Abstract
Objective
To compare the occurrence of falls and fall-related injuries, and the circumstances of falls among individuals with spinal cord injury (SCI) who ambulate full-time, use a wheelchair full-time and ambulate part-time.
Design
A secondary analysis.
Setting
Community.
Participants
Adults with SCI.
Intervention
None.
Outcome measures
The occurrence and circumstances of falls and fall-related injuries were tracked over six-months using a survey. Participants were grouped by mobility and fall status. A chi-square test compared the occurrence of falls and fall-related injuries, and the time and location of falls, and a negative binomial regression was used to predict the likelihood of falls by mobility status. Kaplan-Meier analysis was used to determine differences in the time to first fall based on mobility status. Group characteristics and causes of falls were described.
Results
Data from individuals who ambulated full-time (n = 30), used a wheelchair full-time (n = 27) and ambulated part-time (n = 8) were analyzed. Mobility status was a significant predictor of falls (P < 0.01); individuals who used a wheelchair full-time had a third of the likelihood of falling than those who ambulated full-time (P < 0.01). Type of fall-related injuries differed by mobility status. Those who ambulated full-time fell more in the daytime (P < 0.01). Individuals who ambulated full-time and part-time commonly fell while walking due to poor balance, and their legs giving out, respectively. Those who used a wheelchair full-time typically fell while transferring when rushed.
Conclusion
Mobility status influences the likelihood and circumstances of falls. Mobility status should be considered when planning fall prevention education/training for individuals with SCI.
Introduction
A traumatic spinal cord injury (SCI) results from direct damage to the spinal cord and can be caused by motor vehicle accidents, sports or falls.Citation1 SCI impacts an individual’s motor, sensory and autonomic function, and functional outcomes can vary considerably depending on the severity and location of the injury.Citation1,Citation2 Individuals with SCI can have varying mobility statuses.Citation3,Citation4 Depending on factors such as a person’s neurological examination at admission as well as their age, sex and time course of recovery, individuals with SCI may ambulate with or without a gait aid or require a wheelchair for partial or complete mobility.Citation1,Citation3,Citation5,Citation6 However, regardless of their mobility status, individuals with SCI experience a high number of falls each yearCitation7 and the risk of falls in this population is multifactorial.Citation8,Citation9 Evidence suggests that the occurrence of falls among individuals with SCI is higher than other populations, including older adultsCitation10–13 and individuals living with the effects of strokeCitation14 and Parkinson’s disease.Citation15,Citation16 In one year, up to 82% of participants with SCI who ambulated and 73% of participants with SCI who used a wheelchair reported a fall.Citation7,Citation17,Citation18 This is concerning because falls can cause physical injuries (e.g. cuts, broken bones, and head injuries), as well as psychosocial consequences (e.g. frustration and activity restrictions).Citation7
Despite individuals with SCI having variable mobility statuses, how fall circumstances differ by mobility statuses has not been extensively explored among the SCI population. While many previous studies have examined the occurrence and circumstances of falls among samples consisting of individuals with SCI who ambulateCitation17,Citation19,Citation20 or those who use a wheelchair,Citation8,Citation9,Citation21–24 few have compared falls between these two groups.Citation18,Citation25,Citation26 In 2016, Jørgensen and colleaguesCitation18 retrospectively compared the incidence and circumstances of falls between individuals with chronic (≥1 year) SCI who used a wheelchair for mobility and those who ambulated. The results of this study showed that individuals with SCI who ambulated had a significantly higher occurrence of recurrent falls compared to individuals with SCI who used a wheelchair.Citation18 Following this comparison, these participants were divided into two groups, individuals who were ambulatory and wheelchair users, to prospectively examine their one-year incidence of falls and injurious falls.Citation17,Citation24 Both groups had a high risk of falls and fall-related injuries and the activities during a fall tended to differ between groups.Citation17,Citation24 Individuals who used a wheelchair tended to be at risk of falling while transferring and pushing a wheelchair due to factors such as loss of balance, rushing, equipment failure and muscle spasms.Citation7,Citation8,Citation22–24 Individuals who ambulated tended to fall while changing postures or while walking and standing due to poor balance and legs giving out.Citation7,Citation17,Citation19,Citation20 Mode of mobility was also associated with recurrent falls, wherein individuals who ambulated experienced higher odds of recurrent falls compared to wheelchair users.Citation26 Previous studies have dichotomized participants into wheelchair users and ambulators to maximize statistical power, however, since mode of mobility can vary significantly among individuals with SCI, it can be difficult to dichotomize participants into these two groups.Citation25 While fall risk among individuals who both ambulate and use a wheelchair (i.e. part-time ambulators) was previously recognized as an important construct to investigate,Citation25 falls among this group remains understudied. In the current study, individuals who ambulated part-time were defined as those who ambulate but also use a wheelchair at times.
