ABSTRACT
Learning Health Systems (LHSs) seek continuous improvement through the translation and integration of internally and externally generated knowledge across stakeholders within and external to the organization, yet current approaches are primarily described from the healthcare delivery perspective, leaving teaching and research responsibilities underexposed. Academic medical centers offer a unique perspective on LHSs because their mission includes teaching, research, and healthcare. This introduces an opportunity to enact, educate, and study processes and outcomes of LHSs within a single system. Little information is available to describe these processes and outcomes, resulting in a knowledge gap regarding the role of education and research in the quality improvement cycles and learning of LHSs. To close this knowledge gap, The George Washington University School of Medicine and Health Sciences initiated the Health Research and Education Collaboratory (GW Collaboratory) in 2017. The GW Collaboratory was established to study mechanisms supporting continuous quality improvement and learning in health systems within an academic medical center. We envision the GW Collaboratory as interconnected knowledge nodes facilitating collaboration among clinicians, patients, researchers, and educators to study the knowledge generation, dissemination, application, and evaluation required for continuous quality improvement and learning. We employ a project-based approach to foster communities of learning focused on exploring specific health problems of interest. We propose the GW Collaboratory as one model by which academic medical centers can contribute to the science of LHS.
Introduction
National efforts to make the health system safer and more equitable demand that health care systems engage in a continuous and rapid process of learning and quality improvement. There are many trends converging to drive this call to action for more rapid learning by health care systems, with learning being defined as behavioral and organizational change resulting from reflection upon new knowledge and insight. At a most basic level, the pace at which human knowledge is expanding requires constant learning; it is estimated that as of 2020, human knowledge doubles every 12 h. Yet despite this rapid proliferation of knowledge, it is estimated that new discoveries can take an average of 17 years to influence change in healthcare practice [Citation1]. The development of new knowledge and innovation alone do not eventuate change toward greater efficiency and effectiveness in healthcare systems. At the health system level, processes and mechanisms are required to support system learning, or the ability to translate new knowledge and innovation into improvement cycles for continuous adaptation toward greater system efficiency and effectiveness. Despite the recognized need for ongoing learning in healthcare, little is understood regarding the processes and infrastructure needed to promote integration of continuous cycles of improvement and learning in existing or emerging healthcare systems. An increasingly diverse patient population in an increasingly complex health system requires that learning to be optimized on an individual, team, group, and systems level. Further, the important role of faculty in entry-level healthcare professional education programs to learning in health systems is understudied. As a result, academic medical centers may be missing an important opportunity to study the intersection of education, research, and healthcare, thereby contributing to our understanding of processes and outcomes of Learning Health Systems. Learning Health Systems (LHSs) refer to systems in which “science and informatics, patient–clinician partnerships, incentives, and culture are aligned to promote and enable continuous and real-time improvement in both effectiveness and efficiency of care“ [Citation2,p.17]. For example, a LHS approach to diagnosis and treatment of diabetes draws on data related to incidence, utilization and health outcomes to identify problems and potential solutions to concerns in the area of work processes, protocols, and clinical roles. Currently, such approaches are typically described primarily from the healthcare delivery perspective with limited input from non-clinical stakeholders. Further, little attention is paid to the preparation of future practitioners, researchers, and educators to operate within and contribute to a LHS [Citation3]. As Etheridge notes, ‘there is a need to create a science of learning health systems,’ so that an interconnected system of multiple stakeholders (practitioners, educators, economists, technologies) can learn from one another how to engage in LHSs [Citation4,p.1157]. Consequently, we need to create and study connections among the healthcare research, education, and delivery systems which ensure the uptake of evidence-based innovations that will inform continuous quality improvement and learning within our healthcare system [Citation5]. Learning collaboratives, or learning collaboratories, are proposed as mechanisms to generate and diffuse knowledge and innovation and may be critical to the ‘development and evolution of learning health systems’ [Citation6,p.208]. This paper describes our academic approach to contributing to a science of LHSs through the formation of the GW Health Research and Education Collaboratory (GW Collaboratory) to study mechanisms supporting continuous quality improvement and learning across stakeholders in health systems.
