Abstract
Introduction: Traumatic injury is the fourth leading cause of death in western countries and the leading cause of death in younger age. However, it is still unclear which groups of patients benefit most from advanced prehospital trauma care. A minimal amount is known about the effect of prehospital physician-based care on patients with specifically traumatic brain injury (TBI). The aim of this review is to assess the effect of physician-staffed Emergency Medical Services (EMS) on the outcome of patients with severe TBI.
Methods: Literature searches have been performed in the bibliographic databases of PubMed, EMBASE and The Cochrane Library. Data concerning (physician-staffed) prehospital care for patients with severe TBI were only included if the control group was based on non-physician-staffed EMS. Primarily the mortality rate and secondarily the neurological outcome were examined. Additionally, data concerning hypotension, hypoxia, length of stay (hospital and intensive care unit) and the number of required early neurosurgical interventions were taken into account.
Results: The overall mortality was decreased in three of the fourteen included studies after the implementation of a physician in the prehospital setting. One study found also a decrease in mortality only for patients with a Glasgow Coma Scale of 6–8. Strikingly, two other studies reported higher mortality, one for all the included patients and one for patients with GCS 10–12 only. Neurological outcome was improved in five studies after prehospital deployment of a physician. One study reported that more patients had a poor neurological outcome in the P-EMS group. Results of the remaining outcome measures differed widely.
Conclusion: The included literature did not show a clear beneficial effect of P-EMS in the prehospital management of patients with severe TBI. The available evidence showed contradictory results, suggesting more research should be performed in this field with focus on decreasing heterogeneity in the compared groups.
Introduction
Traumatic injury is the fourth leading cause of death in western countries and the leading cause of death in younger age (Citation1). Furthermore, more years of productive life are lost due to traumatic injury than to any other illnesses (Citation2). In most western countries the prehospital triage system starts with the deployment of paramedic-staffed ambulances to the scene of the accident. The paramedics are experienced in Prehospital Trauma Life Support (PHTLS) and have obtained additional ambulance training. In incidents where serious injury is expected, physician-based Emergency Medical Services (P-EMS) are additionally deployed to the scene of accident, either by helicopter or by car, to provide advanced medical care. The team consists in general of a pilot/driver, a paramedic and a specially trained physician. P-EMS rapidly delivers advanced trauma care in the out of hospital setting according to, but also beyond Advanced Trauma Life Support (ATLS) guidelines. Prehospital medical interventions performed by an EMS physician can differ between emergency care systems, but include in general rapid sequence intubation (RSI), advanced pain management, and invasive surgical interventions such as surgical airway and resuscitative thoracotomy.
Several studies have been performed recently, assessing the expected improvement after the deployment of a physician on the outcome of severely injured patients (Citation3). Yet, the effect of a physician in the prehospital setting for patients with severe traumatic brain injury (TBI) is not clear. The permanent damage of this type of injury creates an enormous burden for patients, their family and the society. Studies regarding this subject reported contradictory results, pointing out the indistinctness of the additional value of a physician on scene. The aim of this review is to assess the effect of physician-staffed EMS on the outcome of patients with severe TBI.
Methods
Search Strategy
A literature search was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)-statement (www.prisma-statement.org). The study was registered at the International Prospective Register of Systematic Reviews (PROSPERO) with number CRD42017070911. (http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017070911)
To identify all relevant publications, we performed systematic searches in the bibliographic databases PubMed, EMBASE and The Cochrane Library (via Wiley) from inception to June 22, 2018. Search terms included indexed terms from MeSH in PubMed and EMtree in EMBASE as well as free text terms. In the Cochrane library, only free text terms were used to increase the probability of finding relevant articles. Search terms expressing “severe traumatic brain injury” were used in combination with search terms comprising “physician assistance” and “emergency medical services.” The references of the identified articles were searched for relevant publications. Duplicate articles were excluded, together with non-English articles. The full search strategies can be found in Supplement 1.
Eligibility Criteria
All types of studies (randomized, prospective, retrospective, case-control) differentiating between the use of P-EMS and other forms of (nonphysician-staffed) EMS were included and analyzed for this review. Patients with a Glasgow Coma Scale (GCS) below nine or a head Abbreviated Injury Score (AIS) above three due to TBI were considered. To maximize the external validity of the results, there was no restriction in age or country.
