ABSTRACT
Background
Medical curricula are constantly evolving in response to the needs of society, accrediting bodies and developments in education and technology. The integration of blended learning modalities has challenged traditional methods of teaching, offering new prospects in the delivery of medical education. The purpose of this review is to explore how medical students adapt their learning behaviours in a Blended Learning environment to become more independent and self-regulated, in addition to highlighting potential avenues to enhance the curriculum and support student learning.
Methods
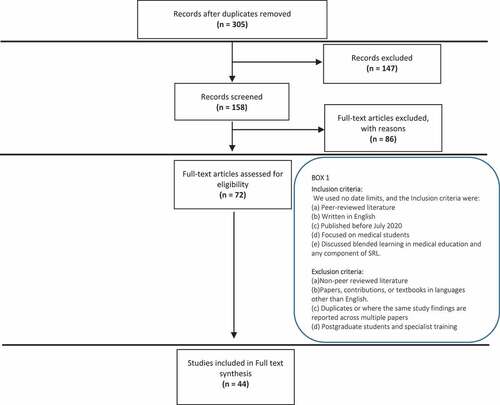
Using the approach described by Levac et al. (2010), which builds on Arksey and O’Malley’s framework, we conducted a literature search of the following databases: MEDLINE (Ovid), ERIC, EBSCO, SCOPUS and Google Scholar, utilising key terms and variants of “medical student’, ‘self-regulated learning’ and ‘blended learning’. The search yielded 305 studies which were further charted and screened according to the Joanna Briggs Institute.
Results
Forty-four studies were identified and selected for inclusion in this review. After full analysis of these studies, underpinned by Self-regulation theory, five major concepts associated with students’ learning behaviours in a Blended Learning environment were identified: Scaffolding of instructional guidance may support self-regulated learning; Self-regulated learning enhances academic performance; Self-regulated Learning improves study habits through resource selection; Blended learning drives student motivation and autonomy; and the Cognitive apprenticeship approach supports Self-regulated learning.
Conclusion
This review uncovers medical students’ learning behaviours within a Blended learning environment which is important to consider for curricular adaptations and student support.
Introduction
Medical educators continue to find more inventive and effective ways in delivering the curriculum to medical students. The delivery methods used within medical education significantly affect how students learn [Citation1]. Although the traditional didactic lecture is still the predominant instructional method used by medical schools, it has been repeatedly criticized for being an inflexible and an ineffective way of learning that lacks student-centredness [Citation2,Citation3]. Blended learning involves the combination of traditional and online teaching methods to encourage a more flexible and student-centred approach to learning. Blended learning facilitates self-regulated learning and, promotes a deeper understanding of concepts, critical thinking and application of knowledge, therefore supporting a development of a fundamental learning and clinical reasoning skills [Citation4,Citation5].
Self-Regulated Learning (SRL) theory is useful in highlighting the strategies and barriers students experience during their interaction with various modes of delivery. SRL involves four main elements planning, learning, self-assessment, and monitoring. Zimmerman defines learners as ‘self-regulating’ when they are ‘metacognitively, motivationally, and behaviourally active participants in their own learning process’ [Citation6]. SRL is a skill that students learn and is not inherently acquired i.e., can be learnt – and therefore taught [Citation7]. Through guidance by the teaching faculty, a learner may be able to construct an effective Self-regulated Learning environment, a skill that is vital for continuing professional development and lifelong learning.
In a blended learning environment, a significant proportion of learning occurs outside of educational institutions. This is because blended learning offers adaptable and flexible routines for students’ learning processes [Citation8], in contrast with the traditional learning settings where students are restricted in routine and set time schedules [Citation5]. However, it is critical that students are able to utilise the learning opportunities that blended learning offers by practicing independent and self-directed learning [Citation9]. For example, medical students are faced with an avalanche of resources either from within their educational institutions or externally and it is expected that students practice a level of autonomy in selecting the most appropriate resources beneficial to their learning [Citation10]. Additionally, the requirement to acquire adult learning skills and is influenced by three important non-cognitive factors: pacing (deadlines, adhering to a schedule etc.), meaningfulness, and motivation. Therefore, it is essential that medical students have intrinsic and extrinsic motivation and planning skills for effective learning [Citation11].
