Abstract
Objective
To describe the development of structure, process, and outcome indicators aimed to advance the quality of Reaching, Grasping & Manipulation (RG&M) rehabilitation for Canadians living with spinal cord injury or disease (SCI/D).
Method
Upper extremity rehabilitation experts developed a framework of indicators for evaluation of RG&M rehabilitation quality. A systematic search of the literature identified potential upper extremity indicators that influence RG&M outcomes. A Driver diagram summarized factors influencing upper extremity outcomes to inform the selection of structure and process indicators. Psychometric properties, clinical utility, and feasibility of potential upper extremity measures were considered when selecting outcome indicators.
Results
The selected structure indicator is the number of occupational and physical therapists with specialized certification, education, training and/or work experience in upper extremity therapy related to RG&M at a given SCI/D rehabilitation center. The process indicator is the total hours of upper extremity therapies related to RG&M and the proportion of this time allocated to neurorestorative therapy for each individual with tetraplegia receiving therapy. The outcome indicators are the Graded Redefined Assessment of Strength, Sensation and Prehension (GRASSP) strength and Spinal Cord Independence Measure III (SCIM III) Self-Care subscores implemented at rehabilitation admission and discharge, and SCIM III Self-Care subscore only at 18 months post-admission.
Conclusion
The selected indicators align with current practice, will direct the timing of routine assessments, and enhance the volume and quality of RG&M therapy delivered, with the aim to ultimately increase the proportion of individuals with tetraplegia achieving improved upper extremity function by 18 months post-rehabilitation.
Introduction
Individuals living with tetraplegia prioritize regaining and enhancing their upper extremity function during rehabilitation in order to: increase their functional abilities; reduce their lifetime burden of care; and, enhance their quality of life.Citation1 In addition, a significant and rising proportion of individuals with non-traumatic spinal cord injury (ntSCI)Citation2 present with tetraplegiaCitation1 and associated declines in upper extremity function.Citation3,Citation4 The most common etiology of ntSCI resulting in tetraplegia/paresis in Canada include: degenerative diseases, infection, tumors and vascular disease.Citation5 Considering the changing demographic of spinal cord injury (SCI) in CanadaCitation6,Citation7 (rising incidence of ntSCI) and the proportion of individuals with tetraplegia or tetra-paresis, restoration of upper extremity function is a domain of rising importance for individuals with traumatic (tSCI) and ntSCI requiring rehabilitation. The known incidence as of 2010 for tSCI and ntSCI in Canada is 41 per million and 68 per million respectively, for a total of 4,071 per annum. In 2010, the prevalence was estimated to be 85,556 persons in Canada, with 51% tSCI and 49% ntSCI. This estimate is conservative as it is derived from the number of inpatients receiving surgical intervention; therefore, the numbers of ntSCI are likely much higher.Citation7
For service providers and administrators, it is important to recognize that not only is the restoration of upper extremity function essential to individuals with SCI and disease (SCI/D), it is a significant component of the volume of the rehabilitation routinely delivered. High-quality rehabilitation care following SCI/D is critical for optimizing neurorecovery, functional restoration, and long-term health outcomes. Currently, there are no evidence-informed guidelines that specify the type and volume of upper extremity therapy to optimize outcome.
Enhancing the delivery of rehabilitation care specific to the upper extremity among individuals with tetraplegia requires therapy to optimize neurorecovery,Citation8 preventive interventions to limit upper extremity injury/overuse or deformity,Citation9 and enhanced community outcomes post-discharge.Citation10 Quality indicators are intended to be feasible for implementation within a tertiary SCI rehabilitation program serving individuals with tetraplegia regardless of injury etiology. This manuscript focuses on establishing a framework of quality indicators to assess rehabilitation specific to the upper extremity function for individuals living with tetraplegia using a methodical approach, available evidence, and expert consensus. To begin this process, we must first understand the current state of rehabilitation delivery, the extent to which the population benefits from rehabilitation therapy, and the natural history of recovery.
Current state of upper extremity, motor and sensory rehabilitation
As a field, we recognize some sensory and motor gains occur after tSCI and ntSCI. The extent of these gains are modulated by the location, completeness, and severity of lesion.Citation11 There are some detailed demonstrations of these recovery curves defining the spatial and temporal recovery of individuals according to their baseline American Spinal Injury Association Impairment Scale (AIS) categories over 12 months.Citation12–15 Beyond the first year, we are certain there is ongoing recovery up to 24 months after injury;Citation16 however, the second year is not as well described in the literature.Citation13,Citation17 Further, much of the development of intensive therapeutic protocols has been conducted among individuals with chronic tetraplegia, inferring this group has potential to make gains.Citation8,Citation18–23 Assuming that spontaneous recovery occurs during inpatient and outpatient tertiary SCI rehabilitation, it is essential to have indicators to capture how the provision of upper extremity therapies influence or optimize: spontaneous recovery, facilitate functional adaptations, and the long-term ability of individuals with tetraplegia to reach, grasp and manipulate objects in their environment.
Indicators can measure the structure, process or outcome of health care services, and their evaluation can facilitate the sustainability of a high-quality health care delivery system that is based on evidence-informed programs and services.Citation24 Structure indicators are defined by the properties of the setting in which the health care services occurCitation25 while process indicators describe the specific activities in providing and receiving care.Citation26 Finally, outcome indicators evaluate health changes that can be attributed to the health care or therapy provided, such as mortality, health-related quality of life, individual/family/provider satisfaction, and functional ability.Citation26 Indicator data can inform comparisons across different health care settings and systems to ensure continuous quality improvement and the establishment of benchmarks for superior organizations.Citation27,Citation28 This manuscript describes the context and approach to developing the Reaching, Grasping & Manipulation (RG&M) indicators for application during the first 18 months after SCI/D rehabilitation admission. This is part of the work developed by the SCI-High Project (www.sci-high.ca) aiming to select, implement, and evaluate quality care indicators for 11 domains of SCI rehabilitation in Canada by 2022. The RG&M Working Group’s objective was to establish a comprehensive framework of structure, process, and outcome indicators specific to the Domain construct of RG&M for implementation in Canada.
