ABSTRACT
Health and social care workers (HSCWs) have an essential role in the uptake of the COVID-19 vaccine. Vaccination is an emotionally charged issue and perceptions of risk associated with COVID19 can contribute towards vaccine hesitancy (VH). The aim of this study was to explore the role of emotion and risk perception associated with HSCWs’ uptake of the COVID-19 vaccine during the initial mass roll-out of the vaccine in Scotland. A cross-sectional online survey with a correlational design was used. An online survey was conducted with HSCWs (N = 1189) aged 18 to 67 years (M = 44.09 yrs, SD = 11.48) working in Scotland during the third lockdown period (26 December – 31 March 2021) of the COVID-19 pandemic. The survey collected data relating to sociodemographic characteristics, vaccine uptake and VH, emotions associated with the COVID-19 vaccine, and risk perception. Open-ended free text data were also collected on HSCWs’ main reasons for VH. Most participants (83.96%) felt positively about the roll-out of the COVID-19 vaccine, stating it would be beneficial for themselves and others to receive it. Nonetheless, 16.04% of HSCWs expressed VH. Occupational group, age, gender and risk perceptions did not affect variance in VH, but positive emotions associated with the COVID-19 vaccine and years of experience did. We emphasise the importance of future interventions to increase COVID-19 vaccine uptake by enhancing positive emotions and reducing ambivalent emotions associated with the COVID-19 vaccine particularly among less experienced HSCWs.
Introduction
While mass vaccination is an essential public health intervention in gaining long-term control of the COVID-19 pandemic (Dubé & MacDonald, Citation2022; Goralnick et al., Citation2021), COVID-19 vaccine hesitancy (VH) is an obstacle to uptake (Heyerdahl et al., Citation2022; Sonawane et al., Citation2021). VH is the mental state of holding back, in doubt or indecision regarding vaccination and includes a broad spectrum of attitudes, beliefs and behaviours from intentional vaccine delay to vaccine refusal (Troiano & Nardi, Citation2021). VH is dependent on context, the specific vaccine(s), and the target population (Verger et al., Citation2022). Research has shown that COVID-19 VH rates differ worldwide (Khubchandani et al., Citation2021; Lazarus et al., Citation2021; Sallam, Citation2021) among children, parents, and diverse adult populations and occupational groups (Alfieri et al., Citation2021; Butter et al., Citation2022; Fridman et al., Citation2021; Holeva et al., Citation2022; Rhodes et al., Citation2020; Tam et al., Citation2022), however, there has been an emerging interest in VH among health and social care workers (HSCWs) who were prioritised for receiving the COVID-19 vaccine (Aw et al., Citation2022; Biswas et al., Citation2021; Chudasama et al., Citation2022; K. H. Nguyen et al., Citation2021; Kwok et al., Citation2021; MacDonald & Dubé, Citation2015). Previous studies have demonstrated the importance of HSCWs in recommending COVID-19 vaccination to increase uptake (Reiter et al., Citation2020). The reasons for VH among HSCWs are complex and involve socio-demographic, contextual, physical, and psychosocial factors (Afzal et al., Citation2022; Betsch et al., Citation2015; Digregorio et al., Citation2022; Kose et al., Citation2021; Murphy et al., Citation2021; Swann et al., Citation2022; Toth-Manikowski et al., Citation2022; Woolf et al., Citation2021). Among various efforts to address VH and foster vaccine confidence, health behaviour scientists have increasingly emphasised affect related concepts, including the role of emotion, in attempts to understand and facilitate change in important health behaviours (Luz et al., Citation2019; Shiota et al., Citation2021; Williams & Evans, Citation2014). For example, negative emotions, such as fear and anxiety, may increase VH, while activating positive emotions, such as altruism and hope, may increase vaccine uptake (Berry et al., Citation2021; Chou & Budenz, Citation2020; Vergara et al., Citation2021). Attention to emotion can complement other aspects of vaccine dissemination, such as building trust and credibility of health agencies and scientific experts (Ferrer & Ellis, Citation2019), yet little research has explored the role of emotion in VH among HSCWs. Emotion has been found to influence public perceptions of risks associated with COVID-19 (Cipolletta et al., Citation2022; Dubé & MacDonald, Citation2022; Zong et al., Citation2021), and risk perception has been identified as a significant factor influencing VH (Dryhurst et al., Citation2020). Individuals may lack confidence in the vaccine and fear undesirable side-effects, or underestimate the severity of the disease and do not perceive a need for a vaccine (Kwok et al., Citation2021; Reiter et al., Citation2020; Zheng et al., Citation2022).
