ABSTRACT
Purpose
The purpose of this study was to evaluate whether crystalloid or colloid solutions could adequately optimize the patient cardiac output and thus improving systemic and microcirculatory blood flow during major orthopedic surgery.
Methods
Eighty-two (ASA) I–III patients were included in this prospective single-center randomized, controlled clinical trial. They were randomized into groups treated with either intra-operative crystalloid (lactated ringer) or colloid (6% hydroxyethyl starch, HES 130/0.4). Demographic data, Hemodynamic variables, pCO2 gap, central venous oxygen saturation and lactate levels were recorded every hour during surgery and until discharge from the Post-Anesthesia Care Unit (PACU). Infused volumes of crystalloids and HES, number of infused PRBCS and estimated intraoperative blood loss were recorded blindly for all patients.
Results
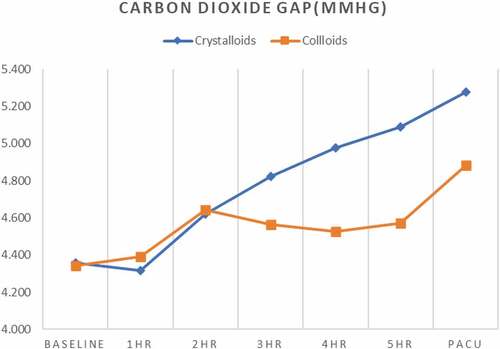
pCO2 gap was significantly lower in colloid group than crystalloid group toward the end of surgery and at PACU admission with values less than 5 mmHg while pCO2 gap was >5 mmHg at 5 hr and at PACU in the crystalloid group. In crystalloid vs colloid group, pCO2 gap was 4.97 vs 4.52 (P 0.023), 5.09 vs 4.057 (0.011) and 5.27 vs 4.88 (0.011) at 4 hr, 5 hr and at PACU respectively. At 5 hr patients received colloid had significantly lower mean pCO2 gap by 0.517 mmHg, average pCO2 gap among patients receiving crystalloid therapy was 5.09 mmHg and 4.57 mmHg in patients with colloids therapy.
Conclusion
Intraoperative fluid resuscitation using colloids is associated with more stable hemodynamics and better tissue perfusion as guided by lower pCO2 gap when compared to crystalloids.
KEYWORDS:
1. Background
Avoiding low tissue perfusion during major surgery resulting from insufficient systemic oxygen delivery has been shown to reduce organ failure and hospital stay [Citation1]. Early identification and adequate management of alarming notes of continuous improper tissue perfusion is of valuable concern especially in frail patients [Citation2]. Failure to cope with surgical trauma induced increase in oxygen demand either by an increase in O2 extraction or a decrease in O2 delivery can result in tissue hypoxia [Citation3]. Using multiple markers of inadequate tissue oxygenation have been used for early detection of complication in surgical patients [Citation4]. Traditionally, measuring the mixed or central venous oxygen saturation (Scv O2) is the most popular marker used to detect occult tissue hypo perfusion. A reduction in Scv O2 denotes that there is an elevation in systemic oxygen extraction and the presence of an insufficient systemic oxygen delivery [Citation5]. However, recent strong evidence showed that increasing central oxygen tension (PaO2) can significantly increase Scv O2 without improving systemic oxygen delivery [Citation6], and this may therefore limit the usefulness of using Scv O2 as a solo marker especially in the perioperative period [Citation7]. Moreover, an elevation of serum lactate which is commonly used as stable marker of tissue hypoxia may be delayed compared with other markers of impaired tissue oxygenation [Citation5] such as oxygen extraction, and therefore not suitable for early detection of tissue hypo perfusion [Citation8]. Recently, a novel marker of adequate tissue perfusion is central venous-to-arterial carbon dioxide gradient (pCO2 gap) as a useful alternative to detect improper flow state in spite of apparently adequate hemodynamic parameters [Citation9]. The pCO2 gap, which has been known to be inversely related to cardiac output (CO) is confirmed as a good reflection of the ability of the venous blood flow to wash out the accumulated CO2 produced in tissues [Citation10]. When applying modified FICK equation to CO2, the pCO2 gap is in linear relationship to CO2 production (VCO2) and inversely related to CO, in condition with proper oxygen extraction/delivered oxygen (VO2/DO2) relationship the flow is adequate enough to washout the CO2 produced by tissues even if there is extra anaerobic VCO2. On the other hand, in situation with inadequate blood flow, pCO2 gap may increase even without increase in VCO2 [Citation10]. Thus, if carbon dioxide production remains constant and as pCO2 gap would not be influenced by mechanical ventilation or minute ventilation, so low blood flow state with resultant impaired tissue perfusion is the main determinant of the elevation of the pCO2 gap [Citation11].
