ABSTRACT
The objective of this experiment was to offer a preliminary exploration into the key factors underlying trust in healthcare systems around the world, in light of the COVID-19 global pandemic. Participants were recruited across ten countries and were asked to complete a two-part questionnaire, in which they rated their country’s healthcare system on a scale from 1–5, according to ten trust-related factors, translated specifically to pertain to healthcare, and 4 key pillars of trust: benevolence, reliability, competence and predictability. Correlation analyses between these two separate measures revealed that honesty, consistency, and reasonableness were the most impactful factors underlying trust across the entire population. All other findings are detailed in the main text. This study allowed us to arrive at a preliminary determination of the most impactful factors underlying trust, both at a global and national level.
Introduction
Social context and importance
Falling levels of trust in public institutions have been well-documented (Hutchinson, Citation2018). Trust in healthcare providers has similarly declined in recent years, albeit at a steeper rate than other public sector institutions (White, Citation2017). From a social perspective, as trust in healthcare provision significantly impacts medical treatment adherence (Gille et al., Citation2015), the implications of trust on public health are deeply impactful.
During the outbreak of the COVID-19 pandemic, stability in trust was further disrupted. Healthcare providers’ resources were stretched thinly (Ranney et al., Citation2020), access to medical treatment became more challenging, and the number of patients in critical conditions rose dramatically (Nacoti et al., Citation2020). Amid this uncertainty, trust in healthcare fluctuated, providing an opportunity for detailed study and examination of how it develops, and conversely, how it deteriorates.
In seeking a more precise understanding of trust, it is important to offer a distinction between trust itself and trustworthiness: trust, according to Currall and Epstein (Citation2003), is partly determined by trustworthiness, in addition to other critical factors. Where trust reflects a largely desirable cognitive and affective state, trustworthiness exists as a personal character trait of an individual. In this sense, trust is partly a product or an outcome of trustworthiness, which serves to inform future trust impressions, and is justified only when the individual exhibits trustworthy behaviour. Currall and Epstein (Citation2003) also suggest that trust is often most vulnerable at points in which the magnitude of damage potentially incurred from untrustworthy behaviour is greatest (Currall & Epstein, Citation2003). Effectively, this suggests that trust is most fragile at points of high volatility and pressure. While the opportunities to improve trust are marginal, assuming trust has already been established, the possibility of trust erosion is high if expectations are not adequately met. As explored in a series of published articles, trust is a relevant factor for consideration in situations involving risk (Corazzini, Citation1977; Mayer et al., Citation1995; Slovic, Citation1993). One party in the situation must assume risk, thereby making themselves vulnerable to the trustee, and establish expectations that the trustee will affect outcomes in good faith (Rawlins, Citation2008). Merging these two ideas together, we see that the greater the amount of risk or dependence from the trustor, the greater the opportunity for failure from the trustee, triggering the subsequent erosion of trust.
In the context of the COVID-19 pandemic, feelings of anxiety and uncertainty with respect to healthcare provision across a multitude of countries (Lee, Citation2020), brings the concept of trust to the fore. Given the virus’ potentially fatal consequences, along with the sheer number of COVID-19 cases reported globally, the risk of inadequate healthcare support is heightened in light of the pandemic. The virus continues to mutate and evolve unpredictably, assuming more aggressive strains that place a greater burden on the healthcare system. As a result, trust in healthcare is currently at a fragile point, and deserves closer investigation.
Defining trust
As a multifaceted construct (Butler, Citation1991), trust cannot be viewed through a singular lens to arrive at a clear understanding of how it is impacted by crisis-related decisions. Butler (Citation1991) developed an inventory of trust-related factors, according to a series of interviews conducted with corporate executives, followed by a detailed survey-based assessment provided to employees. From these exercises, ten factors were identified as relevant pre-conditions to establishing trust. Rather than applying these conditions directly in our questionnaire, we adapted the conditions for trust to COVID-19 specifically, with the intention of testing how healthcare responses across a variety of countries affect citizens’ willingness to trust their respective healthcare systems.
Butler (Citation1991) lists availability, competence, consistency, fairness, integrity, loyalty, openness, overall trust, promise fulfilment and receptivity as the ten trust-relevant factors. In our experiment, we translated these factors into the following variables: track record, consistency, reasonableness, willingness to admit error, honesty, communication logic, sophistication and polish of communication, communication understandability, communication honesty and communication timeliness. In establishing these ten factors, we attempted to discriminate between the degrees of relevance of various factors in establishing healthcare trust, in light of the pandemic.
