Abstract
Introduction: Treosulfan is an alkylating agent that is used for the treatment of ovarian cancer and for conditioning prior to stem cell transplantation. It is a prodrug that is activated non-enzymatically to two active epoxides.
Objectives: To optimize a protocol for both in vivo samples handling and in vitro drug preparation. Treosulfan stability was tested in biological fluids at different conditions as well as for its cytotoxicity on cell lines.
Results: Plasma samples can be safely frozen for a short period up to 8 h, however; for longer periods, samples should be acidified. Urine samples and cell culture media can be safely frozen regardless their pH. For in vitro investigations, incubation of treosulfan at 37 °C for 24 h activated 100% of the drug. Whole blood acidification should be avoided for the risk of hemolysis. Finally; treosulfan cytotoxicity on HL-60 cells has increased following pre-incubation for 24 h at 37 °C compared to K562 cell line.
Conclusion: The stability profiling of treosulfan provided a valuable reference for handling of biological samples for both in vivo and in vitro studies. These results can be utilized for further investigations concerning the drug kinetics and dynamics in addition to the development of new pharmaceutical formulations.
Introduction
Treosulfan is an alkylating agent that is used for the treatment of ovarian cancer (Chekerov et al. Citation2015) and in the conditioning regimen prior to hematopoietic stem cell transplantation (HSCT) due to its strong myeloablative potential (Sjoo et al. Citation2006; Ten Brink et al. Citation2014a; Remberger et al. Citation2017). It is considered a promising therapeutic drug because of its beneficial toxicity profile (Ten Brink et al. Citation2014b).
Treosulfan treatment dose of 5–8 g/m2 per day for ovarian cancer is well tolerated by patients, with reversible myelosuppression (Gropp et al. Citation1998). At higher doses of 10–14 g/m2 daily for three consecutive days, treosulfan exhibits strong myeloablative and immunosuppressive effect and hence, is used in conditioning prior to HSCT (Greystoke et al. Citation2008; Slatter et al. Citation2011; Wachowiak et al. Citation2011).
Treosulfan is a prodrug that is activated non-enzymatically at pH 7.4 and 37 °C into two active metabolites possessing an epoxide ring: (2S,3S)-1,2-epoxy-3,4-butanediol-4-methanesulfonate (S,S-EBDM) and (2S,3S)-1,2:3,4-diepoxybutane (S,S-DEB) (Romański et al. Citation2015). Treosulfan activation is pH and temperature dependent and stops at pH <5.0 (Feit et al. Citation1970; Hartley et al. Citation1999). The value of the rate constant for treosulfan activation in 0.073 M phosphate buffer at pH 7.4 and 37 °C was determined by a linear semilogarithmic regression (k1) to be 0.45/h (Glowka et al. Citation2013). However, treosulfan activation does not depend on the phosphate buffer concentration, the ionic strength or the presence of NaCl in the solution (Romański et al. Citation2015).
Treosulfan is a water soluble drug that is easily administered intravenously to the patients either as a single agent or in combination with other cytostatic agents (Duncan and Clayton Citation1985; Hilger et al. Citation1998; Koyyalamudi et al. Citation2016). It is also available as capsules for oral administration that can provide a satisfactory non-invasive treatment alternative (Hilger et al. Citation2000).
Treosulfan is a well-tolerated drug (Mahner et al. Citation2012; Sehouli et al. Citation2017), however; the drug peak plasma concentration (Cmax) was reported to be significantly higher after intravenous administration compared to drug capsules (Hilger et al. Citation2000). Moreover, higher grades of leukopenia and toxicities may occur after oral capsules of treosulfan (Sehouli et al. Citation2017). Treosulfan is given also intraperitoneally to mice for preclinical experiments (Abedi-Valugerdi et al. Citation2016).
The plasma concentrations of treosulfan were reported to be best fitted by a two-compartment model. Moreover, the drug parameters such as biological half-life (t0.5), volume of distribution (Vss), and total clearance (Cltot) were independent of the dose (Scheulen et al. Citation2000; Beelen et al. Citation2005; Nemecek et al. Citation2011).
Although treosulfan is known to be activated non-enzymatically, an inter-individual variability, up to 68%, was recently reported in several studies (Ten Brink et al. Citation2014a; Mohanan et al. Citation2018; van der Stoep et al. Citation2017) while few studies were reported to develop a limited sampling model for treosulfan in pediatric patients (Ten Brink et al. Citation2014a; Danielak et al. Citation2018).
Since treosulfan is activated non-enzymatically, most of the previous studies have recommended acidifying the blood samples upon collection from the patients or immediately after plasma separation to avoid its ex vivo bioactivation. Such quick acidification step could be cumbersome and extra load for the nurses and medical staff in addition to the risk of hemolysis. Moreover; it was reported that samples should be frozen immediately after plasma separation (Glowka et al. Citation2007; Główka et al. Citation2008; Romański et al. Citation2014; Glowka et al. Citation2015; Koyyalamudi et al. Citation2016). Same procedure was also reported for urine samples (Glowka et al. Citation2007; Główka et al. Citation2008). On the other hand; treosulfan was previously reported to be stable at room temperature and at +4 °C up to 5 h and at −20 °C up to 2 months without acidification (Ten Brink et al. Citation2014a). These controversial results attracted us to establish a solid protocol for samples handling that keeps accurate measurements with the minimum stress on the medical staff.
Additionally, some of the in vitro experiments, such as cell culture and microsomal incubation, are rather short investigations and incubations with treosulfan can give false results since this drug needs time to be activated. We also aimed to develop an accurate protocol for treosulfan bioactivation that ends up with the active epoxides to be utilized for our upcoming in vitro studies. These investigations will certainly help us in developing new drug formulations that may reduce the drug comorbidities and can be used for low-dose outpatient treatment.
Material and methods
All stock solutions were freshly prepared and experiments were run at least in triplicates including blank, negative control, and positive control samples.