Methods
A detailed description of the processes for identifying RG&M as a priority Domain for SCI/D rehabilitation care and the overall SCI-High Project methods have been previously described.Citation29,Citation30 In brief, the approach to developing the structure, process, and outcome indicators for the RG&M Domain followed a modified, but substantially similar, approach to that described by Mainz et al.,Citation27 including: (a) formation and organization of the national and local Working Groups; (b) defining and refining the domain aim and specific target construct; (c) providing an overview or summary of existing evidence and practice; (d) developing and interpreting a Driver diagram; (e) selecting indicators; and (f) pilot testing and refinement of the domain-specific structure, process and outcome indicators prior to implementation. A facilitated discussion occurred amongst the Domain-specific Working Group and the SCI-High Project Team to utilize relevant expertise on the topic while ensuring the broader goals of the SCI-High Project were aligned across the other ten Domain Working Groups. Stakeholders and experts were invited to participate in RG&M Working Group based on their practical or empirical knowledge of SCI/D rehabilitation, reaching, grasping and manipulation, and individual care. The group was composed of occupational therapists (OTs), physical therapists (PTs), physiatrists, rehabilitation scientists, and postdoctoral fellows. Five videoconference meetings of the RG&M Working Group were held between March 2016 and June 2016, totaling five hours of discussion. We also met for additional five hours from Aug 2020–Jan 2021, to refine the indicators and complete manuscript preparation. In addition, individual members of the Working Group completed their own independent review of the prepared materials, and shared resources and/or practice standards with one another outside of the formally scheduled meetings.
The Working Group was asked to develop/select at least one structure, process, and outcome indicator related to the RG&M Domain. The SCI-High Project Team stipulated that the indicators must be relevant, concise (10 min or less to implement), and aligned in their aim across the structure, process, and outcome indicators to achieve a single substantive advance in SCI/D rehabilitation care. The indicators could be measured using established or new measurement tools (i.e. questionnaires, data collection sheets, laboratory exams, and medical record data), depending on the requirements and feasibility considerations specific to each indicator.
Domain-specific working group meetings
The meetings of the RG&M Working Group were organized to frame the context for clinical practice using an “eliminate and concentrate” decision-making approach to review the key constructs related to RG&M, review available outcome indicators, and develop an evidence-informed Driver diagram to establish indicators of the quality of upper extremity rehabilitation for implementation from rehabilitation admission to 18 months thereafter. Initially, the Working Group used a comprehensive mixed method that combined scientific evidence and expert consensus for developing a construct definition for RG&M. A small number of fundamental and strategically important indicators were deemed feasible via group consensus to collect at a clinical level. The development of the activities classification tool for the process indicator and the timelines for implementing the indicators was established through iterative consensus.
Literature search
Two members of the Project Team independently (MA, MO) conducted a systematic search of the literature using MEDLINE, CINAHL and EMBASE while applying a combination of the MeSH terms: “spinal cord injury”, “strength/ or hand/ or hand function”, “reaching”, “grip”, and “grasping”. The search focused on potential outcome indicators for RG&M and the factors that influence RG&M outcomes in SCI/D rehabilitation. Inappropriate references were excluded (i.e. non-English, theses, conference abstracts, qualitative research).
Driver diagram
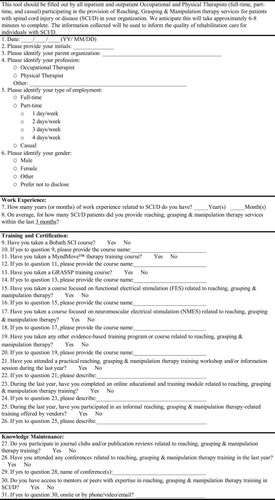
Following the literature search, the challenge of selecting quality indicators was facilitated by creating an Ishikawa (fishbone) or Driver diagram.Citation31 As part of the analysis, a graphic illustration was constructed to convey the relationships between SCI/D rehabilitation care related to upper extremity and factors that influence RG&M outcomes. Following the review of the literature, the RG&M Working Group engaged in a mind-mapping exercise to identify the factors that affect upper extremity rehabilitation. The identified factors were grouped into categories or branches (). Guided by the Driver diagram using RAND/UCLACitation32 methodology, the RG&M Working Group proposed structure, process, and outcome (intermediary and final) indicators. These well-established outcomes have had appropriate psychometric properties (i.e. reliability, validity, and responsiveness) for use in SCI/D populations.Citation33–37
Figure 1 Driver diagram for the RG&M Domain. The Impairment Branch is common to all 11 SCI-High Domains. The red items shown in the diagram represent the aim of the indicators. *Thicker black lines on the Technology branch reflect the greater volume of evidence supporting NMES and FES. UEMS: Upper-Extremity Motor Score, LEMS: Lower-Extremity Motor Score, NLI: Neurological Level of Injury, AIS: ASIA Impairment Scale, HR: Heart Rate, BP: Blood Pressure; FES: Functional Electrical Stimulation, AMES: Assisted Movement with Enhanced Sensation, Bioness Inc., NMES: Neuromuscular Electrical Stimulation, SARA System: Smart Assistive Reacher Arm (SARA) System, SRS System: Stimulus Router System, MeCFES: Myoelectrical Controlled Functional Electrical Stimulation, and PNSS/rTMS: Peripheral Nerve Somatosensory Stimulation System/repetitive Transcranial Magnetic Stimulation.