Surveying individuals across ten separate countries, we hoped to capture possible cultural differences across countries with respect to their relationship to trust. Simultaneously, we wanted to implicitly assess the perceived effectiveness of individual countries’ responses to the pandemic. For example, the United Kingdom was publicly noted for initially proposing a herd immunity scheme to combat the pandemic (Boseley, Citation2020), while South Korea adopted a very early track-and-trace system (McCurry, Citation2020). These divergent strategies would be expected to lead to different results and different perceptions of success and trust.
Responses were gathered from citizens across three continents (North America, Europe, and Asia) that had, to the point of data collection, suffered drastically different infection and mortality rates per capita. Overall, with the present work, we hope to help develop insight into the triggers and conditions underlying trust, while simultaneously acquiring initial impressions regarding any trust-related differences between participants in different countries.
Methods
Sample and data collection
Participants for this experiment were recruited via Prolific Academic. The conditions stipulated that participants had to be at least eighteen years of age, speak English fluently, and be a current resident of one of ten countries: United Kingdom, United States of America, Canada, Italy, Greece, Spain, Sweden, Norway, South Korea, or Japan. Our rationale for recruiting internationally was to arrive at a reasonably representative range of countries, given the range of techniques and levels of success across various countries in response to the virus. To this end, we sought approximately equal sampling per country. In total, 30 participants were recruited per country, for a total of 300 participants. Upon eliminating outliers, consisting of participants that failed to consent properly and participants whose survey completion times were more than three standard deviations above the mean (upper cut-off: 1370 seconds), we were left with 294 participants.
The average age of participants was 28.72 years of age; the youngest participant was 18, while the oldest participant was 67. The participant base consisted of 167 individuals that identified as male, 125 individuals that identified as female, and 2 who preferred not to reveal their gender identity. On average, participants took 4 minutes and 33 seconds to complete the survey. Data collection took place between 18 June 2020, and 22 June 2020.
Questionnaire development
The questionnaire was developed through Qualtrics and subsequently exported to Prolific Academic. The questionnaire was divided into two sections: the first section gathered demographic information from participants, while the second section asked participants to provide trust ratings of their respective countries’ healthcare systems’ response to COVID-19, on a scale ranging from 1–5 (1 being very poor, 5 being excellent). In the trust section, participants were initially asked to provide ratings referring to the ten trust-related factors listed in the introduction, before providing more general trust impressions relating to four pillars of trust: benevolence, reliability, competence, and predictability. In total, participants were asked to provide 14 ratings to trust-related questions.
The demographic section collected data on participants’ age, first language, gender, private health insurance status and primary country of residence during the COVID-19 pandemic.
The subsequent trust section was divided into two subsections, intended to capture both our interpretation of Butler’s (Citation1991) factors of trust inventory, within a healthcare context, as well as provide an assessment of participants’ more general impressions of their healthcare system.
Participants began by responding to ten statements relating to their country’s healthcare system’s performance in response to COVID-19 (see Appendix A). Each of the individual statements captured one of the ten trust-related factors listed in the introduction. Participants were given the general introductory statement: Please consider the following question and rate your country’s healthcare system, in response to COVID-19, on a scale ranging from 1 to 5 (1 being very poor, 5 being excellent). Participants were then asked to consider a list of ten statements, referring individually to each of the ten trust-related factors in Butler’s inventory. For example, the statement relating to track record read as follows: Track record in dealing with health-related crises. Track record is defined as all the achievements or failures that someone or something has had in the past. Based on their impressions and reflections, participants would then respond on a 1–5 scale, ranging from very poor to excellent.
Once participants responded to the ten trust-related factors, they were asked to answer four subsequent trust-related questions regarding their general impression of their country’s healthcare system’s response to COVID-19 (see Appendix B). The four statements related to four pillars of trust, which were established in previous work on trust: benevolence, reliability, competence and predictability (Baier, Citation1986; Brown et al., Citation2011; Buchman & Ho, Citation2014; Huppert et al., Citation2004; Zaheer et al., Citation1998). Participants were provided with a definition of each trust pillar and were asked to rate their country’s healthcare system generally on each of these four pillars. For example, regarding the benevolence trust pillar, participants would read: Has your country’s healthcare system been generally benevolent in providing patients with services? Benevolence is defined as easily accessible services, equal access to services across the patient population, honesty, and well-intentioned services from providers. Again, participants responded on a 1–5 scale, as above.
It is worth noting that each participant encountered the same questions in identical order. Participants were not assigned to conditions that caused their questionnaire experience to differ.
