ABSTRACT
The aim of the present study was to compare visibility of the mandibular canal on cone beam computed tomography (CBCT)-based orthoradial and oblique slices at molar implant sites. CBCT images for 132 mandibular molar implant sites were selected for the study. After generating orthoradial and oblique slices, two observers evaluated the visibility of the mandibular canal using three-point scoring scale (1–3, good to excellent). Wilcoxon signed-rank test compared the visibility scores of the two slices. Both orthoradial and oblique slices obtained from CBCT had only very good to excellent mandibular canal visibility scores. At 114 mandibular molar implant sites, the visibility score was equal on both orthoradial and oblique slices. Although the visibility score was higher on orthoradial slices for 12 implant sites, the visibility score was higher for six implant sites on oblique slices and the difference was not significant. Therefore, the visibility of the mandibular canal was excellent and comparable on most of orthoradial and oblique slices obtained from CBCT images.
Introduction
Over the last few decades, missing teeth have been successfully treated with dental implants.[Citation1] With the introduction of three-dimensional (3D) imaging modalities like computed tomography (CT) and cone beam CT (CBCT), vital anatomical structures like mandibular canal could be visualized in several imaging planes or slices.[Citation2]
As the measurements of available bone depth and hence implant length are influenced by the location of mandibular canal, the visibility of the latter on CT or CBCT scans is paramount, should operative complications at mandibular implant sites be avoided.[Citation3] Therefore, several studies have investigated the visibility of the mandibular canal by using different imaging modalities.[Citation4–Citation15] However, varying observations of mandibular canal have been obtained and this could be due to the imaging modality itself (2D or 3D), voxel size, the tomographic plane angulation, and the course or location of canal on different images.
For proper implant placement, the axial angulation should be carefully determined in order to transmit the occlusal forces vertically through the implant's long axis.[Citation16] However, at mandibular molar implant sites, a slight mesial tilt helps aligning implant-retained prostheses along the curve of Spee. Tilted implants are also useful in cases with severe ridge resorption in order to avoid injury to the mandibular canal,[Citation17] and to avoid the surgery needed for canal transposition or bone grafting.[Citation18] In addition, titling increases the amount of bone available for osseointegration.[Citation19]
In one recent study by Neves et al.,[Citation20] cross-sectional CBCT images were generated by using two different slice inclinations: orthoradial and oblique. Although the main focus of interest of Neves et al.[Citation20] was the height of the mandibular body and not the visibility of the mandibular canal, they reported that bone height measurements on orthoradial slices were statistically different from the gold standard at mandibular molar implant sites.
For CBCT implant planning, several software can be used, and different implant angulations can be determined using different slice inclinations. If different slice inclinations can adversely affect the visibility of mandibular canal, this will result in choosing incorrect implant length and might lead to nerve injury at the time of implant placement. On the other hand, if the visibility of mandibular canal can be enhanced by using different slice inclinations, this can be advantageous and utilized at the time of implant planning. Thus, the aim of our current study is to investigate the influence of different slice inclinations on the visibility of mandibular canal on orthoradial and oblique CBCT slices at mandibular molar implant sites.
Materials and methods
Patients
In our retrospective study, images for all patients who underwent CBCT examination for dental implant treatment and other dental purposes at our dental radiology clinic were retrieved and evaluated between January 2011 and January 2015. Only cases with missing lower molars were included in the study. The number of cases included was 68 (23 males and 45 females) with a mean patient age of 54 years, and the remaining implant sites were 132. Cases with artefacts or pathology affecting the visibility of mandibular canal at the implant sites were excluded. Additionally, it was essential to exclude cases where mandibular canal was not visible on all of the generated slices due to using large voxel size or due to systemic bone diseases like osteoporosis.
CBCT examination
A KODAK 9500 Cone Beam 3D System (Carestream, Rochester, NY) CBCT apparatus with flat panel detector was used. The imaging area of CBCT is a cylinder with a height of 15–20.6 cm and a diameter of 9–18 cm providing isotropic cubic voxels with sides approximating 0.2–0.3 mm. Only cases examined with 0.2 mm were included in the study. The exposure parameters were as follows: 90 kV as a tube voltage, 10 mA as a tube current, and an exposure time of 10.8 seconds.
Examinations were performed by 360° rotation in the occlusal position with the patient standing and closing their teeth.
Images
One calibrated oral radiologist (MA) with eight years of experience with CBCT and dental implants was responsible for generating orthoradial and oblique slices at proposed mandibular molar implant sites after creating pseudo-panoramic images, and then saving the slices in JPEG format for a second evaluation by one oral surgeon (FJ) with eight years of experience.