Results
Construct definition and aim
The Working Group considered the scope and breadth of the upper extremity in healthy populations as well as in individuals with sensorimotor impairments when formulating this construct:Citation38
Reaching, grasping and manipulation are the important components of upper extremity function that allow individuals with tetraplegia (C1-T1, AIS A-D) to use the sensorimotor integrity of their arm and hand to develop abilities and perform activities that meet their personal needs, and enable them to explore and participate in their external environment in meaningful ways.
The aim of the RG&M Domain is to implement standardized routine testing of arm and hand function among individuals with tetraplegia in order to: optimize upper extremity neuro-recovery and functional ability, and to understand the associations between specificity, volume, and intensity of therapy delivery and individual outcome.
Driver diagram
The outcomes of the systematic search guided the constructions of the RG&M Driver diagram (), which focused on physical, surgery, preventive, technology, prevention and therapy related to RG&M rehabilitation care delivery. The Driver diagram reflects the dichotomy within SCI/D rehabilitation, where therapy encompasses attempts at restoration of lost function and teaches compensatory strategies to minimize impairment(s) and augment functional ability. The goals of prevention treatment practices are shown in .
Table 1 Description of the therapeutic constructs underlining the RG&M practices which informed indicator development.
Following group discussions and considering the existing knowledge of what occurs in rehabilitation, and the natural history and severity of the disease, the Working Group decided to focus the indicators on therapy delivery.
Structure indicator
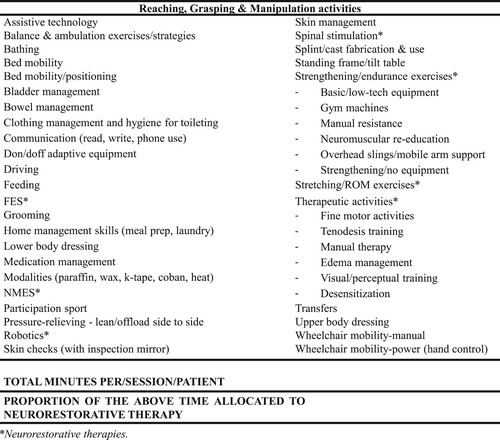
The selected structure indicator reflects the delivery of upper extremity rehabilitation in North America. As shown in the training, technology, prevention, physical, and therapy arms of the Driver diagram, upper extremity therapy consists of a diverse group of interventions. Interventions with the greatest support for their efficacyCitation39 include: task-specific training; repetitive practice of isolated and integrated functional movements of the shoulder elbow, wrist and hand with or without the application of technology (including Neuromuscular Electrical Stimulation (NMES), and Functional Electrical Stimulation (FES))Citation39 and provision of surgical interventions, including tenodesis or peripheral nerve transplant.Citation40,Citation41 For the purpose of this manuscript, NMES refers to as the application of an electrical current of sufficient intensity to elicit or facilitate muscle contraction (i.e. sensorimotor impairments targeted). FES refers to the pairing of NMES, simultaneously or intermittently, to facilitate or allow the performance of a functional task, such as arm cycling or grasping (i.e. functional disability targeted). As the current literature does not strongly favor one form of intervention over another in the subacute rehabilitation setting,Citation39 the Working Group chose description of OT and PT expertise as the key construct underpinning the structure indicator. The selected structure indicator is the number of OTs and PTs at a given site with five or more years of experience in upper extremity rehabilitation related to the SCI/D population or education, training/certification in upper extremity therapy not obtained through their entry-level professional academic degree, relative to the number of OTs and PTs providing care to individuals with SCI/D at each site per fiscal year. The structure indicator will be assessed using the tool shown in .
Process indicator
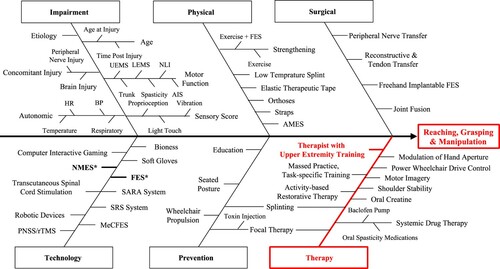
Given that gains in upper extremity function are dependent on the amount of integrated practice and may be dose- and activity-dependent, and require specific technologies, the process indicator is the total number of upper extremity hours of therapy received during their rehabilitation length of stay and the proportion of time allocated to neurorestorative therapy. OTs and PTs will enter the total number of minutes per therapy session per day spent on upper extremity therapy as part of their daily workload documentation. The sum of the total minutes of upper extremity therapy will be calculated (sum of training minutes) for each individual with tetraplegia who meets the requirements for provision of upper extremity therapy during the admission International Standards for Neurological Classification of SCI (ISNCSCI) assessment (individuals with tetraplegia C1 -T1 AIS A-D tetraplegia with voluntary motor function in at least one C5-T1 myotome regardless of cord syndrome). summarizes activities directly or indirectly related to RG&M therapy delivered by OTs and PTs during SCI/D rehabilitation. In addition, the therapist will then be asked to estimate the proportion of time each day allocated to neurorestorative therapy.
Figure 3 Alphabetical list of therapeutic activities intended to facilitate Reaching, Grasping & Manipulation outcomes. This table was modified from Ozelie et al., 2012Citation73 with feedback from Lyndhurst Centre OTs and PTs and RG&M Working Group Members.
Integral to the accurate reporting of this process indicator is a clear guideline of what therapeutic interventions constitute upper extremity interventions (). The RG&M Group agreed upon two criteria for therapists to consider when determining whether a therapeutic activity could count as part of the process of upper extremity therapy. First, the therapeutic activity involves whole-or part-practice of a functional goal or use of skills-focused training in activity-based interventions or, second, the therapeutic activity had a neurorestorative emphasis to facilitate gains in upper extremity sensorimotor function.