Results
General analysis
We began by allocating each of the ten trust factors to one of the four trust pillars, according to the similarity of their definitions, and the subjective appropriateness of each categorization (see, ), before running correlation analyses between the four trust pillars and, separately, correlation analyses between the ten trust factors. The results showed that the trust pillars correlated at no less than r = .699 (see, ), while the trust factors all correlated at least r = .457 (see, ). These results are encouraging because they indicate the expected consistency amongst the trust indices; it would be disconcerting to see a negative correlation between benevolence and reliability, for example, because that would indicate a lack of coherence in the trust framework. The high correlation results suggest that this model’s elements are connected and should be perceived coherently.
Table 1. Allocation of trust variables to the 4-pillared trust model.
Table 2. Broad correlation results between trust pillars.
Table 3. Broad correlation results between factors of trust.
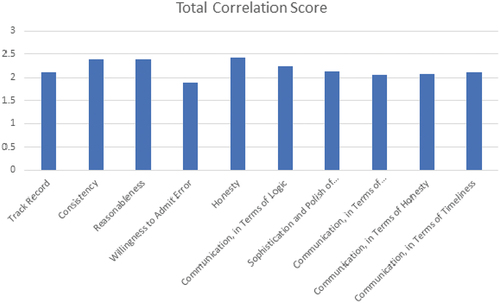
Next, a correlation analysis between the 10 trust-related factors and the four trust pillars was run. In determining the overall impact of each trust-related factor on developing trust in a healthcare system, we summed the four correlations between a trust-related factor and the four trust pillars. In doing this, we were able to develop an approximate measure of how influential each factor was in terms capturing trust, which we modelled, according to the four pillars of trust. Honesty, consistency, and reasonableness were shown to have the largest influence on trust across the entire population, according to the correlations, while willingness to admit error, communication understandability and communication honesty were the least influential factors (see, and ).
Table 4. Broad Correlation Results Between Factors of Trust and Pillars of Trust. NB. The final column adds correlations together as a heuristic index of the extent to which each factor is important in determining trust.
For the purposes of determining statistical significance when comparing participants’ factor ratings, we also converted the differences between individual country averages and the average from the remaining recruited population to Z-scores. This was done using: Zobserved = (z1 – z2)/(square root of [(1/N1 – 3) + (1/N2 – 3)] (Nefzger & Drasgow, Citation1957). From this Z-score, we could determine whether ratings towards two trust factors were reliably different, or whether ratings to an individual factor differed reliably between an individual country and the other countries sampled.
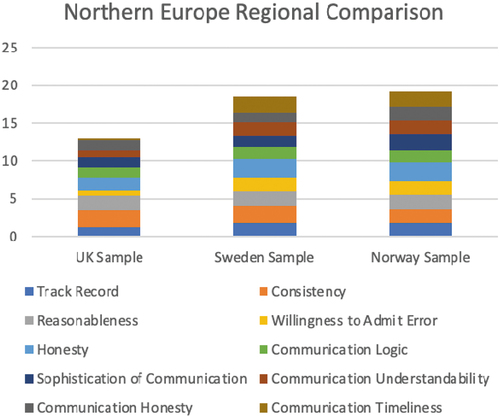
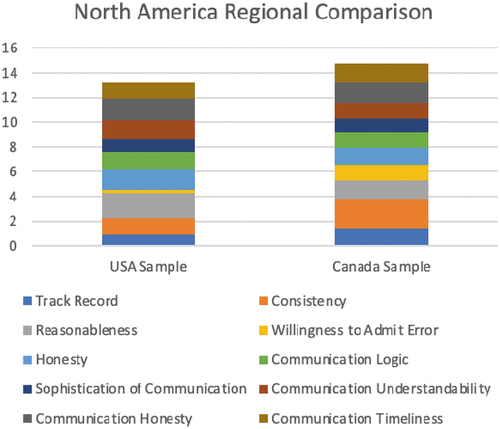
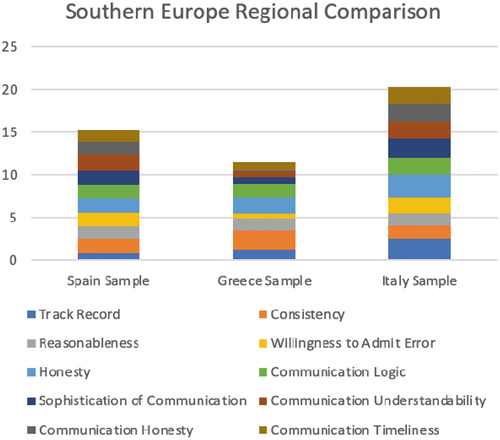
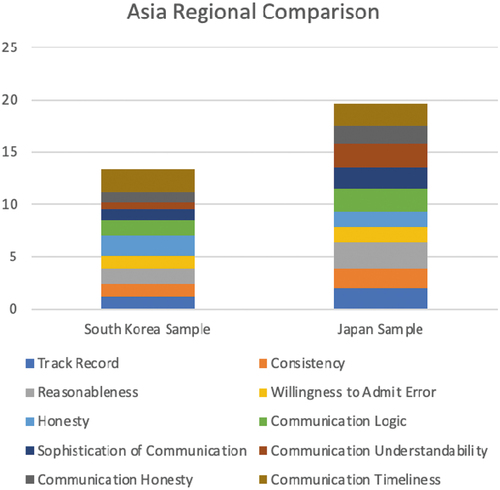
We first used this Z-score conversion approach to test whether individual countries’ factor ratings differed significantly from the global mean, which consisted of the average scores from the remaining nine countries. We then tested differences on a more local level, separating countries into four regions and comparing trust ratings between countries in these regions (see Appendices). The four regions were: Northern Europe, consisting of the UK, Sweden, and Norway (see, , , and Appendix D); North America, consisting of Canada and the United States (see, , , and Appendix C); Southern Europe, consisting of Italy, Spain, and Greece (see, , , and Appendix E); and Asia, consisting of Japan and South Korea (see, , , and Appendix F).
Table 5. Northern Europe Regional Z-Scores.
Table 6. UK Sample Correlation Results.
Table 7. Sweden Sample Correlation Results.
Table 8. Norway Sample Correlation Results.
