster,Citation2,Citation3 (b) Bionic Glove,Citation4 (c) Belgrade Grasping-Reaching System,Citation5 (d) Complex Motion Neuroprosthesis,Citation6 and (e) MyndMove.Citation7 Most of these systems are multi-channel systems that allow for the stimulation of multiple muscle groups and typically target grasping movements, while some support additional reaching movements. Target muscles stimulated are deltoid, biceps brachii, triceps brachii, wrist and finger extensors and finger flexors.
Interestingly, to date none of the transcutaneous FES systems have targeted the three key scapular muscles (lower and upper trapezius and serratus anterior),Citation8–11 even though these muscles play a vital role in producing scapular upward rotation and preventing superior translation of the humeral head during shoulder elevation movements. Decrease in the activity of the scapular muscles due to any pathology results in decreased strength and range of arm elevation.Citation12 One study stimulated the upper limb and one of the key interscapular muscles in patients with chronic stroke.Citation13 In that study Cuesta-Gómez et al., used a four-channel transcutaneous FES system to stimulate the triceps brachii, anterior deltoid, extensor muscles of the wrist, and fingers and the lower trapezius and rhomboid, in two different conditions, i.e. Placebo (lower amplitudes that did not produce muscle contraction) and the FES condition (higher amplitudes that produced a motor contraction).Citation13 The authors found that participants receiving FES performed the reaching movements with less trunk flexion, while shoulder flexion and elbow extension were increased. This study provides preliminary evidence related to the feasibility and potential benefits of stimulating scapular muscles using transcutaneous FES.
In our laboratory we have been retraining the upper extremity function in individuals with stroke and spinal cord injury,Citation14–17 using a fully programmable four-channel surface stimulator.Citation6 The FES protocols have targeted arm, forearm, and hand muscles,Citation14,Citation17 during task-specific movements while manipulating real-life objects. We have attempted to replicate movements using FES such that they closely follow the normal physiological pattern. This philosophy of stimulation had to be balanced against the number of stimulation channels available i.e. if the number of channels was limited, then we would only stimulate the prime movers pertinent to the movement performed. Now, with the stimulators having more than four channelsCitation7 it allows for the stimulation of multiple muscles/muscle groups to produce a closer to physiologically correct movement.
Arm elevation movements in both the frontal and sagittal planes are complex ones and involve the recruitment of various glenohumeral and scapular muscles. The deep rotator cuff muscles play an important role in glenohumeral joint compression and offsetting the superior translatory force of the deltoid during arm elevation.Citation12 The scapular muscles are responsible for optimal scapular positioning during different phases of arm elevation. The movement of the scapula on the thorax is essential for normal function of the upper extremity.Citation18 Among the muscles that surround and attach to the scapula, the upper trapezius (UT), the lower trapezius (LT), and the serratus anterior (SA) muscles are believed to be important for scapulothoracic motion.Citation19 Ebaugh et al. found that the LT, UT, and SA muscles play an important role in producing scapular upward rotation, especially throughout the mid-range of arm elevation.Citation20
In the upper extremity rehabilitation, clinicians are looking for ways to obtain normal shoulder elevation patterns. Studies looking at the contributions of scapulothoracic joints in performing activities of daily living (ADLs), such as feeding, reaching overhead, washing the back, and washing the contralateral axilla, have found that scapulothoracic upward rotation and anterior tipping contribute significantly to the completion of these tasks.Citation21 Hence clinicians working with patients, who present with difficulty in accomplishing ADLs, should consider intervening at these joints specifically. FES can engage the scapular muscles in a functional manner irrespective of muscle strength and severity of the condition.