An academic perspective on learning health systems
Creating a bridge between knowledge generation and its implementation is essential to continuous quality improvement and learning within health systems. Such a bridge is also essential to ensuring that future clinicians develop the requisite knowledge and skills required in today’s complex care delivery environment [Citation5]. The George Washington (GW) University School of Medicine and Health Sciences (SMHS) is linked to delivery systems through its partnerships with the GW University Hospital and the GW Medical Faculty Associates. ‘One GW’ reflects a close alignment and structure among these medical entities which supports three goals: ‘to offer patients the most comprehensive and highest quality of care possible; to train the next generation of medical professionals through technically advanced clinical techniques and modalities; and to improve patient outcomes by advancing biomedical, translational, and health services delivery research’ [Citation7]. The ‘One GW’ partnership provides a strong foundation upon which to build a bridge for continuous learning and quality improvement from a range of stakeholder perspectives, including but not limited to the clinical and patient experience, health care delivery, administration, research and education. Our focus in this paper is the mechanisms by which future practitioners can be engaged in a LHS approach during their entry-level education.
One potential contribution from the academic perspective to the science of LHSs is to focus on the learning processes in a LHS. Specifically, this contribution entails describing how knowledge translation and learning occur among and across key stakeholder populations. What structures, processes, and policies are needed to link healthcare research, education, and delivery systems for reciprocal knowledge generation, dissemination, and application? What are effective mechanisms for implementing systemic change? Addressing questions related to optimal learning processes, context, and activities is a critical contribution to the emerging science of LHSs. Friedman provides a foundational definition of the critical concept of learning in continuous improvement as follows:
“Learning refers to the capability for continuous improvement through the collection and analysis of data, creating new knowledge, and the application of the new knowledge to influence practice … . - - health systems become learning health systems when they acquire the ability to continuously, routinely, and efficiently study and improve themselves” [Citation8,p.1].
Within LHSs, people, technology, processes and policy support cycles of learning in which data converted to knowledge, knowledge influences performance, and ‘documented changes in performance generate new data that seeds the next iteration of the cycle’ [Citation9,p.17]. The purpose of the GW Collaboratory is to investigate and evaluate the processes and outcomes of these learning cycles.
Foley assessed the roles of LHSs in quality improvement and identified six different roles: intelligent automation, clinical decision support, predictive models, positive deviance, surveillance, and comparative effectiveness research [Citation3]. These roles were linked by Foley to the six dimensions of quality as defined by the Institute of Medicine: safe, effective, patient‐centered, timely, efficient, and equitable [Citation3]. Collectively, these conceptualizations describe the requisite system components, processes, and ultimate outcomes of learning at the system’s level of analysis within LHSs. Although the specification of LHSs such a defined by Friedman and its different roles as identified by Foley provides an excellent basis for further development, many of the potential mechanisms of change are still explorative and an empirical approach is needed to generate knowledge about how learning occurs across levels of analysis in LHSs [Citation3,Citation10]. For example, at the individual and inter-individual levels, we have yet to fully conceptualize the person-centered and team-based cognitive and behavioral changes required to support cycles of learning and quality improvement in health systems. At the systems level, we have limited understanding of how knowledge is disseminated across stakeholder groups as the basis for system level learning and change. For example, how is organizational learning affected by the use of formal training programs in comparison to team learning in an informal and aligned context? Further, we need additional insight into the potential role for schools of medicine and health sciences in stimulating the connections among the healthcare research, education, and delivery systems for meta-level change and learning. These future insights may prove critical to the uptake of evidence-based innovations within quality improvement cycles and also to the generation of new knowledge aimed at specific system-related problems, or the recognition of LHSs at the local level, and realization of LHSs on a broader national scale. Finally, as we work toward the realization of LHSs, we need to fully understand how to best prepare future system stakeholders (clinicians, researchers, educators) to participate in cycles of learning aimed at self-study and quality improvement.
The GW health research and education collaboratory
As noted by Nix et al. learning collaboratives ‘can support concurrent learning about what works with respect to diffusion and implementation and support or inform needed research’ [Citation6,p.210]. To establish a system to study the mechanisms supporting continuous quality improvement and learning, GW has launched the GW Collaboratory based upon the principles of LHSs. By forming connections among the healthcare delivery, healthcare education, and health research systems, we aim to create reciprocal knowledge relationships among these stakeholders required to develop scientific knowledge about the mechanisms that support continuous quality improvement and learning at multiple levels of analysis. Adopting a problem-centered approach, we strive to understand how connections among stakeholders influence the integration of evidence-based innovations aimed to improve care while also generating new knowledge about research required to continue the cycle of learning. We also aim to study the mechanisms required to support learning at the system, group, and individual levels of analysis.
