Abstract
Background
Chronic pain is a major and complex health condition associated with reduced work performance. A multimodal rehabilitation programme (MMRP) is a common intervention for chronic pain conditions, the goal being for the person to maintain or return to work.
Aim
To investigate the multivariate relationships between health-related quality of life, life interference, pain, physiological factors before MMRP and full-time sick leave 1 year after MMRP.
Material and Methods
Data were collected from the Swedish Quality Registry for Pain Rehabilitation. The study included 284 participants. Separate analyses were performed for women, men and three age groups.
Results
There were correlations between sick leave, physical functioning, pain duration, health-related quality of life, and self-assessed importance of work before MMRP and sick leave 1 year after MMRP. The patterns of factors associated with full-time sick leave varied for women, men and age groups.
Conclusions
These findings indicate that full-time sick leave for patients with chronic pain is affected by a number of interacting factors. Occupational therapy interventions aiming to develop activity skills in relation to work roles and enable patients to develop skills required to manage the physical, psychological and social demands to return to work or maintain work could be valuable to increase the possibility of attaining a sustainable work situation.
Introduction
Chronic pain is a major complex health condition with multifaceted origins, closely associated with reduced performance of work, less involvement in daily activities and decreased physical functions [Citation1,Citation2]. Chronic pain affects people of all ages and is a comorbid condition with psychosocial symptoms such as depression and anxiety [Citation3]. In addition, chronic pain is a major health problem because of its healthcare costs and human consequences [Citation4]. In a European survey, 19% of the population reported chronic pain and approximately 60% of those were less able or unable to work outside of the home and around one-fifth had lost their employment because of pain [Citation4]. In Sweden, chronic pain was reported by 18% of the population [Citation5]. Equally important, chronic pain is a common cause of sick leave [Citation6]. In the European survey, around 70% of persons with chronic pain were on sick leave [Citation4].
In Sweden, a mean yearly sick leave of 46 days has been reported for people with musculoskeletal diseases including chronic pain [Citation6]. The Swedish social insurance system makes it possible to be on part-time or full-time sick leave (25–75%) depending on the person’s work capacity [Citation7]. In addition, absence due to sick leave results in high costs for society and individual suffering [Citation4]. Previous research has described negative consequences of chronic pain such as decreased activity performance [Citation8] and engagement in meaningful occupations [Citation9]. Moreover, being engaged in meaningful activities, such as work, promotes overall well-being, including identity and self-worth, the satisfaction of contribution and the feeling of belonging [Citation10]. Having a job and being able to work is generally considered to be good for health and the overall well-being. In addition, work is central to individual identity, social roles and social status, and for physical and mental health [Citation11–13]. In contrast, absence from work leads to altered roles and negative changes in daily routines, habits and in participation in social activities [Citation14].
Since chronic pain conditions are associated with increased psychological distress, poor health and sick leave and high socioeconomic cost, a biopsychosocial approach has been adopted as the basis of clinical pain rehabilitation [Citation15]. Several studies have shown that a comprehensive multimodal rehabilitation programme (MMRP) that includes interdisciplinary pain management according to a biopsychosocial framework and considers different aspects of a patient’s life is more effective than unimodal or less complex interventions for patients with chronic pain [Citation16,Citation17]. There is supporting evidence for MMRP in the management of chronic pain in terms of decreased pain and reduced disability [Citation15]. MMRP is a team-based intervention that includes a number of different professions such as occupational therapist, physician, physiotherapist, psychologist and social worker [Citation15,Citation16].
One of the main goals of an MMRP is to reduce sick leave and improve the ability to return to or continue work [Citation16–20]. Today there is support for the efficacy of MMRPs for reducing days on sick leave. However, reduced sick leave and return to work is a multidimensional process which has been found to be related to a number of aspects and involves interaction between personal and social factors [Citation21].
Research has shown that a higher proportion of women than men are offered the opportunity to participate in an MMRP [Citation22] and women are also overrepresented in MMRPs [Citation23]. A possible explanation could be the somewhat higher prevalence of chronic pain among women [Citation24]. In addition, men are more likely to receive unimodal methods instead of MMRP [Citation22]. Despite these differences related to gender, the Swedish Agency for Health Technology Assessment and Assessment of Social Service concluded in a report in 2019 [Citation25] that there is still a lack of studies that investigate women and men separately, and that it is clinically important to investigate whether outcomes after MMRP are related to gender. More knowledge about MMRP and gender could provide important insights of relevance for the design of rehabilitation programmes and thereby increase the possibility of return to work.
In a previous study of persons with chronic pain, our findings showed that the outcome of MMRP (1-year follow-up) varied among age groups in terms of physical functioning, psychological factors and health-related quality of life [Citation26]. However, to our knowledge, very few studies have investigated sick leave patterns or return to work after MMRP in different age groups.
As described above, chronic pain is a multifaceted condition involving a number of factors. Therefore, in order to understand the complexity of chronic pain in relation to sick leave 1 year after MMRP, a multivariate analysis could be a valuable method to improve the understanding of correlating factors. Hence, the aim of this study was to investigate the multivariate relationships between health-related quality of life pain, life interference, psychological factors before MMRP and sick leave after 1 year, with a focus on gender and age.
Materials and methods
Design/settings
A longitudinal retrospective study design was used to investigate factors before MMRP that were related to full-time sick leave 1 year after MMRP. In this study, we used data collected from the Swedish Quality Registry for Pain Rehabilitation (SQRP) on patients referred to the Pain Rehabilitation Clinic, Umeå University Hospital, Sweden and the Department of Rehabilitation Medicine, Sunderby County Hospital, Sweden. The majority of patients had been referred to specialist care via a primary healthcare facility. The inclusion criteria for participation in MMRP according to the SQRP were: (i) disabling non-malignant musculoskeletal pain for >3 months, and (ii) age between 18 and 65 years. Exclusion criteria were: (i) ongoing major somatic or psychiatric disease such as heart disease, cancer, schizophrenia or deep depression, and (ii) substance abuse i.e. of alcohol, narcotics or medication.