The primary objective of our study was to test the feasibility of stimulating LT, UT, and SA muscles along with shoulder muscles using transcutaneous FES. We specifically assessed the (1) feasibility of stimulating the target muscles using surface electrodes; and (2) tolerance to stimulation as reported by adverse events. We also aimed to study the influence of scapular muscle FES on shoulder complex movement in able-bodied individuals. Specifically, we explored the effect of FES of LT, SA, and UT along with FES of the anterior deltoid, and middle deltoid on maximum reach during shoulder flexion and abduction, respectively. To the best of our knowledge, this is the first study that looks at stimulating these muscles using transcutaneous FES.
Methods
Ten able-bodied individuals with no history of shoulder injury and with full active and passive range of shoulder joint movement, were invited to participate in the study (). Participants were 18 years of age or older and provided written consent for participation. Participants recruited to the study took part in a single two-hour session. The set-up for the experiment consisted in: (a) identifying motor points for all the muscle groups and securing FES surface self-adhesive electrodes;(b) determining the sensory, motor, functional and maximum electrical stimulation threshold for all musclesCitation22; and (c) placing reflective markers for collecting the kinematic data.
A four-channel FES stimulator (Complex Motion, Switzerland) was used to stimulate the LT, UT, and SA, along with the anterior or middle deltoid muscles. Once the electrodes were secured and amplitude levels for individual muscles adjusted, the stimulator was operated using a push button by the study participant or a research assistant on cueing by the researcher operating the motion capture system. The FES parameters were as follows: stimulation frequency of 40 Hz, pulse duration of 250 µs, and stimulation intensity was determined by the strength of the contraction or participant tolerance to stimulation (range 20–50 mA, see for details).
The motor points and electrode positioning for FES for the various muscles were as follows ((a,b)):
Serratus Anterior (SA): Electrode between the latissimus dorsi and the pectoralis major, on the muscular bulk of the serratus between the 4th and 9th ribs.
Upper Trapezius (UT): On the superior aspect of the shoulder blade, away from the supero-medial angle of the scapula to limit stimulation of the levator scapulae muscle.
Lower Trapezius (LT): Medially and in line with the muscle fibers next to the spine of T8-T12 vertebrae below the inferior tip of the scapula, to limit stimulation of the rhomboids.
Anterior and middle deltoid: on the bulk of the muscle, one proximal and one distal.
Figure 1 Functional electrical stimulation electrodes and reflective marker placements. (a) Anterior view and (b) posterior view
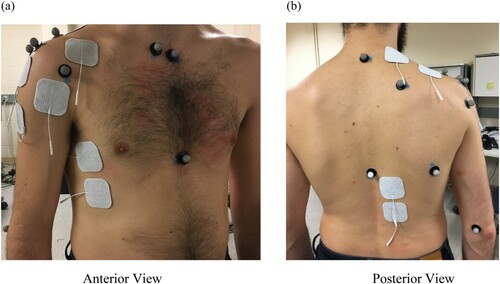
Three-dimensional kinematic data were recorded using Motion Analysis System (Motion Analysis™, USA). The system uses six infra-red cameras connected to the motion analysis data acquisition system. Calibration was carried out to define X-Y-Z reference for all six cameras prior to data collection. The International Society of Biomechanics’ recommended marker set for the upper extremity was used.Citation23 The specific marker locations were as follows ((a,b)):
C7: Processus Spinosus (spinous process) of the 7th cervical vertebra
T8: Processus Spinosus (spinal process) of the 8th thoracic vertebra
IJ: Deepest point of Incisura Jugularis (suprasternal notch)
PX: Processus Xiphoideus (xiphoid process), most caudal point on the sternum
SC: Most ventral point on the sternoclavicular joint
AC: Most dorsal point on the acromioclavicular joint (shared with the scapula)
TS: Trigonum Spinae Scapulae (root of the spine), the midpoint of the triangular surface on the medial border of the scapula in line with the scapular spine
AI: Angulus Inferior (inferior angle), most caudal point of the scapula
AA: Angulus Acromialis (acromial angle), most laterodorsal point of the scapula
PC: Most ventral point of processus coracoideus
Anterior GH: Anterior aspect of the head of the Humerus
Posterior GH: Posterior aspect of the head of the Humerus
EL: Most caudal point on lateral epicondyle
EM: Most caudal point on medial epicondyle
RS: Most caudal–lateral point on the radial styloid
US: Most caudal–medial point on the ulnar styloid
Experimental Conditions: Participants were seated on a wooden stool with the feet resting on the floor and arm hanging by the side of the body off the edge of the stool. Ten trials for each of the below conditions were performed by each study participant using their dominant arm in the order described under experimental conditions. For the FES conditions (experimental conditions: 2, 3, 5, and 6), the participants were instructed specifically not to exert any voluntary effort. FES was turned on with the arm in resting position on a count of 3 by operating a push button. Once maximum range was reached for each of the below conditions, the position was held for about 10 sec, until FES was turned off (experimental conditions: 2, 3, 5, and 6) or until the researcher asked the participant to lower their arm.