Despite the wide acceptance of perioperative normovolemia importance on avoiding the development of organ failure and death following high-risk surgeries, there is still ongoing debate about the proper type of fluid to be given perioperatively in major surgeries [Citation12]. Insufficiently and delayed maintaining of intravascular volume jeopardize hemodynamic parameters, micro vascular circulation and eventually organ dysfunction [Citation13]. Inadequate perioperative fluid therapy is an important cause of diminished O2 transport. It has been confirmed that perioperative deterioration in O2 transport is associated with organ failure and mortality [Citation14]. The kind of fluid namely crystalloid or colloid solution that adequately optimize the patient cardiac output and thus improving systemic and microcirculatory blood flow is still under intense research [Citation15].
The primary outcome of this study was to evaluate the effect two different fluids management during major orthopedic surgeries on pCO2 gap as a tissue perfusion global index. While the secondary outcome was to assess other intraoperative macro circulatory variables (mean arterial pressure, blood loss, O2 saturation, central venous pressure, and heart rate) and other tissue hypo perfusion markers (serum lactate and central venous oxygen saturation).
2. Patients and methods
This randomized, blinded, controlled, clinical trial was approved by the research ethics committee of Faculty of Medicine, Alexandria University and was registered in Pan African Clinical Trial Registry (PACTR 2,019,633,074,119). Written informed consent was obtained from all study participants. The study was conducted at EL Hadara university hospital, Alexandria during the period from first July 2019 to 31 April 2020. Eighty two patients were randomized into two study groups using computer-generated method to remove any selection bias.
Eligible patients scheduled for elective major orthopedic surgeries expected to last at least 4 hours were selected with the following inclusion criteria: American Society of Anesthesiologists (ASA) physical status grade I–III, an age between 40 and 70 years. Exclusion criteria of the patients were: overweight (BMI >35), left ventricular ejection fraction below 45%, significant cardiac arrhythmias, valvular lesions, coagulation disorders, perioperative renal insufficiency (serum creatinine > 2mmoll−1), impaired hepatic function (Aspartate aminotransferase >40 UL−1, Alanine aminotransferase > 40 UL−1), allergy to any drug used in this study, preoperative infection and pregnancy.
Patients were randomized either to colloid group that received hydroxyethyl starch (HES 130/0.4) and Voluven (Fresenius kabi, Germany) or crystalloid group that received lactated ringer (otsuka, Egypt) with 41 patients in each group. Group assignments were done after patient inclusion in the study before any anesthetic interference. A person not indulged in this study allocated the groups to the envelopes labeled with consecutive numbers. After observing the patient’s written consent. The research nurse opened the sealed envelopes in numerical order. Only the patients were blind to group allocation.
Upon arrival to the operating room (OR) an intravenous (IV) access was established, standard monitoring included electrocardiogram (ECG), pulse oximetry (SpO2), capnography, and noninvasive blood pressure (NIBP) were attached to all patients. Core temperature of the patient was measured via nasopharyngeal probe thermometer following induction of anesthesia. Operating room temperature was kept at 23–24°C. Patients received standard general anesthesia that included induction with propofol 1.5 to 2.0 mg/kg, fentanyl 2 to 3 mcg/kg and atracurium 0.5 mg/kg. Maintenance of anesthesia was achieved with isoflurane 1–1.5% and 60:40 oxygen mixed with air, according to decision of the attended anesthetist, additional doses of atracurium to maintain adequate relaxation and additional doses of fentanyl 0.5–1 mcg/kg titrated to maintain hemodynamic stability. Patients were ventilated with 8 ml kg−1 tidal volume in volume control mode to ensure stable ventilation (end-tidal CO2 kept within normal range) and high inspired O2 concentration (FIO2 was 60%) to maintain adequate oxygenation during the operative period. To insure normothermia, core temperature of the patients was kept around 36.5°C and 37°C by active warming with forced air blanket (Bair Hugger, USA) and warmed IV fluids. At the end of surgery, neuromuscular blockade was antagonized with neostigmine 0.05 mg/kg and 0.01 mg/kg of atropine. After induction of anesthesia and before start of surgery, all patients received arterial, central venous and Foley catheters insertion. A 20-gauge radial arterial catheter (Angiocath Becton Dickinson, Brazil) was inserted. Double lumen central venous (internal jugular or subclavian vein) catheter (Arrow international inc., USA) was positioned with the tip within the superior vena cava just above the right atrium. The position was confirmed by chest radiograph and readjusted if necessary. Simultaneous blood gas samples from venous and arterial catheters were collected at base line (before start of surgery) and every hour till discharge from PACU by well-trained nurses blinded to the investigation. Analysis of blood gas samples was done using blood gas machine (Radiometer ABL 700, Denmark).