Due to advances in gait interventions and an increase in the number of individuals with incomplete SCI, ambulation has become a common post-SCI outcome.Citation27 Individuals who ambulate part-time tend to use a wheelchair for community mobility, which may potentially minimize their risk of falls in the community.Citation28 At the same time, individuals who ambulate part-time may be at an elevated risk of falls due to having abnormal motor control, significant muscle weakness/fatigue, reduced balance, and low gait speed.Citation29,Citation30 This group may additionally experience unique fall risk circumstances due to higher levels of pain intensity, pain interference and fatigue with having to exert greater effort to compensate for strength and sensory impairments compared to those that ambulate full-time or use a wheelchair full-time.Citation27 Yet, the occurrence and circumstances surrounding falls in this group remains understudied. To address this knowledge gap, we compared the six-month occurrence of falls and fall-related injuries, as well as the circumstances of falls among individuals with SCI who: (i) ambulated full-time, (ii) used a wheelchair full-time and (iii) ambulated part-time. We hypothesized that differences would exist in the causes of falls and fall-related injuries between individuals with SCI who ambulated full-time, used a wheelchair full-time and ambulated part-time, and the circumstances of falls would differ between these three groups.
Materials and methods
Design: We conducted a secondary analysis of data that were collected over 2.3 years (2017-2019) for a study that examined the causes and consequences of falls among individuals with traumatic SCI.Citation8,Citation20,Citation23,Citation31 Ethical approval for the project was obtained from the Research Ethics Boards of the University Health Network and the University of Toronto.
Data collection: The primary dataset was obtained from a sample of participants that met the following inclusion criteria: (i) traumatic SCI with a neurological level of injury between C1 and L1 (AIS grades A–D), (ii) chronic SCI (≥1 year), (iii) 18 years or older, and (iii) community dwelling, defined as living in the community for at least one month, and (iv) had no other significant co-morbidity that could affect their mobility or physical activity (e.g. stroke). Participants were purposefully recruited for the project through various approaches, including the central recruitment database at the rehabilitation hospital, which contained contact information (e-mail and/or mailing address) of past inpatients that consented to receiving information about research opportunities. Over 200 study flyers were sent to individuals identified from the central recruitment database. Participants were also recruited through the networks of other participants in the study, advertisements posted around the rehabilitation hospital and outpatient rehabilitation community clinics, and social media platforms.Citation8,Citation20,Citation23,Citation31
The primary data contained participants’ demographics and injury characteristics (e.g. time since injury, neurological level of injury), and details about their mobility status; these details had been collected in-person or over the phone during a baseline interview. In addition, the data consisted of fall surveys, which comprised of 11 open-ended and closed-ended questions inquiring about the time, location, causes, circumstances, and consequences of each fall.Citation32 The surveys were completed by participants each time they fell during a six-month tracking period. Participants were provided the following definition of a fall: “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.”Citation33 To minimize recall bias, participants were asked to complete the survey within 24-hours of experiencing a fall.Citation20,Citation23 The surveys were completed electronically (Qualtrics Survey Software, Dallas, TX, USA) or on paper. A researcher had contacted participants approximately every three to four weeks by telephone to inquire whether they had any falls, remind them about the surveys, and offer assistance with survey completion. The primary data were collected by the lead author and a research assistant at a large Canadian tertiary SCI rehabilitation hospital.Citation20,Citation23
Data analysis: A secondary analysis was suitable as we sought to re-examine data that were previously collected to answer a new research question.Citation34 While we previously reported findings for individuals who used a wheelchair and ambulated separately,Citation8,Citation20,Citation23,Citation31 we had not compared the occurrence of falls and fall-related injuries, or fall circumstances among individuals who ambulated full-time, used a wheelchair full-time and ambulated part-time. Thus, in the current study, we re-classified participants into the following three categories based on their mobility status: (i) individuals who ambulated full-time (i.e. those who ambulated 100% of the time), (ii) individuals who used a wheelchair full-time (i.e. those who used a wheelchair 100% of the time) or (iii) individuals who ambulated part-time (i.e. those who ambulated but also used a wheelchair), as well as by their fall status: faller (i.e. ≥1 fall) or non-faller (i.e. no falls).