Selection Process
Two reviewers (ZP and GG) independently screened all potentially relevant titles and abstracts for eligibility. The full text of the selected articles was obtained for further review. The two reviewers independently evaluated the methodological quality of the full text papers, as described in the “risk of bias” section shown in the following section. Differences in judgement were discussed until consensus was reached. Data concerning (physician-staffed) prehospital care for patients with severe TBI were only included if the control group was based on nonphysician-staffed EMS. To study the effects of the different emergency aids on the outcome of patients, primarily the (inhospital) mortality rate and secondarily the neurological outcome were examined. Since hypotension and hypoxia are considered as serious risk factors for secondary injury, the development of both factors at ED arrival was also evaluated (Citation4, Citation5). Additionally, data about the length of stay (hospital and ICU) and the number of required early neurosurgical interventions at ED arrival was taken into account.
Risk of Bias in Individual Studies
The quality assessment was conducted by one reviewer (ZP). The risk of bias of each study was determined using the Newcastle-Ottawa Quality Scale for cohort studies (Citation6). Each study was analyzed separately and a maximum of nine stars could be assigned when the study met all the requirements. For randomized controlled trials, The Cochrane’s Collaboration Tool was used for assessing the risk of bias (Citation7). The risk of bias was defined as “low” or “high” for different types of bias, including selection bias, detection bias, attrition bias and reporting bias. Since blinding of personnel and patients is not possible in this type of studies, the risk of performance bias could not be assessed. Furthermore, the level of evidence of each study was identified, based on the definition given by the Oxford Centre for Evidence-based Medicine (Citation8).
Summary Measures
The primary outcome was (in-hospital) mortality. Survival was concerned as inversely related to the mortality and therefore converted. Additionally, the neurological outcome was investigated, based on the Glasgow Outcome Score (GOS) or the Extended Glasgow Outcome Score (GOSE) (Citation9). The original GOS uses the following classification: (Citation1) death; (Citation2) persistent vegetative state; (Citation3) severe disability; (Citation4) moderate disability; (Citation5) good recovery. However, the scale is clinically often used in a converse way, considering 1 as “recovery” and 5 as “death” (Citation10). Therefore, explanatory texts will be included. For hypotension a systolic blood pressure (SBP) value below 90 mmHg is used and for hypoxia a saturation (SpO2) below 92% (Citation11). Other different, but comparable, scales will be defined in the corresponding tables. Statistical significance was considered at a p-value of less than 0.05.
Results
Study Selection
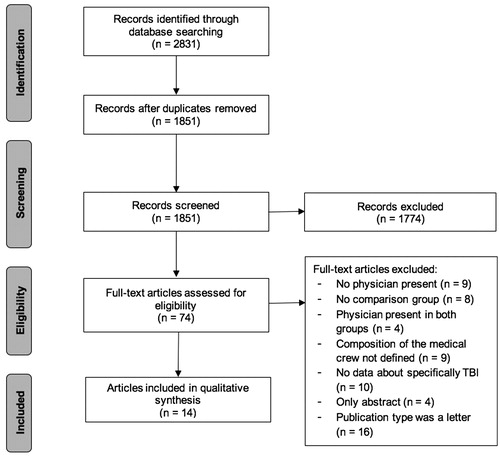
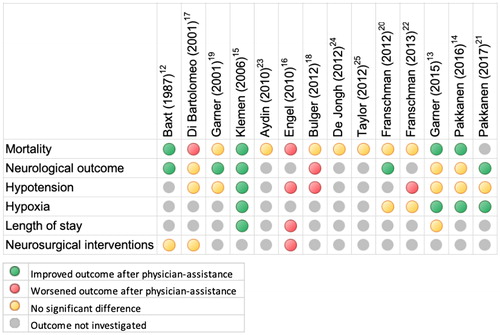
The literature search generated a total of 2,831 articles: 1,066 in PubMed, 1,533 in EMBASE and 232 in The Cochrane Library. After removing duplicates, 1,851 references remained for the initial screening and 74 left for a full text evaluation. Ultimately, a total of 14 studies met all the inclusion criteria and were included in this review. Studies were generally excluded for either the absence of a physician in the EMS or for the absence of data about patients with suspected TBI. Letters to the editor were screened and excluded afterward, since they did not include relevant information for this study. The flow chart of the search and selection process is presented in . Study characteristics can be found in . The investigated outcome measures of each study are summarized in and .