The baseline values of HR and BP that trigger fluid bolus were taken immediately before induction of anesthesia. All patients received a baseline fluid therapy of 1 ml kg−1h−1 of crystalloids (lactated ringer solution) that started immediately after induction of anesthesia and continued till discharge from post anesthesia care unit (PACU). Additional fluid boluses of 250 ml of hydroxy ethyl starch (HES) (130/0.4) over 3–4 min was given to colloid group or 250 ml of lactated ringer solution over 3–4 minutes was given to crystalloid group according to changes in static variables only (Mean arterial pressure, heart rate, central venous pressure and urine output) that were measured during the operation till discharge from PACU.
Hemodynamic variables triggered fluid boluses were: urine output less than 0.5 ml kg-1 h-1, an increase in heart rate more than 20% above base line, a decrease in mean arterial blood pressure less than 20% below base line or central venous pressure minus the actual positive end expiratory pressure (peep) less than 20% of baseline. When mean arterial blood pressure was <60 mmHg in spite of sufficient intravascular volume (central venous pressure > 10 mmHg), norepinephrine infusion was added to keep mean arterial blood pressure > 60 mmHg. Packed red blood cells (PRBCs) was given when hemoglobin was < 8 g/dl-1. Fresh frozen plasma (FFP) was given when a PTT > 70 s. Scv O2, Pcv-aCO2 and lactate level were collected 10 minutes before surgery and hourly during surgery until discharge from the PACU and those parameters were not used to guide clinical management at any stage of the study as they were collected by nurses blinded to the investigation and recorded separately from the study. Infused volumes of crystalloids and HES, number of infused PRBCs and estimated intraoperative blood loss were also recorded.
After awaking from general anesthesia patients were transferred to post anesthesia care unit (PACU) and after fulfilling discharge criteria from (PACU), patients were transferred to their rooms. A standardized postoperative analgesic regimen, consisting of regular iv ketorolac 30 mg every 8 h . In the ward, well-trained nurses were asked to record pain level in each patient over the 10 cm visual analog scale (VAS) at postoperative 1,3,6,12,18 and 24 h during rest
Patient-controlled analgesia (PCA) device which delivered morphine as a 1-mg bolus, with a lockout time of 10 min was delivered to all patients. The PCA was continued postoperatively for 24 h. Patients with VAS score >4 at any point of time received 0.05 mg/kg IV bolus morphine.
3. Statistical analysis
Based on data in a recent research conducted by Laszlo et al. [Citation16], the mean carbon dioxide gap in the crystalloid group at 24 h postoperative was 7.3 ± 2.7 as compared to 5.8 ±2 among the colloid group with an effect size of 0.6 and at 5% level of significance considering a power of 80%, 82 patients were required with equal allocation ratio.
Statistical analysis was done using IBM SPSS statistics program version 21 [Citation17,Citation18]. Quantitative data were described by mean as a measure of central tendency and standard deviation as a measure of dispersion, while categorical variables were summarized by frequency and percent. Chi-square test was used to study significant association between two categorical variables. Fisher exact and Monte Carlo significance were used if more than 20% of total expected cell counts < 5 at 0.05 level of significance. Independent sample t test was used to detect significant difference in the mean quantitative variables between two treatment groups of patients based on normal distribution of variables by Kolmogorov Smirnov test and large sample size >30 per group. We conducted mixed design repeated measures ANOVA to study if statistically significant main effect of time, main effect of treatment whether crystalloids or colloids and if interaction is present in form of pattern change of continuous parameters along with different points of time between both two treatment groups. Adjusted post hoc-pairwise comparisons were employed by either Tukey’s or Bonferroni tests. Pearson’s correlation test was performed to detect significant linear association of different hemodynamic parameters with carbon dioxide gap. Then, we conducted multiple linear regression model using backward stepwise method to detect the independent contribution of therapy whether crystalloids or colloids as well as other parameters on carbon dioxide gap as the outcome variable. We included some hemodynamic parameters even when not significantly associated with the outcome by univariate analysis because there’s evidence from literature [Citation11] that they are influenced carbon dioxide gap. We tested the assumptions in terms of linearity by scatter plot; homoscedasticity and normality by residual plot, histogram, normal probability plot and independence of errors by Durbin-Watson test. We assessed the presence of outliers with influential cases by Standardized residuals and Cook’s distance >1 and no influential outliers were detected. We didn’t detect problems with multicollinearity as assessed by correlation matrix, VIF, tolerance and collinearity diagnostics. All statistical tests were done at 0.05 significance level.