The study was approved by the Regional Ethical Review Board in Umea, Medical Faculty of Umea University (Dnr 2015/240-31).
Participants/procedure
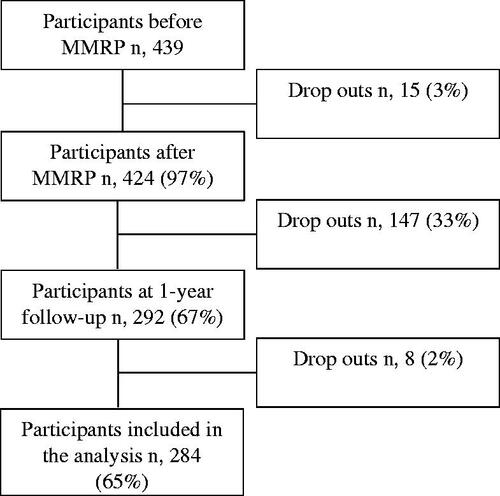
The participants completed the SQRP questionnaires three times: at the start of the rehabilitation programme, after participation in MMRP and 1 year after completed MMRP. The first and third questionnaires were distributed by post while the second was filled in at the clinic. One reminder was sent for the third questionnaire to participants who had not answered. The clinics included in the SQRP were obligated to follow written guidelines for the collection of data. Patients who had participated in MMRP and completed the SQRP questionnaire during the period 2011–2016 were included. A flow chart for the participants included in this study is provided in .
Before participation in MMRP, the patients were assessed by a multi-professional team. The assessment team consisted of an occupational therapist, physician, physiotherapist, psychologist and a social worker. Each professional interviewed and examined the patient individually. After the individual assessment, the results were discussed at a team conference. If the patient met the above-mentioned inclusion criteria for the programme, they were invited to participate in the MMRP. The patients who did not fulfil the inclusion criteria or who needed further investigation were returned to primary care with suggestions for interventions. During the MMRP, patients were encouraged to take an active role in goal setting and their rehabilitation plan. The majority of the interventions were well-coordinated, conducted in group sessions and based on cognitive-behavioural principles, described in detail in a previous study [Citation26]. The scope of the programme was approximately 6 h/day, 4–5 days a week, for 4–5 weeks. The interventions included in the MMRP were in line with the recommendations regarding MMRP in specialist care in Sweden e.g. physical exercise, body awareness training, activity training, ergonomic practice, occupational strategies and information about bodily and psychosocial reactions to chronic pain [Citation27]. No specific workplace intervention was routinely included apart from discussions and planning of workplace adaptations with the team members. As mentioned above, a main goal of MMRP is to reduce sick leave and improve the ability to return to work or maintain work. The general goals for the programme were broad and multifactorial and were focussed on coping strategies to help the patients increase their participation in society, return to work or study and lead an active and meaningful everyday life. These goals were combined with the patients’ individual goals [Citation28].
Most of the participants were themselves responsible for initiating changes at their workplaces and contacting their employers. In Sweden, employers have a work rehabilitation responsibility that includes adapting the workplace to the employee’s limitations and many employers collaborate with occupational healthcare regarding their rehabilitation responsibilities [Citation7]. For unemployed patients or patients who may not return to their previous work, the Swedish Public Employment Service assesses the patient’s work ability and helps the patient find a new job [Citation29].
Instruments
SQRP questionnaires were used to gather data on background information, pain characteristics, work importance, belief about recovery, and degree of sick leave. The instruments used were: EuroQol 5 D-3L(EQ5D) [Citation30], Hospital Anxiety and Depression Scale (HADS) [Citation31], Multidimensional Pain Inventory (MPI) [Citation32], Numeric Pain Rating Scale (NPRS) [Citation4] and Short Form Health Survey (SF-36) [Citation33]. For detailed information on the questionnaires and instruments used in this study, see .
Table 1. Variables and instruments in this study.
Data analysis
An exploratory analysis was applied to detect associations between data before MMRP and full-time sick leave 1 year after MMRP. Software IBM SPSS 26.0 and SIMCA 16. (Umetrics Inc., Umeå, Sweden) were used for all statistics. On the whole, non-parametric statistics were used but for age, number of pain sites and days with pain parametric statistics were used. To compare women and men, and the participants’ characteristics, X2, Mann–Whitney and Student t-test were performed. Comparisons between age groups were made by using X2, Kruskal Wallis and one-way ANOVA (with a post hoc test if there were significant differences). A 95% significance level was used for all tests. Missing data were not replaced for the descriptive statistics.
Multivariate data analysis
To gather and evaluate multi-dimensional data, we used multivariate statistics. Multivariate statistics can be described as a group of tools for reducing the dimensionality of large datasets to render the visualisation and interpretation more manageable. With multivariate analysis, simultaneous patterns and relations between several variables can be found, and the way variables co-vary with each other are displayed [Citation34,Citation35].