Table 1. Study characteristics
Table 2. Outcome measures
Mortality
Three of the 14 studies suggested a significant decrease in overall mortality after the prehospital implementation of a physician (Citation12–14). The study by Klemen and Grmec suggested a decrease of more than 50% in mortality as well, but only for patients with GCS 6–8 (p < 0.01) (Citation15). The study of Engel et al. with more than 10,000 patients presented contradictory results with more fatal outcomes in the group with P-EMS assistance (p < 0.001) (Citation16). Di Bartolomeo et al. showed results in favor of paramedic-staffed EMS as well, but also just for a subgroup of patients with GCS 10–12 (OR 1.54, 95% CI 1.12–2.12) (Citation17). Seven studies did not find any significant differences; one study did not investigate mortality.
Neurological Outcome
According to Bulger et al., more patients had a poor neurological outcome in the P-EMS group (p < 0.001) (Citation18). Five other studies found an improved GOS score after additional deployment of a physician (Citation12, Citation15, Citation19–21). Results from three remaining studies regarding the neurological outcome did not reach significance.
Hypotension
Engel et al. clearly indicated a higher proportion of hypotensive patients in the P-EMS group at hospital arrival (p < 0.05) (Citation16). According to Bulger et al. and Franschman et al., SBP rates at ED arrival were also significantly lower after P-EMS assistance, illustrating the severity of hypotension (p ≤ 0.03) (Citation18, Citation22). The results of Klemen and Grmec conflicted with those previously mentioned with higher SBP rates in the group with P-EMS (p = 0.03) (Citation15).
Hypoxia
The mean SpO2 quantified by Klemen and Grmec was at least 7% higher after the implementation of P-EMS (p = 0.04) (Citation15). Garner et al., Pakkanen et al., and Pakkanen et al. provided significant results as well, suggesting more adequate oxygen supply after additional assistance of a physician (Citation13, Citation14, Citation21).
Length of Stay
Three of the 14 studies investigated the length of stay in the hospital and the ICU after TBI, with conflicting results. Based on the results of Klemen and Grmec, physicians might shorten hospitalization times (p ≤ 0.04) (Citation15). According to Engel et al., however, it leads to a significant longer stay at both the hospital and the ICU (p < 0.0001) (Citation16). Garner et al. did not find significant results regarding the length of stay in the hospital (Citation13).
Neurosurgical Interventions
Engel et al. provided significant results, with almost 7% more craniotomies at the ED after the deployment of a physician on scene (Citation16). Baxt and Moody did not specify the type of neurosurgical interventions performed but did mention that there was no statistical difference between both groups (Citation12). Di Bartolomeo et al. quantified a higher number of patients requiring urgent neurosurgical interventions in the EMS group, not mentioning the significance level (Citation17).
Risk of Bias
Based on the Newcastle-Ottawa Scale, all the included cohort studies received a minimum of seven stars, indicating a relatively low risk on bias. Cochrane Collaboration’s Tool also indicated a low risk of bias for the included RCT. Details about the quality assessment are shown in .
Table 3. Quality assessment
Discussion
This review was performed to assess the additional value of a physician in the prehospital setting for patients with severe TBI. The included studies provided generous information about the effect of P-EMS on these patients. However, as we know, performing adequate research in the prehospital trauma setting is very difficult due to several factors. One of these factors is the difficulty in comparing different EMS systems. The wide variety in, for example, training, geographic locations, and medical tools makes it difficult to generalize internationally. For example, some EMS also includes advanced practical skills such as RSI and surgical interventions in their scope, which makes it possible to also provide ATLS as well. Additionally, in some countries, EMS are more advantageous regardless the presence of physicians, due to the integrated, more advanced equipment. For example, the presence of a helicopter can create substantial differences in prehospital times, especially in roughly shaped landscapes. Studies from different time periods (in this review from 1987 until 2015) are also subject to great differences in prehospital management with revised equipment and protocols (Citation12–25).
