ABSTRACT
Background: Colon interposition is used for delayed surgical repair of esophageal atresia, but congenital esophageal atresia with or without tracheoesophageal fistula (CEA ± TEF) is associated with long-term respiratory morbidity. This study aimed to examine the prevalence of upper airway anomalies, and detect the implications of the preoperative flexible airway endoscopy (FAE) on the decision of performing tracheopexy whether aortopexy or more recently, posterior tracheopexy in cases of severe tracheomalacia. A randomized, prospective, controlled study was conducted in a tertiary care pediatric surgery center from September 2016 to October 2020 where thirty child of either sex, aged 2–8 years, scheduled for a colon interposition repair for esophageal atresia. After induction of general anesthesia dynamic airway endoscopic examination with ultra-thin fibroptic bronchoscopy was performed
Results: Dynamic study of pediatric upper airway showed that only one case out of 30 child enrolled in the present study had grade II subglottic stenosis in the proximal trachea (3.34%), while five cases (16.67%) had tracheomalacia with different degrees and only one severe case required aortopexy
Conclusion: Dynamic airway endoscopic examination can predict airway anomalies associated with esophageal atresia and enhance post colon interposition respiratory outcomes.
1. Background
Congenital esophageal atresia with or without tracheoesophageal fistula (CEA ± TEF) is the most common gastrointestinal (GI) atresia, which has an incidence of 1:2500–3000 live births [Citation1]. The surgical primary repair could be done either by right thoracotomy or thoracoscopy, occasionally esophagostomy and gastrostomy indicated for long atresia [Citation2]. In early 1900s colonic interposition had been used for esophageal reconstruction using either the left or right colon and in both conditions, the transverse colon was required [Citation3].
Even early surgical repair in neonatal period (CEA ± TEF) has long-term effects on respiratory and gastrointestinal function influencing colonic interposition post-operative outcome [Citation4].
Long-term respiratory consequences associated even with repair (CEA± TEF), including tracheomalacia and aspiration pneumonia associated with esophageal dysmotility and/or gastroesophageal reflux, may lead to reduced pulmonary function and bronchiectasis [Citation5].
Tracheomalacia is defined as an expiratory reduction > 50% in the cross-sectional luminal area during quiet respiration considered frequent issue in children with a history of (CEA ± TEF), wherein localized or generalized weakness of the tracheal wall occurs and creates airway obstruction resulting in different degrees of symptoms, in mild cases patient suffers from cough, whereas in severe cases respiratory distress episodes or “near-death” spells (acute life-threatening events, ALTE) and recurrent attacks of pneumonia occur as a result of collapse of trachea during cough which sequentially impairs expulsion of mucous during respiratory infection [Citation6].
Tracheomalacia (TM) is occasionally diagnosed with motion-picture X-rays (fluoroscopy) or computerized tomography scans (ciné-CT scan) of the chest, but most often, tracheomalacia is diagnosed with a bronchoscopy with the patient sedated or under general anesthesia [Citation7]. Although, in some cases, spontaneous improvement can occur, while in other severe cases several possible treatments applied including tracheostomy, non-invasive ventilation, airway stenting, and surgical approaches [Citation8].
Aortopexy is preferred surgical treatment of severe cases of TM in many centers, wherein lifting anteriorly the aorta and suturing it to the posterior surface of the sternum. As the anterior tracheal wall is attached through pre-tracheal fascia to the posterior aortic wall, the tracheal lumen is opened by aortopexy [Citation9]. Interestingly, posterior tracheopexy to the anterior longitudinal spinal ligament applicable in a case of severe tracheomalacia is associated with esophageal atresia (EA), and could be primary treatment at the time of initial EA repair or secondary treatment at the time of esophageal reconstruction surgery [Citation10].
The aim of the present study is to examine the prevalence of upper airway anomalies in patients with (CEA ± TEF) undergoing colon interposition procedure, detect the implications of the preoperative flexible airway endoscopy (FAE) on the decision of performing aortopexy or posterior tracheopexy in cases of severe tracheomalacia, and postoperative outcome.