Data were stored and managed on Microsoft Excel (Microsoft Corporation) and SPSS version 27 (IBM, Armonk, New York) software was used to perform statistical analyses. The normality of continuous data (e.g. age, time since injury, time to first fall) was determined using a Shapiro-Wilks test. Alpha was set to 0.05 and the Bonferroni method was used for post-hoc analyses where appropriate.
Participants’ demographics and injury characteristics (e.g. age, time since injury) were analyzed based on their mobility status, using means with one standard deviation or median with interquartile range (IQR) and frequency counts (e.g. for sex, neurological level of injury). Demographic and injury characteristics by mobility status were compared using a one-way ANOVA or chi-square test of independence, as appropriate. ANOVA calculations were conducted even if normality assumptions had been violated because ANOVA calculations remain applicable under these circumstances.Citation35
Occurrence of falls and fall-related injuries: A chi-square test of independence was used to determine whether the occurrence of falls and fall-related injuries, reported as dichotomous variables for each individual (i.e. presence or absence of fall/fall-related injury), differed between groups (i.e. individuals who ambulated full-time, used a wheelchair full-time, and ambulated part-time). A negative binomial regression was run to determine whether the likelihood of falls differed by mobility status, in which the number of falls experienced by each participant over the six-month period was the dependent variable and mobility status was the independent variable.
Time to first fall: Since participants may have experienced more than one fall, which is not an independent event, time to first fall (from the date of the baseline interview to the date of the first fall) was used.Citation36 Time to first fall was reported using median, interquartile range (IQR) and then compared across the three groups using a Kaplan-Meier analysis. Participants who did not experience a fall during the tracking period are represented as censored events.Citation36 Time to first fall has been used to compare fall data, including risk, among individuals with SCICitation36,Citation37 and has been used as an outcome measure to determine success of fall reduction interventions.Citation38,Citation39
Fall circumstances: A chi-square test of independence was used to examine differences in fall circumstances (i.e. time and location of falls) between groups. The activities performed during falls and perceived causes of falls, as reported on the fall survey, were descriptively compared between the three groups that differed by mobility status.
Results
Sixty-five community-dwelling adults with traumatic SCI were included; 30 ambulated full-time (aged 61.10 ± 12.80 years, 7.00 (IQR: 9.50) years post-SCI), 27 were full-time wheelchair users (aged 50.33 ± 9.87 years, 27.00 (IQR: 16.00) years post-SCI), and eight participants ambulated part-time (aged 53.88± 17.23 years, 7.00 (IQR: 31.50) years post-SCI). Significant differences in age were found across mobility status using a one-way ANOVA (P = 0.03); fallers who used a wheelchair full-time tended to be younger than fallers who ambulated full-time although this difference did not reach statistical significance in the post-hoc analysis. See for a detailed description of the demographics and injury characteristics by mobility status.
Table 1. Participant demographics and injury characteristics
Occurrence of falls and fall-related injuries: A chi-square test of independence revealed no significant relationship between mobility status (i.e. individuals who ambulated full-time, used a wheelchair full-time and ambulated part-time) and the occurrence of falls (P = 0.14) or fall-related injuries (P = 0.95). However, according to the negative binomial regression, the mobility status of an individual was a statistically significant predictor of falls (P < 0.01); individuals who used a wheelchair full-time had a third of the likelihood of falling compared to those who ambulated full-time (0.31, 95% CI: 0.16–0.63, P < 0.01). Bruises and pain were the most common fall-related injuries experienced by individuals who ambulated full-time. Individuals who used a wheelchair full-time reported cuts/scrapes and pain as the most common fall-related injuries. Only one fall-related fracture was reported in the study, by an individual who used a wheelchair full-time. Individuals who ambulated part-time reported bruises, a bumped head, and pain as the most common fall-related injuries.
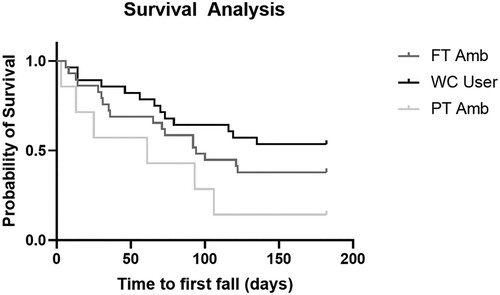
Time to first fall: During the study period, the mean time to first fall for individuals who ambulated full-time was 97.00 days (IQR: 148.00), individuals who used a wheelchair full-time was 182.00 days (IQR: 116.00) and individuals who ambulated part-time was 43.00 days (IQR: 97.00). According to the Kaplan-Meier survival analysis, there were significant differences in the time to first fall across the mobility statuses (χ2 = 7.26, P = 0.03; see for the Kaplan-Meier curve). Through post-hoc testing, only one pairwise comparison demonstrated that time to first fall for individuals who ambulated part-time and used a wheelchair full-time was approaching statistical significance (P = 0.07).