4. Results
There were statistically insignificant differences between both groups as regards Age (p 0.669), BMI (p 0.964), Duration of operation (p 0.764) and Gender (p 0.641). As regards ASA status, insignificant difference existed between both groups in the proportion of patients classified as I, II, or III between groups taking colloids and crystalloids (p 0.849), (, ).
Table 1. Demographic Characteristics, fluid intake, type of surgery and ASA status fluid intake,type of surgery and ASA status fluid intake,type of surgery and ASA status of included participants in Crystalloids and Colloids groups.
demonstrates insignificant differences existed between both groups as regards changes in mean heart rate (MHR), mean central venous pressure (CVP), mean oxygen (O2) saturation and mean urine output (UO) along different periods of times (p > 0.05). As regards mean value of mean arterial pressure (MAP), except at 2 h intraoperative which in colloid group was significantly lower than crystalloid group. There were insignificant mean differences existed between both groups for the rest of the measurements. No statistically significant differences between both groups regards baseline infusion (p 0.927) and total blood loss (p 0.810).
Table 2. Comparison of different parameters between Crystalloids and Colloids groups
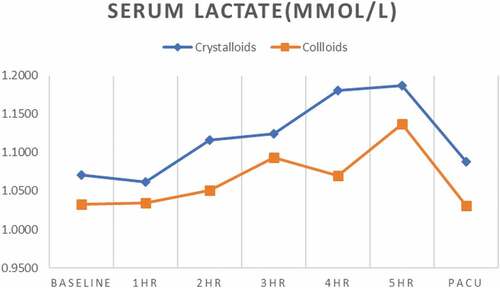
Mean serum lactate levels were significantly lower at 2 h (p0.005), 4 h(p <001), 5 h (p 0.017) and PACU (p 0.015) in colloid group than crystalloid group, while at baseline,1 h and 3 h, no significant differences existed between both groups (p > 0.05) (, ).
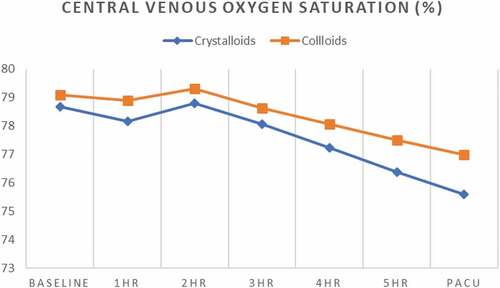
and reveals insignificant differences between both groups for mean central venous oxygen saturation (ScvO2) at baseline, and 1–4 h intraoperative (p > 0.05) while at 5 hours and PACU they were significantly higher in colloid group than crystalloid group (p 0.006) and (p 0.001), respectively.
Insignificant difference was existed between both groups for mean pCO2 gap at baseline, 1-, 2-, and 3-h intraoperative (p > 0.5), while, mean pCO2 gap was significantly lower in patients taking colloids than crystalloids at 4 h (0.023), 5 h (0.011) and at PACU (0.001), respectively, (, ).
We assessed if any MHR, MAP, CVP, O2 Saturation, amount of blood loss, serum lactate and ScvO2 correlate with carbon dioxide gap. () displayed insignificant association of any of these parameters with the pCO2 gap at 5 h intraoperative follow-up period (p > 0.05), ().
Table 3. Correlation of different parameters with Carbon Dioxide gap (ml) at 5 hours intraoperative
We performed multivariate linear regression analysis to assess the individual adjusted contribution of each included variable with pCO2 gap. As expected from univariate analysis that none of MHR, MAP, CVP, Blood loss and O2 saturation at 5 h intraoperative could significantly predict pCO2 gap, multivariate analysis proved the same insignificant association too (p > .05), the only significant predictor was mode of therapy. Patients received colloids had significantly lower mean Carbon dioxide gap by 0.517 mmHg. Thus, average pCO2 gap among patients receiving crystalloids therapy is 5.09 mmHg and 4.57 mmHg in patients with colloids therapy ().
Table 4. Linear regression model for prediction of Carbon Dioxide gap
5. Discussion
There is much concern about optimization of intraoperative hemodynamics that results in adequate tissue perfusion and oxygenation with subsequent better outcomes. Inadequate fluid therapy is a leading cause of diminished oxygen transport with subsequent organ failure and death. All surgical patients received IV fluids during perioperative period. The proper type of fluid to be selected for usage has not so far been selected.
This randomized clinical trial was conducted to evaluate the effect of crystalloid versus colloid fluid therapy during intraoperative period in lengthy orthopedic surgeries on pCO2 gap as a marker of global tissue perfusion. It was found that patients in crystalloid group significantly consumed more fluid than colloid group to achieve no differences between both groups as regards adequacy of macro circulatory hemodynamic parameters (MHR, mean CVP, mean O2 saturation, mean UO and mean value of MAP).