2. Methods
Randomized prospective controlled study was conducted in a tertiary care pediatric surgery center from September 2016 to October 2020 after the approval of the regional ethical committee.
A written informed consent was obtained from the parents for the participation of their children in this study.
Thirty children of either sex, aged 2–8 years, scheduled for a colon interposition repair for congenital esophageal atresia were selected. Children suffering from Acquired TEF/EA, post corrosive esophageal stricture, and malnourishment were excluded from the study.
Premedication with atropine (0.02 mg/Kg) was administered intramuscularly less than 45 minutes before induction of anesthesia. Nebulized 2% lidocaine (4 mg/kg) by face mask prior to induction of anesthesia [Citation11]. All patients were fasting according to the American Society of Anesthesiology fasting rules [Citation12].
In the operation theatre, all patients were attached to a multichannel monitor in the form of continuous electrocardiogram, heart rate, pulse oximeter and non-invasive arterial blood pressure.
Anesthesia was induced with incremental concentrations of inhalational agent sevoflurane in 1–1 oxygen/air mixture using a silicone face mask size 1 or 2 connected to a Jackson-Rees circuit while maintaining spontaneous ventilation. A 24 G intravenous cannula was secured in place vein and bolus ringer’s lactate (2 ml/Kg), dexamethasone (0.6 mg kg) to minimize airway oedema with fentanyl 1 µg/kg had been given intravenously.
Proper sized Air-Q intubating laryngeal mask (ILM) was inserted and connected to a Jackson Rees anesthesia breathing system to maintain spontaneous ventilation of the child under inhalational anesthesia. Ensure appropriate position with ETCO2.
Prepared ultra-thin Olympus BF-XP60 fibroptic bronchoscopy of 2.8-mm outer diameter with defogging and lubrication was introduced through inserted Air-Q ILMA via an angle piece with a sealed port to perform dynamic study involving vocal cords movement, appearance, and tracheobronchial tree collapse, stenosis, or pulsation.
The problems confronting the anesthesiologist as hypoxia occured for many reasons include spontaneous ventilation obstruction so the scope might need to be repeatedly withdrawn, excessive suctioning would cause atelectasis, and bronchospasm could be secondary to irritation of the tracheobronchial tree, required supplemental 1% lidocaine sprayed via syringe through the bronchoscopic working channel into the airways, then withdrawal of fiberscope, shift to 100% oxygen concentration, deepening of anesthesia, 6–8 puffs of metered dose inhaler of salbutamol through laryngeal mask and 10 mcg intravenous epinephrine in severe unresponsive cases [Citation13].
After a complete dynamic study of pediatric upper airway removal of flexible bronchoscopy and Air-Q ILMA was done, and proper sized ETT was carried out with a Macintosh blade size 1–2 facilitated by rocuronium (0.6 mg/Kg).
After confirmation of ETT position with five consecutive waves of capnography, patients diverted to a circle system anesthesia breathing circuit and anesthesia maintained with rocuronium 0.2 mg/kg, fentanyl 1 µg/kg and sevoflurane 2–3% in a mixture of oxygen-air 1: 1
The patient is placed in a supine position with full neck extension using a roller under the shoulders, and the head rotated to the right to allow a clear left cervical operating field. Preparation of the left colon was done through median xipho-pubic incision, then the gastro-colic ligament was sectioned along the whole transverse colon in order to access the transverse mesocolon. The colon was completely mobilized by releasing and lowering the splenic and the hepatic flexures completely and continuing the dissection to the left until the colon-sigmoid junction, and to the right until the cecum, then measure the colon segment necessary for the reconstruction.
The medium colic vessels and the marginal arch were ligated and the colon was sectioned after verifying the effectiveness of the residual vascularization by placing vascular clamps at the base of the medium colic pedicle [Citation14].
A left cervical incision was carried out and the incision of the deep cervical fascia was extended to gain access to the retrosternal space.
Colon conduit pull-up was done through retrosternal route by blunt hand dissection of the retrosternal tunnel up to the neck. After the cervical esophago-colic anastomosis was completed, the transposed colon must be interrupted in the abdomen to have two sufficiently long portions to perform the proximal anastomosis (colon-gastric or colon-jejunal) and the distal colon-colic anastomosis [Citation15].