To identify which variables were of significance for full-time sick leave 1 year after MMRP, an Orthogonal Partial Least Square analysis (OPLS) was performed in SIMCA (Umetrics Inc., Umeå, Sweden). This technique does not require normal distributions of the included variables and can handle several variables. To explain the variance in the data, OPLS reduced the variables and found relations among them and transformed the variables into new uncorrelated components, known as principal components (PC), for both X variables (all variables before MMRP, see ) and Y variables (full-time sick leave 1 year after MMRP). The PC represented the maximum variance direction in the data. Each observation got a score value for X variables and for the Y variable (the distance from origin to the projected point). A cross-validation technique was used to identify non-trivial components. Included variables were assigned a loading for each of the extracted components. The loadings corresponded to which variables were dominant and how the variables were correlated to each other. The loadings of each variable were scaled as a correlation coefficient, thus standardising the range from −1 to +1. Variables close to 1 or −1 were the most important while a value close to zero had no influence on the model. Loadings with the same sign were positively correlated while those with opposite signs were negatively correlated. OPLS endeavoured to find relationships among the data before MMRP (input data) and full-time sick leave 1 year after MMRP (output data). This analysis provided a prediction model that explained which variables were of most significance for being on full-time sick leave 1 year after MMRP. Separate analyses were then performed for women, men and the three age groups.
In the model, R2 expresses the goodness of fit – the fraction of sum of squares of all the variables explained by PCs, while Q2 describes the goodness of prediction – the fraction of the total variation of the variables that can be predicted by a PC using cross validation methods [Citation35]. For each OPLS model, we reported R2Ycum and Q2).
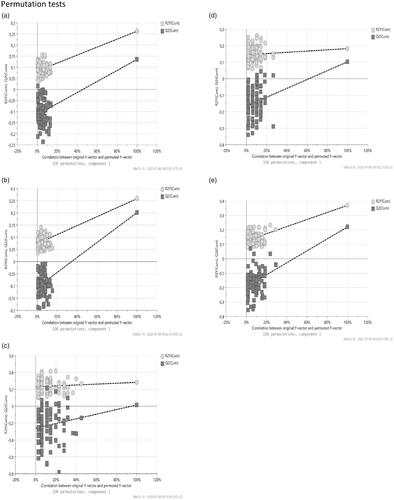
Permutation tests were used to check the validity of the models (). For each regression, we reported R2 and Q2. A permutation test compared the goodness of fit (R2 and Q2) of the original model with the goodness of fit of several models based on data where the order of the Y observations had been randomly permuted (100 times), while X matrix had been intact.
Figure 2. The plot showed a validate plot (after 100 permutations) of the Orthogonal Partial Least Square regression model (OPLS) for the selected Y (full-time sick leave) for: (a) all participants; (b) women; (c) men; (d) age group 31–45 years and (e) age group 46–65 years. The horizontal axis showed the correlation between the permuted Y vectors and the original vector of the full-time sick leave. The original Y had the correlation 1.0 with itself and defined the high point of the horizontal axis. For validity, the values of R2 and Q2 for the original model on the right are higher than the permuted model to the left or the Q2 regression line intersects the vertical axis at or below zero.
All variables included in the OPLS were rescaled so higher values indicated more serious problems. The following variables were rescaled: all eight scales in SF-36, both scales in EQ-5D and Life control scale in MPI. Variance scaling and mean-centering were used to give the variables equal importance in the analysis [Citation35]. A principal component analysis (PCA) was carried out to detect whether there were any moderate or strong outliers among all the observations. For that analysis, Hotelling’s T2 and distance to model in X-space were used. No extreme outliers were identified. In addition, non-linear Iterative Partial Least Squares algorithms were used to handle missing data. This corresponds to a missing completely at random assumption. Furthermore, a jack-knife procedure was used for estimate standard errors for the loadings. Only variables with a 95% jack-knife confidence interval are shown in the figures.
Results
Participants’ characteristics
In total, 439 chronic pain patients, 83 men and 356 women, filled in the questionnaires before MMRP. The present study is based on the patients who answered the SQRP questions (n = 284) (65%) () about sick leave both at baseline and at 1-year follow-up after MMRP. For details of the participants’ characteristics, see and for sick leave, see . The participants who did not answer the questions about sick leave at 1-year follow-up (n = 155) were younger (p ≤ 0.001), had lower scores on anxiety (p = 0.023), higher affective distress (p = 0.021), less role-emotional function (p = 0.011) and worse mental health (p = 0.003) than the participants who answered the questions.
Table 2. Participants’ characteristics.
Table 3. Sick leave before and one year after MMRP .
The women and men included in this study gave similar responses regarding background variables, but a few significant differences were found. A higher percentage of women had university education, a higher number of pain sites and better health-related quality of life (EQ-5D index) compared with men. In addition, men reported longer pain duration and higher life interference compared with women ().
A comparison of baseline data between the three age groups showed significant differences in terms of employment, work importance, physical functioning, number of pain sites, pain duration, anxiety, affective distress and mental health (). In addition, there were also differences between the age groups regarding the proportions of patients that were not on sick leave ().
The participants in the 18–30 years age group reported significantly lower duration of pain than the other age groups, 31–45 years (p = 0.010) and 46–65 years (p ≤ 0.001). In addition, the youngest age group (18–30 years) reported significantly better physical functioning than the 46–65 years age group (p = 0.002). Furthermore, the 46–65 years age group showed significantly better mental health than the 31–45 years age group (p ≤ 0.001).
Explaining variables related to sick leave
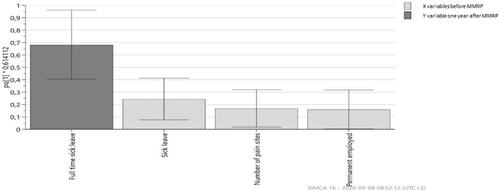
The OPLS analysis showed that the most important variables (loadings ≥ 0.15) at baseline associated with full-time sick leave 1 year after MMRP were high degree of sick leave, low physical functioning, longer pain duration, low health-related quality of life (EQ-5D VAS and EQ-5D index) and low work importance (). The model explained 26% of the variance (R2Ycum) and the prediction value was 20% (Q2). Gender and psychological variables (anxiety, depression, role-emotional functioning, mental health) were not associated with full-time sick leave 1 year after MMRP.