Of the few studies that have explored COVID-19 risk perception and VH among occupational groups (Arslanca et al., Citation2021; Paudel et al., Citation2021), the focus has commonly been on medical staff (Yilmaz et al., Citation2021). Research conducted in Israel prior to the roll out of the COVID-19 vaccine found that most healthcare workers intended to accept the vaccine; however, 22% of doctors and 39% of nurses were VH (Dror et al., Citation2020). Similarly, a study of US healthcare workers reported that only 33% would get a vaccine when made available to them (Gadoth et al., Citation2021). A study conducted in US healthcare employees on the eve of vaccine roll out found that when asked whether they would accept the COVID-19 vaccine, 55.3% of respondents said yes, 16.3% said no, and 28.4% were undecided (Meyer et al., Citation2021). Further, healthcare workers directly involved in the care of COVID-19 patients are less likely to report VH than medical workers who are not; with 94% indicating that they would accept a vaccine (Dror et al., Citation2020). A recent integrative review of VH among US healthcare workers found that estimates of VH were similar to the general population (Caiazzo & Stimpfel, Citation2022). Research suggests that even among healthcare workers, there is a reliance on personal risk-benefit perception which contrasts concerns regarding the safety, efficacy, and potential side effects of the vaccine against risks of contracting the disease (Biswas et al., Citation2021). To date, little is known about VH among social care workers.
The present study explored which socio-demographic and psychosocial factors (specifically, emotion and risk perception) predicted COVID-19 VH among HSCWs and their reasons for VH. It should be noted that during the conduct of the sudy, HSCWs were operating under difficult and challenging conditions. Even prior to the COVID-19 pandemic, a prolonged period of austerity measures had resulted in cuts to public sector spending (Cavero & Poinasamy, Citation2013). Although the budget for the NHS was not reduced, a below average increase in funding alongside cuts in other areas of public spending, particularly in relation to social care had an adverse impact (Kerasidou et al, Citation2019), including staff shortages and resource constraints across health and social care, all of which combined to create difficult working conditions for staff. The significant political and social uncertainties within Scotland were exacerbated by the challenges raised by Brexit (Leith & Sim, Citation2020) and the onset of the COVID-19 pandemic. As a devolved nation, the Scottish Government established five ‘protection’ levels of COVID-19 restrictions setting out the rules that should be followed in each Local Authority area. On the 26th of December 2020 mainland Scotland was moved to Level 4 restrictions to contain a new variant of the COVID-19 virus. In Level 4, only essential shops and places of worship were allowed to open while up to 4 people from two households could meet outside and hospitality was closed. The first vaccines were offered from the 8 December 2020 with HSCWs being a priority group. A full lockdown and a ‘stay at home’ order was re-introduced on the 5th of January 2021. By the 10th of February 2021, over one million people in Scotland had been vaccinated. The ‘stay at home’ order was lifted on the 5th of April 2021 with restrictions gradually being relaxed over the coming months.
Methods
Participants and procedure
HSCWs aged 18 or older and working within the health and/or social care sector in Scotland for at least 6 months were invited to participate in the study. This included HSCWs working in the National Health Service as well as local authorities, non-statutory social care and charitable organisations. A cross-sectional online survey was conducted to identify factors associated with VH among HSCWs. The research was ethically approved by the Ethics Committee. Informed consent was obtained prior to completing the survey via Qualtrics, and participants received a debrief upon completion. The study took place during the first phase of the roll out of mass vaccination for COVID-19 (December 2020 to March 2021), during which HSCWs were prioritised. Participants were recruited using a convenience sample through social media posts (Facebook and Twitter), and NHS and third sector intranet platforms.
Measures
Socio-demographical characteristics: Socio-demographic information including occupation, education, years of experience, age, gender, health, vaccination status, personal history of experiencing COVID-19 symptoms or a diagnosis, and whether they had been asked to work remotely.
COVID-19 Vaccination. Participants were asked if they had received or been offered the COVID-19 vaccine, and whether they perceived it would be beneficial to them and others to get vaccinated when available. Response options included ‘Yes’, ‘No’, and ‘I am hesitant about it’. We dichotomised these responses into ‘hesitant’ and ‘non-hesitant’ by merging the latter two options as indicative of VH.
Emotions associated with COVID-19 vaccine: Guided by earlier work exploring the role of emotions and VH (Berry et al., Citation2021; Dubé et al., Citation2018; Tomljenovic et al., Citation2020), we presented participants with a range of positive and negative emotions to select those that they associated with the COVID-19 vaccine. Participants could select as many as were applicable. Participants who selected both a minimum of one positive and one negative emotion were coded as ‘ambivalent’, while those who ticked at least one positive were coded as ‘positive’ and at least one negative as ‘negative’.
COVID-19 Risk Perception Scale. The COVID-19 Perceived Risk Scale to assessed participant’s perceived risks associated with COVID-19. This 8-item questionnaire on a 5-point Likert scale is a psychometrically-sound scale includes emotional as well as a cognitive dimensions (Yıldırım & Güler, Citation2020). A higher score reflects greater perceived risk of COVID-19 when all of the items are scored to generate a total score.
Free Text Response. An open-ended question (what are the main reasons for you being hesitant about the COVID-19 vaccine?) was used to offer HSCWs, who reported that they were VH, the opportunity to provide further information about their main reasons for COVID-19 VH.
Analysis
Descriptive statistics, chi-square and bi-serial correlations for the primary variables of interest were computed and a binomial logistic regression model was performed to explore potential predictors of VH. The predictors included in the model were socio-demographical characteristics, emotions associated with the COVID-19 vaccine, and COVID-19 risk perception. Analyses were carried out using IBM SPSS (version 26) and using a .05 significance level. For responses to the qualitative, open-ended question, content analysis of participants’ comments was undertaken (see Krippendorff, Citation2018; Schreier, Citation2012). Initial descriptive codes were applied to participants’ written responses. Subsequent text was compared to previously coded text and either allocated an existing code or provided a new one, thus grouping responses by similarity (Leech & Onwuegbuzie, Citation2007). The categories of meaning (key categories) represented the highest level of abstraction for the reporting of the results. The final coded data were treated as variables for analysis conducted using descriptive statistics (frequency counts and percentages) in Microsoft Excel.