The curved slicing module was used for creating pseudo-panoramic images, and the arch was manually created on the horizontal section. The horizontal section was automatically displayed by the software and the thickness of the focal trough was adjusted in order to fit the mandible of each patient. Then the mandible was only displayed by using the function ‘displaying region of interest’.
To generate orthoradial slices, a vertical blue line on the displayed panoramic image was moved to the proposed implant site while keeping it perpendicular to the occlusal plane. The oblique slices were generated by moving the blue line to the same site and then tilting it 10° mesially, if it is in the area of missing first molar, and tilting it 14° mesially, if it is in the area of missing second molar. The 10° and 14° of mesial tilting represent the natural angulations of mandibular first and second molars, respectively,[Citation21] and for applying these angulations, all implant sites had to be the last distal sites considered for implant placement and preceded by missing tooth mesially. In addition to this, 9 mm of mesiodistal space was left between the implant sites and nearby teeth, which is considered suitable for another implant placement if needed.
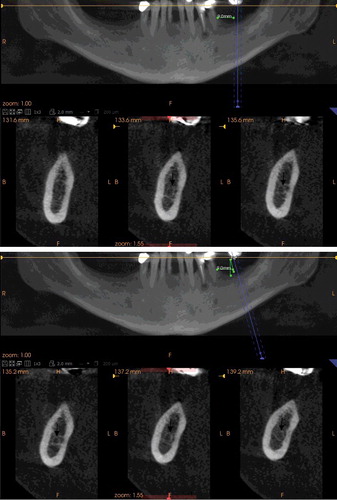
For each implant site, three orthoradial and three oblique slices were generated by setting the interslice distance to 2 mm; therefore, the diameter of the proposed implants was 4 mm. The mandibular canal was considered visible and given a score of 1 (good) if it was detected and was possible to be delineated from the surrounding bone marrow spaces on one slice, a score 2 (very good) if it was visible on two slices, and a score of 3 (excellent) if it was visible on three slices (–).
Figure 1. Second molar implant site in which the visibility score of the mandibular canal (arrow) was equal on both of orthoradial (a) and oblique slices (b).
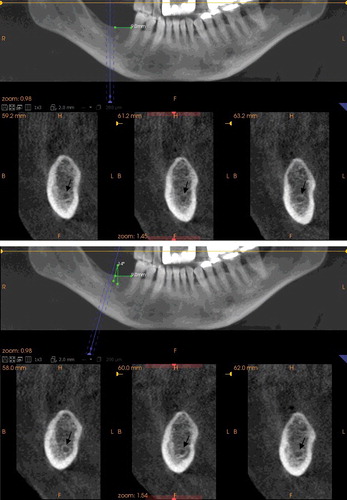
Figure 2. First molar implant site in which the visibility score of the mandibular canal (arrow) was more on orthoradial (a) than oblique slices (b).
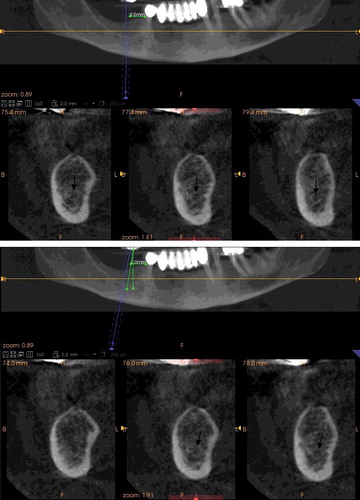
Figure 3. Second molar implant site in which the visibility score of the mandibular canal (arrow) was less on orthoradial (a) than oblique slices (b).
All images were evaluated on LCD monitor with installed CS 3D imaging viewer (CS 3D imaging viewer, 3.2.9 Carestream, Rochester, NY). When necessary, the window settings were adjusted to optimize the images for evaluation.
Statistical analysis
Intraclass correlation coefficient (ICC) was used to assess interobserver agreement, and Wilcoxon signed-rank test was used to compare the visibility of mandibular canal at molar implant sites on orthoradial and oblique slices. Statistical significance was set at a level of 0.05.
All statistical analyses were performed by using a statistical software package (SPSS version 16; Chicago, IL).
Results and discussion
For the 132 molar implant sites (55 first molars and 77 second molars), the interobserver agreement for the visibility scores of orthoradial and oblique CBCT slices was excellent; ICCs for single measures were 0.848 and 0.885, respectively. Between the two observers, disagreement was present in five cases and consensus was reached after discussion.