The experimental conditions were as follows:
No FES active flexion (i.e. full range forward flexion movement produced by the participant’s voluntary muscle contraction).
FES for anterior deltoid muscle only.
FES for anterior deltoid and scapular muscles (LT, UT, and SA) simultaneously.
No FES active abduction (i.e. full range abduction movement produced by the participant’s voluntary muscle contraction).
FES for middle deltoid muscle only.
FES for middle deltoid and scapular muscles (LT, UT, and SA) simultaneously.
The motion capture data were processed using Cortex software (Motion Analysis™, USA). Once the motion capture data were visually inspected and correct movement verified, then a template with a marker set was created. Each marker set was labeled using a frame in which all the markers were clearly visible and in the correct position. The template was used to rectify by extrapolating it into the remaining frames in the recording. This process was repeated for the first file of every data set for each participant. Markers in the remaining files were then identified using the template created. Once all markers were labeled for the entire data set, each individual file was reviewed to identify gaps which were then corrected using a linear, or cubic interpolation or a virtual joint function. Selection of the specific technique used to correct the gap was based on the size of the gap (i.e. number of missing samples) and the expected trajectory of the maker. Other elements that were corrected manually included mislabeled or swapped markers, as well as those displaying an unexpected movement.
Data analysis was performed using MATLAB (MathWorks®, USA). Marker positions (X, Y, and Z) for the anterior and posterior shoulder, the medial and lateral humeral epicondyle, the suprasternal notch, the xiphoid process, T8, and C7 were extracted. Two vectors were defined: one for the upper arm and one for the thorax. The upper arm vector was defined by the midpoint between the shoulder’s anterior and posterior markers, and the midpoint between the elbow’s medial and lateral epicondyle markers. The thorax vector was defined by the midpoint between the xiphoid process and T8, and the midpoint between the suprasternal notch and C7. The angle between the upper arm and thorax vectors was calculated for each frame as the inverse cosine of the dot product of both vectors divided by the product of the magnitude of both vectors: . The maximum reach of the arm was defined as the maximum angle achieved. This analysis was performed for all trials of all study participants.
Statistical Analysis: Means for maximum reach across all ten trials for all ten participants for all conditions were computed. Wilcoxon signed-rank test was used to compare the scores between anterior deltoid and anterior deltoid+ LT + UT + SA as well as between middle deltoid and middle deltoid + LT + UT + SA conditions. We also calculated the percentage of movement achieved during all FES conditions relative to the study participants’ voluntary range of motion in both abduction and flexion. Wilcoxon signed-rank test was used to compare the mean percent range of motion between middle deltoid and middle deltoid + LT + UT + SA as well as anterior deltoid and anterior deltoid + LT + UT + SA.
All analyses were done using SPSS version 26 and an α of 0.05 was considered statistically significant.