Results
Socio-demographic characteristics: The total sample comprised 1189 HSCWs who were predominately of white Scottish origin, identified as female (85.4%), aged 18 to 67 years (M = 44.09 yrs, SD = 11.48); university educated (62.71%) with an average of 16 years of respective professional experience (M = 16.83, SD = 11.02). Almost half of HSCWs worked in the NHS (46.9%) followed by a local authority (25.8%). Participants were most likely to work with adults (36%), followed by older adults (25%), people with intellectual disabilities (22%), children and families (12%), and others (5%). In terms of their self-reported health status, 4.2% of HSCWs had been advised to ‘shield’ due to underlying health conditions at the time of the study. See, for further socio-demographic characteristics.
Table 1. HSCWs’ socio-demographic data.
VH among HSCWs: At the time of data collection (December 2020-March 2021), 66.7% of HSCWs reported that they had received the COVID-19 vaccine and 10.8% had been offered it and were due to receive it. Approximately a fifth (22.4%) had not yet received it. The majority of HSCWs in the sample reported to have no hesitancies in relation to the COVID-19 vaccine (83.97%). However, a sizable portion of the sample were found to be VH (16.03%). There was no significant association between health and social care occupational groups and VH (X2 (2, N = 956) = 2.4, p = .123).
Socio-demographical characteristics and VH: Correlational analysis (see, ) showed that less years of experience, younger age and being female were factors that were associated with being VH.
Table 2. Bi-serial correlation of variables of socio-demographic and psychosocial variables and VH.
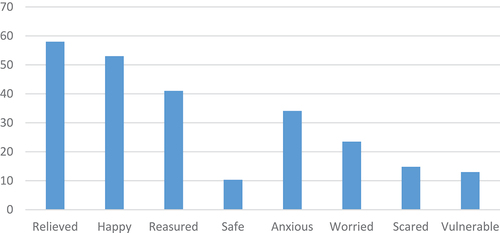
Emotions and VH: The majority of HSCWs associated positive emotions with the COVID vaccine (see, ) with over half reporting feelings of relief (58%), and happiness (53%), followed by reassurance (41%) and safety (10.3%). Conversely, approximately one third of HSCWs reported feelings of anxiety (34.1%) followed by worry (23.5%), fear (14.8%) and vulnerability (13%). Almost half of HSCWs identified only positive emotions associated with the COVID-19 vaccination (n = 49.2%) and over 15% identified only negative emotions. Over a quarter of HSCWs reported ambivalent emotions (27.83%) to the COVID-19 vaccine (see, ). Emotion was found to be associated with VH; fewer positive emotions and more negative emotions concerning the COVID-19 vaccine were associated with higher VH (see, ).
Risk perception and VH: Higher scores on COVID-19 risk perception were associated with higher HV (see, ). HSCWs who reported higher COVID-19 perceived risks tended to be younger in age and less experienced in terms of years in their working roles.
Predictors of VH: A multivariate binomial logistic regression was performed to establish whether the following variables predicted HSCWs being VH: socio-demographic variables (age, gender, education, health, years of experience; note, ethnicity was not considered due to lack of variation); emotions associated with the COVID-19 vaccine and risk perception. Years of experience was a predictor of VH; that is HSCWs with less years of experience in their working role were more likely to be VH. Positive emotion was a predictor of VH, that is HSCWs who reported positive emotions associated with the COVID-19 vaccine were less likely to be VH. Further, ambivalent emotions was a predictor of VH indicating that HSCWs who were ambivalent in the emotions they associated with the COVID-19 vaccine were more likely to be VH. The model was statistically significant, χ2(4) = 27.402, p < .0005. The model explained 8.8% (Nagelkerke R2) of the variance in VH and correctly classified 84.2% of cases (see, ).
Table 3. Regression analysis of psychosocial factors as predictors of vaccine hesitancy.
Reasons for VH: In total, 136 (71.57% of those that were VH) participants provided reasons for VH. Overall, responses generated a total of 34 associated codes (sub-codes), resulting in 10 categories of meaning (see, ). Categories of meaning (key codes) were: 1) Concerns about safety; 2) Worried about side-effects; 3) Questioning the effectiveness of COVID-19 vaccine; 4) Lack of evidence; 5) Lack of information; 6) Scaremongering; 7) Fertility concerns; 8) Natural immunity; 9) Conspiracy theories; and 10) Pressure to accept it (see, ).
Table 4. Reasons for VH: Categories of meaning (key categories) and associated codes (sub-codes).