The visibility scores of orthoradial and oblique CBCT slices are shown in . At all implant sites, the visibility scores were very good to excellent (2 or 3). Among them, 114 implant sites (48 first molars and 66 second molars) had equal visibility scores, 12 implant sites (6 first molars and 6 second molars) had higher visibility scores on orthoradial slices, and 6 implant sites (1 first molar and 5 second molars) had higher visibility scores on oblique slices. According to Wilcoxon signed-rank test, the difference between visibility scores was not significant.
Table 1. The visibility scores of orthoradial and oblique CBCT slices according to location of implant site.
In this study, we evaluated the visibility of mandibular canal on othroradial and oblique CBCT slices at molar implant sites, and at all implant sites, the visibility score was very good to excellent, this means that the mandibular canal was visible on most of CBCT slices. Such findings are in agreement with Shokri et al.[Citation13] The canal could be identified and considered visible even if it was not corticated, and the usage of small voxel size could be also a contributing factor to the attained excellent visibility of the canal.
In the study of Neves et al.,[Citation20] a comparison was made between bone height measurements on oblique, orthoradial CBCT slices, and dried mandibles with the latter being the gold standard. At molar implant sites, the orthoradial slices were found inaccurate for such measurements. This could be due to different visibility of the crest of the ridge or the inferior border of the mandible which were used for bone height measurements. In the same study of Neves et al.,[Citation20] the slice angulation used for obtaining oblique CBCT slices was not reported and the visibility of mandibular canal was not studied. In clinical dental implant practice, the bone height must be measured from the crest of the ridge till the superior border of the mandibular canal,[Citation3] in order to avoid injury to the canal at the time of implant placement. Thus in contrast to the previous study, we used specific slice angulation for obtaining oblique slices and evaluating the visibility of mandibular canal. Our results showed that the visibility on most of orthoradial and oblique CBCT slices was equal in most slices and different only in few slices. In these few slices, changing slice angulation leads to different orientation of the canal in relation to bone marrow spaces, which in turn affected the visibility of the canal, especially if it was not corticated.
To the best of the authors’ knowledge, only one study reported the visibility of mandibular canal on different slice angulations.[Citation11] However, different horizontal slice angulations were used by that study and the slices were cross-sectional tomographic. Therefore, up to our knowledge, there has not been any published works showing the influence of mesial slice angulation on the visibility of mandibular canal on orthoradial and oblique CBCT slices at molar implant sites.
Some studies evaluated the visibility of mandibular canal on digital panoramic and CT or CBCT cross-sectional images.[Citation4,Citation8,Citation10,Citation12,Citation13] In all of these studies, the visibility of mandibular canal was declined when moving from third molar area towards first molar area. In addition, when the visibility was compared between CBCT or CT cross-sectional images and digital panoramic images, CBCT and CT cross-sectional images outperformed digital panoramic images in identification of the mandibular canal.[Citation4,Citation10] In contrast with these results, the visibility of mandibular canal was significantly higher in panoramic views when reformatted from CT and compared with cross-sectional CT views.[Citation15] This could be due to the high quality and minimum thickness of reformatted CT panoramic views when compared with conventional digital panoramic radiographs.[Citation8]
Although the depiction of mandibular canal is consistent and comparable between CT and CBCT,[Citation6,Citation7] CBCT is recommended and preferred over CT due to low radiation dose and high image resolution.[Citation22] Therefore, a drawback can be noticed in the previous studies which used CT images for visualizing of the mandibular canal before implant placement.[Citation10,Citation15] Moreover, rather than comparing the visibility of the canal on reformatted panoramic views with cross-sectional views,[Citation15] it is necessary to identify the canal on both of the views,[Citation9] since the canal has different locations on them.
The visibility of mandibular canal may vary according to its location and course on panoramic images.[Citation4,Citation23] Jung et al.[Citation4] reported the highest visibility of the canal when it displays a spoon-shaped curve on panoramic radiographs. In our current study, there was no attempt to study the influence of canal shape or angulation on panoramic radiographs on its visibility on cross-sectional CBCT images, but mesial slice angulation was studied, and the visibility of canal was affected by this angulation at few implant sites. At five implant sites, oblique CBCT slices outperformed orthoradial CBCT slices at the second molar area, thus in cases with poor visibility of the canal at the second molar area, slight change in mesial slice angulation might be recommended to improve the visibility of the canal.