Figure 3. Combined OPLS loading column plot for the predictive component in the model for full-time sick leave 1 year after MMRP with 95% jack-knife confident interval bars. Relationship between the X variables (loadings before MMRP, light grey) and the loading for the Y variable (full-time sick leave 1 year after MMRP, dark grey). Only significant variables are shown in the model. In the figure, column height indicates the importance of each variable. Values closer to zero being less important irrespective of sign (±). Same sign for Y variable and X variable means they are positively correlated. High loadings of the Y variable indicate high correlation with the predictive component and X. Model variance R2Y =26% and prediction value Q = 20%.
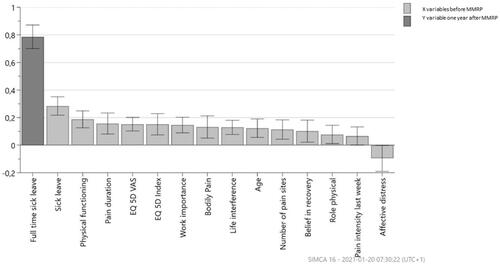
Women and men
The separate OPLS regressions model for women (R2Ycum = 26%, Q2 = 13%) () and men (R2Ycum = 28%, Q2 = 2%) () showed that degree of sick leave was of significance for both women and men for full-time sick leave 1 year after MMRP. The OPLS analysis for women showed that low physical functioning, low health-related quality of life (EQ-5D VAS) and low work importance and low affective distress were associated with full-time sick leave 1 year after MMRP (). The OPLS model for men showed that being unemployed and having a higher number of pain sites seemed to be associated with full-time sick leave 1 year after MMRP ().
Figure 4. Combined OPLS loading column plot for the predictive component in the model for full-time sick leave 1 year after MMRP with 95% jack knife confident interval bars for women. Relationship between the X variables (loadings before MMRP, light grey) and the loading for the Y variable (full-time sick leave 1 year after MMRP, dark grey). Only significant variables are shown in the model. In the figure, column height indicates the importance of each variable. Values closer to zero being less important irrespective of sign (±). Same sign for Y variable and X variable means they are positively correlated. High loadings of the Y variable indicate high correlation with the predictive component and X. Model variance R2Y = 26.3% and prediction value Q = 13.5%.
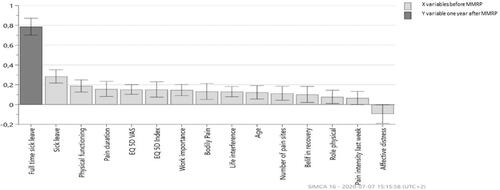
Figure 5. Combined OPLS loading column plot for the predictive component in the model for full-time sick leave 1 year after MMRP with 95% jack knife confident interval bars for men. Relationship between the X variables (loadings before MMRP, light grey) and the loading for the Y variable (full-time sick leave 1 year after MMRP, dark grey). Only significant variables are shown in the model. In the figure, column height indicates the importance of each variable. Values closer to zero being less important irrespective of sign (±). Same sign for Y variable and X variable means they are positively correlated. High loadings of the Y variable indicate high correlation with the predictive component and X. Model variance R2Y = 28% and prediction value Q = 2%.
Age groups
Three separate OPLS analyses were done for the age groups. Of these analyses, the 31–45 years age group (R2Ycum = 18, Q2 = 10%) () and the 46–65 years age group (R2Ycum =37, Q2 = 22%) () resulted in significant models. The analyses showed that different variables at baseline were important for sick leave in two of the age groups (31–45 years and 46–65 years) where the variables EQ-5D index and sick leave before MMRP turned out to be influential in both models.
Figure 6. Combined OPLS loading column plot for the predictive component in the model for full-time sick leave 1 year after MMRP with 95% jack-knife confident interval bars for age group 31–45 years. Relationship between the X variables (loadings before MMRP, (light grey) and the loading for the Y variable (full-time sick leave 1 year after MMRP, dark grey). Only significant variables are shown in the model. In the figure, column height indicates the importance of each variable. Values closer to zero being less important irrespective of sign (±). Same sign for Y variable and X variable means they are positively correlated. High loadings of the Y variable indicate high correlation with the predictive component and X. Model variance R2Y = 18.3% and prediction value Q = 10%.

Figure 7. Combined OPLS loading column plot for the predictive component in the model for full-time sick leave 1 year after MMRP with 95% jack-knife confident interval bars for the age group 46–65 years. Relationship between the X variables [loadings before MMRP, (light grey) and the loading for the Y variable (full-time sick leave 1 year after MMRP, dark grey)]. Only significant variables are shown in the model. In the figure, column height indicates the importance of each variable. Values closer to zero being less important irrespective of sign (±). Same sign for Y variable and X variable means they are positively correlated. High loadings of the Y variable indicate high correlation with the predictive component and X. Model variance R2Y = 37% and prediction value Q = 22%.
![Figure 7. Combined OPLS loading column plot for the predictive component in the model for full-time sick leave 1 year after MMRP with 95% jack-knife confident interval bars for the age group 46–65 years. Relationship between the X variables [loadings before MMRP, (light grey) and the loading for the Y variable (full-time sick leave 1 year after MMRP, dark grey)]. Only significant variables are shown in the model. In the figure, column height indicates the importance of each variable. Values closer to zero being less important irrespective of sign (±). Same sign for Y variable and X variable means they are positively correlated. High loadings of the Y variable indicate high correlation with the predictive component and X. Model variance R2Y = 37% and prediction value Q = 22%.](/cms/asset/214ba4ce-38ac-4ea9-b21d-8470e20ed513/iocc_a_1903990_f0007_b.jpg)
According to the OPLS regression model for the 31–45 years age group, it seems that the pain variables (bodily pain, pain severity and pain intensity during last week), sick leave, health-related quality of life (EQ-5D index and EQ-5D VAS), social functioning, physical functioning, life interference, vitality and depression (before MMRP) are all important variables of significance for predicting which people will be on full-time sick leave 1 year after MMRP (). Furthermore, the OPLS model for the 46–65 years age group showed that together with EQ-5D index and sick leave, other important variables that were associated with full-time sick leave 1 year after MMRP were unemployment, low work importance and no university education ().