Discussion
This study is the first in Scotland to detail factors associated with COVID-19 VH among HSCWs during the roll out of mass vaccination. In order to determine potential statistical predictors of VH, socio-demographic data were collected, along with emotions associated with the vaccine and COVID-19 risk perception. Similar to earlier work (Caiazzo & Stimpfel, Citation2022; Dror et al., Citation2020; Gadoth et al., Citation2021), the majority of HSCWs in the sample were accepting of the COVID-19 vaccine, yet a sizable proportion (one in every 6 HSCWs) were VH. No significant differences in VH were found across occupational groups, however, this may have been due to the study not having explored those who had worked directly with COVID-19 patients, as there is some evidence suggesting this may impact on VH (Dror et al., Citation2020). In terms of socio-demographic factors, lower educational attainment, less experience in their working role, being younger, being female, and being in poorer health were socio-demographical characteristics associated with VH; only less years of experience in working role was a predictor of VH. These findings are in line with earlier work (Afzal et al., Citation2022; Caiazzo & Stimpfel, Citation2022) and extend our understanding of socio-demographical factors to be considered for VH. The majority of HSCWs associated positive emotions with the COVID-19 vaccine including relief, happiness, reassurance and feelings of safety. Less positive emotions associated with the COVID-19 vaccine predicted VH among HSCWs as did ambivalent emotions. In support of previous work (Boness et al., Citation2022; Chou & Budenz, Citation2020), findings indicate that targeting and promoting positive emotions associated with the COVID-19 vaccine may be an important strategy to reduce VH among HSCWs in future public health campaigns seeking to increase uptake and reduce ambivalence. While negative emotions such as anxiety, worry, fear and vulnerability were associated with VH, they did not predict VH. These findings are in line with research focused on health communication which suggests that it is equally, if not more, important to consider positive emotions as it is negative emotions when addressing VH by activating positive emotions, such as relief (Berry et al., Citation2021; Chou & Budenz, Citation2020; Gharpure et al., Citation2021).
Qualitative data largely supported the above findings, while also contributing further insights. HSCWs’ reasons for VH included safety concerns, worries about side effects, questioning the effectiveness of COVID-19 vaccine, lack of evidence and information, indicating that they share many of the same concerns as the wider general public (L. H. Nguyen et al., Citation2022; Walsh et al., Citation2022). While a small proportion of HSCWs reported VH relating to scaremongering, fertility concerns, natural immunity, conspiracy theories and pressure to accept the vaccine, these concerns are worthy of further research, to understand their possible impact on future decisions to uptake the COVID-19 vaccine. We need to understand and combat these concerns to build trust and confidence in vaccines among HSCWs moving forward, particularly given that HSCWs may be prioritised for future booster vaccinations (Karafillakis et al., Citation2022; Shekhar et al., Citation2021; Williams, Citation2020). Such efforts may not only reduce COVID-19 VH but it is possible this may also increase acceptance of vaccines more generally (Williams, Citation2020). Providing transparent information and communication about both the benefits and potential side-effects of the vaccine, how they work, and how they have been tested is essential (Williams et al., Citation2020). In this context, addressing VH among HSCWs is particularly important. HSCWs themselves need to feel confident in the COVID-19 vaccines so that they can communicate effectively about them with the public, listening to and addressing any concerns they have (Heyerdahl et al., Citation2022).
Implications
The findings suggests that, to increase vaccine coverage in HSCWs, the role of emotion in communication strategies to address VH is crucial; this needs to be tailored to the requirements of the COVID-19 vaccine (Williams et al., Citation2020). Targeting interventions to HSCWs who are less experienced in their working roles, given they are more likely to be VH is recommended. Enhancing HSCWs’ knowledge regarding COVID-19 vaccination effectiveness could potentially increase recommendations to vaccinate and reduce their own hesitancies about the vaccine (Briggs et al., Citation2019;; Schneeberg et al., Citation2014; Toth-Manikowski et al., Citation2022). Key strengths of this study include the incorporation of both health and social care workers’ perspectives and having gained a relatively representative sample of HSCWs within Scotland. As well as quantitative data, the qualitative component largely supported and provided further insights into the factors relating to COVID-19 VH among HSCWs. It is recommended that further longitudinal research explore VH among HSCWs in the recovery phase of this pandemic and incorporate a multi-method approach to data collection in order to capture the depth and breadth of perspectives on VH and reasons for it. It is also recommended that future work explores diverse and under-represented HSCWs (e.g., ethnic minority groups, those with protected characteristics) using qualitative interviews. Further attention to broader socio-political factors that are likely to have an influence on vaccine acceptance among health and social care workers (Paudel et al., Citation2021), such as the association between political measures from the Scottish Government and vaccine uptake. This may help illuminate some of the broader social and structural barriers to vaccine uptake faced by specific groups of HSCWs.
Conclusions
The majority of HSCWs were found to be accepting of the COVID-19 vaccine during mass roll out in Scotland. However, a considerable proportion (one in every 6 HSCWs) were unsure about whether to get vaccinated, revealing the need for targeted and tailored interventions, particularly geared towards less experienced HSCWs. The promotion of positive emotions associated with the COVID-19 vaccine should be emphasised in future interventions to increase vaccine uptake and reduce ambivalent emotions, particularly among less experienced HSCWs. Greater awareness and targeted education around perceived risk and COVID-19 vaccine benefits may be required to increase vaccine coverage among HSCWs. It is hoped that our findings will influence future research and intervention development aimed at addressing vaccine coverage in HSCWs.