In a cases of severe tracheomalacia (STM) secondary posterior tracheopexy was performed by passing autologous pledged polypropylene sutures into but not through the posterior tracheal membrane, and securing them to the anterior longitudinal spinal ligament under direct bronchoscopic guidance [Citation16].
At the end of surgery they were reversed with sugammadex 2 mg/kg and were extubated.
In recovery room staff monitored closely vital signs (heart rate, pulse oximeter, and non-invasive blood pressure), signs of stridor secondary to subglottic oedema, which managed with nebulized epinephrine 1:1000 administered in a dose of 0.5 ml/kg, maximum 5 ml per administration. Nebulized epinephrine has a transient vasoconstricting effect, therefore dose might have to be repeated frequently, but intravenous dexamethasone produced constant relief of stridor with delayed onset of action. Re-intubation might be required in unresponsive cases [Citation17].
Demographic information (age, sex, weight), pre-operative respiratory symptoms, cardiorespiratory physiological changes including heart rate, systolic blood pressure (SBP), end-tidal CO2, and oxygen saturation (pre-induction, throughout the upper airway endoscopic examination procedure, every 15 minutes intra-operative, recovery period), dynamic study of pediatric upper airway findings as [Tracheomalacia; grading was done by visual inspection as mild (50–75% reduction), moderate (75–90% reduction), severe (>90%) [Citation18], subglottic stenosis: grading by Myer-Cotton classification [Citation19], recurrent TEF, or tracheal pouch], procedure time started from introduction of airway endoscopy till removal of Air Q ILMA, procedure-related complications including hypoxemia (oxygen saturation < 90%), hypotension (systolic blood pressure (SBP) below the 5th percentile for age <70 + 2(age in years) [Citation20]), and need for aortopexy or posterior tracheopexy in sever degree of tracheomalcia were recorded.
3. Statistical methods
The sample size is approved to be sufficient by the department of Statistics, Medical Research Institute [Citation21].
Data were analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp).). Student t-test was used to compare two groups for normally distributed quantitative variables.
Fisher exact test and Mann-Whitney test were used as appropriate. Results were expressed as mean and interquartile range. P < 0.05 was considered significant.
4. Results
A total of 39 infants were screened for eligibility; 34 patients met inclusion criteria and were approached to participate, and four parents refused to engage their infants in the study [Flowchart 1].
Flowchart 1: Flow diagram
There was no statistically significant difference between the two groups regarding age, gender, and weight ().
Table 1. Demographic data
Regarding respiratory symptoms most of children enrolled in the present study (78%) suffered from cough and frequent attacks of chest infection, only six cases suffered from exertional dyspnea (20%), whereas two cases had “near-death” spells (acute life-threatening events, ALTE) (6.67%).
During flexible bronchoscopic examination the cardiorespiratory physiological changes showed a statistically significant increase in SBP and heart rate during compared to pre-induction readings simultaneously with increased end-tidal CO2 level while oxygen saturation decline was statistically insignificant compared to pre-induction level ().while intraoperative and recovery period cardiorespiratory parameters yielded no statistically significant differences compared to pre-induction readings.
Table 2. Comparison between pre-induction and throughout procedural cardiorespiratory parameters
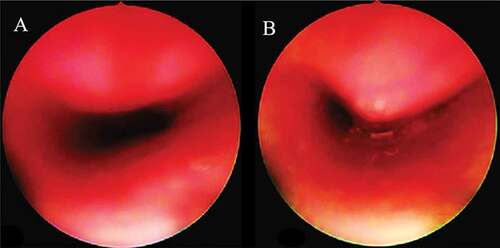
Dynamic study of pediatric upper airway in children with CEA±TEF scheduled for colon interposition completed in about (5.2 ± 1.2 minutes) showed that only one case out of 30 child enrolled in the present study had grade II subglottic stenosis () in the proximal trachea (3.34%), while five cases (16.67%) had different degrees of tracheomalacia (mild = 40%, moderate = 40, severe = 20% respectively) only one case of severe tracheomalacia () required posterior tracheopexy. There were no procedure-related complication.