Results
Ten able-bodied participants (Male = 9 and Female = 1) completed the study. The participants age ranged from 21 to 31 yrs. (Mean = 25.1, SD = 3.47). Their height ranged from 165 to 182 cm (Mean = 174.9, SD = 6.22). Their weight ranged from 67.58 to 102.05 kg (Mean = 79.15, SD = 9.92). Nine out of ten participants were right-arm dominant (please refer to for individual participant demographics). For all the study participants we were successfully able to stimulate LT, UT, SA, anterior deltoid and middle deltoid using surface FES as established by muscle palpation and visual movement inspection (for FES amplitudes for each participant’s individual muscles, please refer to ). No adverse events were reported for any of the study participants.
Table 1 Participant demographics.
Table 2 FES intensity in milliamperes (mA) for individual muscles for each study participant.
The mean and standard deviation of maximum reach in flexion during FES of anterior deltoid and FES of anterior deltoid along with LT, UT and SA condition was 66.17° ± 28.85° (Range: 16°–110°) and 63.32° ± 26.45° (Range: 22°–104°), respectively (). Similarly, the mean and standard deviation in abduction during FES of middle deltoid and FES of middle deltoid along with LT, UT and SA condition was 43.76° ± 15.32° (Range: 33°–84°) and 51.78° ± 17.54° (Range: 31°–96°), respectively. For individual mean values across ten trials in all four FES conditions, please refer to . The maximum reach in abduction achieved with FES of middle deltoid along with LT, UT and SA was greater than that achieved with FES of middle deltoid alone in 9 out of 10 participants (). A Wilcoxon signed-rank test indicated that the FES of middle deltoid along with LT, UT and SA (mean rank = 6) produced a higher maximum reach in abduction than FES of middle deltoid alone (mean rank = 1; Z = −2.701, P = 0.007). There was no significant difference in maximum reach between FES of anterior deltoid and FES of anterior deltoid along with LT, UT and SA; however, six out of ten participants achieved a higher maximum reach in flexion with scapular muscle stimulation (). Displacement of the arm in flexion and abduction for a single participant (SCA18) across all experimental conditions is presented in .
Figure 2 Means of the maximum arm reach across all experimental conditions. AFF – Active forward flexion; AD – FES of anterior deltoid; ADALL – FES of anterior deltoid along with LT, UT and SA; AB – Active abduction; MD – FES of middle deltoid; ABALL – FES of middle deltoid along with LT, UT, and SA
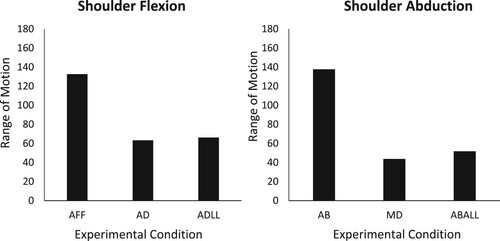
Figure 3 Displacement of the arm in flexion and abduction for one study participant (SCA18) across all experimental conditions. X-axis is the time in seconds and Y-axis is the displacement of the upper arm in degrees. AFF – Active forward flexion; AD – FES of anterior deltoid; ADALL – FES of anterior deltoid along with LT, UT, and SA; AB – Active abduction; MD – FES of middle deltoid; ABALL – FES of middle deltoid along with LT, UT, and SA
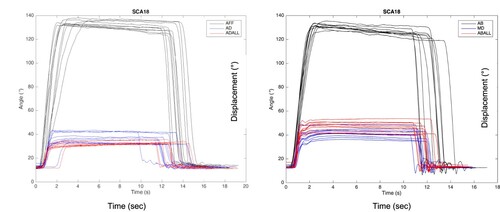
Table 3 Maximum reach in degrees across ten trials for each experimental condition for individual study participant.
The mean percent range of motion achieved during flexion for the anterior deltoid condition was 48.09%and for anterior deltoid along with LT, UT and SA was 50.31%. The mean percent range of motion achieved during abduction for middle deltoid condition was 31.70% and for middle deltoid along with LT, UT and SA condition was 37.57%. The percent range achieved with the scapular stimulation was greater for both flexion and abduction; however, this difference was statistically significant only in abduction (Z = −2.701, P = 0.007).