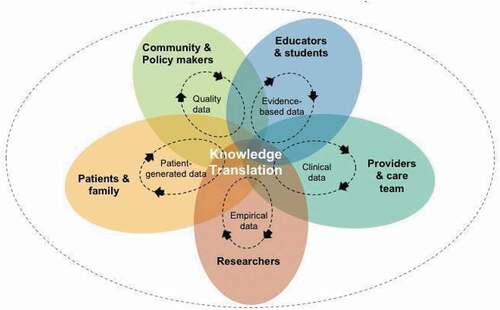
The GW Collaboratory aspires to be globally recognized as a pre-eminent center for the comprehensive study of health research and education. In , we adapted Nelson and colleagues’ model of a LHS [Citation11] to conceptualize the GW Collaboratory as a center for knowledge generation and knowledge translation through interaction of the participating stakeholders via continuous feedback loops (reflection on past performance) and feed forward loops (future-oriented solutions) supporting knowledge generation, knowledge translation, dissemination, and learning from data application.
Structure
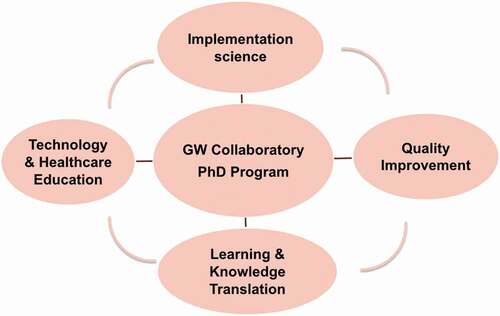
The GW Collaboratory builds from an informal network toward knowledge ecosystem model. The concept of knowledge ecosystem is used to define an interconnected community of practice that builds knowledge in a bottom-up, networked, and dynamic fashion [Citation11]. The GW Collaboratory is envisioned as a variety of interconnected knowledge nodes which anchor connections among the community, medical and health professions educators, researchers, health provision organizations, and patients and their families (see ). The GW Collaboratory is currently composed of four knowledge nodes: Implementation Science, Quality Improvement, Technology in Healthcare and Education, and Learning and Knowledge Translation. Yet, because we will adopt a problem-centered approach to knowledge generation, additional nodes are expected to develop as specific disciplinary expertise is required for problem exploration.
The networking structure is conceptualized as consisting of ‘members’ and ‘scholars.’ Clinicians, patients, and other interested stakeholders can become ‘members’ of the GW Collaboratory and gain from two main components: (a) information sharing-through webinars, seminar series, newsletters etc. – and (b) advice and consultancy services. Advice and consultancy include continuous professional development and support for developing and implementing quality improvement and learning projects. ‘Scholars’ support the needs of Collaboratory members and conduct joint research projects through funding from sources both internal and external to GW. The knowledge generated in these projects is used for dissemination and implementation among members and the broader scientific community [Citation10].
Initially, activities of the GW Collaboratory are aimed at creating the policies, processes, and structures required for knowledge generation, translation, and dissemination across stakeholder groups and at specific problem-based projects involving appropriate nodes. While the GW Collaboratory has an Executive Director to address administrative functions, node leaders have worked through a distributive structure to establish leadership on grants and writing projects and to create internal and external connections related to initial projects. The knowledge node leaders have all been engaged in writing research grants to support collaborations among researchers, clinicians and doctoral students aimed at quality improvement, implementation, and continuous learning in specific clinical contexts. Leadership on grant applications is determined by requisite expertise with the goal of engaging as many nodes as is appropriate for the project. These initial projects will allow us to determine the types of processes and structures required for reciprocal knowledge generation and dissemination across nodes and between scholars, members, and external partners. Additional activities and services of the GW Collaboratory are summarized in .