The objective of this study was to explore medical student learning behaviours, adaptations, and implementation of learning strategies in a blended learning environment using the lens of Self-Regulated Learning Theory. This insight will aid medical educators in identifying methods to enhance the curriculum and support student learning.
Methods
We conducted a systematic scoping review to map out key findings regarding how medical students learn and self-regulate their learning in a blended learning environment by employing the five stages described originally by Arksey and O’Malley (2005) and Levac et al. (2010): (i) Identifying the research questions; (ii) Identifying the relevant studies; (iii) Study selection; (iv) Charting the data, and (v) Collating, summarising and reporting results [Citation12–14].
Identifying the research questions
We sought to answer the following research questions:
What are the associations (if any) between Blended Learning and Self-Regulated Learning behaviours in medical students?
What Self-Regulated Learning strategies are used by medical students in a Blended Learning environment?
What Blended Learning approaches facilitate Self- Regulated Learning in medical students?
Identifying relevant studies
A literature search was carried out, with the help of a medical librarian, between June 2019 and October 2020 with no date/year limit, searching for the main concepts in the following databases: MEDLINE (Ovid), ERIC, EBSCO, SCOPUS and google scholar. The Boolean search query used for our database search encompassed ‘medical student’ and its alternative terms, combined with the term ‘self-regulated learning’ and the varied terms of ‘blended learning’ such as e-learning, online learning and technology enabled learning.
Study selection
illustrates the search and selection process implemented by the research team, as guided by the Joanna Briggs Institute [Citation14]. A total of 305 articles were initially identified and downloaded into EndNote®. Researchers IH, VM and RB screened article titles for abstract inclusion. Abstracts were then divided amongst the researchers IH, VM, BD and JM while RB independently screened all the abstracts (n = 158). RB met with each researcher individually to discuss their independent assessment of the abstracts to determine eligibility for full-text review against the inclusion criteria (: Box 1). This resulted in the identification of 72 articles that were reviewed fully by all researchers. Any discrepancies were discussed amongst all researchers until consensus. Finally, 44 papers were deemed to fulfil the criteria set to be included in this review.
Charting the data
A descriptive analysis approach was employed to the 44 articles identified from the selection process described in . Data was recorded in an Excel spreadsheet summarising characteristics of each article including year of publication, location of study, author, research objective, type of study, data collection methods, a summary of results and key messages.
Collating, summarising, and reporting results
The team assigned various descriptors to each full-text article that was reviewed, added to the to the Excel spreadsheet to be collated and coded by RB. RB and IH thematically analysed the findings, with reference to SRL theory, using an interpretive qualitative approach [Citation15] to address the research questions of this study. Codes were assigned and reassigned creating categories. These categories were continuously refined evolving into conceptual themes. RB conferred the resulting themes and links to SRL with the research team (IH, JM, VM and BD), until consensus was reached.
Results
Descriptive summary
Of the 44 articles that we identified and analysed, 40 were published between 2015–2020 with the majority published in 2015 (n = 31) followed by those published in 2019/2020 (n = 9). The remaining 4 articles were published between 2009 and 2014. Most of the articles were comparative studies (n = 24), followed by perspective papers (n = 9), mixed methods (n = 8) and three review papers, two of which were metanalyses and one scoping. Geographic distribution revealed primary studies were conducted in the USA (n = 16), Asia (n = 11), Europe (n = 9), Australia (n = 5), Canada (n = 2) and Brazil (n = 1).
Conceptual themes resulting from the interpretive qualitative analysis
From the 44 studies that were included in this review, we identified five conceptual themes that focused on the links between blended learning and medical student learning behaviours, in the context of SRL theory: (i) Scaffolding of instructional guidance may support self-regulated learning; (ii) Self-Regulated Learning enhances academic performance; (iii) Self-Regulated Learning improves study habits through resource selection; (iv) Blended Learning drives student motivation and autonomy; and (v) The Cognitive apprenticeship approach supports SRL. These conceptual themes are described in more detail below and are summarised in .