Figure 1 Kaplan-Meier curve for time to first fall. Participants who did not experience falls during the six-month period are reported as censored events.
Time of fall: According to the chi-square test of independence, the time of day of the fall differed by mobility status (P < 0.01). Post-hoc tests revealed significant differences in the time of falls; individuals who ambulated full-time fell more during the daytime compared to individuals who used a wheelchair full-time (76.92% vs 40.91%; P < 0.01).
Locations of falls: There were no group differences in the location of falls (P = 0.21). Participants from all three mobility statuses experienced most of their falls inside or just outside of their home (see for fall circumstances).
Table 2 Fall circumstances by mobility status.
Activities during falls: The activities during a fall for each mobility status are displayed in . The most common activities during a fall reported by individuals who ambulated full-time were walking (46.15%), changing positions (i.e. “getting into and out of a body position and moving from one location to another, such as rolling from one side to the other, sitting, standing, getting up out of a chair to lie down on a bed, and getting into and out of positions of kneeling or squatting”)Citation40 (26.92%) and standing (8.97%). The most common activities during a fall reported by individuals who used a wheelchair full-time were transferring (getting into/out of bed, shower/bath or vehicle) (27.27%), going over uneven ground (18.18%), playing sports/exercising (13.64%) and changing position (13.64%). The most common activities during a fall reported by individuals who ambulated part-time were walking (25.00%), transferring (getting into/out of bed, shower/bath or vehicle) (18.75%), and other (e.g. sleeping, taking a photo, driving a scooter) (18.75%).
Table 3 Activity during a fall for individuals who ambulated full-time, used a wheelchair full-time and ambulated part-time.
Activities reported by all three groups included: changing positions, transferring (i.e. getting into/out of bed, bath, or a vehicle), and sports/exercise. In contrast, assisted standing, going up or down an incline, and going over uneven ground were activities only reported by individuals who used a wheelchair full-time.
Causes of falls: The top perceived causes of falls reported by individuals who ambulated full-time were having poor balance (16.43%), legs giving out (e.g. knee buckling) (13.15%) and feeling weakness in the legs (11.74%). The top perceived causes of falls reported by individuals who used a wheelchair full-time were moving too quickly or rushing (19.15%), other (e.g. new equipment, caregiver error) (19.15%) and distraction (10.64%). The top perceived causes of falls reported by individuals who ambulated part-time were legs giving out (e.g. knee buckling) (17.95%), feeling weakness in the legs (15.38%) and other (e.g. wet floor, spasm, swollen lower extremity; 12.82%) (see ).
Table 4 Causes of falls experienced by individuals who ambulated full-time, used a wheelchair full-time and ambulated part-time.
Discussion
In this study, we compared the occurrence of falls and fall-related injuries as well as circumstances of falls between individuals with SCI who ambulated full-time, used a wheelchair full-time and ambulated part-time. In line with previous research,Citation18 our results indicated that mobility status influenced the likelihood of falls, with individuals that ambulated full-time experiencing a higher likelihood of falls. We found group differences in the time of day of falls, time to first fall, activities and causes of falls, and the type of fall-related injuries.
Following SCI, activity patterns could be impacted; the activities a person engages in and how they perform those activities could vary by mobility status.Citation41,Citation42. Not only could activities be impacted by a person’s mobility status, but also by a person’s age, sex/gender, and neurological level of injury.Citation41,Citation42 We believe this may be another reasonable explanation for why we had observed differences by mobility status in the likelihood of falling and the circumstances (e.g. activities, time, causes) surrounding participants’ falls. For instance, individuals who used a wheelchair full-time reported more falls while participating in sports/exercise compared to those that ambulated. This finding may be related to the younger age of the wheelchair users in our sample, as younger individuals with SCI tend to spend more time engaged in sports.Citation43 Moreover, our findings indicated that transfers were a high fall risk activity since all groups reported a fall during a transfer, but individuals who use a wheelchair may be at the highest risk of falls during transfers as this was the activity during which they reported the most falls. To reduce the risk of falls during transfers, routine re-assessments of a person’s transfer skills and more supportive equipment to increase their safety may be warranted.Citation44,Citation45 Furthermore, since activities,Citation41 risk willingness, fear of falling,Citation46 odds of reporting recurrent fallsCitation18 and fall risk may be impacted by a person’s sex and gender, future research should explore sex and gender-based differences in circumstances and outcomes of falls as well as fall prevention needs.