Discussion
Researchers have tried to stimulate certain scapular muscles noting the significance of these muscles in normal glenohumeral movement.Citation24,Citation25 The first evidence of successful stimulation of SA muscle to treat winged scapula was reported back in 1953.Citation24 To the best of our knowledge, this is the first study looking at the feasibility of stimulating all three key scapular muscles, i.e. the lower trapezius (LT), the upper trapezius (UT), and serratus anterior (SA) using transcutaneous FES during shoulder elevation movements.
It is widely noted in the literature that scapular muscles play a vital role in glenohumeral movement, specifically the LT, UT, and SA. These are critical in the production and control of scapulothoracic motion which is important for the normal function of the upper extremity.Citation19,Citation20 For the upper extremity to move through its greatest range of motion, the shoulder complex must work in a synchronized manner.Citation12 There have been several studies that have examined three-dimensional (3D) shoulder complex motion, while performing ADLs.Citation26–29 Triffitt et al., determined the relationship between active humerothoracic range of motion (ROM) and completion of 14 ADLs (e.g. combing hair, reaching overhead, and feeding) in 125 pathologic participantsCitation28, and concluded that humerothoracic ROM correlates with the ability to perform ADLs.Citation28 Magermans et al., examined ADLs in 24 healthy, female subjects and found that washing the axilla required the most glenohumeral flexion (99.6°), reaching overhead required the most glenohumeral abduction (121°) and external rotation (60.6°), and combing hair required the most scapulothoracic upward rotation (34.4°).Citation27 Despite this evidence, in neuro-rehabilitation there are limited techniques that functionally recruit the scapular muscles during the task-specific training of ADLs, especially in low functioning stroke and cervical spinal cord injury patients who have minimal voluntary movement.
The current study results showed that while there was a wide variation in the range of shoulder movements across all able-bodied participants, stimulating the scapular muscles resulted in higher arm reach in abduction. However, it did not have any significant impact on the range of arm reach in flexion. Overall, irrespective of the muscles being stimulated, the maximum reach as well as percent of voluntary movement achieved in flexion was greater than that in abduction. It is important to note that in able-bodied individuals the contribution of scapular movement to total arm elevation varies widely across individualsCitation30; and this could have potentially resulted in the wide variations in the range of motion recorded across participants and across various experimental conditions. Since the movement of the arm started with the shoulder in neutral rotation, it allowed for clearance of the greater tubercle under the acromion during forward flexion. However, it may have restricted its clearance during abduction,Citation12 resulting in decreased range. Secondly, we found that for abduction the maximum reach achieved with FES of scapular muscles along with middle deltoid was greater compared to the stimulation of middle deltoid alone. In abduction, the force of the trapezius is more critical to produce upward rotation of the scapula than the force of the SA.Citation12 Given the superficial location and size of the trapezius, and the fact that there were total four electrodes (two channels) dedicated to the trapezius muscle, this might have resulted in increased contribution of the muscle toward the movement produced. This is important for patients with high cervical spine injury for two reasons. First, the shoulder complex biomechanics is altered in these patients secondary to paralysis/weakness of the deltoid and second, shoulder abduction and scapulothoracic upward rotation are critical for the execution of ADLs.Citation21
In contrast, for the flexion trials, the maximum range did not change with additional stimulation of scapular muscles. During flexion, the anterior orientation of the scapula is importantCitation12 and can be produced only by SA.Citation12 The SA has a relatively smaller muscle bulk and can be stimulated in isolation along the narrow strip where it is nestled between the latissimus dorsi and pectoralis major. In our study, it was stimulated using one channel and lower current amplitudes to prevent the radiation of current to the neighboring larger abdominal muscles and hence might not have been recruited most optimally to observe its effect in flexion. Nonetheless, trapezius and SA, besides contributing to an increase in range, serve an equally important function as stabilizing synergists for the deltoid acting at the glenohumeral joint and should be actively engaged during shoulder complex movements.