Treosulfan stability in Milli-Q water
A preliminary test was first carried out in which treosulfan (Medac, Hamburg, Germany) at a concentration of 5 mM was dissolved in Milli-Q water obtained from in-house system (measured pH 6.99) and left at room temperature for 7 d. Treosulfan was measured upon preparation, after 24 h and after 7 d.
Treosulfan stability in human plasma
Treosulfan stability was evaluated at different temperature conditions (room temperature, +37 °C, +4 °C, −20 °C, and three cycles of freezing/thawing) and at different pHs (7.4, 4.5, and 8.3) over several time points up to 72 h in addition to and long term freezing at −20 °C for 6 months. Samples were freshly prepared and aliquoted before storage. Frozen aliquots were thawed only at one specific time point except samples for three cycles of freezing/thawing. The intact plasma pH was measured to be 7.4. Plasma pH was acidified using 0.35 M citric acid (Sigma Aldrich, Steinheim, Germany) or alkalified using 0.1 M sodium hydroxide (Merck, Darmstadt, Germany). It was interesting to test treosulfan bioactivation rate in alkaline pH in order to compare it with the neutral pH which can be important for drug preparation for in vitro experiments. The obtained plasma pH was initially checked using pH meter (Jenway 3510, Staffordshire, UK).
Heparinized pooled plasma from healthy individuals, obtained from the blood and transfusion center at Karolinska University Hospital, was stored at −20 °C until needed.
A stock solution of 100 mM treosulfan in Milli-Q water was first prepared then diluted in plasma at various pH to reach final concentrations of 0.5, 1, and 5 mM of treosulfan. The aliquots were stored at different temperatures conditions as mentioned above. The concentrations of treosulfan in all samples were measured upon preparation and after 0.5, 1, 2, 4, 6, 8, 24, 48, and 72 h for samples at pH 7.4 and only after 24, 48, and 72 h for the both pH 4.5 and 8.3. Treosulfan in the samples for freezing and thawing were measured after the third cycle and samples for long-term freezing were measured after 6 months of storage (Shah et al. Citation1991, Citation2000).
Treosulfan stability in human urine
The same previous experiment in plasma was repeated to measure treosulfan stability in urine. Urine from healthy individuals was freshly collected and pooled upon the start of the experiment. Urine pH was altered similar to plasma samples and treosulfan stock solutions were prepared as previously reported. Since the physiological variability of human urine pH is high, it was important to adjust our samples pH carefully even for pH 7.4.
All samples were measured upon preparation and after 24, 48, and 72 h, with the exception of the samples for freezing and thawing that were measured after the third cycle and samples for long-term freezing that were measured after 6 months.
Treosulfan stability in cell culture media
The same experiment was also repeated to measure treosulfan stability in cell culture media using Dulbecco's Modified Eagle's medium (DMEM) (Life technologies, Paisley, UK), supplemented with 10% heat inactivated fetal bovine serum (FBS) and 1% penicillin (100 U/mL) and streptomycin (100 µg/mL) to mimic conditions used when cytotoxicity will be done for treosulfan in different cell lines.
Media pH was altered similar to plasma samples and treosulfan stock solutions were prepared as previously reported. All samples were measured upon preparation and after 24, 48, and 72 h, with the exception of the samples for freezing and thawing that were measured after the third cycle and samples for long-term freezing that were measured after 6 months.
Treosulfan in whole blood
The aim of this experiment was to evaluate the treosulfan stability during the process of plasma extraction in normal blood compared to acidified blood.
Whole blood from a healthy individual was obtained from the blood and transfusion center at Karolinska University Hospital and EDTA was used as anti-coagulant. Blood was acidified using citric acid (0.35 M, 50 µL/1 mL blood) (Główka et al. Citation2008). Treosulfan was prepared in Milli-Q water and diluted in whole blood samples to reach final concentrations of 0.5, 1, and 5 mM. Plasma was then separated according to the hospital protocol by centrifugation at 4000 g for 10 min and samples were immediately prepared for treosulfan measurement as mentioned later in Section Treosulfan measurement using high-performance liquid chromatography (HPLC). The same experiment was also repeated in normal blood (non-acidified, pH 7.4).
Cytotoxicity assay and cell viability
The cytotoxicity of treosulfan on the leukemic cells HL-60 (DSMZ, Braunschweig, German) and K562 (LGC Promochem Ab, Borås, Sweden) was determined through the water-soluble tetrazolium salt-1 (WST-1) assay (Roche, Indianapolis, IN). A stock solution of 1 mM treosulfan was freshly prepared in complete DMEM and diluted further in order to estimate the half maximal inhibitory concentration (IC50) of treosulfan in both cells lines. Concentration used for treosulfan were; 0.001, 0.005, 0.01, 0.05, 0.1, 0.5, 1 mM; and 0.05, 0.1, 0.5, 1, 2, 5, 10 mM, respectively, for HL-60 and K652 cell lines. The HL-60 cells and the K562 cells were cultivated in a complete DMEM supplemented with 10% FBS and 1% PS at 37 °C with 5% CO2.
The cytotoxicity of the cells after adding treosulfan was estimated by measuring absorbance of the viable stained cells with trypan blue at a 1:1 ratio. Cell suspension (90 μL, 10 × 103) and treosulfan (10 μL, different concentrations) were added in each well of a 96-well plate. The experiment was carried out with five replicates for each dilution of treosulfan. The absorbance was measured at two time points, 24 h and 48 h. The controls used in this experiment were cell culture media without cells; cell culture media; and the highest concentration of treosulfan and cell culture media and cells with no treosulfan. The same experiment was repeated after pre-incubation of treosulfan in complete DMEM for 24 h at 37 °C.