The time of falls differed among individuals who ambulated full-time and individuals who used a wheelchair full-time. Individuals who ambulated full-time tended to fall during the daytime, whereas those who used a wheelchair full-time commonly fell during the nighttime. This could potentially reflect between-group differences in the level and amount of support/assistance from a caregiver (e.g. personal support worker or family member). For instance, individuals who use a wheelchair may receive more support/assistance during the daytime compared to those who ambulate. Also, individuals who use a wheelchair may be more likely to fall in the evening or at night while going to the bathroom (i.e. getting in or out of their bed, going over floor transitions from one room to another, or changing positions) due to being tired and moving too quickly/rushing to return to bed.Citation8,Citation20,Citation47 A higher number of falls during the nighttime among individuals who use a wheelchair may also be associated with using the washroom more frequently at night compared to those who ambulate. For instance, voiding dysfunction or urinary tract infections are common in people with SCI.Citation48,Citation49 This finding suggests healthcare professionals should consider which activities an individual performs during specific periods of the day and how the activities are performed. This consideration may provide insight into how routines can be restructured to reduce their fall risk.
As expected, falls during walking were common for individuals who ambulated full-time and part-time, but those who ambulated full-time reported a higher proportion of falls while walking than those who ambulated part-time. This finding could simply reflect individuals who ambulated full-time spending more time walking during the day than those who ambulated part-time. Not only is walking needed to complete activities of daily living, but it is also considered a leisure activity that individuals with SCI who ambulate engage in.Citation43 Walking is a high fall risk activity for multiple reasons, including the presence of environmental hazards (e.g. tripping hazards) and the influence of intrinsic factors (e.g. poor balance).Citation19,Citation47,Citation50 Individuals who ambulated part-time reported more falls while walking indoors compared to those who ambulated full-time. Participants who ambulated full-time fell more while walking outdoors. This finding may reflect that individuals who ambulate part-timeCitation51 may mostly ambulate indoors, whereas those who ambulate full-time ambulate indoors and outdoors.
Although the occurrence of fall-related injuries did not differ between the groups, our study found that the type of injuries most often reported by each mobility status differed; individuals who ambulated part-time and full-time tended to sustain bruises after a fall, whereas those who used a wheelchair full-time had cuts/scrapes. This could be due to engagement in different activities during a fall as well as their surroundings. For instance, individuals who used a wheelchair tended to fall while transferring in/out of their wheelchair and onto/off of another surface. In these situations, there are sharp edges in the vicinity that could penetrate the skin and cause cuts and scrapes. Individuals who ambulated commonly fell while walking; the height from which they fall results in hard contact with the ground, resulting in a bruise. Fortunately, consistent with previous literature, most falls did not result in injuries that required medical attention in all groups.Citation7,Citation18
It is important to acknowledge that the findings of this study may be limited by the following factors. First, falls were self-reported by participants and there could be errors in self-reported data (e.g. recall bias).Citation52 As such, the occurrence of falls and fall-related injuries may be under or over-reported. Second, we failed to inquire about the location of the fall within the home,Citation23 which could have further enriched our findings related to the circumstances of falls. Third, the small sample of individuals who ambulated part-time limits statistical power and these findings should be interpreted with caution. Unfortunately, due to this small sample size, we were unable to identify significant differences in the occurrence and circumstances of falls. However, we noted that individuals who ambulated part-time reported falls while walking and transferring. Based on these preliminary findings, we believe a deeper delve into the circumstances of falls experienced by this group is warranted. This knowledge could provide greater insight into situations where they are more likely to fall and assist in highlighting key considerations for fall prevention. Lastly, a longer tracking period (i.e. ≥6 months) could have resulted in a greater number of falls/fallers.Citation7 Regardless of these limitations, this study shed light onto new knowledge that can be used to inform fall prevention interventions for individuals with SCI.
In conclusion, the experience of falls tends to differ based on mobility status. The unique circumstances encountered by individuals who have differing mobility status must be considered when assessing fall risk and planning fall prevention strategies. Furthermore, falls among individuals who ambulate part-time are understudied in prior literature, but warrant further investigation.