It is important to notice the heterogeneity in this category of patients in (e.g., age and comorbidity). Likewise, there are great differences in the group sizes of the several studies. For example, Klemen and Grmec included 64 patients in their study and presented results in favor of P-EMS (Citation15). The study of Engel et al., however, consisted of more than 10.000 patients from Germany and Australia, but they presented contradictory results (Citation16).
There seems to be an improved outcome after the implementation of a physician, but there might be an overestimation. Severe TBI cannot always be recognized as such by bystanders who called the emergency services in the first place. This might have resulted in the absence of P-EMS in cases where it should have been dispatched, with subsequent worse outcome owed to EMS. However, in contrast, physicians were probably more often deployed for the more serious accidents, with a higher risk on mortality in advance. Furthermore, the improved care in the field possibly led to the survival of sicker patients, who have then reached the ED. Both scenarios can be used to explain the remaining contradictory results, with subsequent worse outcomes now actually owed to P-EMS. Lastly, a lot of studies did not take the hypotension and hypoxia rate into account when evaluating the mortality, what might have had significant impact as well.
Despite an enhanced analysis of the articles, the included literature did not always provide the requested data completely. Additionally, the performed quality assessment might be as well a limitation of this review. The S4-section of the quality assessment indicated that the outcome of interest was not already present at the start of the study. For this analysis, “mortality” was used as the outcome of interest, but the neurologic outcome was a major outcome of interest as well. Since the neurologic state of the patients was not measured before the brain injury in the majority of the included studies, no accurate statements about the effect on neurologic functions can be made. Furthermore, the quality assessment suggested a great comparability between the studies, but still a meta-analysis was not possible due to the large number of missing variables and the wide range of different variables.
Nonetheless, most of the studies presented results in favor of P-EMS. Mortality rates decreased in the majority of the studies after additional assistance of a physician. Neurological outcome scores were often improved as well, suggesting better neurological outcome with a physician on scene. Additionally, tissue oxygenation seems to be maintained better by physicians, reducing the risk of secondary injury, again encouraging their deployment in addition to paramedics. In practice, we suggest low-threshold dispatch of P-EMS for patients suspected for severe traumatic brain injury, but adjustments for differences in injury severity or randomization are crucial for more accurate results. Additional analysis from the point of view of a related paramedic might create more insight as well.
Conclusion
Based on the results of this review of the literature, we can state that there seems not to be a clear beneficial effect of P-EMS in the prehospital management of patients with severe TBI. The available evidence showed contradictory results, suggesting more research should be performed in this field with focus on decreasing heterogeneity in the compared groups.
Supplemental Material
Download MS Word (14.2 KB)References
- Ramaiah R, Grabinsky A, Williamson K, Bhanankar SM. Trauma care today, what’s new? Int J Crit Illn Inj Sci. 2011;1(1):22–6.
- Organization WH, Cii F, Series I: guidelines for essential trauma care. Health Syst Transit. 2015;34(9):80.
- Galvagno S.M. J, Sikorski R, Hirshon JM, Floccare D, Stephens C, Beecher D, Thomas S. Helicopter emergency medical services for adults with major trauma. Cochrane Database Syst Rev. 2015;2015(12).
- Chi JH, Knudson MM, Vassar MJ, McCarthy MC, Shapiro MB, Mallet S, et al. Prehospital hypoxia affects outcome in patients with traumatic brain injury: a prospective multicenter study. J Trauma. 2006;61(5):1134–41.
- Spaite DW, Hu C, Bobrow BJ, Chikani V, Barnhart B, Gaither JB, et al. The effect of combined out-of-hospital hypotension and hypoxia on mortality in major traumatic brain injury. Ann Emerg Med. 2017;69(1):62–72. doi: 10.1016/j.annemergmed.2016.08.007.
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa Hosp Res Inst. doi: 10.2307/632432 (Epub ahead of print).
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343(7829):889–93.
- OCEBM Levels of Evidence Working Group; Durieux N, Pasleau F, Howick J. The oxford 2011 levels of evidence. Group. 2011;1:5653.
- Hudak AM, Caesar RR, Frol AB, Krueger K, Harper CR, Temkin NR, et al. Functional outcome scales in traumatic brain injury: a comparison of the Glasgow outcome scale (extended) and the functional status examination. J Neurotrauma. 2005;22(11):1319–26. doi: 10.1089/neu.2005.22.1319.