Table 1. Activities and services of the GW collaboratory*
Competencies
The GW Collaboratory supports the continuous development of members’ competencies in their specific roles as clinicians, researchers, or educators, and also in establishing links among the different roles. Forrest and colleagues have developed core competencies for researchers in LHSs [Citation12]. Through a consensus procedure seven competency domains were identified containing a total of 33 core competencies: 1. systems science; 2. research questions and standards of scientific evidence; 3. research methods; 4. informatics; 5, ethics of research and implementation in health systems; 6. improvement and implementation science; and 7. engagement, leadership, and research management [Citation12]. These competencies form the framework for researchers in our Collaboratory to build the body of knowledge supporting LHSs and continuous quality improvement. In addition, we aim to use these research competencies as the basis for developing core competencies for each of the other core stakeholder groups: clinicians, patients, and educators. For example, educators, clinicians, researchers, and students in the Learning and Knowledge Translation node are currently conducting a scoping review on requisite competencies for educators. Results from this review will be used to provide recommendations for academic and training programs within GW SMHS. The results will also be published in a peer-review journal.
Connections with doctoral education
The GW Collaboratory is closely connected to several doctoral level educational programs in the SMHS, including the Doctorate of Health Sciences (DHSci) and the Occupational Therapy entry-level and post-professional doctorates (OTD). A particularly close connection exists with the GW PhD program in Translational Health Science (THS), which aims to educate the next generation of healthcare leaders to meet the complex challenges of translating evidence into practice. The PhD in THS is based on an innovative, transdisciplinary curriculum emphasizing the importance of cross-disciplinary collaboration for generating and disseminating research that will have the greatest potential to influence systemic uptake and social impact [Citation13]. Continued efficacy of the THS curriculum requires a reciprocal relationship among scholars, educators, students, and the healthcare delivery system to ensure that future knowledge generation projects are targeted to meet the needs of multiple stakeholders within the broader healthcare system. Further, such a reciprocal relationship is critical to investigate the complex, real-world problems within and across our 'One GW' system.
The connections between several SMHS doctoral programs and the GW Collaboratory will serve as one mechanism by which knowledge generated in student dissertation research can readily be translated to a broader audience of health system stakeholders. The connections also ensure that knowledge gained from research can influence curricula for these future scholars.
Initial approach and projects
In forming the GW Collaboratory, we used a logic model to plan how the GW Collaboratory will meet the ultimate outcome of promoting the knowledge generation, application, and evaluation required for continuous learning and quality improvement. A logic model specifies the inputs, activities, and outputs (processes) required to meet short and long-term goals. Our short-term goals include but are not limited to 1) increasing the number of dissertations contributing to implementation science and knowledge translation, 2) serving as a valued resource for studying, teaching, and applying principles of knowledge translation, and 3) expanding the number of grants that study quality improvement from a multidisciplinary perspective [Citation14]. Activities required to meet these short- and long-term goals are conceptualized as either crossing several nodes or promoting knowledge generation, application, and evaluation within one node. For example, the Technology in Healthcare and Education node is conducting a study to test a caregiver-centered, online, interactive program to build caregiver skills for dementia care (known as C-TIPS) (www.go.gwu.edu/ctips). This intervention serves as a starting point for focused discussions with a range of service providers, family caregivers, administrators for aging services across the nation, and doctoral students. These focused discussions are a valuable knowledge translation mechanism to lay the groundwork for multidisciplinary efforts for the community of stakeholders to identify problems and solutions that can be tested using rigorous research methods. Further, a doctoral student from the PhD in THS is employed as a research assistant and will build on C-TIPS as the basis of their dissertation (preferred pronouns are they/them/theirs). provides the GW Collaboratory logic model with evaluation methods related to short-term, intermediate, and long-term outcomes.
Table 2. GW collaboratory logic model
The node-specific activities are complemented by cross-node activities to explore knowledge translation from a multidisciplinary perspective. For example, we initiated a six-part discussion series of knowledge translation and invited educators, researchers, policymakers, providers, students, and administrators to attend. Each meeting of this knowledge translation discussion series starts with a brief presentation about translating knowledge either generally or within a specific area, such as neuroaesthetics or treatment of traumatic brain injury. We are fortunate by virtue of our location in Washington, DC to be able to invite participation from federal agencies and special interest organizations with a national scope, as well as a broad network of providers, service agencies, and educational institutions. Though, we do rely heavily upon virtual meetings to facilitate both local and international participation in these discussions. The widespread use of virtual meeting formats makes this discussion approach relevant for any institution, regardless of location.