Table 1. Concepts identified from the literature that relate to medical students’ self-regulation of learning in a blended learning environment
(i) Scaffolding of instructional guidance may support self-regulated learning
Twelve studies reported on the advantages of the integration of scaffolds to support the SRL processes during medical students’ learning [Citation4,Citation16–26]. These studies collectively reported that enhancing students’ learning occurs through the modification and adjustment of their learning behaviour using various innovative blended teaching models and strategies, and regular feedback [Citation19,Citation23]. They depicted that insufficient direction and structure can disadvantage students in a blended learning classroom, especially when they are assigned extensive pre-class work [Citation27]. Students who lacked self-regulation were less likely to review the content prior to class, limiting their ability to actively participate in the learning activity. This in turn, caused the students to lose the opportunity to engage in interactive reflective experiences to enhance and deepen their learning capabilities. However, it was found that different cohorts adopted different SRL strategies depending on their phase of learning [Citation19,Citation25]. SRL strategies mostly used in the early stages of learning were planning and reflection, whereas the learning and monitoring phases were less frequent. This accounts for the varying levels of SRL skill development in medical students.
(ii) Self-regulated learning enhances academic performance
Fourteen articles presented the relationship of SRL enhancing academic performance, whilst also examining the students’ application of deep learning strategies and the integration of knowledge [Citation27–38]. Greater use of learning strategies, such as elaboration and critical thinking, was associated with students’ higher levels of performance in their exams [Citation28,Citation37]. Students adopting these learning strategies were more likely to progress and obtain better academic results than those who did not use these strategies [Citation32].
(iii) Self-regulated learning improves study habits through resource selection
The association between SRL and the ability to identify relevant resources was highlighted by 9 studies that were incorporated in this review [Citation25,Citation29,Citation37,Citation39–43]. Online resources, clinical videos, and interactive resources using mobile devices were among the most relevant resources identified for use by medical students. Online resources such as quizzes and white boards provided opportunities for learner collaboration and feedback and students found that formative learning, in the form of short quizzes was a valuable tool enabling reflection and enhancing their learning processes [Citation40]. These tools promoted their intrinsic motivation and goal-setting skills, especially when accompanied by teacher feedback. Additionally, participants using interactive resources were able to engage in more-adaptive decision-making behaviours and share their understandings when faced with rapidly evolving scenarios, more effectively than students using traditional resources [Citation37,Citation39]. This is also the case for researchers using hypermedia learning environments to promote and monitor SRL through learning tasks. The results confirmed that students benefited from the convenience of accessibility and more frequently accessed resources, including high-yield materials, via this medium [Citation39,Citation44].
(iv) Blended learning drives student motivation and autonomy
Eighteen studies compared the impact of different learning environments on students’ learning [Citation4,Citation16,Citation26,Citation27,Citation33–35,Citation40,Citation45–54]. Having a blended learning curriculum allowed medical students to practice their SRL skills early in their medical education which led to an increase in engagement, motivation, and proactivity to learn. These skills were also shown to be essential in students’ transition into clinical training and were more successfully developed in blended learning than in a didactic teaching environment [Citation48,Citation55]. For example, Problem-Based Learning in a blended environment allowed students to apply SRL skills earlier than students in a traditional curriculum, increasing the former’s retention of knowledge, motivation levels and overall drive to learn [Citation32].
(v) The cognitive apprenticeship approach supports SRL
The cognitive apprenticeship model encapsulated the significance of the students’ ability to learn a skill with the help of their educator [Citation45]. Most of the studies found blended learning to be a supportive environment to encourage apprenticeship through a strategy of effective modelling and continuous feedback [Citation17,Citation32,Citation35,Citation39,Citation56–60]. More successful students demonstrated an evolving interactive-transactive stance with their instructor, which actively strengthened their SRL skills, encouraged their participation and enhanced their professional identity development [Citation56–58]. The processing of knowledge in fast-paced environments promoted students to foster regulation strategies and to actively adopt new skills best suited to that setting. It was evident that students’ cognitive and metacognitive skills prospered in blended learning environments whether on campus or remotely.
The Full Analysis of the 44 Articles Is Available in the Supplementary Materials (Table S1) [Citation17].
Discussion
The rapid evolution of technology has led to innovative pedagogical approaches changing the landscape of medical education. Students are now required to acquire skills from beyond traditional settings, to be successful in the more prevalent blended learning environment. On initial examination, there was limited evidence in the literature for how self-regulation can be adapted in a Blended Learning environment. This limitation of the literature informed the basis of our systematic scoping review. In this study, we aimed to analytically review the current perspectives in the literature regarding how medical students control their learning in a blended learning setting to effectively promote self-regulation of learning. We also aimed to explore and identify strategies and learning behaviours that have been shown to be effective in supporting medical students’ learning needs in a blended setting.