We used changes in static variables only (MAP, MHR, CVP and UO) to detect fluid status and hypervolemia during intraoperative period. Despite they were less accurate than advanced detailed hemodynamic monitoring; they were applied for both groups to decrease the error of being less valuable monitoring method. Our results provide further support to the original belief that during fluid therapy, less colloid is needed to get the same hemodynamic stability when compared to crystalloid [Citation18]. The superiority of colloid over crystalloid resulted from the difference of volumes of distribution between them, being extracellular space for crystalloid and plasma volume for colloid and this leads to colloid remains primary in the intravascular compartment whereas crystalloid shifts to interstitium several minutes from initial infusion [Citation19]. HES solution was used in our study as colloid while lactated ringer solution was the crystalloid used. HES is proved superior over lactated ringer because of its long-lasting intravascular half-life, augmented intravascular volume effect and its positive effect on tissue oxygenation [Citation20]. Moreover, stabilization of hemodynamics was statistically proven for HES solution [Citation21]. On the other hand, multicenter large randomized clinical trials reported no clinical benefits and even worse outcomes from using HES to optimize hemodynamics during perioperative period when compared with crystalloid [Citation22].
However, these results could be attributed to the general condition of the majority of cases included in these trials. They were critically ill patients and may suffer from damaged vascular endothelium and using colloid in this situation is associated with their redistribution into the interstitium with subsequent tissue edema and detrimental recovery [Citation23]. In our study, the situation is different as all our patients included in the trial were elective non critically ill with intact glycocalyx and adequate semipermeable function of the endothelium, so colloid could not escape into the interstitial space in large quantities [Citation24].
We must notify that during routine postoperative follow up we did not observe any influence of HES solutions used in our trial on renal function in both groups. Adequate urine output was maintained during perioperative period. Creatinine clearance was at the normal range in comparison to the preoperative value, and fractionated sodium clearance was slightly elevated from base line in colloid group. We used in this study modern, third generation of HES preparation (voluvin, 6%) with a low molecular weight (Mw) 130kD and low degree of substitution (DS) 0.4 which is considered to have excellent urinary excretion in moderate renal impairment patient. Moreover, in our trial, only patients with almost normal preoperative renal function were included and adequate volume support guided by static variables changes was maintained during perioperative period.
Since colloids provide more hemodynamic stability than crystalloids and this superiority also may be extended to microcirculatory perfusion [Citation20]. In this study, we tried to evaluate the effect of colloid vs crystalloid on microcirculatory perfusion. As many previous trials evaluations were mainly based on clinical experience of the anesthetists and other macro circulatory parameters such as MAP, UO, MHR and CVP. pCO2 gap could be used as a reliable tool for fluid resuscitation to evaluate the adequacy of tissue perfusion. pCO2 gap could be also used with other markers to diagnose inadequate fluid therapy [Citation9]. In our study ScvO2 at 5 hours and PACU were significantly higher in colloid group than crystalloid group, however, all values were above 70% in both groups during the study period. Elevation of serum lactate which is considered as a valuable marker of tissue perfusion is often of late onset compared to other tissue hypo perfusion markers as ScvO2 [Citation25]. Mean serum lactate levels also were significantly lower in colloid group than crystalloid group toward the end of surgery and at PACU admission and all values in both groups were less than 2 mmol/l on average during study period.
Tissue hypoxia is developed as a result of failure to cope with an increase in oxygen demand either by reduction in O2 delivery or elevation in O2 extraction [Citation26]. Tissue hypoxia could be existed with normal and even high values of ScvO2 (≥ 75%) in case of impaired O2 extraction which may therefore decrease the importance of ScvO2 measurement so, normal and even high ScvO2 measurements do not mean adequate microcirculatory flow. ScvO2 <70% is universally accepted as a landmark of inadequate systemic oxygen delivery with subsequent elevation in tissue oxygen extraction [Citation27]. In fact, our patients in both groups were in adequate compensated state as evidenced by stable hemodynamic parameters, little increase of serum lactate levels (< 2 mmol/l) and ScvO2 (≥70%) during the study period.