Disclaimer statements
Contributors None.
Funding This work was supported by the Craig H. Neilsen Foundation, grant number 440070 to KEM and a CIHR Fellowship and Toronto Rehabilitation Institute student scholarship to HS.
Conflicts of interest Authors have no conflict of interests to declare.
References
- Alizadeh A, Dyck SM, Karimi-Abdolrezaee S. Traumatic spinal cord injury: an overview of pathophysiology, models and acute injury mechanisms. Front Neurol 2019;10:282–282. doi:https://doi.org/10.3389/fneur.2019.00282.
- Hou S, Rabchevsky AG. Autonomic consequences of spinal cord injury. Compr Physiol Oct 2014;4(4):1419–1453. doi:https://doi.org/10.1002/cphy.c130045.
- Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M. Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Front Hum Neurosci 2014;8:141–141. doi:https://doi.org/10.3389/fnhum.2014.00141.
- Menon N, Gupta A, Khanna M, Taly AB. Ambulation following spinal cord injury and its correlates. Ann Indian Acad Neurol. Apr–Jun 2015;18(2):167–170. doi:https://doi.org/10.4103/0972-2327.150605.
- Burns AS, Marino RJ, Flanders AE, Flett H. Clinical diagnosis and prognosis following spinal cord injury. Handb Clin Neurol 2012;109:47–62. doi:https://doi.org/10.1016/b978-0-444-52137-8.00003-6.
- Burns SP, Golding DG, Rolle WA, Jr., Graziani V, Ditunno JF, Jr. Recovery of ambulation in motor-incomplete tetraplegia. Arch Phys Med Rehabil 1997;78(11):1169–1172.
- Khan A, Pujol C, Laylor M, Unic N, Pakosh M, Dawe J, et al. Falls after spinal cord injury: a systematic review and meta-analysis of incidence proportion and contributing factors. Spinal Cord 2019;57(7):526–539.
- Singh H, Scovil CY, Yoshida K, Oosman S, Kaiser A, Craven BC, et al. Factors that influence the risk of falling after spinal cord injury: a qualitative photo-elicitation study with individuals that use a wheelchair as their primary means of mobility. BMJ Open 2020;10:e034279–e034279.
- Sung J, Trace Y, Peterson EW, Sosnoff JJ, Rice LA. Falls among full-time wheelchair users with spinal cord injury and multiple sclerosis: a comparison of characteristics of fallers and circumstances of falls. Disabil Rehabil 2019;41(4):389–395. doi:https://doi.org/10.1080/09638288.2017.1393111.
- Gale CR, Cooper C, Aihie Sayer A. Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing. Age Ageing 2016;45(6):789–794. doi:https://doi.org/10.1093/ageing/afw129.
- Pirrie M, Saini G, Angeles R, Marzanek F, Parascandalo J, Agarwal G. Risk of falls and fear of falling in older adults residing in public housing in Ontario, Canada: findings from a multisite observational study. BMC Geriatr 2020;20(1):11, doi:https://doi.org/10.1186/s12877-019-1399-1.
- Sharif SI, Al-Harbi AB, Al-Shihabi AM, Al-Daour DS, Sharif RS. Falls in the elderly: assessment of prevalence and risk factors. Pharm Pract (Granada) 2018;16(3):1206–1206. doi:https://doi.org/10.18549/PharmPract.2018.03.1206.
- Prudham D, Evans JG. Factors associated with falls in the elderly: a community study. Age Ageing Aug 1981;10(3):141–146. doi:https://doi.org/10.1093/ageing/10.3.141.
- Simpson LA, Miller WC, Eng JJ. Effect of stroke on fall rate, location and predictors: a prospective comparison of older adults with and without stroke. PLoS One 2011;6(4):e19431, doi:https://doi.org/10.1371/journal.pone.0019431.
- Stack E, Ashburn A. Fall events described by people with Parkinson's disease: implications for clinical interviewing and the research agenda. Physiother Res Int 1999;4(3):190–200. doi:https://doi.org/10.1002/pri.165.
- Wood BH, Bilclough JA, Bowron A, Walker RW. Incidence and prediction of falls in Parkinson's disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry 2002;72(6):721–725. doi:https://doi.org/10.1136/jnnp.72.6.721.
- Jørgensen V, Butler Forslund E, Opheim A, Franzén E, Wahman K, Hultling C, et al. Falls and fear of falling predict future falls and related injuries in ambulatory individuals with spinal cord injury: a longitudinal observational study. J Physiother 2017;63(2):108–113.