Acknowledgments
The research team would like to thank all the health and social care workers in Scotland that took time to engage with our study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Afzal, A., Shariff, M. A., Perez-Gutierrez, V., Khalid, A., Pili, C., Pillai, A., & Menon, V. (2022). Impact of local and demographic factors on early COVID-19. Vaccine Hesitancy among Health Care Workers in New York City Public Hospitals. Vaccines, 10(2), 273.
- Alfieri, N. L., Kusma, J. D., Heard-Garris, N., Davis, M. M., Golbeck, E., Barrera, L., & Macy, M. L. (2021). Parental COVID-19 vaccine hesitancy for children: Vulnerability in an urban hotspot. BMC Public Health, 21(1), 1–9. https://doi.org/10.1186/s12889-021-11725-5
- Arslanca, T., Fidan, C., Daggez, M., Dursun, P., & Villar, L. M. (2021). Knowledge, preventive behaviors and risk perception of the COVID-19 pandemic: A cross-sectional study in Turkish health care workers. PloS One, 16(4), e0250017. https://doi.org/10.1371/journal.pone.0250017
- Aw, J., Seah, S. S. Y., Seng, B. J. J., & Low, L. L. (2022). COVID-19-related vaccine hesitancy among community hospitals’ healthcare workers in Singapore. Vaccines, 10(4), 537. https://doi.org/10.3390/vaccines10040537
- Berry, S. D., Johnson, K. S., Myles, L., Herndon, L., Montoya, A., Fashaw, S., & Gifford, D. (2021). Lessons learned from frontline skilled nursing facility staff regarding COVID −19 vaccine hesitancy. Journal of the American Geriatrics Society, 69(5), 1140–1146. https://doi.org/10.1111/jgs.17136
- Betsch, C., Böhm, R., & Chapman, G. B. (2015). Using behavioral insights to increase vaccination policy effectiveness. Policy Insights from the Behavioral and Brain Sciences, 2(1), 61–73. https://doi.org/10.1177/2372732215600716
- Biswas, N., Mustapha, T., Khubchandani, J., & Price, J. H. (2021). The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. Journal of Community Health, 46(6), 1244–1251. https://doi.org/10.1007/s10900-021-00984-3
- Boness, C. L., Nelson, M., & Douaihy, A. B. (2022). Motivational interviewing strategies for addressing COVID-19 vaccine hesitancy. The Journal of the American Board of Family Medicine, 35(2), 420–426. https://doi.org/10.3122/jabfm.2022.02.210327
- Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing vaccination: putting psychological science into action. Psychological Science in the Public Interest, 18(3), 149–207. https://doi.org/10.1177/1529100618760521
- Briggs, L., Fronek, P., Quinn, V., & Wilde, T. Perceptions of influenza and pneumococcal vaccine uptake by older persons in Australia. Vaccine, 37(32), Epub 2019 Jul 2. PMID: 31277956, 4454–4459. https://doi.org/10.1016/j.vaccine.2019.06.079
- Butter, S., McGlinchey, E., Berry, E., & Armour, C. (2022). Psychological, social, and situational factors associated with COVID‐19 vaccination intentions: A study of UK key workers and non‐key workers. British Journal of Health Psychology, 27(1), 13–29. https://doi.org/10.1111/bjhp.12530
- Caiazzo, V., & Stimpfel, A. W. (2022). Vaccine hesitancy in American healthcare workers during the COVID-19 vaccine roll out: An integrative review. Public Health, 207, 94–104. http://doi.org/10.1016/j.puhe.2022.03.017
- Cavero, T., & Poinasamy, K. (2013). A cautionary tale: the true cost of austerity and inequality in Europe. Oxford International. https://www-cdn.oxfam.org/s3fs-public/file_attachments/cs-true-cost-austerity-inequality-uk-120913-en_0.pdf
- Chou, W. Y. S., & Budenz, A. (2020). Considering emotion in COVID-19 vaccine communication: Addressing vaccine hesitancy and fostering vaccine confidence. Health Communication, 35(14), 1718–1722. https://doi.org/10.1080/10410236.2020.1838096
- Chudasama, R. V., Khunti, K., Ekezie, W. C., Pareek, M., Zaccardi, F., Gillies, C. L., Chudasama, R. V., Seidu, S., Davies, M. J., & Chudasama, Y. V. (2022). COVID-19 vaccine uptake and hesitancy opinions from frontline health care and social care workers: Survey data from 37 countries. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 16(1), 102361. https://doi.org/10.1016/j.dsx.2021.102361
- Cipolletta, S., Andreghetti, G. R., & Mioni, G. (2022). Risk Perception towards COVID-19: A systematic review and qualitative synthesis. International Journal of Environmental Research and Public Health, 19(8), 4649. https://doi.org/10.3390/ijerph19084649
- Digregorio, M., Van Ngoc, P., Delogne, S., Meyers, E., Deschepper, E., Duysburgh, E., Scholtes, B., De Burghgraeve, T., Coen, A., De Clercq, N., Sutter, A. D., Verbakel, J. Y., Cools, P., Heytens, S., Buret, L., & Scholtes, B. (2022). Vaccine hesitancy towards the COVID-19 vaccine in a random national sample of Belgian nursing home staff members. Vaccines, 10(4), 598. https://doi.org/10.3390/vaccines10040598
- Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A., Srouji, S., & Sela, E. (2020). Vaccine hesitancy: The next challenge in the fight against COVID-19. European Journal of Epidemiology, 35(8), 775–779. https://doi.org/10.1007/s10654-020-00671-y
- Dryhurst, S., Schneider, C. R., Kerr, J., Freeman, A. L., Recchia, G., Van Der Bles, A. M., Van Der Linden, S., & van der Linden, S. (2020). Risk perceptions of COVID-19 around the world. Journal of Risk Research, 23(7–8), 994–1006. https://doi.org/10.1080/13669877.2020.1758193
- Dubé, E., Gagnon, D., MacDonald, N., Bocquier, A., Peretti-Watel, P., & Verger, P. (2018). Underlying factors impacting vaccine hesitancy in high income countries: A review of qualitative studies. Expert Review of Vaccines, 17(11), 989–1004. https://doi.org/10.1080/14760584.2018.1541406
- Dubé, E., & MacDonald, N. E. (2022). COVID-19 vaccine hesitancy. Nature Reviews. Nephrology, 18(1), 1–2. https://doi.org/10.1038/s41581-022-00571-2
- Ferrer, R. A., & Ellis, E. M. (2019). Moving beyond categorization to understand affective influences on real world health decisions. Social and Personality Psychology Compass, 13(11), 1–16. https://doi.org/10.1111/spc3.12502
- Fridman, A., Gershon, R., Gneezy, A., & Capraro, V. (2021). COVID-19 and vaccine hesitancy: A longitudinal study. PloS One, 16(4), e0250123. https://doi.org/10.1371/journal.pone.0250123
- Gabarda, A., & Butterworth, S. W. (2021). Using best practices to address COVID-19 vaccine hesitancy: The case for the motivational interviewing approach. Health Promotion Practice, 22(5), 611–615. https://doi.org/10.1177/15248399211016463
- Gadoth, A., Halbrook, M., Martin-Blais, R., Gray, A., Tobin, N. H., Ferbas, K. G., Aldrovandi, G. M., & Rimoin, A. W. (2021). Cross-sectional assessment of COVID-19 vaccine acceptance among health care workers in Los Angeles. Annals of Internal Medicine, 174(6), 882–885.
- Gatwood, J., McKnight, M., Fiscus, M., Hohmeier, K. C., & Chisholm-Burns, M. (2021). Factors influencing likelihood of COVID-19 vaccination: A survey of Tennessee adults. American Journal of Health-System Pharmacy, 78(10), 879–889. https://doi.org/10.1093/ajhp/zxab099
- Gharpure, R., Guo, A., Bishnoi, C. K., Patel, U., Gifford, D., Tippins, A., Link-Gelles, R., Shulman, E., Stone, N., Mungai, E., Bagchi, S., Bell, J., Srinivasan, A., Patel, A., & Link-Gelles, R. (2021). Early COVID-19 first-dose vaccination coverage among residents and staff members of skilled nursing facilities participating in the pharmacy partnership for long-term care program—United States. Morbidity and Mortality Weekly Report, 70(5), 178. https://doi.org/10.15585/mmwr.mm7005e2
- Goralnick, E., Kaufmann, C., & Gawande, A. A. (2021). Mass-vaccination sites—an essential innovation to curb the Covid-19 pandemic. New England Journal of Medicine, 384(18), e67. https://doi.org/10.1056/NEJMp2102535
- Heyerdahl, L. W., Dielen, S., Nguyen, T., Van Riet, C., Kattumana, T., Simas, C., & Gryseels, C. (2022). Doubt at the core: Unspoken vaccine hesitancy among healthcare workers. The Lancet Regional Health–Europe, 12, 100289. https://doi.org/10.1016/j.lanepe.2021.100289
- Holeva, V., Parlapani, E., Nikopoulou, V. A., Nouskas, I., & Diakogiannis, I. (2022). COVID-19 vaccine hesitancy in a sample of Greek adults. Psychology, Health & Medicine, 27(1), 113–119. https://doi.org/10.1080/13548506.2021.1948579
- Karafillakis, E., Dinca, I., Apfel, F., Cecconi, S., Wűrz, A., Takacs, J., Suk, J., Celentano, L. P., Kramarz, P., & Larson, H. J. (2016). Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine, 34(41), 5013–5020. https://doi.org/10.1016/j.vaccine.2016.08.029
- Karafillakis, E., Van Damme, P., Hendrickx, G., & Larson, H. J. (2022). COVID-19 in Europe: New challenges for addressing vaccine hesitancy. The Lancet, 399(10326), 699–701. https://doi.org/10.1016/S0140-6736(22)00150-7
- Kerasidou, A. (2019). Empathy and efficiency in healthcare at times of austerity. Health Care Analysis, 27(3), 171–184. https://doi.org/10.1007/s10728-019-00373-x
- Khubchandani, J., Sharma, S., Price, J. H., Wiblishauser, M. J., Sharma, M., & Webb, F. J. (2021). COVID-19 vaccination hesitancy in the United States: A rapid national assessment. Journal of Community Health, 46(2), 270–277. https://doi.org/10.1007/s10900-020-00958-x
- Kose, S., Mandiracioglu, A., Sahin, S., Kaynar, T., Karbus, O., & Ozbel, Y. (2021). Vaccine hesitancy of the COVID‐19 by health care personnel. International Journal of Clinical Practice, 75(5), e13917. https://doi.org/10.1111/ijcp.13917
- Krippendorff, K. (2018). Content analysis: An introduction to its methodology. Sage publications.