Discussion
In this study, we investigated multivariate associations between pain, psychological factors, life interference, health-related quality of life before MMRP and sick leave 1 year after MMRP, with a focus on gender and age. The main results were:
The interplay of high level of sick leave, low physical functioning, long duration of pain, high life interference and low health-related quality of life before MMRP increased the risk of being on full-time sick leave after 1 year.
The relationship between factors that affected sick leave after 1 year showed different patterns in women and men. Low physical functioning, low self-assessed work importance, long duration of pain and low health-related quality of life were of most significance among women, while for men, a high number of pain sites and not being employed were seen to be the most crucial factors.
Health-related quality of life, pain, social functioning, life interference, vitality and physiological factors seemed to be of significance for being on full-time sick leave for the 31–45 years age group.
Work-related variables and health-related quality of life were found to be of importance for being on full-time sick leave for patients in the 46–65 years age group.
In this study, we found that patients on full-time sick leave 1 year after MMRP had a complex situation in terms of long duration of pain, high life interference, low psychological and social impact before MMRP. That indicated a connection between the complexity of pain consequences and full-time sick leave. The associations between pain, life interference as well as health-related quality of life in chronic pain confirm results from other studies [Citation2,Citation36]. Research has shown that high life interference includes disrupted family life, reduced work ability and limited social recreational activities [Citation32]. More specifically, our results indicate that life interference can have a negative effect on the ability to return to work or stay at work for people with chronic pain. Findings from previous research [Citation37,Citation38] have shown that reduced life interference after MMRP was associated with a lower risk of full-time sick leave 1 year after MMRP. In addition, high health-related quality of life [Citation39] and short duration of sick leave before MMRP have been found to be important factors for return to work 1 year after MMRP [Citation40].
Our results show that patients in a better state of health before MMRP were at a lower risk of being on full-time sick leave 1 year after MMRP. This is in line with previous studies that have shown that low pain intensity, high health-related quality of life and self-assessed low work importance and high level of education before MMRP are associated with decreased pain, improved psychological symptoms, increased activity and participation as well as positive effects on health-related quality of life 1 year after MMRP [Citation41].
Our findings that sick leave before MMRP was associated with full-time sick leave 1 year after MMRP are not surprising. This is consistent with results from previous studies showing that earlier sick leave [Citation42] and duration of sick leave increased the risk of prolonged sick leave [Citation40].
Several of the participants in our study had had pain for a long time before MMRP, and prolonged pain was found to be an important factor for being on full-time sick leave 1 year after MMRP. These results indicate the urgency to offer early interventions to persons with chronic pain in need of multimodal rehabilitation. These findings should be viewed in light of previous research which has presented links between long pain duration and less positive treatment outcomes regarding health-related quality of life [Citation43] as well as return to work, after multimodal pain rehabilitation [Citation44].
The separate analyses for women and men showed different patterns for which factors before MMRP were associated with sick leave 1 year after MMRP. However, the degree of sick leave was an important factor for both women and men. More specifically, the results showed that low physical functioning, low health-related quality of life, high life interference and long duration of pain before MMRP seemed to affect women more than men in relation to sick leave 1 year after MMRP. This is in line with previous research that has shown that health-related quality of life [Citation43] and physical disabilities [Citation45] can have an impact on the possibility of a successful return to work.
The model for men was significant but had a low predictive value. Still, the results indicate that the interplay of unemployment and a high number of pain sites before MMRP was associated with being on full-time sick leave 1 year after MMRP for men. Previous research has found that widespread pain causes the same worsening of health status for both men and women [Citation46] and is associated with long-term sick leave [Citation47]. Furthermore, results from a longitudinal follow-up study [Citation46] revealed that men recovered from widespread pain to a greater extent than women. More women than men participate in MMRP [Citation22,Citation36] and most of the studies on MMRP are based on a majority of women. The low number of men in research studies may have led to less knowledge about the outcomes of pain rehabilitation for men with chronic pain.
The results revealed that high age increased the risk of being on full-time sick leave 1 year after MMRP. This is in accordance with reviews [Citation21,Citation42,Citation44] that have shown that younger people with chronic pain were more likely to return to work compared with older people. In contrast, another review [Citation48] showed evidence that age is a prognostic factor for return to work. Truxillo et al found that factors, e.g. physical, cognitive, personality and motivational changes could have an impact on ageing at work [Citation49]. This may affect people’s ability to stay at work or return to work. Knowledge about ageing at work needs to be considered when designing interventions to support workers in different points across the life span [Citation49].
The separate analyses for the age groups showed different patterns for the factors before MMRP that affected sick leave 1 year after MMRP. The models for each age group in our study revealed that associated factors with full-time sick leave differ between the 31–45 years and the 46–65 years age groups. Furthermore, no significant model was found for the 18–30 years age group. The reason for this could be that there were few patients on full-time sick leave 1 year after MMRP in that age group.