Treosulfan measurement using high-performance liquid chromatography (HPLC)
All treosulfan samples were prepared and measured according to Główka et al. (Citation2013). Each sample (500 µL) was mixed with an equal volume of phosphate buffer (0.01 M, pH 4.5) adjusted by 0.35 M citric acid to avoid treosulfan activation (Glowka et al. Citation2013). Acetaminophen at a concentration of 5 mM was used as an internal standard and 50 µL were added to the previous mix (Glowka et al. Citation2013). Samples were vortexed, centrifuged (30,000 g) for 10 min at 4 °C and filtered using a 4 mm syringe filter (Koyyalamudi et al. Citation2016) into HPLC tubes (100 µL). Samples prepared in cell culture media did not need any filtration and directly transferred to HPLC tubes after the vortex step.
The HPLC system used to measure treosulfan consisted of an Agilent 1100 series autosampler connected to a refractometric detector heated at 35 °C. The column was a ReproSil-Pur basic C18 (150 × 4 mm, 5 μm microspheres) purchased from Dr Maisch HPLC GmbH (Entringen, Germany). The mobile phase was composed of sodium acetate-acetic acid buffer (pH 4.5) and acetonitrile (95:5, v/v) and the flow rate was 1 ml/min (Glowka et al. Citation2013). The retention time under these conditions was 7.2 min for treosulfan and 11.6 min for acetaminophen.
Because of the different matrixes used in our study, method was revalidated for plasma, urine, and cell culture media (Shah et al. Citation1991, Citation2000). Calibration curves were run for at least three times for each matrix (plasma, urine, and cell culture media). Each curve consisted of 8–10 points in addition to the blank sample. The quantification analysis was based on the ratio peak area treosulfan/peak area IS and equal weighting in a linear regression analysis equation. Samples for quality control (QC) were run daily and randomly among the unknown samples for accuracy and precision (Shah et al. Citation1991).
Data collection, chromatogram integration, and determination of the treosulfan concentrations were carried out using a Clarity chromatographic station (version 7.2, DataApex Ltd., Prague, The Czech Republic) as integration software.
Statistical analysis
Calculations, statistics and graphs were performed using Microsoft Excel and GraphPad Prism (version 5.0, Graph-Pad Software, Inc., La Jolla, CA).The absorbance values obtained from the multi-well plate reader were normalized to percentages to make the results from the two cell lines comparable.
Treosulfan concentrations were calculated as mean and standard deviation of the three experiments followed by calculating its stability at different time points as a percentage of its concentration at zero-time point. The IC50 was calculated from the results of the cytotoxicity assay. The half-life (t1/2) of treosulfan was calculated using GraphPad Prism one phase decay model.
Results and discussion
Treosulfan stability in Milli-Q water
Treosulfan was 100% stable in Milli-Q water for the 7-d period at room temperature. Milli-Q water is ultrapure deionized water while treosulfan is a water soluble compound. The absence of ions in this water preserved the drug stability. Milli-Q water can be safely used for drug preparation and for testing new pharmaceutical formulation.
Treosulfan stability in human plasma
All plasma stability results are listed in , while presents the short-term stability for plasma samples at pH 7.4 at different temperatures.
Figure 1. Short-term stability for plasma samples at pH 7.4 at different temperatures. Treosulfan stability in plasma was evaluated at different temperature conditions (room temperature, +4 °C and −20 °C) for short-term incubation at pH 7.4 over several time points up to 8 h and different treosulfan concentrations. Treosulfan degraded almost in the same pattern at different temperatures regardless the drug concentration. At room temperature, treosulfan was stable up to 80% in the first 2 h, after that it started to be metabolized. The rate of treosulfan degradation at +4 °C was slower than what was obtained at room temperature. Frozen samples at −20 °C had the highest stability; treosulfan stability was 91% at 8 h. Plasma samples containing treosulfan can be safely stored at −20 °C for short period up to 8 h.
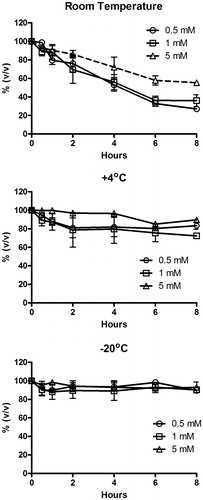
Table 1. Treosulfan stability in plasma at different conditions.
At room temperature, treosulfan at a concentration of 5 mM was stable up to 72 h only in the acidified plasma (94% of treosulfan left) whereas stability dropped to 5% and 1% after 48 h at pH 7.4 and 8.3, respectively. At pH 7.4, treosulfan was stable up to 80% within the first 2 h, after that it started to be metabolized till 40% at 8 h and 22% at 24 h. Similar results were obtained with samples stored at +37 °C, however; treosulfan was completely degraded within 24 h at pH 7.4. When temperature decreased to 4 or −20 °C, treosulfan stability increased at both pH 7.4 and 8.3 compared with 37 °C and room temperature. However, the temperature did not altered stability of treosulfan at pH 4.5.
Treosulfan degradation had almost the same pattern at different concentrations regardless the temperature. However, treosulfan had a higher half-life (10.8 h) at 5 mM compared with the half-lives at 0.5 mM (4.0 h) and 1 mM (3.6 h) at room temperature. Samples at pH 8.3 (5 mM) had a half-life of 7.7 h indicating that treosulfan is metabolized more quickly at alkaline pH. Since treosulfan in acidified plasma samples was stable all the time, its half-life was not possible to be calculated. These findings are in agreement with previous reports that pharmacodynamics of drugs such as treosulfan are influenced by administration routes, distribution, metabolism and elimination (Lin and Lu Citation1998; Huang et al. Citation2010).
Similar to samples stored at room temperature, treosulfan was stable at +4 °C only in acidified plasma. The rate of treosulfan degradation at +4 °C was slower than what was obtained at room temperature. Samples at pH 8.3 showed quicker degradation and only 16% of treosulfan was left after 72 h in comparison to 40% at pH 7.4. Samples pH 7.4, had stability of treosulfan up to 82% in the first 8 h.