- Kwok, K. O., Li, -K.-K., Wei, W. I., Tang, A., Wong, S. Y. S., & Lee, S. S. (2021). Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. International Journal of Nursing Studies, 114(1), 103854. https://doi.org/10.1016/j.ijnurstu.2020.103854
- Lazarus, J. V., Ratzan, S. C., Palayew, A., Gostin, L. O., Larson, H. J., Rabin, K., Kimball, S., & El-Mohandes, A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27(2), 225–228. https://doi.org/10.1038/s41591-020-1124-9
- Leech, N. L., & Onwuegbuzie, A. J. (2007). An array of qualitative data analysis tools: A call for data analysis triangulation. School Psychology Quarterly, 22(4), 557.
- Leith, M. S., & Sim, D. (2020). ‘Brexit’and the Scots in England: A diaspora facing uncertainty? Scottish Affairs, 29(3), 354–369. https://doi.org/10.3366/scot.2020.0328
- Luz, P. M., Brown, H. E., & Struchiner, C. J. (2019). Disgust as an emotional driver of vaccine attitudes and uptake? A mediation analysis. Epidemiology and Infection, 147(1), e182. https://doi.org/10.1017/S0950268819000517
- MacDonald, N. E., & Dubé, E. (2015). Unpacking vaccine hesitancy among healthcare providers. EBioMedicine, 2(8), 792–793. https://doi.org/10.1016/j.ebiom.2015.06.028
- Meyer, M. N., Gjorgjieva, T., & Rosica, D. (2021). Trends in health care worker intentions to receive a COVID-19 vaccine and reasons for hesitancy. JAMA Network Open, 4(3), e215344–e215344. https://doi.org/10.1001/jamanetworkopen.2021.5344
- Murphy, J., Vallières, F., Bentall, R. P., Shevlin, M., McBride, O., Hartman, T. K., Hyland, P., Bennett, K., Mason, L., Gibson-Miller, J., Levita, L., Martinez, A. P., Stocks, T. V. A., Karatzias, T., & Hyland, P. (2021). Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature Communications, 12(1), 1–15. https://doi.org/10.1038/s41467-020-20226-9
- Nguyen, L. H., Joshi, A. D., Drew, D. A., Merino, J., Ma, W., Lo, C. H., Chan, A. T., & Marcia, M. (2022). Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nature Communications, 13(1), 1–9. https://doi.org/10.1038/s41467-021-27699-2
- Nguyen, K. H., Srivastav, A., Razzaghi, H., Williams, W., Lindley, M. C., Jorgensen, C., Abad, N., & Singleton, J. A. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States. (2021). Morbidity and Mortality Weekly Report, 70(6), 217. September and December 2020. https://doi.org/10.15585/mmwr.mm7006e3
- Paudel, S., Palaian, S., Shankar, P. R., & Subedi, N. (2021). Risk perception and hesitancy toward COVID-19 vaccination among healthcare workers and staff at a medical college in Nepal. Risk Management and Healthcare Policy, 14, 2253. https://doi.org/10.2147/RMHP.S310289
- Reiter, P. L., Pennell, M. L., & Katz, M. L. (2020). Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine, 38(42), 6500–6507. https://doi.org/10.1016/j.vaccine.2020.08.043
- Rhodes, M. E., Sundstrom, B., Ritter, E., McKeever, B. W., & McKeever, R. (2020). Preparing for a COVID-19 vaccine: A mixed methods study of vaccine hesitant parents. Journal of Health Communication, 25(10), 831–837. https://doi.org/10.1080/10810730.2021.1871986
- Sallam, M. (2021). COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines, 9(2), 160. https://doi.org/10.3390/vaccines9020160
- Schneeberg, A., Bettinger, J. A., McNeil, S., Ward, B. J., Dionne, M., Cooper, C., & Halperin, S. A. (2014). Knowledge, attitudes, beliefs and behaviours of older adults about pneumococcal immunization. A Public Health Agency of Canada/canadian Institutes of Health Research Influenza Research Network (PCIRN) Investigation. BMC Public Health, 14(1), 1–9.
- Schreier, M. (2012). Qualitative content analysis in practice. Sage publications.