We found that patients in the 31–45 years age group had a high risk of being on full-time sick leave 1 year after MMRP if they had low health-related quality of life, high pain, low social and physical functioning, low vitality, psychological factors and had sick leave before MMRP (). A reason for this could be that their life situations often lead to double burdens such as a stronger foothold on the labour market [Citation50] while at the same time establishing a family life with children, leading to an increased workload of housework during that phase of life [Citation51]. In addition, a previous study has shown that mood, stress and somatoform disorders have a peak in this age group [Citation50]. This together with pain might influence the ability to work. Furthermore, previous studies have found that both depression [Citation40,Citation44] and anxiety [Citation40] were negatively associated with return to work while low emotional distress and low physical disability were important factors for promoting staying at work despite pain [Citation45].
The analysis of the 46–65 years age group showed a pattern of interplay where work-related variables (i.e. unemployment, self-assessed low work importance) and no university education before MMRP were associated with full-time sick leave 1 year after MMRP. In general, having employment is considered to be important for a person’s identity and social status [Citation12,Citation52]. One explanation for our results could be that persons without university education often have physically demanding duties [Citation53,Citation54] and, less opportunity for adaptations or modified duties at the workplace [Citation53,Citation55]. Furthermore, it has been found in previous research that high education contributes to knowledge and understanding about health-related factors including healthier behaviours which supports people to take healthier decisions in their everyday lives, including working life [Citation56].
The focus of an MMRP is on improving or maintaining the ability to perform daily life chores including work. Return to work is a multidimensional process involving both personal and contextual factors which the individual is not always able to influence [Citation44,Citation57]. In addition, the whole compensation system in Sweden [Citation58], the possibility to receive occupational health care, and work-related factors [Citation44] have been found to be important factors for a successful return to work following long-term sick leave. Moreover, personal factors such as age, a positive attitude, self-efficacy and a high level of education affect the likelihood of reduced sick leave and return to work [Citation21].
Rehabilitation and support to return to work are essential interventions to avoid recurrent sick leave. There is evidence supporting the involvement of different professions in the interdisciplinary team in MMRP [Citation15]. Occupational therapists play an important role in the team since their unique competence regarding engagement in activities and adaptation in environment are of importance to support the patients achieve their goals in relation to health and wellbeing [Citation59,Citation60]. In addition, occupational therapists in MMRP enable patients to develop skills required to manage the physical, psychological and social demands needed to return to work or maintain work [Citation61]. Interventions from different actors need to be coordinated and implemented in order to achieve a sustained return to work [Citation62,Citation63]. Our findings indicate the importance of considering how factors related to the patient’s, state of health and factors related to work interact and affect the ability to return to work for patients with chronic pain 1 year after MMRP. Changes in any of these factors or modifying the interaction among them may either hinder or facilitate return to work. Thus, occupational therapy interventions and an occupational perspective which focuses on the patient’s whole life situation are of importance. In addition, the huge variety of symptoms for patients with chronic pain and different types of work means there must be a diverse range of interventions to promote return to work or reduce sick leave [Citation64].
Further research is needed to investigate other factors apart from sick leave for evaluating and studying short-term and long-term effects of MMRP, in relation to women and men as well as age groups. Furthermore, it is important to study the effect of MMRP for women, men and different age groups separately. Such knowledge can lead to the development of interventions provided in MMRP which could facilitate the possibilities to return to work or stay at work.
Methodological considerations
The multivariate statistics analysis with the use of OPLS statistics gave rise to correlated patterns, repeat measures and regression when there was an obvious risk for multicollinearity. Other common methods such as logistic regression and multiple linear regression can quantify the effect of individual factors but disregard interrelationships among different variables [Citation35].
Some limitations of this study should be noted. One limitation was that the patients were referred to specialist clinics and they represented severe cases of patients with chronic pain. These circumstances affect the ability to generalise our results to all persons with chronic pain. The MMRP interventions in this study did not focus solely on return to work. Instead, the implemented interventions aimed to improve the psychological and physical well-being of the patients, as well as their participation in daily life. These interventions have been shown to be important and to contribute to the long-term process of being able to return to work after a long period of absence from work because of chronic pain [Citation65].
The decision was taken to dichotomise the age groups (18–30, 31–45 and 46–65 years) [Citation66] was made with respect to the characteristics of each age group. The authors assumed that the 18–30 years age group, lived by themselves, were studying or were at the start of their working life [Citation11], while the 31–45 years age group had probably come further in their professional career and/or started a family [Citation50]. The oldest age group may have found their life role, with children starting to grow up and/or may have been at the end of their professional careers [Citation50,Citation66].
Conclusion
Our findings indicate that full-time sick leave for patients with chronic pain is affected by a number of interacting factors that differ among women and men and in different age groups. Occupational therapy interventions aiming to develop individual activity skills in relation to work roles and enable patients to develop skills required to manage the physical, psychological and social demands to return to work or maintain work, could be valuable to increase the possibility of attaining a sustainable work situation. Patients participating in MMRP may need different forms of support and tailored interventions in order to achieve reduced sick leave and increased return to work or maintain work despite their pain.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Linton SJ, Shaw WS. Impact of psychological factors in the experience of pain. Phys Ther. 2011;91(5):700–711.
- Andersen LN, Kohberg M, Juul-Kristensen B, et al. Psychosocial aspects of everyday life with chronic musculoskeletal pain: a systematic review. Scand J Pain. 2014;5(2):131–148.
- Milton MB, Börsbo B, Rovner G, et al. Is pain intensity really that important to assess in chronic pain patients? A study based on the Swedish Quality Registry for Pain Rehabilitation (SQRP). PLoS One. 2013;8(6):e65483.
- Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333.
- Harker J, Reid KJ, Bekkering GE, et al. Epidemiology of chronic pain in Denmark and Sweden. Pain Res Treat. 2012;2012:371248.