Frozen samples at −20 °C had the highest stability. As previous results, acidified samples were stable up to 72 h (90%) and alkalified samples had the lowest stability (52% after 72 h). In samples stored at pH 7.4, treosulfan stability was 91% at 8 h and 61% at 72 h.
Except for acidified plasma, samples measured after three cycles of freezing/thawing showed significant degradation after the third cycle when compared with the samples that were frozen at −20 °C and defrosted once for measurement.
Results obtained from long-term freezing for 6 months confirmed the previous results, acidic samples were the most stable samples (94%) compared with alkalified samples (79%). Samples at pH 7.4 had concentration dependent stability; samples at concentration of 0.5 mM, had stability of 43% compared with 1 mM (60%) and 5 mM (83%). Furthermore, acidified samples were the easiest to filter after long-term freezing compared to other samples.
Currently, most of the samples from patients undergoing treatment with treosulfan are acidified after collection to prevent artificial degradation of the drug which can be an extra load for the medical staff (Glowka et al. Citation2007; Główka et al. Citation2008; Glowka et al., Citation2015; Koyyalamudi et al. Citation2016). Our results are in agreement with previous publications reporting that acidified samples are more stable than samples at other pH. Plasma samples acidification could be sufficient and that the freezing step could be unnecessary as treosulfan does not degrade at acidic pH. Samples can be safely stored at room temperature up to 72 h after acidification.
On the other hand; Ten Brink et al. have reported that treosulfan in plasma was stable at +4 °C up to 5 h and at −20 °C up to 2 months without acidification (Ten Brink et al. Citation2014a). We have shown that samples had variable stability at different temperatures without acidification; however, freezing the samples at −20 °C or less will keep them more stable for at least 24 h. Samples stored for longer time should be acidified. Acidification should also be recommended if the plasma samples are in a risk of thawing and refreezing.
To summarize; plasma samples containing treosulfan can be safely stored in −20 °C for short time up to 8 h. For longer storage time or for repeated thawing/freezing, samples should be acidified to avoid treosulfan degradation and to facilitate plasma filtration.
Based on these findings, some part of the dissolved treosulfan in the intravenous solution should be already activated before it enters the human body by the end of the infusion.
Treosulfan stability in urine
Similar to plasma samples, urine samples had the same pattern with slightly higher stability compared to plasma samples. At room temperature, acidified samples had stability of 98% after 72 h compared to alkalified samples (37%) and samples at pH 7.4 (61%). As in plasma, treosulfan was stable at pH 4.5 regardless the storage temperature. At both neutral and basic pH, Treosulfan was less stable at 37 °C than room temperature, at 4 °C or at −20 °C (). When samples were frozen at −20 °C, treosulfan was over 89% stable up to 72 h regardless the samples pH. Moreover, the three cycles of thawing/freezing did not affect the samples as stability was also over 87%. Results obtained from long-term freezing for 6 months showed that all samples had treosulfan stability over 91% regardless the samples pH or drug concentrations (). Since treosulfan was more stable in most of the urine samples, its half-life was not possible to be calculated.
Table 2. Treosulfan stability in urine at different conditions.
To the best of our knowledge, only few studies have previously reported treosulfan quantification in urine samples (Hilger et al. Citation1998, Citation2000; Glowka et al. Citation2007; Główka et al., Citation2008). All these studies have acidified the samples upon collection. Based on results, there is no major need for urine samples to be acidified if samples are stored at −20 °C or less.
Treosulfan stability in cell culture media
The stability tests of treosulfan in cell culture media have confirmed our previous findings; treosulfan at room temperature was unstable, dropping to below 32% within 24 h in all samples except for those at pH 4.5 which kept the same stability up to 72 h (99%). Over the 72-h period, treosulfan degraded most quickly at pH 8.3 (1%) compared with pH 7.4 (4%).Similarly, samples at 37 °C were the most unstable except for pH 4.5, with concentration of treosulfan dropping to zero over 24 h. Treosulfan was stable at 4 °C only in acidic pH while the other samples had average stability of 46% after 72 h.
Treosulfan was most stable at −20 °C, losing less than 8% in 24 h at all pH tested. After 72 h, treosulfan stability was up to 78% or more in all pH. Treosulfan samples that underwent three cycles of freezing and thawing were stable only at pH 4.5 (100%). Samples at pH 7.4 and 8.3 had stability of 51% and 45%, respectively. Treosulfan stability was not affected by its concentration with the exception of samples kept at room temperature which showed that 5 mM treosulfan was slightly more stable.
Following storage of samples for 6 months at −20 °C, acidified samples were the most stable samples (99%) compared with alkalified samples (86%). Samples at pH 7.4 did not have concentration-dependent stability; samples at a concentration of 0.5 mM, had stability of 92% compared with 1 mM (91%) and 5 mM (97%). Similar to urine samples, treosulfan was slightly more stable in cell culture media compared with plasma ().
Table 3. Treosulfan stability in cell culture media at different conditions.
The half-life of treosulfan at room temperature at pH 8.3 (9.7 h) was 32% shorter compared to that calculated at pH 7.4 (14.2 h) confirming what was observed in plasma that treosulfan is metabolized at a slightly faster rate at alkaline pH compared with neutral pH. The half-life of treosulfan did not have significant variations among lower treosulfan concentrations (8.8 h at concentration of 0.5 mM and 9.7 h at concentration of 1 mM). Similar to plasma samples, treosulfan in acidified samples was stable all the time and its half-life was not possible to be calculated.
Due to the instability at neutral pH, samples containing treosulfan should be acidified and/or stored at −20 °C or lower in order to prevent significant loss of the drug. For in vitro studies such as metabolic pathway, cytotoxicity and/or inhibition or induction of cytochrome P450 enzymes, rapid activation of treosulfan may be required; hence pre-incubation of treosulfan at 37 °C could be used since 100% of treosulfan is activated within 24 h.