- Jørgensen V, Butler Forslund E, Franzen E, Opheim A, Seiger A, Stahle A, et al. Factors associated with recurrent falls in individuals with traumatic spinal cord injury: a multicenter study. Arch Phys Med Rehabil 2016;97(11):1908–1916.
- Brotherton SS, Krause JS, Nietert PJ. Falls in individuals with incomplete spinal cord injury. Spinal Cord 2007;45(1):37–40. doi:https://doi.org/10.1038/sj.sc.3101909.
- Singh H, Shibi Rosen A, Bostick G, Kaiser A, Musselman KE. Exploring the causes and impacts of falls among ambulators with spinal cord injury using photovoice: a mixed-methods study. BMJ Open 2020;10(8):e039763, doi:https://doi.org/10.1136/bmjopen-2020-039763.
- Rice LA, Sung J, Peters J, Bartlo WD, Sosnoff JJ. Perceptions of fall circumstances, injuries and recovery techniques among power wheelchair users: a qualitative study. Clin Rehabil Jul 2018;32(7):985–993. doi:https://doi.org/10.1177/0269215518768385.
- Nelson A, Groer S, Palacios P, Mitchell D, Sabharwal S, Kirby RL, et al. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil 2010;91(8):1166–1173.
- Singh H, Scovil CY, Bostick G, Kaiser A, Craven BC, Jaglal SB, et al. Perspectives of wheelchair users with spinal cord injury on fall circumstances and fall prevention: a mixed methods approach using photovoice. PloS one 2020;15(8):e0238116–e0238116. doi:https://doi.org/10.1371/journal.pone.0238116.
- Forslund EB, Jorgensen V, Franzen E, Opheim A, Seiger A, Stahle A, et al. High incidence of falls and fall-related injuries in wheelchair users with spinal cord injury: a prospective study of risk indicators. J Rehabil Med 2017;49(2):144–151.
- Forslund EB. Falls in wheelchair users with spinal cord injury – incidence, risks and concerns. Karolinska Institutet; 2017. https://openarchive.ki.se/xmlui/bitstream/handle/10616/45417/Thesis_Emelie_Butler_Forslund.pdf?sequence=1&isAllowed=y.
- Jørgensen V. Falls in ambulatory individuals with spinal cord injury. Karolinska Institutet; 2016. https://openarchive.ki.se/xmlui/bitstream/handle/10616/45247/Thesis_Vivien%20J%c3%b8rgensen.pdf?sequence=1&isAllowed=y.
- Saunders LL, Krause JS, DiPiro ND, Kraft S, Brotherton S. Ambulation and complications related to assistive devices after spinal cord injury. J Spinal Cord Med 2013;36(6):652–659. doi:https://doi.org/10.1179/2045772312Y.0000000082.
- van Silfhout L, Hosman AJF, Bartels RHMA, Edwards MJR, Abel R, Curt A, et al. Ten meters walking speed in spinal cord–injured patients: does speed predict who walks and who rolls? Neurorehabil Neural Repair 2017;31(9):842–850. doi:https://doi.org/10.1177/1545968317723751.
- Barbeau H, Nadeau S, Garneau C. Physical determinants, emerging concepts, and training approaches in gait of individuals with spinal cord injury. J Neurotrauma 2006;23(3-4):571–585. doi:https://doi.org/10.1089/neu.2006.23.571.
- Franceschini M, Rampello A, Agosti M, Massucci M, Bovolenta F, Sale P, et al. Walking performance: correlation between energy cost of walking and walking participation. New statistical approach concerning outcome measurement. Plos One 2013;8(2):e56669, doi:https://doi.org/10.1371/journal.pone.0056669.
- Singh H, Scovil CY, Yoshida K, Oosman S, Kaiser A, Jaglal SB, et al. Capturing the psychosocial impacts of falls from the perspectives of wheelchair users with spinal cord injury through photo-elicitation. Disabil Rehabil 2020: 1–10. doi:https://doi.org/10.1080/09638288.2019.1709911.
- Unger J, Chan K, Scovil CY, Craven BC, Mansfield A, Masani K, et al. Intensive balance training for adults with incomplete spinal cord injuries: protocol for an assessor-blinded randomized clinical trial. Phys Ther 2019;99(4):420–427. doi:https://doi.org/10.1093/ptj/pzy153.