Finally, activities of the GW Collaboratory include leadership to convene an international committee of scholars for the purposes of establishing an international research agenda and implementation plan to reflect different levels of analysis from local to global conceptualizations of LHSs. This work seeks to build on the recommendations of a 2013 workshop funded by the National Science Foundation to establish a research agenda for LHSs in the USA [Citation10]. This international committee, a global community of scholars in health systems representing four countries (Australia, the Netherlands, the UK and US), has met virtually several times over the past year to share ideas, collaborate on related projects, and write a grant to fund an international conference. Consistent with the concept of an interconnected system of stakeholders, the work of the international committee is informed and supported by doctoral students, educators, policymakers, and researchers.
Conclusions
In this paper we have described the approach of the GW academic medical center to develop infrastructure supporting the study, education, and practice of continuous learning and quality improvement in health systems. The GW Collaboratory will build from an informal network toward a knowledge ecosystem model with clinicians, patients, researchers, and educators. We aim at conducting research and teaching activities through a continuous learning cycle, and we will provide services to members and scholars. We hope that our perspective inspires other academic institutions and will be used as an example of how such a learning collaboratory may be initiated. Thus, we aim to contribute to the essence of a learning health system: sharing knowledge and data for continuous improvement and learning.
Within the GW Collaboratory, we hope to demonstrate how schools of medicine and health professions education can promote learning health systems by not only creating structures and processes for continuous knowledge generation, application, and evaluation across multiple health system stakeholders but also by educating future educators and researchers for full participation health systems which embrace the value of continuous learning and quality improvement. Additionally, the initial activities described within this paper will allow us to gain insight into how to optimize future collaborations on a larger scale.
Abbreviations
C-TIPS: Caregiver-centered, Online, Interactive Program; GW: George Washington University; GW SMHS: George Washington University School of Medicine and Health Sciences; LHS: Learning Health System; THS: Translational Health Sciences.
Ethics Approval and Consent to Participate
This paper presents an argument for an academic approach to Learning Health Systems. It does not report research. Ethics approval and consent to participate were not required to create this writing.
Disclosure statement
The authors declare that they have no conflicting interests.
Additional information
Funding
References
- Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform. 2000;1(1):65–8.
- Institute of Medicine (IOM). Best care at lower cost: the path to continuously learning health care in America. Washington, DC: Institute of Medicine; 2013.
- Foley TJ, Vale L. What role for learning health systems in quality improvement within healthcare providers? Learn Health Sys. 2017; 1:e10025.
- Etheredge LM. Rapid learning: a breakthrough agenda. Health Affairs. 2014;33(7):1155–1162.
- Stuart G, Triola M. Enhancing health professions education through technology: building a continuously learning health system. Proceedings of a conference recommendations; 2015 April 9–12; Arlington, VA: The Josiah Macy Jr.Foundation;2015.
- Nix M, McNamara P, Genevero J, et al. Learning collaboratives: insights and a new taxonomy from AHRQ’s two decades of experience. Health Affairs. 2018;37(2):205–212.
- University GW. One GWU: aligning under one umbrella. Available from: https://smhs.gwu.edu/news/one-gw-aligning-under-one-umbrella.
- Friedman CP, Allee NJ, Delaney BC, et al. The science of learning health systems: foundations for a new journal. Learn Health Syst. 2017;1(1):e10020–n/a.
- Friedman CP, Rubin JC, Sullivan KJ. Toward an information infrastructure for global health improvement. Yearb Med Inform. 2017;26(1):16–23.
- Friedman CP, Rubin J, Brown J, et al. Toward a science of learning systems: a research agenda for the high-functioning learning health system. J Am Med Inf Assoc. 2015;22(1):43–50. .
- Nelson EC, Dixon-Woods M, Batalden PB, et al. Patient focused registries can improve health, care, and science. BMJ. 2016;354:i3319.
- Maracine V, Scarlat E. Dynamic knowledge and healthcare knowledge ecosystems electronic. J Knowl Manag. 2009;7:99–110.
- Forrest CB, Chesley FD, Tregear ML, et al. Development of the learning health system researcher core competencies. Health Serv Res. 2017;53(4):2615–2632.
- Funnell SC, Rogers PJ. Purposeful program theory: effective use of theories of change and logic models. San Francisco CA: Jossey-Bass; 2011.