There was a significant loss of treosulfan following three cycles of thawing and refreezing at −20 °C in comparison with samples that were thawed only once. It would be optimal to prepare the treosulfan fresh for in vitro studies; however, if freezing was required aliquots should be made so that the treosulfan is thawed only once.
These results demonstrate that treosulfan stability in DMEM is pH and temperature dependent but not concentration dependent. To the best of our knowledge; this is the first study to examine the stability of treosulfan in cell culture media.
Treosulfan in whole blood
No significant difference was found in treosulfan degradation in neutral blood samples compared with acidified samples (93%). Treosulfan was stable during the short process of plasma separation (86%, 93%, and 100% for treosulfan concentrations of 0.5, 1, and 5 mM, respectively). Obviously there is a trend of concentration-dependent stability; samples with expected low treosulfan concentrations should be centrifuged quickly and plasma should immediately be acidified or quantified.
Acidified plasma was hemolyzed compared with the other samples (Supplementary Figure 1). These hemolyzed samples may not be valid for other biochemical investigations as the hemolysis can interfere with several methods of detection.
As mentioned previously, samples from patients undergoing treatment with treosulfan are acidified upon collection (Glowka et al. Citation2007; Główka et al., Citation2008; Glowka et al., Citation2015; Koyyalamudi et al. Citation2016). Our results have shown that treosulfan is stable in whole blood during plasma separation. Moreover, the risk for samples hemolysis is rather high when samples are acidified. In agreement with our results; Ten Brink et al. have also reported that treosulfan in whole blood samples is stable during 5 h at room temperature without acidification (Ten Brink et al. Citation2014a).
Cytotoxicity assay and cell viability
Our results showed that HL-60 cell line was more sensitive to treosulfan compared with K562 cell line. The HL-60 cells showed that 90% and 20% of the cells were viable after 24 and 48 h, respectively. In order to estimate the IC50 in HL-60 cells, the concentrations of treosulfan were further adjusted. The final concentrations of treosulfan chosen were 0.001, 0.005, 0.01, 0.05, 0.1, 0.5, and 1 mM. HL-60 cells viability was concentration dependent; the IC50 of HL-60 cells after 24 h (9.2 μM) was almost six times higher than the IC50 after 48 h (1.6 μM). The present results are in agreement with the previously reported IC50 values (Gil et al. Citation2007).
On the other hand, no toxicity was observed in K562 cells up to a concentration of 0.1 mM treosulfan. The concentrations of treosulfan were further adjusted to 0.05, 0.1, 0.5, 1, 2, 5, and 10 mM in order to calculate the IC50. Higher concentrations of treosulfan (up to 5 mM) were required to kill the K562 cells after 24 h. These findings are consistent with previous studies of the effects of treosulfan on K562 cells which showed that cross-links form slowly up to 1 mM (Hartley et al. Citation1999). In K562 cells, the IC50 after 24 h (151 μM) was more than two times higher than the IC50 after 48 h (62 μM). The IC50 values obtained for K562 cells were in accordance with the values reported previously (Hartley et al. Citation1999; Munkelt et al. Citation2008).
As mentioned previously; the IC50 of the K562 cells was higher than the value for the HL-60 cells after 24 h. K562 cells are a chronic myeloid leukemia (CML) cell line while HL-60 cells are an acute myeloid leukemia (AML) cell line, the IC50 values suggest that CML patients can be more resistant to treosulfan compared with AML patients explaining the higher frequency and efficacy of treosulfan use nowadays for conditioning regimen prior to stem cell transplantation in AML – compared with CML – patients (Holowiecki et al. Citation2008; Gyurkocza et al. Citation2014; Maschan et al. Citation2016; Holtick et al. Citation2017; Nagler et al. Citation2017; Sakellari et al. 2017).
In agreement with our results obtained for the stability of treosulfan at pH 7.4 and 37 °C, the IC50 values indicates that treosulfan becomes more active over time, leading to an increase in cell death in both cell lines studied. These findings are supported by previous studies of the effect of treosulfan on protein kinase C (PKC) which showed that PKC-δ underwent membrane translocation in the presence of treosulfan that led to apoptosis (Schmidmaier et al. Citation2004).
Several mechanisms of drug resistance employed by cancer cells is known, they includes drug inactivation, drug target alteration, drug efflux, DNA damage repair, and cell death inhibition (Housman et al. Citation2014). The apoptotic effects of etoposide, another cytostatic agent, were previously examined on both K562 and HL-60 cells and showed also that K562 were more resistant to apoptosis than HL-60 cells (Sanchez-Garcia and Martin-Zanca Citation1997; O'Hare et al. Citation2007). K562 cells did not display any apoptotic changes for 3–4 d with a concentration of 17 μM etoposide, however, apoptosis started after 24–48 h following an increased dose of etoposide up to 68 μM (Martins et al. Citation1997). In accordance with our results, the K562 cells were killed only after incubation with high doses of treosulfan compared with the HL-60 cells but also signs of K562 cell death were only observed after 24 h treatment with 100 μM treosulfan. In agreement with Martins et al., the HL-60 cells were apoptosis proficient with signs of apoptosis within 2–3 h (Martins et al. Citation1997).
HL-60 cell death had increased following treosulfan pre-incubation for 24 h at 37 °C. Only 52% of the cells were viable after pre-incubation with 0.01 mM treosulfan compared with 80% of cells following treatment with freshly prepared treosulfan at the same concentration. On the other hand; 90% of the K562 cells were viable following incubation with 0.01 mM treosulfan in both conditions ().