5. Disscusion
Esophageal atresia (EA) is a congenital malformation with a frequency of 1 per 3,000 to 3,500 live births [Citation22]. The surgical treatment for EA is reliable; however, complications such as anastomotic stricture, gastro-esophageal reflux disease (GERD), and anastomotic leak are often observed after surgery [Citation23].
Late complications of EA/TEF include tracheomalacia, a recurrence of the TEF, esophageal stricture, and gastroesophageal reflux [Citation24]. Tracheomalacia (TM) is a condition of excessive tracheal collapsibility, due either to disproportionate laxity of the posterior wall (pars membranacea) or compromised cartilage integrity [Citation25].
Dynamic study of pediatric upper airway in children with CEA±TEF showed that only 5 cases (16.67%) had different degrees of tracheomalacia only one case of severe tracheomalacia required aortpexy.
In contrast with present study Hseu et al. [Citation26] found that prevalence of tracheomalacia in children undergone surgery for CEA ± TEF ranging from 37.5% to 75% of patients, however Fraga et al [Citation27] concluded that most of the cases of tracheomalacia are self-limiting, with spontaneous resolution in the first months/years of life.
In agreement with the present study Sadreameli et al [Citation28] reported that severe expression of tracheomalacia is found in 11–33% of children. Furthermore Corbally et al [Citation29] concluded that surgical intervention of aortopexy is recommended in severe cases.
Moreover the dynamic upper airway endoscopic examination showed that only one case had grade II subglottic stenosis in the proximal trachea (3.34%), in agreement with the present result Andrea Conforti et al [Citation30] found that incidence of grade II subglottic stenosis was 4% in 207 patients with EA/TEF.
Additionally no procedure related complications faced in the present study, likeminded Dustin et al [Citation31] concluded that using a small caliber flexible endoscope in anesthetized patient offers excellent visualization of the proximal and distal airways with no risk of complications.
6. Conclusion
Dynamic airway endoscopic examination can detect airway anomalies associated with esophageal atresia and enhance post colon interposition respiratory outcomes.
Abbreviations
ALTE; Acute Life Threatening Events, STM; Sever Tracheomalacia, CEA ± TEF; Congenital Esophageal Atresia with or without Tracheo-Esophageal Fistula, FAE; Flexible Airway Endoscopy, TM: Tracheomalacia, EA; Esophageal Atresia, ETT; Endotracheal Tube, ILMA; Intubating Laryngeal Mask Airway, CT; Computerized Tomography, SBP; Systolic Blood Pressure, GERD; Gastro-esophageal Reflux Disease.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the author(s).
References
- DeBoer EM, Prager JD, Ruiz AG, et al. Multidisciplinary care of children with repaired esophageal atresia and tracheoesophageal fistula. Pediatr Pulmonol. 2016;51(6):576–581.
- Bairdain S, Ricca R, Riehle K. Early results of an objective feedback-directed system for the staged traction repair of long-gap esophageal atresia. J Pediatr Surg. 2013;48(10):2027–2031.
- Boukerrouche A. Isoperistaltic left colic graft interposition via a retrosternal approach for esophageal reconstruction in patients with a caustic stricture: mortality, morbidity, and functional results. Surg Today. 2014;44:827–833.
- Acher CW, Ostlie DJ, Leys CM, et al. Long-term outcomes of patients with tracheoesophageal fistula/esophageal atresia: survey results from tracheoesophageal fistula/esophageal atresia online communities. Eur J Pediatr Surg. 2016;26(6):476–480.
- Shah R, Varjavandi V, Krishnan U. Predictive factors for complications in children with esophageal atresia and tracheoesophageal fistula. Dis Esophagus. 2015;28(3):216–223.
- Cartabuke RH, Lopez R, Thota PN. Long-term esophageal and respiratory outcomes in children with esophageal atresia and tracheoesophageal fistula. Gastroenterol Rep. 2015;1–5.
- Carden KA, Boiselle PM, Waltz DA, et al. Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth review. Chest. 2005;127:984–1005.