Outcome indicator
The systematic search of outcomes highlighted a variety of outcome measurement tools related to upper extremity function, which are summarized in . The selected outcome indicators are the Graded Redefined Assessment of Strength, Sensation and Prehension (GRASSP) strength and the Spinal Cord Independence Measure III (SCIM III) Self-Care subscores implemented at rehabilitation admission and discharge, and SCIM III Self-Care subscore only at 18 months post-admission. The criterion for the selection of outcome indicators were: feasibility for implementation; robustly studied with sound psychometric properties in SCI/D. The choice of outcomes was predicated upon the established Rick Hansen SCI Registry (RHSCIR) practice of measuring ISNCSCI motor scores and SCIM scores at rehabilitation admission and the correlation of the recovery rate with the duration of follow-up (p=0.001) observed in a recent systematic review and meta-analysis.Citation42 Studies with follow-up duration of approximately six months or less reported significantly lower recovery rates for incomplete SCI compared to studies with long-term follow-up. The RG&M working group anticipated that hours of activity-based therapies would result in measurable improvement in SCIM III Self-Care subscores and that neurorestorative therapies would be reflected in GRASSP strength subscores.
Table 2 Systematic search of outcomes related to reaching, grasping and manipulation.
summarizes the structure, process and outcome indicators or the RG&M Domain.
Table 3 Minimal data set of reaching, grasping and manipulation indicators.
Discussion
This SCI-High Project manuscript is part of a concerted effort to identify priority indicators of quality care for SCI/D rehabilitation that can be readily incorporated into usual clinical care. The manuscript describes and defines a framework of structure, process, and outcome indicators for implementation during upper extremity rehabilitation among individuals with tetraplegia during inpatient rehabilitation and post-discharge in the community. Indicator development incorporated the engagement of an expert Working Group, systematic search and synthesis, Driver diagram development, and the selection of indicators was based on evidence and expert consensus. Indicator selection was guided by the widely documented limitations of resources in terms of infrastructure, time and personnel.Citation43,Citation44 The selected indicators will provide crucial information regarding rehabilitation intensity and specifications, and associated RG&M outcomes. The data will inform the future creation of benchmarksCitation45 for optimal and equitable upper extremity rehabilitation post-SCI. Further, this indicator data, once prospectively collected, will help the field to better understand how the existing rehabilitation services across Canada can optimize upper extremity function in individuals with tetraplegia by elucidating the recovery profiles and the role of rehabilitation in maximizing upper extremity functional restoration.
Structure indicator
The structure indicator will be the number of OTs and PTs with specialized certification, education, training and/or work experience in upper extremity intervention and therapy related to RG&M relative to the number of OTs and PTs providing upper extremity therapy to individuals with SCI/D per site per fiscal year.Citation46,Citation47 The field of upper extremity rehabilitation for individuals with tetraplegia has gained significant momentum in the past 2–3 decades, specifically from a technology perspectiveCitation48 with increased research in robotics and FES. With newer rehabilitation techniques being evaluated, institutional best practices are evolving and vary across different rehabilitation settings in Canada.Citation49 Therapist skill and willingness to embrace evidence-based practice are amongst the many provider factors attributed to individual outcomes following rehabilitation.Citation50,Citation51 However, the limitations to adoption of evidence-based practice are well documented and include lack of understanding and consensus of the meaning of evidence-based practice,Citation52 lack of time, support and/or resources to research literature, lack of knowledge and skills to assess research findings,Citation53 and difficulty in managing the process of translating evidence to practice.Citation54 For these reasons, and to ensure clinical feasibility of the indicators, we must capture the structure indicator within the context of institutional best practices and their influence on process and outcome indicators with minimal manipulation of therapy delivery. The goal of the current quality improvement project is to understand and highlight the positive or negative association between therapy delivery and RG&M individual outcomes hoping that it will set a tone for healthcare policy discussions and assist with continuing education efforts.
Process indicator
The process indicator will be the total number of hours of therapy directed towards retraining upper extremity function. Whereas these hours are more easily identified in OT and PT practices, we will miss those hours spent with the Physical and Occupational Therapy Assistants, and hence global understanding of therapy delivery will not be complete. The process indicators have value in understanding the relationship between intensity of therapy, the proportion of therapy time allocated to neurorestorative therapy, and individual functional outcomes. There is mixed evidence related to the benefit of increased therapy intensity on functional outcomes.Citation55–57 Although the selected indicators do not capture specific upper extremity rehabilitation techniques used, the literature supports that rehabilitation goals vary based on level and severity of SCI/D,Citation58,Citation59 and techniques will vary based on therapist evaluations and therapist training, individual clinician biases towards specific interventions,Citation60 and the individual’s ability to participate in therapy without service interruptions due to concomitant health conditions (e.g. orthostatic hypotension, urinary tract infections, pressure injury, etc). Thus, this gives us an opportunity to study the outcome indicators in “real world” settings. The Working Group anticipated that an understanding of the activities and the volume of therapy will provide insights into individual outcomes.