- Jennett B, Bond M. assessment of outcome after severe brain damage. A practical scale. Lancet. 1975;305(7905):480–4.
- ATLS Subcommittee. American College of Surgeons’ Committee on Trauma, International ATLS working group: Advanced trauma life support (ATLS®). J Trauma Acute Care Surg. 2013;74(5):1363–6.
- Baxt WG, Moody P. The impact of advanced prehospital emergency care on the mortality of severely brain-injured patients. The Journal of Trauma. 1987;27:365–9. doi: 10.1097/00005373-198704000-00004.
- Garner AA, Mann KP, Fearnside M, Poynter E, Gebski V. The head injury retrieval trial (HIRT): a single-centre randomised controlled trial of physician prehospital management of severe blunt head injury compared with management by paramedics only. Emerg Med J. 2015;32:869–75. doi: 10.1136/emermed-2014-204390.
- Pakkanen T, Virkkunen I, Kämäräinen A, Huhtala H, Silfvast T, Virta J, Randell T, Yli-Hankala A. Pre-hospital severe traumatic brain injury - comparison of outcome in paramedic versus physician staffed emergency medical services. Scand J Trauma Resusc Emerg Med. 2016;24(1):62.
- Klemen P, Grmec S. Effect of pre-hospital advanced life support with rapid sequence intubation on outcome of severe traumatic brain injury. Acta Anaesthesiol Scand. 2006;50(10):1250–4. doi: 10.1111/j.1399-6576.2006.01039.x.
- Engel DC, Mikocka-Walus A, Cameron PA, Maegele M. Pre-hospital and in-hospital parameters and outcomes in patients with traumatic brain injury: a comparison between German and Australian trauma registries. Injury. 2010;41(9):901–6.
- Di Bartolomeo S, Sanson G, Nardi G, Scian F, Michelutto V, Lattuada L. Effects of 2 patterns of prehospital care on the outcome of patients with severe head injury. Arch Surg. 2001;136(11):1293–300.
- Bulger EM, Guffey D, Guyette FX, MacDonald RD, Brasel K, Kerby JD, et al. Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. J Trauma Acute Care Surg. 2012;72(3):567–73; discussion 573–5; quiz 803.
- Garner A, Crooks J, Lee A, Bishop R: Efficacy of prehospital critical care teams for severe blunt head injury in the Australian setting. Injury. 2001;32(6):455–60.
- Franschman G, Verburg N, Brens-Heldens V, Andriessen TMJC, Naalt J Van Der, Peerdeman SM, et al. Effects of physician-based emergency medical service dispatch in severe traumatic brain injury on prehospital run time. Injury. 2012;43(11):1838–42. doi: 10.1016/j.injury.2012.05.020.
- Pakkanen T, Kämäräinen A, Huhtala H, Silfvast T, Nurmi J, Virkkunen I, Yli-Hankala A. Physician-staffed helicopter emergency medical service has a beneficial impact on the incidence of prehospital hypoxia and secured airways on patients with severe traumatic brain injury. Scand J Trauma Resusc Emerg Med. 2017;25(1).
- Franschman G, Andriessen TMJC, Boer C, Naalt J Van Der, Horn J, Haitsma I, Vos PE. Physician-based emergency medical service deployment characteristics in severe traumatic brain injury: A Dutch multicenter study. Injury. 2013;44(9):1232–6. doi: 10.1016/j.injury.2013.06.002.
- Aydin S, Overwater E, Saltzherr TP, Jin PHPFK, Exter P, van Ponsen KJ, Luitse JSK, Goslings JC. The association of mobile medical team involvement on on-scene times and mortality in trauma patients. J Trauma. 2010;69(3):589–594; discussion 594.
- Jongh MA de, Stel HF van, Schrijvers AJ, Leenen LP, Verhofstad MH. The effect of helicopter emergency medical services on trauma patient mortality in the Netherlands. Injury. 2012;43(9):1362–7. doi: 10.1016/j.injury.2012.01.009.
- Taylor C, Jan S, Curtis K, Tzannes A, Li Q, Palmer C, Dickson C, Myburgh J. The cost-effectiveness of physician staffed helicopter emergency medical service (HEMS) transport to a major trauma centre in NSW, Australia. Injury. 2012;43(11):1843–9. doi: 10.1016/j.injury.2012.07.184.