Blended Learning creates a medium for developing SRL skills and can be highly beneficial in preparing medical students for their continuing education after graduation [Citation30,Citation55]. Blended learning can be quite effective if it encompasses structures that are purposely crafted to create an environment for active participation and interaction of learners. Scaffolding of instructional guidance throughout the activity has been shown to support effective interaction within the learning process [Citation45,Citation56]. Studies of flexibility in adaptive scaffolding encourage customised student support until the student can independently adopt the learning process [Citation23,Citation61]. In a blended environment, peer learning, and help-seeking behaviours can provide external structure and guidance, varying from goal setting, strategising, planning and the development of metacognition. This will in turn accommodate students to eventually adapt to the cyclical process of SRL. However, if students are left unguided, studies have illustrated the possibility for learning to decline, emphasising the impact of direct guidance and its correlation with an increase in determination, dedication and value of accomplishing an activity [Citation62,Citation63].
It has been shown that a positive correlation exists between SRL and academic performance, conveying that this deep learning approach encourages learners to make sense of their studies in an active manner by using their metacognitive capabilities to self-regulate their learning [Citation27,Citation40]. These SRL skills are also needed for effective future clinical practice, including ongoing professional development, strategies to keep up-to-date with new medical information, and source selection especially when referring to new medical research [Citation64]. Studies have reported that goal setting initiates the process of self-regulation and, consequently, results in higher performance for the activity at hand [Citation64,Citation65]. This skill is further refined through the application of tiered feedback at different stages of the process. Other studies have also acknowledged the importance of having educators trained in the application of SRL skills in a positive manner to further the academic performance of learners [Citation66,Citation67]. However, regardless of these developments, the evaluative measures for SRL of students in blended learning environments remains limited [Citation68]. Furthermore, most of the SRL measures were developed for traditional settings that are still used in an online environment, finding a substantial need to develop an evaluative measure that is specific for the current and/or advancing educational settings [Citation69].
Students conveyed that the blended classroom approach helped them to engage with content, promoted in-class participation and sustained motivation and autonomy. It was reported that medical students’ intrinsic motivation and autonomy, which are essential components of SRL, were facilitated by the BL environment, especially when clear student learning outcomes were incorporated into the learning activity [Citation25,Citation33]. Intrinsically motivated students inherit the belief of learning as challenging and rewarding at the same time. Studies have supported this finding by demonstrating that learners take initiative for their learning as they set the goals and evaluate the value of tasks to strategies [Citation40,Citation46].
The cognitive apprenticeship analogy is based on Bandura’s theory of modelling, describing the actions of humans functioning in a transaction between the self and society [Citation70]. Hence, this model involves the reciprocal relationship between individual (medical student) influences and environmental effects (Blended learning setting). Researchers have used this model to study the core processes of the self-regulation cycle i.e., forethought, performance and reflection as educators’ direct learners’ focus for the task at hand, leading to an increase in effort and determination [Citation63].
Conclusion
This scoping review has identified five concepts that emphasise the association between blended learning and SRL. It exhibits that SRL mechanisms of feedback positively enhanced the understanding of medical students’ learning and academic performance. This is particularly demonstrated in a blended learning environment when sufficient guidance is provided, driving the underlying motivation of the student to learn whilst regulating their behaviour in accordance with the educator’s feedback. Feedback allows the learner to consistently reflect and adjust their learning strategies in an active manner to reach their objective. It is important to understand medical students’ study habits and how this adapts in a blended learning environment. Consequently, appropriate changes can be made to the design and delivery of the medical curriculum to support the development of SRL and enhance students’ academic abilities and future performance as practitioners. These findings will help to inform the structure, design, delivery and feedback aspects of the medical curriculum but the principles can be applicable to other disciplines.
Limitations and future studies
The current study was constrained by the specific criteria focusing on English literature and undergraduate medical students, excluding those articles written in languages other than English, postgraduate medical students, and other health care professional education. Hence, a future focus may include expanding the scope to other disciplines, and to translate relevant non-English papers to obtain a broader insight on students’ learning behaviours in different educational settings with reference to geography and culture.