Outcome indicator
The baseline, intermediary, and final outcome indicators (SCIM Self-Care subscores and GRASSP strength) are commonly used in the SCI/D population and time-effective.Citation3,Citation15,Citation35,Citation61–63 The SCIM, a well-accepted measure given its psychometric properties is commonly used to describe for individual self-report of disease among individuals with SCI/D; and the fact that an interview format is being used improves the likelihood of collecting data at the 18 months follow-up time point, which is often considered challenging in quality improvement and research trials. The GRASSP consists of five subtests that characterize sensorimotor hand function. Of the subtests, GRASSP strength is the most reliable, precise and responsive. GRASSP strength also plays a significant role in predicting hand function as it relates to prehension.Citation34,Citation64 The GRASSP strength subscore is reported to be the strongest predictor for upper extremity function and self-care outcomes.Citation15,Citation65,Citation66 Hence, we expect that the implementation of outcome indicators at baseline and both intermediary and final time points will be feasible.Citation67
Application and use
Successful implementation of the structure, process, and outcome indicators will have a multi-level impact on the delivery of RG&M care and individuals living with tetraplegia. At the policy level, it will allow us to study the impact of resources: staffing, length of stay, capital resources for rehabilitation equipment, and resources for improving evidence-based practices, to name a few. At the site-specific level, it will provide insight into quality of care and how it stands against national benchmarks. At the practice level, it will help answer the very important question of therapy intensity and its relationship with long-term functional outcomes. If, in fact, we find a strong correlation across the three indicators, then the specific therapeutic maneuvers used might become less relevant, or alternatively, we might find that therapist expertise is more critical to better recovery profiles, or that more intense therapy irrespective of therapist level of expertise produces better outcomes. These hypotheses are speculative in nature, and in-depth analysis of the planned indicator data may provide new insights into which parameters modify quality of care. In any case, at the client level, it will help to improve best practices. Currently, the only data available is changes in the Functional Independence Measure (FIM), the length of stay, and the FIM efficiency which is the change in FIM divided by the length of stay. We need more SCI/D-specific measures that allow us to study recovery profiles over a longer-term. At this juncture, we have limited data regarding outpatient therapy provision, and functional gains or deterioration following rehabilitation discharge.Citation68 We also have to take into consideration that there may be an overlap between the indicator data collected for other Domains of rehabilitation care such as WalkingCitation69 and Wheeled Mobility,Citation70 within the SCI-High Project. The risk with the proposed indicators is that there is a potential for double counting of interventions that can be substantially reduced with a detailed implementation plan and significant staff training for appropriate workload reporting.
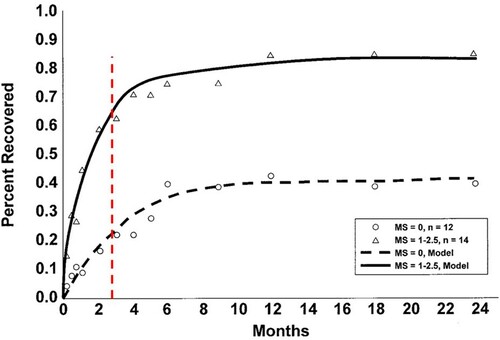
Based on what is known about the natural history of motor recovery, a majority of inpatients are discharged at a time point when the slope of their recovery is greatest (), suggesting that we may be missing an important therapeutic window.Citation71
Figure 4 Illustration of the intersection between rehabilitation discharge (red vertical line) and the slope of change in upper extremity motor scores (MS). The red dotted line represents the median rehabilitation length of stay in Canada.Citation74 The recovery timeline graph was adapted from Burns and Ditunno, 2001,Citation71 displaying functional motor recovery in individuals with C6 tetraplegia with an initial MS at the C5 myotome. Solid and dotted black lines depict modeled data resulting from individuals with different motor scores.
The RG&M Domain indicators have great potential to advance the field and provide new insights that are not currently available in public datasets, and may contribute to identifying responders and non-responders to specific types of interventions, thereby enhancing individuals’ outcomes. The routine collection of the selected indicators will enable the field to understand “restoration recovery”, the upper extremity injury prevention and education needs of patients with tSCI or ntSCI, as well to describe sub-populations, their needs, recovery and responsiveness to intervention using this inclusive approach. The selected RG&M indicators will be integrated into the larger SCI-High Project framework to create a group of indicators and related best practices for routine implementation within a single rehabilitation program with project-wide report cards enabling cross-site comparisons of structure, process, and outcomes.
Conclusion
The plan is to implement this framework of RG&M indicators routinely in Ontario (across five tertiary rehabilitation sites- London, Hamilton, Toronto, Kingston, Ottawa), while looking at opportunities to expand its implementation to other provinces across Canada. The structure and process indicators will characterize the volume and type of therapy delivered to individuals with tetraplegia. The outcome indicators are intended to define the benefits of rehabilitation and were selected based on their perceived feasibility and robust psychometric properties established in individuals with SCI.Citation35,Citation72
Disclaimer statements
Contributors None.
Funding This work is embedded in the larger SCI-High Project funded by the Praxis Spinal Cord Institute (former Rick Hansen Institute - Grant #G2015-33), Ontario Neurotrauma Foundation (ONF – Grant #2018-RHI-HIGH-1057), and the Toronto Rehab Foundation.
Conflicts of interest Dr. Kalsi-Ryan is the CEO of Neural Outcomes Consulting Inc., company that manufactures and distributes GRASSP. Naaz Kapadia is a PhD candidate funded by the Canadian Institute of Health Research (CIHR) Frederick Banting and Charles Best Canada Graduate Scholarship (CIHR-201810GSD-422024-294480); she also participated in the development of the commercial version of Myndmove, but she has no financial or personal conflicts. Dr. Wiest is funded by the Ontario Neurotrauma Foundation and the CIHR Health Systems Impact Fellowship (HI5-166374). Dr. Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation, and receipt of consulting fees from the Rick Hansen Institute. Dr. S. Mohammad Alavinia, Farnoosh Farahani, Heather Flett, Dr. Dany H. Gagnon, Jennifer Holmes, Maryam Omidvar, and Prof. Molly Verrier report no conflicts of interest.
Declaration of interest None.
Acknowledgements
The authors would like to acknowledge the time, energy and expertise of Drs. Mark T. Bayley, Gaya Jeyathevan and Sander L. Hitzig, and the Occupational Therapy team of Toronto Rehab Lyndhurst Centre throughout the development of the indicators.
References
- Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004;21(10):1371–83.
- New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord 2014;52(2):97–109.
- Kalsi-Ryan S, Riehm LE, Tetreault L, Martin AR, Teoderascu F, Massicotte E, et al. Characteristics of upper limb impairment related to degenerative cervical myelopathy: development of a sensitive hand assessment (Graded redefined assessment of strength, sensibility, and prehension version myelopathy). Neurosurgery 2020;86(3):E292–E9.