- WHO. Falls. Accessed December 3, 2020. https://www.who.int/news-room/fact-sheets/detail/falls#:~:text=A%20fall%20is%20defined%20as,floor%20or%20other%20lower%20level.
- Finlayson M, Egan M, Black C. Secondary analysis of survey data: a research method with potential for occupational therapists. Can J Occup Ther 1999;66(2):83–91. doi:https://doi.org/10.1177/000841749906600204.
- Blanca MJ, Alarcón R, Arnau J, Bono R, Bendayan R. Non-normal data: is ANOVA still a valid option? Psicothema 2017;29(4):552–557. doi:https://doi.org/10.7334/psicothema2016.383.
- Musselman KE, Arora T, Chan K, Alavinia M, Bone M, Unger J, et al. Evaluating intrinsic fall risk factors after incomplete spinal cord injury: distinguishing fallers from nonfallers. Arch Rehabil Res Clin Transl 2021;3(1):100096–100096. doi:https://doi.org/10.1016/j.arrct.2020.100096.
- Butler Forslund E, Jorgensen V, Skavberg Roaldsen K, Hultling C, Wahman K, Franzen E. Predictors of falls in persons with spinal cord injury—a prospective study using the downton fall risk index and a single question of previous falls. Spinal Cord 2019;57(2):91–99. doi:https://doi.org/10.1038/s41393-018-0175-y.
- Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing 2006;35(1):5–10. doi:https://doi.org/10.1093/ageing/afi218.
- Unger J. Assessing and training reactive stepping for individuals with incomplete spinal cord injury or disease [Doctoral]. University of Toronto; 2020. http://hdl.handle.net/1807/103380
- WHO. International classification of functioning, disability and health. https://apps.who.int/iris/bitstream/handle/10665/43737/?sequence=1.
- Hetz SP, Latimer AE, Ginis KA. Activities of daily living performed by individuals with SCI: relationships with physical fitness and leisure time physical activity. Spinal Cord 2009;47(7):550–554. doi:https://doi.org/10.1038/sc.2008.160.
- Wilson SKM, Hasler JP, Dall PM, Granat MH. Objective assessment of mobility of the spinal cord injured in a free-living environment. Spinal Cord 2008;46(5):352–357. doi:https://doi.org/10.1038/sj.sc.3102153.
- Jörgensen S, Martin Ginis KA, Lexell J. Leisure time physical activity among older adults with long-term spinal cord injury. Spinal Cord 2017;55(9):848–856. doi:https://doi.org/10.1038/sc.2017.26.
- Rice LA, Sung JH, Keane K, Peterson E, Sosnoff JJ. A brief fall prevention intervention for manual wheelchair users with spinal cord injuries: a pilot study. J Spinal Cord Med 2020;43(5):607–615. doi:https://doi.org/10.1080/10790268.2019.1643070.
- Chaves ES, Boninger ML, Cooper R, Fitzgerald SG, Gray DB, Cooper RA. Assessing the influence of wheelchair technology on perception of participation in spinal cord injury. Arch Phys Med Rehabil 2004;85(11):1854–1858. doi:https://doi.org/10.1016/j.apmr.2004.03.033.
- Jørgensen V, Roaldsen KS. Negotiating identity and self-image: perceptions of falls in ambulatory individuals with spinal cord injury - a qualitative study. Clin Rehabil 2017;31(4):544–554. doi:https://doi.org/10.1177/0269215516648751.
- Musselman KE, Arnold C, Pujol C, Lynd K, Oosman S. Falls, mobility, and physical activity after spinal cord injury: an exploratory study using photo-elicitation interviewing. Spinal Cord Ser Cases 2018;4:39–39. doi:https://doi.org/10.1038/s41394-018-0072-9.
- Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29(5):527–73.
- García Leoni ME, Esclarín De Ruz A. Management of urinary tract infection in patients with spinal cord injuries. Clin Microbiol Infect 2003;9(8):780–785. doi:https://doi.org/10.1046/j.1469-0691.2003.00643.x.
- Amatachaya S, Pramodhyakul W, Wattanapan P, Eungpinichpong W. Ability of obstacle crossing is not associated with falls in independent ambulatory patients with spinal cord injury. Original article. Spinal Cord 2015;53(598). doi:https://doi.org/10.1038/sc.2015.22.
- Lam T, Noonan VK. Eng JJ, the SRT. A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord 2008;46(4):246–254. doi:https://doi.org/10.1038/sj.sc.3102134.
- Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Healthc Res 2011;2(4):320–332. doi:https://doi.org/10.1504/IJBHR.2011.043414.