We recommend the development of an evaluative tool that measures students’ SRL strategies in a Blended Learning Setting [Citation69]. [Ballouk R, Mansour V, Dalziel B and Hegazi I]. Through this, medical educators can gauge how students learn and how they select and use resources to support their leaning in a blended learning environment. This would help identify potential avenues to enhance and enable medical educators to better support and guide their students.
Supplemental Material
Download MS Word (35 KB)Supplemental data
Supplemental data for this article can be accessed here
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006;81(3):207–8.
- Hoyo LM, Yang CY, Larson AR. Relationship of medical student lecture attendance with course, clerkship, and licensing exam scores. Med Sci Educator Internet. 2020 Sep;30(3):1123–1129.
- Tsang A, Harris DM. Faculty and second-year medical student perceptions of active learning in an integrated curriculum. Adv Physiol Educ. 2016;40(4):446–453.
- Klein M, Otto B, Fischer MR, et al. Fostering medical students’ clinical reasoning by learning from errors in clinical case vignettes: effects and conditions of additional prompting procedures to foster self-explanations. Adv Health Sci Educ Theory Pract. 2019;24(2):331–351.
- van Houten‐schat MA, Berkhout JJ, van Dijk N, et al. Self‐regulated learning in the clinical context: a systematic review. Med Educ. 2018;52(10):1008–1015.
- Zimmerman BJ, Schunk DH. Self-regulated learning and academic achievement: theoretical perspectives. New York: Routledge; 2001.
- Garcia T. The role of motivational strategies in self-regulated learning. New Directions Teach Learn. 1995;1995(63):29.
- Teunissen P, Scheele F, Scherpbier A, et al. How residents learn: qualitative evidence for the pivotal role of clinical activities. Med Educ. 2007;41(8):763–770.
- Ifenthaler D. Determining the effectiveness of prompts for self-regulated learning in problem-solving scenarios. J Educ TechnolSoc. 2012;15(1):38–52.
- Bransen D, Govaerts MJ, Sluijsmans DM, et al. Relationships between medical students’ co-regulatory network characteristics and self-regulated learning: a social network study. Perspect Med Educ. 2021;11(1):1–8.
- White CB, Gruppen LD, Fantone JC. Self-regulated learning in medical education. Understand Med Educat. 2013; 2:201–211.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):1–9.
- Peters MD, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–146.
- Elliott R, Timulak L. Descriptive and interpretive approaches to qualitative research. A handbook of research methods for clinical and health psychology. New York NY US: Oxford University Press; 2005. p. 147–159.
- Liebert CA, Mazer L, Bereknyei Merrell S, et al. Student perceptions of a simulation-based flipped classroom for the surgery clerkship: a mixed-methods study. Surgery. 2016;160(3):591–598.
- Steiner CM, Wesiak G, Moore A, et al. Cultural variations in E-learning – a case study on medical training. Int J E-Learn. 2017;16(1):81–98.
- Zheng B, Ward A, Stanulis R. Self-regulated learning in a competency-based and flipped learning environment: learning strategies across achievement levels and years. Med Educ Online. 2020;25(1):1686949.
- Venkatesh S, Rao YK, Nagaraja H, et al. Factors influencing medical students’ experiences and satisfaction with blended integrated e-learning. Med Princ Pract. 2020;29(4):396–402.
- Ramnanan CJ, Pound LD. Advances in medical education and practice: student perceptions of the flipped classroom. Adv Med Educ Pract. 2017;8:63–73.
- Gaupp R, Fabry G, Körner M. Self-regulated learning and critical reflection in an e-learning on patient safety for third-year medical students. Int J Med Educ. 2018;9:189–194.
- Abraham RR, Fisher M, Kamath A, et al. Exploring first-year undergraduate medical students’ self-directed learning readiness to physiology. Adv Physiol Educ. 2011;35(4):393–395.
- Chernikova O, Heitzmann N, Stadler M, et al. Simulation-based learning in higher education: a meta-analysis. Rev Educ Res. 2020;90(4):499–541.
- Zheng B, Zhang Y. Self-regulated learning: the effect on medical student learning outcomes in a flipped classroom environment. BMC Med Educ. 2020;20(1):1–7.