Cardiac output (CO) and pCO2 gap are inversely related to each other, pCO2 gap is taken as a landmark that reflect the capacity of venous blood flow to get rid of the CO2 excess produced in tissues [Citation28]. Deteriorated tissue perfusion during decreased blood flow is the main cause of increase pCO2 gap [Citation29]. Vallet et al. proved that pCO2 gap increased as a result to low blood flow-induced tissue hypoxia (ischemic hypoxia), on the other hand it did not change during hypoxemia-induced hypoxia (hypoxic hypoxia) [Citation29]. pCO2 gap can be applied as surrogate for CO adequacy and as tissue perfusion marker. It can be used successfully with other markers of tissue hypoxia especially in situation where oxygen diffusion capacity is impaired such as tissue edema and occluded blood flow that impair microcirculation, so it could be used as reliable marker of fluid resuscitation to evaluate tissue perfusion [Citation10]. pCO2 gap which was previously considered as a tissue perfusion global index could be proposed as a valuable rapid measurement of inadequate flow state despite adequate and normal microcirculatory parameters [Citation25]. In patients with low ScvO2, an elevation of pCO2 gap is reflecting a state of low CO and evaluation of pCO2 gap at this situation could be of value in integrating therapies that help improving CO. When ScvO2 (≥ 70%), persistent elevation of pCO2 gap is indication of impaired perfusion and in this way evaluation of pCO2 gap could help in choosing the ideal decisions regarding fluids and inotropes [Citation30,Citation31].
The main finding of our clinical trial was a significantly lower pCO2 gap in colloid group than crystalloid group toward the end of surgery and at PACU admission and with values less than 5 mmHg, while pCO2 gap >5 mmHg values were at 5 H and at PACU in the crystalloid group. Moreover, mean pCO2 gap significantly changed along with different points of time, particularly high from 2 h intraoperative till PACU than baseline with significant main effect of treatment whether Crystalloid or Colloid on pCO2 gap. It is evident from previous trials that normal pCO2 gap is less than 5 mmHg and pCO2 gap <5 mmHg had a high sensitivity (93%) and negative predictive value (74%) than pCO2 gap <6 mmHg in excluding occult tissue hypo perfusion [Citation32].
In our study elevation of pCO2 gap was gradual and exceeding the cutoff point of 5 mmHg toward the end of surgery in the crystalloid group with normal limits of both lactate and ScvO2 values, reflecting a state of impaired tissue perfusion notably in the crystalloid group.
Since there was no correlation between pCO2 gap and other intraoperative macro circulatory variables (MAP, blood loss, O2 saturation, CVP, and MHR) and other tissue hypo perfusion markers (serum lactate and ScvO2) as evidenced from linear regression model, we found that toward end of surgery the only significant predictor to changes in pCO2 gap was the type of fluid (colloid vs crystalloid) used in the current study. Patients received colloid solutions had significantly lower mean pCO2 gap when compared with patients received crystalloid solutions. Our results reported the efficacy of colloid over crystalloid as regards microcirculatory perfusion. To the best of our knowledge, this is the first study to evaluate the effect of intraoperative fluids regimen (colloid vs crystalloid) on pCO2 gap. These results give a more credit for colloids in the debate that existed since years between them as regards the best to use in the perioperative period.
These results could be attributed to the unique and better pharmacological characters of colloids. Inadequate fluid therapy is a leading cause of diminished oxygen transport with subsequent organ failure and death. Colloids are strongly expanding the intravascular volume with increase of CO with higher persistence result in better regional blood flow when compared to crystalloids [Citation33]. Moreover, colloids have better expansion of micro vascular volume with minimal leakage from capillaries associated with higher blood viscosity which result in adequate capillaries recruitment and micro vascular flow adjustment [Citation34]. More stability of hemodynamics with colloids is also believed to have a great influence on regional microcirculation [Citation35]. Last important aspect of enhancement of microcirculatory perfusion is the efficacy of colloids to enhance tissue oxygenation with subsequent improvement of cellular O2 utilization to avoid cellular hypoxia [Citation36]. Conversely, crystalloids are distributed within the entire extracellular space leaving the intravascular space and thus expanding the extravascular space with gradual accumulation of interstitial fluids and subsequent decrease of microcirculatory perfusion [Citation37]. The efficacy of colloid solution over crystalloid solution in the current study has been proved from different clinical trials.
Wu et al. [Citation38] found HES 6% and not normal saline restore intestinal microcirculation during hemorrhagic shock in a rodent model. Microcirculatory blood flow among various splanchnic organs, namely the kidney, liver, and intestine (mucosa, serosal muscular layer, and Peyer’s patch), and the gracilis muscle, were compared using laser speckle contrast imaging. Hiltebrand et al. [Citation39] agrees with the results of the present study, they reported that goal-directed colloid therapy markedly elevate microcirculatory blood flow of the small intestine after abdominal surgery in pig model when compared to crystalloid. microcirculatory blood flow was measured using laser Doppler flowmetry.