- Tetreault L, Kopjar B, Nouri A, Arnold P, Barbagallo G, Bartels R, et al. The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J 2017;26(1):78–84.
- Ho C, Guilcher SJT, McKenzie N, Mouneimne M, Williams A, Voth J, et al. Validation of algorithm to identify persons with non-traumatic spinal cord dysfunction in Canada using Administrative Health Data. Top Spinal Cord Inj Rehabil 2017;23(4):333–42.
- Guilcher SJ, Munce SE, Couris CM, Fung K, Craven BC, Verrier M, et al. Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord 2010;48(1):45–50.
- Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG, et al. Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology 2012;38(4):219–26.
- Lu X, Battistuzzo CR, Zoghi M, Galea MP. Effects of training on upper limb function after cervical spinal cord injury: a systematic review. Clin Rehabil 2015;29(1):3–13.
- Boninger ML, Koontz AM, Sisto SA, Dyson-Hudson TA, Chang M, Price R, et al. Pushrim biomechanics and injury prevention in spinal cord injury: recommendations based on CULP-SCI investigations. J Rehabil Res Dev 2005;42(3 Suppl 1):9–19.
- Simpson LA, Eng JJ, Hsieh JT, Wolfe DL. Spinal Cord injury Rehabilitation Evidence Scire Research T. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma 2012;29(8):1548–55.
- Miyanji F, Furlan JC, Aarabi B, Arnold PM, Fehlings MG. Acute cervical traumatic spinal cord injury: MR imaging findings correlated with neurologic outcome--prospective study with 100 consecutive patients. Radiology 2007;243(3):820–7.
- Martin AR, et al. Clinical outcomes of nonoperatively managed degenerative cervical myelopathy: an ambispective longitudinal cohort study in 117 patients” has been accepted for publication in the Journal of Neurosurgery: Spine. In Press.
- Kalsi-Ryan S, Beaton D, Curt A, Popovic MR, Verrier MC, Fehlings MG. Outcome of the upper limb in cervical spinal cord injury: profiles of recovery and insights for clinical studies. J Spinal Cord Med 2014;37(5):503–10.
- Tanadini LG, Steeves JD, Hothorn T, Abel R, Maier D, Schubert M, et al. identifying homogeneous subgroups in neurological disorders: unbiased recursive partitioning in cervical complete spinal cord injury. Neurorehabil Neural Repair 2014;28(6):507–15.
- Velstra IM, Bolliger M, Tanadini LG, Baumberger M, Abel R, Rietman JS, et al. Prediction and stratification of upper limb function and self-care in acute cervical spinal cord injury with the graded redefined assessment of strength, sensibility, and prehension (GRASSP). Neurorehabil Neural Repair 2014;28(7):632–42.
- Ditunno JF, J, Stover SL, Freed MM, Ahn JH. Motor recovery of the upper extremities in traumatic quadriplegia: a multicenter study. Arch Phys Med Rehabil 1992;73(5):431–6.
- Petersen JA, Spiess M, Curt A, Weidner N, Rupp R, Abel R, et al. Upper limb recovery in spinal cord injury: involvement of central and peripheral motor pathways. Neurorehabil Neural Repair 2017;31(5):432–41.
- Beekhuizen KS, Field-Fote EC. Sensory stimulation augments the effects of massed practice training in persons with tetraplegia. Arch Phys Med Rehabil 2008;89(4):602–8.
- Dolbow DR, Gorgey AS, Recio AC, Stiens SA, Curry AC, Sadowsky CL, et al. Activity-based restorative therapies after spinal cord injury: inter-institutional conceptions and perceptions. Aging Dis 2015;6(4):254–61.
- Hoffman L, Field-Fote E. Effects of practice combined with somatosensory or motor stimulation on hand function in persons with spinal cord injury. Top Spinal Cord Inj Rehabil 2013;19(4):288–99.
- Kapadia N, Masani K, Catharine Craven B, Giangregorio LM, Hitzig SL, Richards K, et al. A randomized trial of functional electrical stimulation for walking in incomplete spinal cord injury: Effects on walking competency. J Spinal Cord Med 2014;37(5):511–24.
- Kapadia NM, Zivanovic V, Furlan JC, Craven BC, McGillivray C, Popovic MR. Functional electrical stimulation therapy for grasping in traumatic incomplete spinal cord injury: randomized control trial. Artif Organs 2011;35(3):212–6.
- Popovic MR, Kapadia N, Zivanovic V, Furlan JC, Craven BC, McGillivray C. Functional electrical stimulation therapy of voluntary grasping versus only conventional rehabilitation for patients with subacute incomplete tetraplegia: a randomized clinical trial. Neurorehabil Neural Repair 2011;25(5):433–42.
- Burns AS, Yee J, Flett HM, Guy K, Cournoyea N. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord 2013;51(2):165–9.
- Idvall E, Rooke L, Hamrin E. Quality indicators in clinical nursing: a review of the literature. J Adv Nurs 1997;25(1):6–17.
- Selim AJ, Berlowitz DR, Fincke G, Rosen AK, Ren XS, Christiansen CL, et al. Risk-adjusted mortality rates as a potential outcome indicator for outpatient quality assessments. Med Care 2002;40(3):237–45.
- Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care 2003;15(Suppl 1):i5–11.
- Rubin HR, Pronovost P, Diette GB. The advantages and disadvantages of process-based measures of health care quality. Int J Qual Health Care 2001;13(6):469–74.
- Alavinia SM, Hitzig SL, Farahani F, Flett H, Bayley M, Craven BC. Prioritization of rehabilitation Domains for establishing spinal cord injury high performance indicators using a modification of the hanlon method: SCI-High project. The J Spinal Cord Med 2019;42(sup1):43–50.