Our study has some limitations. For implant planning, we applied specific implant angulations at specific implant sites, this may not necessarily represent a true clinical situation and other factors may affect the final plan. Moreover, the visibility of mandibular canal might have a relation with the degree of cortication rather than the slice angulations and longitudinal studies may be needed to resolve this issue.
Conclusions
In conclusion, mesial slice angulation has minimal effect on the visibility of mandibular canal. Therefore, the visibility is excellent and comparable on most of orthoradial and oblique CBCT slices at molar implant sites.
Disclosure statement
The authors deny any conflicts of interest. The authors declare that they have no competing interests.
References
- van Velzen FJ, Ofec R, Schulten EA, et al. 10-year survival rate and the incidence of peri-implant disease of 374 titanium dental implants with a SLA surface: a prospective cohort study in 177 fully and partially edentulous patients. Clin Oral Implants Res. 2015;26:1121–7.
- White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th ed. St. Louis (MO): Mosby Elsevier; 2014.
- Mehra A, Pai KM. Evaluation of dimensional accuracy of panoramic cross-sectional tomography, its ability to identify the inferior alveolar canal, and its impact on estimation of appropriate implant dimensions in the mandibular posterior region. Clin Implant Dent Relat Res. 2012;14:100–7.
- Jung YH, Cho BH. Radiographic evaluation of the course and visibility of the mandibular canal. Imaging Sci Dent. 2014;44:273–7.
- de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16:387–7.
- Liang X, Jacobs R, Hassan B, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT). Part I. On subjective image quality. Eur J Radiol. 2010;75:265–7.
- Naitoh M, Nakahara K, Suenaga Y, et al. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:25–7.
- Angelopoulos C, Thomas SL, Hechler S, et al. Comparison between digital panoramic radiography and cone-beam computed tomography for the identification of the mandibular canal as part of presurgical dental implant assessment. J Oral Maxillofac Surg. 2008;66:2130–7.
- Gerlach NL, Meijer GJ, Maal TJ, et al. Reproducibility of 3 different tracing methods based on cone beam computed tomography in determining the anatomical position of the mandibular canal. J Oral Maxillofac Surg. 2010;68:811–7.
- Kamrun N, Tetsumura A, Nomura Y, et al. Visualization of the superior and inferior borders of the mandibular canal: a comparative study using digital panoramic radiographs and cross-sectional computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:550–7.
- Naitoh M, Katsumata A, Kubota Y, et al. The role of objective plane angulation on the mandibular image using cross-sectional tomography. J Oral Implantol. 2006;32:117–7.
- Oliveira-Santos C, Capelozza AL, Dezzoti MS, et al. Visibility of the mandibular canal on CBCT cross-sectional images. J Appl Oral Sci. 2011;19:240–7.
- Shokri A, Shakibaei Z, Langaroodi AJ, et al. Evaluation of the mandibular canal visibility on cone-beam computed tomography images of the mandible. J Craniofac Surg. 2014;25:273–7.
- Lofthag-Hansen S, Gröndahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res. 2009;11:246–7.
- Takahashi A, Watanabe H, Kamiyama Y, et al. Localizing the mandibular canal on dental CT reformatted images: usefulness of panoramic views. Surg Radiol Anat. 2013;35:803–7.
- Machtei EE, Oettinger-Barak O, Horwitz J. Axial relationship between dental implants and teeth/implants: a radiographic study. J Oral Implantol. 2014;40:425–7.
- DE Vico G, Bonino M, Spinelli D, et al. Rationale for tilted implants: FEA considerations and clinical reports. Oral Implantol (Rome). 2011;4:23–7.
- Krekmanov L, Kahn M, Rangert B, et al. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15:405–7.
- Pancko F, Dyer J, Weisglass S, et al. Use of tilted implants in treatment of the atrophic posterior mandible: a preliminary report of a novel approach. J Oral Maxillofac Surg. 2010;68:407–7.
- Neves FS, Vasconcelos TV, Oenning AC, et al. Oblique or orthoradial CBCT slices for preoperative implant planning: which one is more accurate? Braz J Oral Sci. 2014;13:104–7.
- Nelson S, Ash MM. Wheeler's dental anatomy, physiology and occlusion. 9th ed. St. Louis (MO): Saunders Elsevier; 2009.
- Tyndall DA, Price JB, Tetradis S, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:817–7.
- Gowgiel JM. The position and course of the mandibular canal. J Oral Implantol. 1992;18:383–7.