Figure 2. Cytotoxicity of treosulfan on (A) HL-60 and (B) K562 cells following incubationfor 24 h at 37 °C. The cytotoxicity of treosulfan on the leukemic cells HL-60 and K562 was determined through the WST-1 assay. The HL-60 cell line was more sensitive to treosulfan compared with K562 cell line. The HL-60 cells decrease in cell viability was concentration dependent. On the other hand, no toxicity was found in the K562 cells up to a concentration of 0.1 mM treosulfan. The IC50 of the HL-60 cells was 9.2 μM after 24 h and 1.6 μM after 48 h. In K562 cells, the IC50 was 151 μM after 24 h and 62 μM after 48 h treatment. Treosulfan cytotoxicity increased following pre-incubation for 24 h at 37 °C. Only 52% of the HL-60 cells were viable after treatment with the pre-incubated 0.01 mM treosulfan compared to 80% of HL-60 cells following treatment with freshly prepared treosulfan at the same concentration (A). On the other hand; 90% of the K562 cells were viable following incubation with 0.01 mM treosulfan with or without pre-incubation (B).
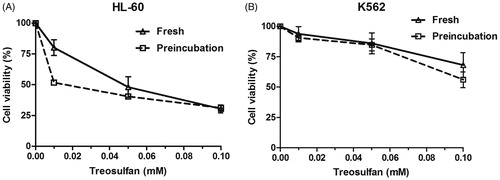
The results obtained for the stability of treosulfan in cell culture media at pH 7.4 have shown that following pre-incubation at 37 °C for 24 h treosulfan has been bioactivated to its both active epoxides. These data could be used for further in vitro studies on the toxicity of the epoxides as individual cytotoxic entities.
Treosulfan measurement using HPLC
The limit of quantitation was 10 µM for all biological fluids and the calibration curve was linear between 25 and 5000 µM. Accuracy and precision were established from the analysis of standard curves and QCs using different matrices. R2 for all curves was between 0.996 and 0.999 and the QC results showed a standard deviation <15% for all values obtained.
Conclusion
The stability profiling of treosulfan at different conditions was established and provided important reference for proper handling of biological samples containing treosulfan for both in vivo and in vitro studies. Biological samples containing treosulfan can be safely stored at −20 °C for short time points up to 8 h. For longer storage time, samples should be acidified to avoid treosulfan degradation.
A significant higher cytotoxicity was observed HL-60 cells compared to K562 cells. Treosulfan toxicity was increased following pre-incubation for 24 h at 37 °C. These data are applicable not only for in vivo studies but also for in vitro studies where treosulfan is required to be prepared before the experiment.
These results can be utilized as a corner stone for several upcoming investigations that will help in better understanding for the drug kinetics and dynamics and decrease its toxicity. Our findings will be also valuable in developing new pharmaceutical formulations that may reduce the drug comorbidities and enhance the use of low-dose outpatient treatment. Such studies are required in order to personalize treosulfan treatment and improve the clinical outcome.
Supplementary Figure
Download MS Word (538.1 KB)Disclosure statement
The authors declare that they have no conflict of interest.
Additional information
Funding
References
- Abedi-Valugerdi M, Wolfsberger J, Pillai PR, Zheng W, Sadeghi B, Zhao Y, Hassan M. 2016. Suppressive effects of low-dose 5-fluorouracil, busulfan or treosulfan on the expansion of circulatory neutrophils and myeloid derived immunosuppressor cells in tumor-bearing mice. Int Immunopharmacol. 40:41–49.
- Beelen DW, Trenschel R, Casper J, Freund M, Hilger RA, Scheulen ME, Basara N, Fauser AA, Hertenstein B, Mylius HA. 2005. Dose-escalated treosulphan in combination with cyclophosphamide as a new preparative regimen for allogeneic haematopoietic stem cell transplantation in patients with an increased risk for regimen-related complications. Bone Marrow Transplant. 35:233–241.
- Chekerov R, Kaltenecker G, Reichert D, Gohler T, Klare P, Oskay-Ozcelik G, Sauer U, Wischnik A, Vehling-Kaiser U, Becker M. 2015. Treosulfan in the treatment of advanced ovarian cancer – results of a German Multicenter Non-interventional Study. Anticancer Res. 35:6869–6875.
- Danielak D, Twardosz J, Kasprzyk A, Wachowiak J, Kałwak K, Główka F. 2018. Population pharmacokinetics of treosulfan and development of a limited sampling strategy in children prior to hematopoietic stem cell transplantation. Eur J Clin Pharmacol. 74:79–89.
- Duncan ID, Clayton LA. 1985. Combination chemotherapy of ovarian carcinoma with cisplatinum and treosulfan – a phase II study. Br J Obstet Gynaecol. 92:762–767.
- Feit PW, Rastrup-Andersen N, Matagne R. 1970. Studies on epoxide formation from (2S,3S)-threitol 1,4-bismethanesulfonate. The preparation and biological activity of (2S,3S)-1,2-epoxy-3,4-butanediol 4-methanesulfonate. J Med Chem. 13:1173–1175.
- Gil L, Styczynski J, Dytfeld D, Debski R, Kazmierczak M, Kolodziej B, Rafinska B, Kubicka M, Nowicki A, Komarnicki M, et al. 2007. Activity of bortezomib in adult de novo and relapsed acute myeloid leukemia. Anticancer Res. 27:4021–4025.
- Glowka F, Kasprzyk A, Romanski M, Wrobel T, Wachowiak J, Szpecht D, Kalwak K, Wiela-Hojenska A, Dziatkiewicz P, Tezyk A. 2015. Pharmacokinetics of treosulfan and its active monoepoxide in pediatric patients after intravenous infusion of high-dose treosulfan prior to HSCT. Eur J Pharm Sci: Off J Eur Federation Pharm Sci. 68:87–93.
- Główka FK, Karaźniewicz-Łada M, Grund G, Wróbel T, Wachowiak J. 2008. Pharmacokinetics of high-dose i.v. treosulfan in children undergoing treosulfan-based preparative regimen for allogeneic haematopoietic SCT. Bone Marrow Transplant. 42(Suppl 2):S67–S70.
- Glowka FK, Lada MK, Grund G, Wachowiak J. 2007. Determination of treosulfan in plasma and urine by HPLC with refractometric detection; pharmacokinetic studies in children undergoing myeloablative treatment prior to haematopoietic stem cell transplantation. J Chromatogr B: Analyt Technol Biomed Life Sci. 850:569–574.