- Craven BC, Alavinia SM, Wiest MJ, Farahani F, Hitzig SL, Flett H, et al. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-High project. J Spinal Cord Med 2019;42(sup1):51–67.
- Phillips J SL. Change management tools part 1: using analysis to investigate problems. Nursing Times 2013;109:18–20.
- Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, et al. The RAND/UCLA Appropriateness Method User's Manual. Santa Monica (CA): RAND Corporation; 2001; Available from https://www.rand.org/pubs/monograph_reports/MR1269.html.
- Catz A, Greenberg E, Itzkovich M, Bluvshtein V, Ronen J, Gelernter I. A new instrument for outcome assessment in rehabilitation medicine: Spinal cord injury ability realization measurement index. Arch Phys Med Rehabil 2004;85(3):399–404.
- Kalsi-Ryan S, Beaton D, Ahn H, Askes H, Drew B, Curt A, et al. Responsiveness, sensitivity, and minimally detectable difference of the graded and redefined assessment of strength, sensibility, and prehension, version 1.0. J Neurotrauma 2016;33(3):307–14.
- Kalsi-Ryan S, Beaton D, Curt A, Duff S, Popovic MR, Rudhe C, et al. The graded redefined assessment of strength sensibility and prehension: reliability and validity. J Neurotrauma 2012;29(5):905–14.
- Kalsi-Ryan S, Curt A, Verrier MC, Fehlings MG. Development of the Graded Redefined Assessment of Strength, Sensibility and Prehension (GRASSP): reviewing measurement specific to the upper limb in tetraplegia. J Neurosurg Spine 2012;17(1 Suppl):65–76.
- Kalsi-Ryan S, Riehm LE, Tetreault L, Martin AR, Teoderascu F, Massicotte E, et al. Characteristics of upper limb impairment related to degenerative cervical myelopathy: development of a sensitive hand assessment (graded redefined assessment of strength, sensibility, and prehension version myelopathy). Neurosurgery 2019;86(3):E292–E9.
- Sollerman C, Ejeskar A. Sollerman hand function test. A standardised method and its use in tetraplegic patients. Scand J Plast Reconstr Surg Hand Surg 1995;29(2):167–76.
- Upper Limb Rehabilitation Following Spinal Cord Injury [Internet]. Available from https://scireproject.com/wp-content/uploads/SCIRE_Upper-limb_V7.pdf.
- Fox IK, Miller AK, Curtin CM. Nerve and tendon transfer surgery in cervical spinal cord injury: individualized choices to optimize function. Top Spinal Cord Inj Rehabil 2018;24(3):275–87.
- Hill EJR, Fox IK. Current best peripheral nerve transfers for spinal cord injury. Plast Reconstr Surg 2019;143(1):184e–98e.
- Khorasanizadeh M, Yousefifard M, Eskian M, Lu Y, Chalangari M, Harrop JS, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine 2019;15:1–17.
- Swinkels RA, van Peppen RP, Wittink H, Custers JW, Beurskens AJ. Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. BMC Musculoskelet Disord 2011;12:106.
- Van Peppen RP, Maissan FJ, Van Genderen FR, Van Dolder R, Van Meeteren NL. Outcome measures in physiotherapy management of patients with stroke: a survey into self-reported use, and barriers to and facilitators for use. Physiother Res Int 2008;13(4):255–70.
- Weissman NW, Allison JJ, Kiefe CI, Farmer RM, Weaver MT, Williams OD, et al. Achievable benchmarks of care: the ABCs of benchmarking. J Eval Clin Pract 1999;5(3):269–81.
- Al Zoubi F, Mayo N, Rochette A, Thomas A. Applying modern measurement approaches to constructs relevant to evidence-based practice among Canadian physical and occupational therapists. Implement Sci 2018;13(1):152.
- Buchanan H, Siegfried N, Jelsma J. Survey instruments for knowledge, skills, attitudes and behaviour related to evidence-based practice in occupational therapy: a systematic review. Occup Ther Int 2016;23(2):59–90.
- Singh H, Unger J, Zariffa J, Pakosh M, Jaglal S, Craven BC, et al. Robot-assisted upper extremity rehabilitation for cervical spinal cord injuries: a systematic scoping review. Disabil Rehabil Assist Technol 2018;13(7):704–15.
- Craven BC, Verrier M, Balioussis C, Wolfe D, Hsieh J, Noonan V, et al. Rehabilitation environmental scan atlas: capturing capacity in Canadian SCI rehabilitation. Rick Hansen Institute; 2012. Available from http://rickhanseninstitute.org/images/stories/ESCAN/RHESCANATLAS2012WEB_2014.pdf
- Shepherd RB. Some factors influencing the outcome of stroke rehabilitation. Aust J Physiother 1979;25(4):173–8.
- von Zweck C. The promotion of evidence-based occupational therapy practice in Canada. Can J Occup Ther 1999;66(5):208–13.
- Egan M, Dubouloz CJ, Von Zweck C, Vallerand J. The client-centred evidence-based practice of occupational therapy. Can J Occup Ther 1998;65(3):136–43.
- Law M, Baum C. Evidence-based occupational therapy. Can J Occup Ther 1998;65(3):131–5.
- Dubouloz CJ, Egan M, Vallerand J, Von Zweck C. Occupational therapists’ perceptions of evidence-based practice. The Am J Occup Ther: Official Publ Am Occup Ther Assoc 1999;53(5):445–53.
- Kapadia NM, Bagher S, Popovic MR. Influence of different rehabilitation therapy models on patient outcomes: hand function therapy in individuals with incomplete SCI. J Spinal Cord Med 2014;37(6):734–43.
- Leech KA, Hornby TG. High-intensity locomotor exercise increases brain-derived neurotrophic factor in individuals with incomplete spinal cord injury. J Neurotrauma 2017;34(6):1240–8.