- Lidwall U. Sick leave diagnoses and return to work: a Swedish register study. Disabil Rehabil. 2015;37(5):396–410.
- Swedish Social Insurance Agency. Social Insurance in figures 2019, 2019. Available from: https://www.forsakringskassan.se/wps/wcm/connect/cec4cea8-1d6c-4895-b442-bc3b64735b09/socialforsakringen-i-siffror-2019-engelsk.pdf?MOD=AJPERES&CVID.
- Persson E, Lexell J, Rivano-Fischer M, et al. Everyday occupational problems perceived by participants in a pain rehabilitation programme. Scand J Occup Ther. 2013;20(4):306–314.
- Borell L, Asaba E, Rosenberg L, et al. Exploring experiences of “participation” among individuals living with chronic pain. Scand J Occup Ther. 2006;13(2):76–85.
- Steger MF, Dik BJ, Duffy RD. Measuring meaningful work: the work and meaning inventory (WAMI). J Career Assess. 2012;20(3):322–337.
- Waddell G, Burton AK. Is work good for your health and well-being? United Kingdom: The Stationery Office; 2006.
- Selenko E, Mäkikangas A, Stride CB. Does job insecurity threaten who you are? Introducing a social identity perspective to explain well-being and performance consequences of job insecurity. J Organiz Behav. 2017;38(6):856–875.
- de Vries HJ, Reneman MF, Groothoff JW, et al. Workers who stay at work despite chronic nonspecific musculoskeletal pain: do they differ from workers with sick leave? J Occup Rehabil. 2012;22(4):489–502.
- Johansson C, Isaksson G. Experiences of participation in occupations of women on long-term sick leave. Scand J Occup Ther. 2011;18(4):294–301.
- Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. BMJ. 2015;350:h444.
- Scascighini L, Toma V, Dober-Spielmann S, et al. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670–678.
- The Swedish Council on Health Technology Assessment (SBU) Rehabilitation for long-lasting pain. A litterature review. SBU-report 198 (In Swedish). Stockholm (Sweden). The Swedish Council on Health Technology Assessment (SBU); 2010.
- Norlund A, Ropponen A, Alexanderson K. Multidisciplinary interventions: review of studies of return to work after rehabilitation for low back pain. J Rehabil Med. 2009;41(3):115–121.
- Fischer MR, Persson EB, Stålnacke B-M, et al. Return to work after interdisciplinary pain rehabilitation: one-and two-year follow-up study based on the Swedish Quality Registry for Pain Rehabilitation. J Rehabil Med. 2019;51(4):281–289.
- The Swedish Council on Health Technology Assessment (SBU). Methods for treatments for long-lasting pain. A litterature review. SBU-report 177/1 (in Swedish). Stockholm (Sweden). The Swedish Council on Health Technology Assessment (SBU). 2006.
- Etuknwa A, Daniels K, Eib C. Sustainable return to work: a systematic review focusing on personal and social factors. J Occup Rehabil. 2019;29(4):679–700.
- Stålnacke B-M, Haukenes I, Lehti A, et al. Is there a gender bias in recommendations for further rehabilitation in primary care of patients with chronic pain after an interdisciplinary team assessment? J Rehabil Med. 2015;47(4):365–371.
- Gerdle B, Boersma K, Åsenlöf P, et al. Influences of sex, education, and country of birth on clinical presentations and overall outcomes of interdisciplinary pain rehabilitation in chronic pain patients: a cohort study from the Swedish Quality Registry for Pain Rehabilitation (SQRP). JCM. 2020;9(8):2374.
- Wijnhoven HA, de Vet HC, Picavet HSJ. Explaining sex differences in chronic musculoskeletal pain in a general population. Pain. 2006;124(1–-2):158–166.
- The Swedish Council on Health Technology Assessment (SBU). Treatment of Long-Term Pain States. Focusing on Women; SBU-report 301 (In swedish). Stockholm (Sweden). The Swedish Council on Health Technology Assessment (SBU); 2019.
- Spinord L, Kassberg A-C, Stenberg G, et al. Comparison of two multimodal pain rehabilitation programmes, in relation to sex and age. J Rehabil Med. 2018;50(7):619–628.
- The National Board of Health and Welfare. Swedish Association of Local Authorities and Regions, The Swedish Council on Health Technology Assessment. [Indication for multimodal rehabilitation in chronic pain.] Stockholm: Rapport 2011. 2 (in Swedish).
- Turk DC, Dworkin RH, Allen RR, et al. Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain. 2003;106(3):337–345.
- Swedish Public employment Service. Available from: https://www.government.se/government-policy/labour-market/.
- van Agt HM, Essink-Bot M-L, Krabbe PF, et al. Test-retest reliability of health state valuations collected with the EuroQol questionnaire. Soc Sci Med. 1994;39(11):1537–1544.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Kerns RD, Turk DC, Rudy TE. The west haven-yale multidimensional pain inventory (WHYMPI). Pain. 1985;23(4):345–356.
- Sullivan M, Karlsson J, Ware JJ. The Swedish SF-36 Health Survey – I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med. 1995;41(10):1349–1358.
- Henningsson M, Sundbom E, Armelius BÅ, et al. PLS model building: a multivariate approach to personality test data. Scand J Psychol. 2001;42(5):399–409.
- Eriksson L, Byrne T, Johansson E, et al. Multi-and megavariate data analysis basic principles and applications. 3rd rev. ed. Malmö: Umetrics Academy; 2013.
- Gerdle B, Akerblom S, Brodda Jansen G, et al. Who benefits from multimodal rehabilitation – an exploration of pain, psychological distress, and life impacts in over 35,000 chronic pain patients identified in the Swedish Quality Registry for Pain Rehabilitation. JPR. 2019;12:891–908.