- Torre M, Carlucci M, Speggiorin S, et al. Aortopexy for the treatment of tracheomalacia in children: review of the literature. Ital J Pediatr. 2012;38:62.
- Jennings RW, Hamilton TE, Smithers CJ. Surgical approaches to aortopexy for severe tracheomalacia. J Pediatr Surg. 2014;49:66–71.
- Shieh HF, Smithers CJ, Hamilton TE, et al. Posterior tracheopexy for severe tracheomalacia associated with esophageal atresia (EA): primary treatment at the time of initial EA repair versus secondary treatment. Front Surg. 2017;4:80.
- Suzette TG, Lowenthal DB, Dozor AJ. Nebulized lidocaine administered to infants and children undergoing flexible bronchoscopy. CHEST. 1997;112(6):1665–1669.
- Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the american society of anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126:376–393.
- Londino AV, Jagannathan N. Anesthesia in Diagnostic and Therapeutic Pediatric Bronchoscopy. Otolaryngol Clin North Am. 2019;52(6):1037–1048.
- Bakshi A, Sugarbaker DJ, Burt BM. Alternative conduits for esophageal replacement. Ann Cardiothorac Surg. 2017;6(2):137–143.
- Fisher RA, Griffiths EA, Evison F, et al. A national audit of colonic interposition for esophageal replacement. Dis Esophagus. 2017;30(5):1–10.
- Shieh HF, Smithers CJ, Hamilton TE, et al. Posterior tracheopexy for severe tracheomalacia. J Pediatr Surg. 2017;52(6):951–955.
- Roberts S, Thornington RE. Paediatric bronchoscopy. Continuing education in anaesthesia. Crit Care Pain. 2005;5(2):41–44.
- Bergeron M, Cohen AP, Cotton RT. The management of cyanotic spells in children with oesophageal atresia. Front Pediatr. 2017;5:106.
- Myer CM, O’connor DM, Cotton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol. 1994;103(4):319–323.
- Ikram U, Haque AL, Zaritsky. Analysis of the evidence for the lower limit of systolic and mean arterial pressure in children. Pediatr Crit Care Med. 2007;8(2):138–144.
- Sharma N, Srinivas M. Laryngotracheobronchoscopy prior to esophageal atresia and tracheoesophageal fistula repair–its use and importance. J Pediatr Surg. 2014;49(2):367–369.
- Rothenberg S. Thoracoscopic repair of esophageal atresia and tracheo-esophageal fistula in neonates: the current state of the art. Pediatr Surg Int. 2014;30:979–985.
- Yoo HJ, Kim WS, Cheon JE, et al. Congenital esophageal stenosis associated with esophageal atresia/tracheoesophageal fistula: clinical and radiologic features. Pediatr Radiol. 2010;40:1353–1359.
- Kovesi T, Rubin S. Long-term complications of congenital esophageal atresia and/or tracheoesophageal fistula. Chest. 2004;126(3):915–925.
- Ridge CA, O’Donnell CR, Lee EY, et al. Tracheobronchomalacia: current concepts and controversies. J Thorac Imaging. 2011;26:278–289.
- Hseu A, Recko T, Jennings R, et al. Upper airway anomalies in congenital tracheoesophageal fistula and esophageal atresia patients. Ann Otol Rhinol Laryngol. 2015;124:808–813.
- Fraga JC, Jennings RW, Kim PCW. Pediatrc tracheomalacia. Semin Pediatr Surg. 2016;25:156–164.
- Sadreameli SC, McGrath-Morrow SA. Respiratory care of infants and children with congenital tracheo-oesophageal fistula and oesophageal atresia. Paediatr Respir Rev. 2016;17:16–23.
- Corbally MT, Spitz L, Kiely E, et al. Aortopexy for tracheomalacia in oesophageal anomalies. Eur J Pediatr Surg. 1993;3:264–266.
- Conforti A, Valfrè L, Scuglia M, et al. Laryngotracheal abnormalities in esophageal atresia patients: a hidden entity. Front Pediatr. 2018;6:401.
- Walters DM, Wood DE. Operative endoscopy of the airway. J Thorac Dis. 2016 Mar;8(2):130–139.