- Zhang XM, Yu JY, Yang Y, et al. A flipped classroom method based on a small private online course in physiology. Adv Physiol Educ. 2019;43(3):345–349.
- Kopp V, Stark R, Heitzmann N, et al. Self-regulated learning with case-based worked examples: effects of errors. Eval Res Educat. 2009;22(2–4):107–119.
- Wang X, Li J, Wang C. The effectiveness of flipped classroom on learning outcomes of medical statistics in a Chinese medical school. Biochem Mol Biol Educ. 2020;48(4):344–349.
- Boysen-Osborn M, Anderson CL, Navarro R, et al. Flipping the advanced cardiac life support classroom with team-based learning: comparison of cognitive testing performance for medical students at the University of California, Irvine, USA. J Educ Eval Health Prof. 2016;13:11.
- Ikram UZ, Essink-Bot ML, Suurmond J. How we developed an effective e-learning module for medical students on using professional interpreters. Med Teach. 2015;37(5):422–427.
- Lupi C, Ward-Peterson M, Chang W. Advancing non-directive pregnancy options counseling skills: a pilot study on the use of blended learning with an online module and simulation. Contraception. 2016;94(4):348–352.
- Morgan H, Marzano D, Lanham M, et al. Preparing medical students for obstetrics and gynecology milestone level one: a description of a pilot curriculum. Med Educ Online. 2014;19(1):25746.
- Papinczak T. Are deep strategic learners better suited to PBL? A preliminary study. Adv Health Sci Educ. 2009;14(3):337–353.
- Pizzimenti MA, Axelson RD. Assessing student engagement and self‐regulated learning in a medical gross anatomy course. Anat Sci Educ. 2015;8(2):104–110.
- Sagheb MM, Amini M, Saber M, et al. Teaching Evidence-Based Medicine (EBM) to undergraduate medical students through flipped classroom approach. Shiraz E-Med J. 2018;19(2):e57150.
- Shimizu I, Nakazawa H, Sato Y, et al. Does blended problem-based learning make Asian medical students active learners?: a prospective comparative study. BMC Med Educ. 2019;19(1):147.
- Song HS, Kalet AL, Plass JL. Assessing medical students’ self-regulation as aptitude in computer-based learning. Adv Health Sci Educ. 2011;16(1):97–107.
- Song HS, Kalet AL, Plass JL. Interplay of prior knowledge, self-regulation and motivation in complex multimedia learning environments. J Comput Assist Learn. 2016;32(1):31–50.
- van de Ridder JMM, McGaghie WC, Stokking KM, et al. Variables that affect the process and outcome of feedback, relevant for medical training: a meta-review. Med Educ. 2015;49(7):658–673.
- Fischer F, Grasel C, Mandl H. Fostering problem-oriented learning with auxiliary hypertext and graphical information. 2000.
- Kassab SE, Al-Shafei AI, Salem AH, et al. Relationships between the quality of blended learning experience, self-regulated learning, and academic achievement of medical students: a path analysis. Adv Med Educ Pract. 2015;6:27–34.
- Lajoie SP, Lu J. Supporting collaboration with technology: does shared cognition lead to co-regulation in medicine? Metacogn Learn. 2012;7(1):45–62.
- Jang HW, Kim K-J. Use of online clinical videos for clinical skills training for medical students: benefits and challenges. BMC Med Educ. 2014;14(1):1–6.
- Taylor JA, Shaw CM, Tan SA, et al. Are the kids alright? Review books and the internet as the most common study resources for the general surgery clerkship. Am J Surg. 2018;215(1):191–195.
- Kim K-J, Jang HW. Changes in medical students’ motivation and self-regulated learning: a preliminary study. Int J Med Educ. 2015;6:213.
- Williams C, Perlis S, Gaughan J, et al. Creation and implementation of a flipped jigsaw activity to stimulate interest in biochemistry among medical students. Biochem Mol Biol Educ. 2018;46(4):343–353.
- White CB. Smoothing out transitions: how pedagogy influences medical students’ achievement of self-regulated learning goals. Adv Health Sci Educ. 2007;12(3):279–297.
- Sajid MR, Laheji AF, Abothenain F, et al. Can blended learning and the flipped classroom improve student learning and satisfaction in Saudi Arabia? Int J Med Educ. 2016;7:281.