There are certain limitations to the current study. Given the preliminary nature of the study and its primary objective of assessing feasibility, we used a convenience sample of healthy volunteers. Second, given the wide variation of scapular contributions to glenohumeral movement, the results of the study should be interpreted with caution; that is during clinical application of FES emphasis should be placed on optimal shoulder complex biomechanics rather than individually focusing on the degree of scapular rotation only. Third, it was not possible to confirm with any certainty that no voluntary effort was used during FES trials. Future studies may use EMG to ensure total muscle relaxation prior to and upon cessation of FES. Nonetheless, in this study we demonstrated that we can successfully recruit scapular muscles using surface FES. This provides an avenue for rehabilitation specialists to engage these muscles during the upper extremity rehabilitation.
Disclaimer statements
Contributors None.
Funding The Primary author of the paper is funded by CIHR Frederick Banting Fellowship.
Conflicts of interest Authors NK, MMC, MM, KLF and KM have no conflicts to declare. MRP is the co-founder and the Director of MyndTec, Inc. a company that manufactures transcutaneous functional electrical stimulators. BM works for Myant, Inc. which may have industrial applications for the methods presented in the paper. CMC is a member of the Executive Board and Treasurer of the International Functional Electrical Stimulation Society
Acknowledgements
The authors would like to acknowledge the graduate and post-graduate students in the laboratory for their help during data collection.
References
- Long C 2nd. An electrophysiologic splint for the hand. Arch Phys Med Rehabil 1963;44:499–503.
- Snoek GJ, IJzerman, in ‘t Groen FACG, Stoffers TS, Zilvold G. Use of the NESS handmaster to restore handfunction in tetraplegia: clinical experiences in ten patients. Spinal Cord 2000;38(4):244–9.
- Marquez-Chin C, Popovic MR. Functional electrical stimulation therapy for restoration of motor function after spinal cord injury and stroke: a review. Biomed Eng Online 2020;19(1):34.
- Prochazka A, Gauthier M, Wieler M, Kenwell Z. The bionic glove: an electrical stimulator garment that provides controlled grasp and hand opening in quadriplegia. Arch Phys Med Rehabil 1997;78(6):608–14.
- Fisekovic N, Popovic DB. New controller for functional electrical stimulation systems. Med Eng Phys 2001;23(6):391–9.
- Thrasher TA, Flett HM, Popovic MR. Gait training regimen for incomplete spinal cord injury using functional electrical stimulation. Spinal Cord 2006;44(6):357–61.
- Hebert DABJ, Ho C, Antunes I, O’Reilly DJ, Bayley M. Examining a new functional electrical stimulation therapy with people with severe upper extremity hemiparesis and chronic stroke: a feasibility study. Br J Occup Ther 2017;80:651–9.
- Chae J, Bethoux F, Bohine T, Dobos L, Davis T, Friedl A. Neuromuscular stimulation for upper extremity motor and functional recovery in acute hemiplegia. Stroke 1998;29(5):975–9.
- Gritsenko V, Prochazka A. A functional electric stimulation-assisted exercise therapy system for hemiplegic hand function. Arch Phys Med Rehabil 2004;85(6):881–5.
- Meadmore KL, Exell TA, Hallewell E, Hughes AM, Freeman CT, Kutlu M, et al. The application of precisely controlled functional electrical stimulation to the shoulder, elbow and wrist for upper limb stroke rehabilitation: a feasibility study. J Neuroeng Rehabil 2014;11:105.
- Peckham PH, Knutson JS. Functional electrical stimulation for neuromuscular applications. Annu Rev Biomed Eng 2005;7:327–60.