- Glowka FK, Romanski M, Tezyk A, Zaba C. 2013. Direct high-performance liquid chromatography method with refractometric detection designed for stability studies of treosulfan and its biologically active epoxy-transformers. J Pharm Biomed Anal. 72:145–149.
- Greystoke B, Bonanomi S, Carr TF, Gharib M, Khalid T, Coussons M, Jagani M, Naik P, Rao K, Goulden N, et al. 2008. Treosulfan-containing regimens achieve high rates of engraftment associated with low transplant morbidity and mortality in children with non-malignant disease and significant co-morbidities. Br J Haematol. 142:257–262.
- Gropp M, Meier W, Hepp H. 1998. Treosulfan as an effective second-line therapy in ovarian cancer. Gynecol Oncol. 71:94–98.
- Gyurkocza B, Gutman J, Nemecek ER, Bar M, Milano F, Ramakrishnan A, Scott B, Fang M, Wood B, Pagel JM. 2014. Treosulfan, fludarabine, and 2-Gy total body irradiation followed by allogeneic hematopoietic cell transplantation in patients with myelodysplastic syndrome and acute myeloid leukemia. Biol Blood Marrow Transplant. 20:549–555.
- Hartley JA, O'Hare CC, Baumgart J. 1999. DNA alkylation and interstrand cross-linking by treosulfan. Br J Cancer. 79:264–266.
- Hilger RA, Harstrick A, Eberhardt W, Oberhoff C, Skorzec M, Baumgart J, Seeber S, Scheulen ME. 1998. Clinical pharmacokinetics of intravenous treosulfan in patients with advanced solid tumors. Cancer Chemother Pharmacol. 42:99–104.
- Hilger RA, Jacek G, Oberhoff C, Kredtke S, Baumgart J, Seeber S, Scheulen ME. 2000. Investigation of bioavailability and pharmacokinetics of treosulfan capsules in patients with relapsed ovarian cancer. Cancer Chemother Pharmacol. 45:483–488.
- Holowiecki J, Giebel S, Wojnar J, Krawczyk-Kulis M, Markiewicz M, Holowiecka-Goral A, Freund M, Casper J. 2008. Treosulfan and fludarabine low-toxicity conditioning for allogeneic haematopoietic stem cell transplantation in chronic myeloid leukaemia. Br J Haematol. 142:284–292.
- Holtick U, Herling M, Pflug N, Chakupurakal G, Leitzke S, Wolf D, Hallek M, Scheid C, Chemnitz JM. 2017. Similar outcome after allogeneic stem cell transplantation with a modified FLAMSA conditioning protocol substituting 4 Gy TBI with treosulfan in an elderly population with high-risk AML. Ann Hematol. 96:479–487.
- Housman G, Byler S, Heerboth S, Lapinska K, Longacre M, Snyder N, Sarkar S. 2014. Drug resistance in cancer: an overview. Cancers (Basel). 6:1769–1792.
- Huang J, Bathena SP, Alnouti Y. 2010. Metabolite profiling of praziquantel and its analogs during the analysis of in vitro metabolic stability using information-dependent acquisition on a hybrid triple quadrupole linear ion trap mass spectrometer. Drug Metab Pharmacokinet. 25:487–499.
- Koyyalamudi SR, Kuzhiumparambil U, Nath CE, Byrne JA, Fraser CJ, O'Brien TA, Earl JW, Shaw PJ. 2016. Development and validation of a high pressure liquid chromatography-UV method for the determination of treosulfan and its epoxy metabolites in human plasma and its application in pharmacokinetic studies. J Chromatogr Sci. 54:326–333.
- Lin JH, Lu AY. 1998. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet. 35:361–390.
- Mahner S, Oskay-Ozcelik G, Heidrich-Lorsbach E, Fuxius S, Sommer H, Klare P, Belau A, Ruhmland B, Heuser T, Kolbl H. 2012. A prospective multicenter study of treosulfan in elderly patients with recurrent ovarian cancer: results of a planned safety analysis. J Cancer Res Clin Oncol. 138:1413–1419.
- Martins LM, Mesner PW, Kottke TJ, Basi GS, Sinha S, Tung JS, Svingen PA, Madden BJ, Takahashi A, McCormick DJ, et al. 1997. Comparison of caspase activation and subcellular localization in HL-60 and K562 cells undergoing etoposide-induced apoptosis. Blood. 90:4283–4296.
- Maschan M, Shelikhova L, Ilushina M, Kurnikova E, Boyakova E, Balashov D, Persiantseva M, Skvortsova Y, Laberko A, Muzalevskii Y, et al. 2016. TCR-alpha/beta and CD19 depletion and treosulfan-based conditioning regimen in unrelated and haploidentical transplantation in children with acute myeloid leukemia. Bone Marrow Transplant. 51:668–674.
- Mohanan E, Panetta JC, Lakshmi KM, Edison ES, Korula A, Na F, Abraham A, Viswabandya A, George B, Mathews V, et al. 2018. Pharmacokinetics and pharmacodynamics of treosulfan in patients with Thalassemia major undergoing allogeneic hematopoietic stem cell transplantation. Clin Pharmacol Therapeut. 104:575–583.
- Munkelt D, Koehl U, Kloess S, Zimmermann SY, Kalaaoui RE, Wehner S, Schwabe D, Lehrnbecher T, Schubert R, Kreuter J, et al. 2008. Cytotoxic effects of treosulfan and busulfan against leukemic cells of pediatric patients. Cancer Chemother Pharmacol. 62:821–830.
- Nagler A, Labopin M, Beelen D, Ciceri F, Volin L, Shimoni A, Foa R, Milpied N, Peccatori J, Polge E, et al. 2017. Long-term outcome after a treosulfan-based conditioning regimen for patients with acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Cancer. 123:2671–2679.