- Nyberg VE, Novo M, Sjolund BH. Do Multidimensional Pain Inventory scale score changes indicate risk of receiving sick leave benefits 1 year after a pain rehabilitation programme? Disabil Rehabil. 2011;33(17-18):1548–1556.
- Merrick D, Sundelin G, Stalnacke BM. An observational study of two rehabilitation strategies for patients with chronic pain, focusing on sick leave at one-year follow-up. J Rehabil Med. 2013;45(10):1049–1057.
- Sviridova O, Gard G, Michaelson P. Predictors for return to work after multimodal rehabilitation in persons with persistent musculoskeletal pain. Edorium J Disabil Rehabil. 2018;4:100038D05SO2018.
- Brendbekken R, Vaktskjold A, Harris A, et al. Predictors of return-to-work in patients with chronic musculoskeletal pain: a randomized clinical trial. J Rehabil Med. 2018;50(2):193–199.
- Gerdle B, Molander P, Stenberg G, et al. Weak outcome predictors of multimodal rehabilitation at one-year follow-up in patients with chronic pain – a practice based evidence study from two SQRP centres. BMC Musculoskelet Disord. 2016;17(1):1–14.
- Cancelliere C, Donovan J, Stochkendahl MJ, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropr Man Therap. 2016;24(1):32.
- Vartiainen P, Heiskanen T, Sintonen H, et al. Health-related quality of life change in patients treated at a multidisciplinary pain clinic. Eur J Pain. 2019;23(7):1318–1328.
- Steenstra IA, Munhall C, Irvin E, et al. Systematic review of prognostic factors for return to work in workers with sub acute and chronic low back pain. J Occup Rehabil. 2017;27(3):369–381.
- de Vries HJ, Reneman MF, Groothoff JW, et al. Factors promoting staying at work in people with chronic nonspecific musculoskeletal pain: a systematic review. Disabil Rehabil. 2012;34(6):443–458.
- Sylwander C, Larsson I, Andersson M, et al. The impact of chronic widespread pain on health status and long-term health predictors: a general population cohort study. BMC Musculoskelet Disord. 2020;21(1):36.
- Mose S, Christiansen DH, Jensen JC, et al. Widespread pain – do pain intensity and care-seeking influence sickness absence? – A population-based cohort study. BMC Musculoskelet Disord. 2016;17:197.
- Verkerk K, Luijsterburg PA, Miedema HS, et al. Prognostic factors for recovery in chronic nonspecific low back pain: a systematic review. Phys Ther. 2012;92(9):1093–1108.
- Truxillo DM, Cadiz DM, Hammer LB. Supporting the aging workforce: a review and recommendations for workplace intervention research. Annu Rev Organ Psychol Organ Behav. 2015;2:351–381.
- Lidwall U, Bill S, Palmer E, et al. Mental disorder sick leave in Sweden: a population study. Work. 2018;59(2):259–272.
- Landstedt E, Harryson L, Hammarstrom A. Changing housework, changing health? A longitudinal analysis of how changes in housework are associated with functional somatic symptoms. Int J Circumpolar Health. 2016;75:31781.
- Olsson A, Erlandsson LK, Hakansson C. The occupation-based intervention REDO™-10: Long-term impact on work ability for women at risk for or on sick leave. Scand J Occup Ther. 2020;27(1):47–55.
- Ionescu AM, Cuza A. How does education affect labour market outcomes. Rev Appl Socio-Econ Res. 2012;4(2):130–144.
- Ballo JG. Labour market participation for young people with disabilities: the impact of gender and higher education. Work Employ Soc. 2020;34(2):336–355.
- Durand MJ, Coutu MF, Tremblay D, et al. Insights into the sustainable return to work of aging workers with a work disability: an interpretative description study. J Occup Rehabil. 2021;31(1):92–106.
- Piha K, Laaksonen M, Martikainen P, et al. Interrelationships between education, occupational class, income and sickness absence. Eur J Public Health. 2010;20(3):276–280.
- Lynöe N, Wessel M, Olsson D, et al. Respectful encounters and return to work: empirical study of long-term sick-listed patients' experiences of Swedish healthcare. BMJ Open. 2011;1(2):e000246–e000246.
- SOU 2014:74 Jämställdhet i socialförsäkringen? Forskningsrapport till Delegationen för jämställdhet i arbetslivet. Stockholm;2014.
- Townsend EA, Polatajko HJ. Advancing an occupational therapy vision for health, well-being, and justice through occupation. Ottawa (ON): CAOT Publications AC; 2007.
- Kielhofner G. Model of human occupation: Theory and application. 4th ed. Baltimore: Lippincott Williams & Wilkins; 2008.
- Hill W, Macartney M. The role of occupational therapy in enabling people with chronic pain to return to work or education. Anaesthesia Intens Care Med. 2019;20(8):443–445.
- Sturesson M, Edlund C, Fjellman-Wiklund A, et al. Work ability as obscure, complex and unique: views of Swedish occupational therapists and physicians. Work. 2013;45(1):117–128.
- Svanholm F, Liedberg GM, Lofgren M, et al. Factors of importance for return to work, experienced by patients with chronic pain that have completed a multimodal rehabilitation program – a focus group study. Disabil Rehabil. 2020;25:1–9.
- Stigmar K, Grahn B, Ekdahl C. Work ability-experiences and perceptions among physicians. Disabil Rehabil. 2010;32(21):1780–1789.
- Hellman T, Jensen I, Bergstrom G, et al. Returning to work – a long-term process reaching beyond the time frames of multimodal non-specific back pain rehabilitation. Disabil Rehabil. 2015;37(6):499–505.
- Levinson DJ. A conception of adult development. Am Psychol. 1986;41(1):3–13.