- Levangie PKNC. Joint structure and function: a comprehensive analysis. 4th ed. Philadelphia: F.A. Davis Company; 2005.
- Cuesta-Gómez A, Carratalá-Tejada M, Molina-Rueda F, Miangolarra-Page JC. Functional electrical stimulation improves reaching movement in the shoulder and elbow muscles of stroke patients: a three-dimensional motion analysis. Restor Neurol Neurosci 2019;37(3):231–8.
- Kapadia N, Zivanovic V, Popovic MR. Restoring voluntary grasping function in individuals with incomplete chronic spinal cord injury: pilot study. Top Spinal Cord Inj Rehabil 2013;19(4):279–87.
- Kapadia NM, Nagai MK, Zivanovic V, Bernstein J, Woodhouse J, Rumney P, et al. Functional electrical stimulation therapy for recovery of reaching and grasping in severe chronic pediatric stroke patients. J Child Neurol 2014;29(4):493–9.
- Kapadia NM, Zivanovic V, Furlan JC, Craven BC, McGillivray C, Popovic MR. Functional electrical stimulation therapy for grasping in traumatic incomplete spinal cord injury: randomized control trial. Artif Organs 2011;35(3):212–16.
- Popovic MR, Kapadia N, Zivanovic V, Furlan JC, Craven BC, McGillivray C. Functional electrical stimulation therapy of voluntary grasping versus only conventional rehabilitation for patients with subacute incomplete tetraplegia: a randomized clinical trial. Neurorehabil Neural Repair 2011;25(5):433–42.
- Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg 2003;11(2):142–51.
- Ludewig PM, Cook TM, Nawoczenski DA. Three-dimensional scapular orientation and muscle activity at selected positions of humeral elevation. J Orthop Sports Phys Ther 1996;24(2):57–65.
- Ebaugh DD, McClure PW, Karduna AR. Three-dimensional scapulothoracic motion during active and passive arm elevation. Clin Biomech (Bristol Avon) 2005;20(7):700–9.
- Rundquist PJ, Obrecht C, Woodruff L. Three-dimensional shoulder kinematics to complete activities of daily living. Am J Phys Med Rehabil 2009;88(8):623–9.
- Kapadia N, Moineau B, Popovic MR. Functional electrical stimulation therapy for retraining reaching and grasping after spinal cord injury and stroke. Front Neurosci 2020;14:718.
- Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion–part II: shoulder, elbow, wrist and hand. J Biomech 2005;38(5):981–92.
- Rudd JL. Electrical stimulation in serratus anterior paralysis (winged scapula). Phys Ther Rev 1953;33(2):64–7.
- Bdaiwi AH, Mackenzie TA, Herrington L, Horsley I, Cools AM. Acromiohumeral distance during neuromuscular electrical stimulation of the lower trapezius and serratus anterior muscles in healthy participants. J Athl Train 2015;50(7):713–18.
- Pearl ML, Harris SL, Lippitt SB, Sidles JA, Harryman DT 2nd., Matsen FA 3rd. A system for describing positions of the humerus relative to the thorax and its use in the presentation of several functionally important arm positions. J Shoulder Elbow Surg 1992;1(2):113–18.
- Magermans DJ, Chadwick EK, Veeger HE, van der Helm FC. Requirements for upper extremity motions during activities of daily living. Clin Biomech (Bristol Avon) 2005;20(6):591–9.
- Triffitt PD. The relationship between motion of the shoulder and the stated ability to perform activities of daily living. J Bone Jt Surg Am. Vol 1998;80(1):41–6.
- Doorenbosch CA, Harlaar J, Veeger DH. The globe system: an unambiguous description of shoulder positions in daily life movements. J Rehabil Res Dev 2003;40(2):149–55.
- McQuade KJ, Smidt GL. Dynamic scapulohumeral rhythm: the effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther 1998;27(2):125–33.