- Sehatzadeh S. Effect of increased intensity of physiotherapy on patient outcomes after stroke: an evidence-based analysis. Ont Health Technol Assess Ser 2015;15(6):1–42.
- Kalsi-Ryan S, Verrier MC. A synthesis of best evidence for the restoration of upper-extremity function in people with tetraplegia. Physiother Can 2011;63(4):474–89.
- Wallace MA, Kendall MB. Transitional rehabilitation goals for people with spinal cord injury: looking beyond the hospital walls. Disabil Rehabil 2014;36(8):642–50.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics 2017;18(1):19.
- Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM–spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord 1997;35(12):850–6.
- Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Luthi H, et al. Development and validation of a self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord 2013;51(1):40–7.
- Itzkovich M, Tripolski M, Zeilig G, Ring H, Rosentul N, Ronen J, et al. Rasch analysis of the Catz-Itzkovich spinal cord independence measure. Spinal Cord 2002;40(8):396–407.
- Velstra IM, Curt A, Frotzler A, Abel R, Kalsi-Ryan S, Rietman JS, et al. Changes in strength, sensation, and prehension in acute cervical spinal cord injury: European multicenter responsiveness study of the GRASSP. Neurorehabil Neural Repair 2015;29(8):755–66.
- Kalsi-Ryan S, Beaton D, Curt A, Duff S, Jiang D, Popovic MR, et al. Defining the role of sensation, strength, and prehension for upper limb function in cervical spinal cord injury. Neurorehabil Neural Repair 2014;28(1):66–74.
- Zariffa J, Curt A, Verrier MC, Fehlings MG, Kalsi-Ryan S, Team GC-SS, et al. Predicting task performance from upper extremity impairment measures after cervical spinal cord injury. Spinal Cord 2016;54(12):1145–51.
- Kalsi-Ryan S, Curt A, Fehlings M, Verrier M. Assessment of the hand in tetraplegia using the Graded Redefined Assessment of Strength, Sensibility and Prehension (GRASSP) impairment versus function. Top Spinal Cord Inj Rehabil 2009;14(4):34–46.
- Rowan CP, Chan BCF, Jaglal SB, Catharine Craven B. Describing the current state of post-rehabilitation health system surveillance in Ontario - an invited review. J Spinal Cord Med 2019;42(sup1):21–33.
- Musselman KE, Verrier MC, Flett H, Nadeau S, Yang JF, Farahani F, et al. Development of walking indicators to advance the quality of spinal cord injury rehabilitation: SCI-High project. J Spinal Cord Med 2019;42(sup1):119–29.
- Bayley MT, Kirby RL, Farahani F, Titus L, Smith C, Routhier F, et al. Development of wheeled mobility indicators to advance the quality of spinal cord injury rehabilitation: SCI-high project. J Spinal Cord Med 2019;42(sup1):130–40.
- Burns AS, Ditunno JF. Establishing prognosis and maximizing functional outcomes after spinal cord injury: a review of current and future directions in rehabilitation management. Spine (Phila Pa 1976) 2001;26(24 Suppl):S137–45.
- Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil 2007;29(24):1926–33.
- Ozelie R, Gassaway J, Buchman E, Thimmaiah D, Heisler L, Cantoni K, et al. Relationship of occupational therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med 2012;35(6):527–46.
- Catharine Craven B, Kurban D, Farahani F, Rivers CS, Ho C, Linassi AG, et al. Predicting rehabilitation length of stay in Canada: it's not just about impairment. J Spinal Cord Med 2017;40(6):676–86.
- Huang H, Chen L. Neurorestorative process, law, and mechanisms. J Neurorestoratology 2015;3:23–30.
- Hall KM, Cohen ME, Wright J, Call M, Werner P. Characteristics of the functional independence measure in traumatic spinal cord injury. Arch Phys Med Rehabil 1999;80(11):1471–6.
- Stineman MG, Shea JA, Jette A, Tassoni CJ, Ottenbacher KJ, Fiedler R, et al. The functional independence measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil 1996;77(11):1101–8.
- Mulcahey MJ, Smith BT, Betz RR. Psychometric rigor of the Grasp and Release Test for measuring functional limitation of persons with tetraplegia: a preliminary analysis. J Spinal Cord Med 2004;27(1):41–6.
- Wuolle KS, Van Doren CL, Thrope GB, Keith MW, Peckham PH. Development of a quantitative hand grasp and release test for patients with tetraplegia using a hand neuroprosthesis. J Hand Surg Am 1994;19(2):209–18.
- Gresham GE, Labi ML, Dittmar SS, Hicks JT, Joyce SZ, Stehlik MA. The Quadriplegia Index of Function (QIF): sensitivity and reliability demonstrated in a study of thirty quadriplegic patients. Paraplegia 1986;24(1):38–44.
- Almeida C, Coelho JN, Riberto M. Applicability, validation and reproducibility of the spinal cord independence measure version III (SCIM III) in patients with non-traumatic spinal cord lesions. Disabil Rehabil 2016;38(22):2229–34.
- Kapadia N, Zivanovic V, Verrier M, Popovic MR. Toronto rehabilitation institute-hand function test: assessment of gross motor function in individuals with spinal cord injury. Top Spinal Cord Inj Rehabil 2012;18(2):167–86.
- Post MW, Van Lieshout G, Seelen HA, Snoek GJ, Ijzerman MJ, Pons C. Measurement properties of the short version of the Van Lieshout test for arm/hand function of persons with tetraplegia after spinal cord injury. Spinal Cord 2006;44(12):763–71.
- Spooren AI, Janssen-Potten YJ, Post MW, Kerckhofs E, Nene A, Seelen HA. Measuring change in arm hand skilled performance in persons with a cervical spinal cord injury: responsiveness of the Van Lieshout Test. Spinal Cord 2006;44(12):772–9.