Dubin et al. [Citation40] also found that fluid management with 6% HES 130/0.4 is associated with higher capillary micro vascular flow index, percentage of perfused capillaries and perfused capillaries than normal saline to increase sublingual microcirculation in septic patients. The authors also found that less than half of the fluid volume was needed in colloid group when compared to crystalloid to achieve the target macro circulatory parameters. Our results contradict with the results of Wefa et al. [Citation41] they reported that HES solutions did not improve microcirculation when compared to crystalloids during fluid resuscitation in sepsis. Intravital microscopy of the mesenteric microcirculation (plasma extravasation; leukocyte–endothelial interactions) and arterial blood gas analysis were performed before and after fluid resuscitation, however, the point to be considered that it was an experimental sepsis model in rats with induced septic peritonitis.
6. Limitations
Our study has some limitations: it was a single center clinical trial with average sample size. Hemodynamic monitoring and intraoperative fluid management were guided by changes in static variables only and we could not use advanced detailed hemodynamic monitoring as they were not available. However, the changes were used for both groups and hence the variation were equal for both groups to decrease any defect in the accuracy of the measurements. Also the lack of postoperative measurements of these parameters could be considered as a limitation. Another limitation is the lack of correlation of pCO2 gap with incidence of post operative complications and.lack of correlation of carbon dioxide gap with incidence of post operative compilactions (AKI,Neurological deficit)
7. Conclusions
Based on this study it could be concluded that: in complex major orthopedic surgeries, fluid resuscitation using colloids (HES 130/0.4) is associated with more stable hemodynamics and better tissue perfusion as guided by lower pCO2 gap when compared to crystalloids.
Financial Disclosures
None
Trial registration
Pan African Clinical Trial Registry (PACTR 2,019,633,074,119)- 19 September 2019
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Bland RD, Shoemaker WC, Abraham E, et al. Hemodynamic and oxygen transport patterns in surviving and non-surviving postoperative patients. Crit Care Med. 1985;13(2):85–90.
- Gurgel ST, Do Nascimento P Jr. Maintaining tissue perfusion in high-risk surgical patients: a systematic review of randomized clinical trials. Anesth Analg. 2011;112(6):1384–1391.
- Vallet B, Futier E. Perioperative oxygen therapy and oxygen utilization. Curr Opin Crit Care. 2010;16(4):359–364.
- Pearse R, Dawson D, Fawcett J, et al. Changes in central venous saturation after major surgery, and association with outcome. Crit Care. 2005;9(6):R694–9.
- Donati A, Loggi S, Preiser JC, et al. Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk surgical patients. Chest. 2007;132(6):1817–18246.
- Litton E, Silbert BI, Ho KM, et al. Clinical predictors of a low central venous oxygen saturation after major surgery: a prospective prevalence study. Anaesth Intensive Care. 2015;43(1):59–65.
- Munoz-Price LS, Sands L, Lubarsky DA, et al. Effect of high perioperative oxygen supplementation on surgical site infections. Clin Infect Dis. 2013;57(10):1465–1472.
- Jansen TC, Van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182(6):752–761.
- Vallee F, Vallet B, Mathe O, et al. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock?. Intensive Care Med. 2008;34(12):2218–2225.
- Teboul JL, Mercat A, Lenique F, et al. Value of the venous-arterial PCO2 gradient to reflect the oxygen supply to demand in humans: effects of dobutamine. Crit Care Med. 1998;26(6):1007–1010.
- Vallet B, Teboul JL, Cain S, et al. Venoarterial CO2 difference during regional ischemic or hypoxic hypoxia. J Appl Physiol. 2000;89(4):1317–1321.
- Lopes MR, Oliveira MA, Pereira VO, et al. Goal-directed fluid management based on pulse pressure variation monitoring during high-risk surgery: a pilot randomized controlled trial. Crit Care. 2007;11(5):R100.
- Hoffmann JN, Vollmar B, Laschke MW, et al. Hydroxyethyl starch (130 kD), but not crystalloid volume support, improves microcirculation during normotensive endotoxemia. Anesthesiology. 2002;97(2):460–470.
- Mythen MG, Webb AR. Intra-operative gut mucosal hypoperfusion is associated with increased post-operative complications and cost. Intensive Care Med. 1994;20(2):99–104.
- Grocott MP, Mythen MG, Gan TJ, et al. Perioperative fluid management and clinical outcomes in adults. Anesth Analg. 2005;100(4):1093–1106.
- László I, Á J, Lovas A, et al. Effects of goal-directed crystalloid vs. colloid fluid therapy on microcirculation during free flap surgery: a randomised clinical trial. Eur J Anaesthesiol. 2019;36(8):592–604.
- Spss I. IBM SPSS statistics version 21. Boston, Mass: International Business Machines Corp; 2012.
- Field A. P. Discovering statistics using IBM SPSS statistics. Thousand Oaks, CA: SAGE Publications; 2013.