- Ruiz JG, Smith M, Rodriguez O, et al. An interactive e-learning tutorial for medical students on how to conduct the performance-oriented mobility assessment. Gerontol Geriatr Educ. 2007;28(1):51–60.
- Nilsson M, Fors U, Östergren J, et al. Why medical students choose to use or not to use a web-based electrocardiogram learning resource: mixed methods study. JMIR Med Educ. 2019;5(2):e12791.
- Micheal S, Marjadi B. Blended learning to teach gender in medical school. Clin Teach. 2018;15(3):208–213.
- Ilic D, Nordin RB, Glasziou P, et al. A randomised controlled trial of a blended learning education intervention for teaching evidence-based medicine. BMC Med Educ. 2015;15(1):1–10.
- Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med Educ. 2018;18(1):1–12.
- Gilliland KO. The flipped classroom and learning analytics in histology. Med Sci Educator. 2017;27(1):9–13.
- Bédard D, Lison C, Dalle D, et al. Problem-based and project-based learning in engineering and medicine: determinants of students’ engagement and persistance. Interdiscip J Prob Based Learn. 2012;6(2):8.
- Foerst NM, Klug J, Jöstl G, et al. Knowledge vs. action: discrepancies in university students’ knowledge about and self-reported use of self-regulated learning strategies. Front Psychol. 2017;8:1288.
- Demirören M, Turan S, Taşdelen Teker G. Determinants of self-regulated learning skills: the roles of tutors and students. Adv Physiol Educ. 2020;44(1):93–98.
- Evensen DH, Salisbury-Glennon JD, Glenn J. A qualitative study of six medical students in a problem-based curriculum: toward a situated model of self-regulation. J Educ Psychol. 2001;93(4):659.
- Lucieer SM, van der Geest JN, Elói-Santos SM, et al. The development of self-regulated learning during the pre-clinical stage of medical school: a comparison between a lecture-based and a problem-based curriculum. Adv Health Sci Educ. 2016;21(1):93–104.
- Papinczak T, Young L, Groves M, et al. Effects of a metacognitive intervention on students’ approaches to learning and self-efficacy in a first year medical course. Adv Health Sci Educ. 2008;13(2):213–232.
- Schauber SK, Hecht M, Nouns ZM, et al. The role of environmental and individual characteristics in the development of student achievement: a comparison between a traditional and a problem-based-learning curriculum. Adv Health Sci Educ. 2015;20(4):1033–1052.
- Azevedo R, Hadwin AF. Scaffolding self-regulated learning and metacognition–Implications for the design of computer-based scaffolds. Instructional science: Springer; 2005 Nov 1; 33(5-6):367–379.
- Pintrich PR. Multiple goals, multiple pathways: the role of goal orientation in learning and achievement. J Educ Psychol. 2000;92(3):544.
- Latham GP, Locke EA, Fassina NE. The high performance cycle: standing the test of time. Psychol Manag Individ Perf. 2002;201–228.
- Bougioukas KI, Bouras EC, Avgerinos KI, et al. How to keep up to date with medical information using web-based resources: a systematised review and narrative synthesis. Health Info Libr J. 2020;37(4):254–292.
- Sitzmann T, Ely K. A meta-analysis of self-regulated learning in work-related training and educational attainment: what we know and where we need to go. Psychol Bull. 2011;137:421–442.
- Lee D, Watson SL, Watson WR. Systematic literature review on self-regulated learning in massive open online courses. Aust J Educat Technol. 2019;35(1). DOI:10.14742/ajet.3749
- Garcia R, Falkner K, Vivian R. Systematic literature review: self-regulated learning strategies using e-learning tools for computer science. Comput Educ. 2018;123:150–163.
- Araka E, Maina E, Gitonga R, et al. Research trends in measurement and intervention tools for self-regulated learning for e-learning environments—systematic review (2008–2018). Res Pract Technol Enhanc Learn. 2020;15(1):1–21.
- Ballouk R, Mansour V, Dalziel B, and Hegazi I. The development and validation of a questionnaire to explore medical students’ learning in a blended learning environment. BMC medical education. 2022;22(1):1–9.
- Bandura A. Social cognitive theory of self-regulation. Organizational Beha Human Decis Processes. 1991;50(2):248–287.