- Schwarzinger, M., Watson, V., Arwidson, P., Alla, F., & Luchini, S. (2021). COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. The Lancet Public Health, 6(4), e210–e221. https://doi.org/10.1016/S2468-2667(21)00012-8
- Shekhar, R., Garg, I., Pal, S., Kottewar, S., & Sheikh, A. B. (2021). COVID-19 vaccine booster: to boost or not to boost. Infectious Disease Reports, 13(4), 924–929. https://doi.org/10.3390/idr13040084
- Shiota, M. N., Papies, E. K., Preston, S. D., & Sauter, D. A. (2021). Positive affect and behavior change. Current Opinion in Behavioral Sciences, 39(1), 222–228. https://doi.org/10.1016/j.cobeha.2021.04.022
- Sonawane, K., Troisi, C. L., & Deshmukh, A. A. (2021). COVID-19 vaccination in the UK: Addressing vaccine hesitancy. The Lancet Regional Health–Europe, 1, 100016. https://doi.org/10.1016/j.lanepe.2020.100016
- Swann, M. C., Bendetson, J., Johnson, A., Jatta, M., Schleupner, C. J., & Baffoe-Bonnie, A. (2022). Examining Drivers of COVID-19 Vaccine Hesitancy Among Healthcare Workers. Infection Control & Hospital Epidemiology, 1–9. https://doi.org/10.1017/ice.2022.34
- Tam, C. C., Qiao, S., & Li, X. (2022). Factors associated with decision making on COVID-19 vaccine acceptance among college students in South Carolina. Psychology, Health & Medicine, 27(1), 150–161. https://doi.org/10.1080/13548506.2021.1983185
- Tomljenovic, H., Bubic, A., & Erceg, N. (2020). It just doesn’t feel right–the relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychology & Health, 35(5), 538–554. https://doi.org/10.1080/08870446.2019.1673894
- Toth-Manikowski, S. M., Swirsky, E. S., Gandhi, R., & Piscitello, G. (2022). COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. American Journal of Infection Control, 50(1), 20–25. https://doi.org/10.1016/j.ajic.2021.10.004
- Troiano, G., & Nardi, A. (2021). Vaccine hesitancy in the era of COVID-19. Public Health, 194(1), 245–251. https://doi.org/10.1016/j.puhe.2021.02.025
- Vergara, R. J. D., Sarmiento, P. J. D., & Lagman, J. D. N. (2021). Building public trust: A response to COVID-19 vaccine hesitancy predicament. Journal of Public Health, 43(2), e291–e292. https://doi.org/10.1093/pubmed/fdaa282
- Verger, P., Fressard, L., Dauby, N., Dauby, N., Fasce, A., Karlsson, L., Gagneur, A., Gagneur, A., Dubé, E., & Verger, P. (2022). An instrument to measure psychosocial determinants of health care professionals’ vaccination behavior: Validation of the Pro-VC-Be questionnaire. Expert Review of Vaccines, https://doi.org/10.1080/14760584.2022.2046467
- Walsh, J. C., Comar, M., Folan, J., Williams, S., & Kola-Palmer, S. (2022). The psychological and behavioural correlates of COVID-19 vaccine hesitancy and resistance in Ireland and the UK. Acta Psychologica, 225(1), 103550. https://doi.org/10.1016/j.actpsy.2022.103550
- Williams, L. (2020). COVID vaccine: Even healthcare workers may be hesitant – But new evidence can be reassuring. The Conversation. 9 December 2020 https://theconversation.com/covid-vaccine-even-healthcare-workers-may-be-hesitant-but-new-evidence-can-be-reassuring-151404
- Williams, D. M., & Evans, D. R. (2014). Current emotion research in health behavior science. Emotion Review, 6(3), 277–287. https://doi.org/10.1177/1754073914523052
- Williams, L., Gallant, A. J., Rasmussen, S. B., Nicholls, L. A., Cogan, N., Deakin, K., Young, D., & Flowers, P. (2020). Towards intervention development to increase the uptake of COVID‐19 vaccination among those at high risk: Outlining evidence‐based and theoretically informed future intervention content. British Journal of Health Psychology, 25(4), 1039–1054. https://doi.org/10.1111/bjhp.12468
- Woolf, K., McManus, I. C., Martin, C. A., Nellums, L. B., Guyatt, A. L., Melbourne, C., Group, U. R. S. C., Gogoi, M., Wobi, F., Al-Oraibi, A., Hassan, O., Gupta, A., John, C., Tobin, M. D., Carr, S., Simpson, S., Gregary, B., Aujayeb, A., Zingwe, S., … Pareek, M. (2021). Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. The Lancet Regional Health-Europe, 9(1), 100180. https://doi.org/10.1016/j.lanepe.2021.100180
- Yıldırım, M., & Güler, A. (2020). Factor analysis of the COVID-19 Perceived Risk Scale: A preliminary study. Death Studies, 1–8. https://www.tandfonline.com/doi/full/10.1080/07481187.2020.1784311
- Yilmaz, S., Çolak, F. Ü., Yilmaz, E., Ak, R., Hökenek, N. M., & Altıntaş, M. M. (2021). Vaccine hesitancy of health-care workers: Another challenge in the fight against COVID-19 in Istanbul. Disaster Medicine and Public Health Preparedness, 1–7. https://doi.org/10.1017/dmp.2021.257
- Zheng, H., Jiang, S., & Wu, Q. (2022). Factors influencing COVID-19 vaccination intention: The roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Education and Counseling, 105(2), 277–283. https://doi.org/10.1016/j.pec.2021.09.023
- Zong, H. M., Wang, Y. J., Shi, L. L., & Wu, Y. B. (2021). The risk perception, behavior of the public and public emotional guidance under emergency of public health research. Journal of Emergency Management and Disaster Communications, 2(1), 23–37. https://doi.org/10.1142/S2689980921310023