- Hahn RG, Drobin D, Sta° Hle L, et al. Volume kinetics of ringer’s solution in female volunteers. Br J Anaesth. 1997;78(2):144–148.
- Neff TA, Fischler L, Mark M, et al. The influence of two different hydroxyethyl starch solutions (6% HES 130/0.4 and 200/0.5) on blood viscosity. Anesth Analg. 2005;100(6):1773–1780.
- Gandhi S, Warltier D, Weiskopf R, et al. Volume substitution therapy with HES 130/0.4 (Voluven) versus HES 450/0.7 (hetastarch) during major orthopedic surgery. Crit Care. 2005;9(Suppl. 1):206.
- Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus ringer’s acetate in severe sepsis. N Engl J Med. 2012;367(2):124–134.
- Steppan J, Hofer S, Funke B, et al. Sepsis and major abdominal surgery lead to flaking of the endothelial glycocalyx. J Surg Res. 2011;165(1):136–141.
- Jacob M, Bruegger D, Rehm M, et al. The endothelial glycocalyx affords compatibility of starling’s principle and high cardiac interstitial albumin levels. Cardiovasc Res. 2007;73(3):575–586.
- Shoemaker WC, Appel PL, Kram HB, et al. Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest. 1992;102(1):208–215.
- Pope JV, Jones AE, Gaieski DF, et al. Multicenter study of central venous oxygen saturation (ScvO(2)) as a predictor of mortality in patients with sepsis. Ann Emerg Med. 2010;55(1):40–46.
- Futier E, Robin E, Jabaudon M, et al. Central venous O (2) saturation and venous-to-arterial CO (2) difference as complementary tools for goal-directed therapy during high-risk surgery. Crit Care. 2010;14(5):R193.
- Bakker J, Vincent JL, Gris P, et al. Veno-arterial carbon dioxide gradient in human septic shock. Chest. 1992;101(2):509–515.
- Futier E, Teboul JL, Vallet B, et al. Tissue carbon dioxide measurement as an index of perfusion: what have we missed?. TACC. 2011;1(1):95–99.
- Silbert BI, Litton E, Ho KM, et al. Central venous-to-arterial carbon dioxide gradient as a marker of occult tissue hypoperfusion after major surgery. Anaesth Intensive Care. 2015;43(5):628–634.
- Cuschieri J, Rivers EP, Donnino MW, et al. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med. 2005;31(6):818–822.
- Vallet B, Pinsky MR, Cecconi M, et al. Resuscitation of patients with septic shock: please ‘mind the gap’!. Intensive Care Med. 2013;39(9):1653–1655.
- Lobo DN, Stanga Z, Aloysius MM, et al. Effect of volume loading with 1 liter intravenous infusions of 0.9% saline, 4% succinylated gelatine (Gelofusine) and 6% hydroxyethyl starch(Voluven) on blood volume and endocrine responses: a randomized, three-way crossover study in healthy volunteers. Crit Care Med. 2010;38(2):464–470.
- He H, Liu D, Ince C, et al. Colloids and the microcirculation. Anesthesia Analg. 2018;126(5):1747–1754. 1.
- Kimberger O, Arnberger M, Brandt S, et al. Goal-directed colloid administration improves the microcirculation of healthy and perianastomotic colon. Anesthesiology. 2009;110(3):496–504.
- Konrad FM, Mik EG, Bodmer SI, et al. Acute normovolemic hemodilution in the pig is associated with renal tissue edema, impaired renal microvascular oxygenation, and functional loss. Anesthesiology. 2013;119(2):256–269.
- Chappell D, Jacob M, Hofmann-Kiefer K, et al. A rational approach to perioperative fluid management. Anesthesiology. 2008;109(4):723–740.
- Wu CY, Chan KC, Cheng YJ, et al. NTUH center of microcirculation medical research. effects of different types of fluid resuscitation for hemorrhagic shock on splanchnic organ microcirculation and renal reactive oxygen species formation. Crit Care. 2015;19(1):434.
- Hiltebrand LB, Kimberger O, Arnberger M, et al. Crystalloids versus colloids for goal-directed fluid therapy in major surgery. Crit Care. 2009;13(2):R40.
- Dubin A, Pozo MO, Casabella CA, et al. Comparison of 6% hydroxyethyl starch 130/0.4 and saline solution for resuscitation of the microcirculation during the early goal-directed therapy of septic patients. J Crit Care. 2010;25(4):659.e1–659.e8.
- Wafa K, Herrmann A, Kuhnert T, et al. Short time impact of different hydroxyethyl starch solutions on the mesenteric microcirculation in experimental sepsis in rats. Microvasc Res. 2014;95:88–93.