- Nemecek ER, Guthrie KA, Sorror ML, Wood BL, Doney KC, Hilger RA, Scott BL, Kovacsovics TJ, Maziarz RT, Woolfrey AE, et al. 2011. Conditioning with treosulfan and fludarabine followed by allogeneic hematopoietic cell transplantation for high-risk hematologic malignancies. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 17:341–350.
- O'Hare T, Eide CA, Deininger MW. 2007. Bcr-Abl kinase domain mutations, drug resistance, and the road to a cure for chronic myeloid leukemia. Blood. 110:2242–2249.
- Remberger M, Torlen J, Serafi IE, Garming-Legert K, Bjorklund A, Ljungman P, Sundin M, Hassan M, Mattsson J. 2017. Toxicological effects of fludarabine and treosulfan conditioning before allogeneic stem-cell transplantation. Int J Hematol. 106:471–475.
- Romański M, Teżyk A, Zaba C, Główka FK. 2014. Rapid and sensitive liquid chromatography-tandem mass spectrometry method for determination of protein-free pro-drug treosulfan and its biologically active monoepoxy-transformer in plasma and brain tissue. Talanta. 127:123–132.
- Romański M, Urbaniak B, Kokot Z, Główka FK. 2015. Activation of prodrug treosulfan at pH 7.4 and 37 °C accompanied by hydrolysis of its active epoxides: kinetic studies with clinical relevance. J Pharm Sci. 104:4433–4442.
- Sakellari I, Mallouri D, Gavriilaki E, Batsis I, Kaliou M, Constantinou V, Papalexandri A, Lalayanni C, Vadikolia C, Athanasiadou A. 2017. Survival advantage and comparable toxicity in reduced-toxicity treosulfan-based versus reduced-intensity busulfan-based conditioning Regimen in Myelodysplastic Syndrome and acute myeloid leukemia patients after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplan. 23:445–451.
- Sanchez-Garcia I, Martin-Zanca D. 1997. Regulation of Bcl-2 gene expression by BCR-ABL is mediated by Ras. J Mol Biol. 267:225–228.
- Scheulen ME, Hilger RA, Oberhoff C, Casper J, Freund M, Josten KM, Bornhauser M, Ehninger G, Berdel WE, Baumgart J. 2000. Clinical phase I dose escalation and pharmacokinetic study of high-dose chemotherapy with treosulfan and autologous peripheral blood stem cell transplantation in patients with advanced malignancies. Clin Cancer Res: Off J Am Assoc Cancer Res. 6:4209–4216.
- Schmidmaier R, Oellerich M, Baumgart J, Emmerich B, Meinhardt G. 2004. Treosulfan-induced apoptosis in acute myeloid leukemia cells is accompanied by translocation of protein kinase C delta and enhanced by bryostatin-1. Exp Hematol. 32:76–86.
- Sehouli J, Tome O, Dimitrova D, Camara O, Runnebaum IB, Tessen HW, Rautenberg B, Chekerov R, Muallem MZ, Lux MP, et al. 2017. A phase III, open label, randomized multicenter controlled trial of oral versus intravenous treosulfan in heavily pretreated recurrent ovarian cancer: a study of the North-Eastern German Society of Gynecological Oncology (NOGGO). J Cancer Res Clin Oncol. 143:541–550.
- Shah VP, Midha KK, Dighe S, McGilveray IJ, Skelly JP, Yacobi A, Layloff T, Viswanathan CT, Cook CE, McDowall RD, et al. 1991. Analytical methods validation: bioavailability, bioequivalence and pharmacokinetic studies. Conference report. Eur J Drug Metab Pharmacokinet. 16:249–255.
- Shah VP, Midha KK, Findlay JW, Hill HM, Hulse JD, McGilveray IJ, McKay G, Miller KJ, Patnaik RN, Powell ML, et al. 2000. Bioanalytical method validation-a revisit with a decade of progress. Pharm Res. 17:1551–1557.
- Sjoo F, Hassan Z, Abedi-Valugerdi M, Griskevicius L, Nilsson C, Remberger M, Aschan J, Concha H, Gaughan U, Hassan M. 2006. Myeloablative and immunosuppressive properties of treosulfan in mice. Exp Hematol. 34:115–121.
- Slatter MA, Rao K, Amrolia P, Flood T, Abinun M, Hambleton S, Nademi Z, Goulden N, Davies G, Qasim W, et al. 2011. Treosulfan-based conditioning regimens for hematopoietic stem cell transplantation in children with primary immunodeficiency: United Kingdom experience. Blood. 117:4367–4375.
- Ten Brink MH, Ackaert O, Zwaveling J, Bredius RG, Smiers FJ, den Hartigh J, Lankester AC, Guchelaar HJ. 2014a. Pharmacokinetics of treosulfan in pediatric patients undergoing hematopoietic stem cell transplantation. Ther Drug Monit. 36:465–472.
- Ten Brink MH, Zwaveling J, Swen JJ, Bredius RG, Lankester AC, Guchelaar HJ. 2014b. Personalized busulfan and treosulfan conditioning for pediatric stem cell transplantation: the role of pharmacogenetics and pharmacokinetics. Drug Discov Today. 19:1572–1586.
- Wachowiak J, Sykora KW, Cornish J, Chybicka A, Kowalczyk JR, Gorczynska E, Choma M, Grund G, Peters C, Party EPDW. 2011. Treosulfan-based preparative regimens for allo-HSCT in childhood hematological malignancies: a retrospective study on behalf of the EBMT pediatric diseases working party. Bone Marrow Transplant. 46:1510–1518.
- van der Stoep M, Bertaina A, Ten Brink MH, Bredius RG, Smiers FJ, Wanders DCM, Moes D, Locatelli F, Guchelaar HJ, Zwaveling J, et al. 2017. High interpatient variability of treosulfan exposure is associated with early toxicity in paediatric HSCT: a prospective multicentre study. Br J Haematol. 179:772–780.