Table 9. North American Sample Z-Score Results.
Table 10. USA Sample Correlation Results.
Table 11. Canada Sample Correlation Results.
Table 12. Southern Europe Z-Scores.
Table 13. Italy Correlation Results.
Table 14. Greece Correlation Results.
Table 15. Spain Correlation Results.
Table 16. Asia Regional Z-Scores.
Table 17. South Korea Correlation Table.
Table 18. Japan Correlation Results.
Discussion
The purpose of this experiment was to test which of the ten factors underlying trust, according to Butler’s (Citation1991) inventory, demonstrated the greatest capacity to predict trust ratings. Using the COVID-19 pandemic as a context through which trust in healthcare can be explored, we created a simple experimental structure: by asking participants to rate their healthcare system according to both the ten factors underlying trust, and according to the resulting four pillars of trust, we intended to examine both sides of the trust variable. The goal was to offer a more complete picture of the construct, both in terms of contributions and outcomes.
In doing so, as we recruited participants from 10 countries, we observed that we could indirectly make inferences about respondents’ trust relationships with their healthcare systems, across a variety of nations.
Our objective in this study was to present as close to a complete construct of trust via our 4-pillar model as could reasonably be expected. By employing Butler’s (Citation1991) inventory of trust, which ostensibly presents a complete representation of the factors underlying trust, we can conclude that the stronger the total relationships between factors of trust and trust pillars when aggregated together, the higher the general trust towards a particular healthcare system should be.
To summarize, we maintained two primary objectives in this study: to determine the most impactful factors underlying trust, and to determine levels of trust in healthcare systems across the 10 countries from which participants were recruited.
Given the large statistical output generated by this analysis, this discussion section will be devoted to patterns throughout the data that apply across the countries surveyed. While cultural norms are undoubtedly an interesting research topic, this section will refrain from engaging in any sociological or anthropological analysis of the results, focusing instead on the psychological underpinnings of trust and the primary motivators of trust, according to the empirical evidence presented. According to the statistics, we will then try to place the results in the context of our four-pillared trust model.
For interpretive purposes, we allocated each of the variables to one of the four trust pillars, according to their correlation results (see, ): track record, consistency and communication logic were allocated to the predictability pillar; reasonableness, honesty and communication honesty were allocated to the benevolence pillar; willingness to admit error and sophistication and polish in terms of communication were allocated to the reliability pillar; and communication understandability and communication timeliness were allocated to the competence pillar. Each of these individual factors will be interpreted through the specific pillar with which the factors have been allocated.
Analysing the complete collection of data before conducting a more precise examination of individual countries’ results, we observed that honesty, consistency, and reasonableness appeared to be the most influential factors driving trust. According to the four pillars of trust, honesty directly applies to the notion of ‘good faith’, suggesting it is most directly tied to the benevolence pillar, as evidenced by correlations (r = .621). Consistency, meanwhile, relates most directly to the predictability pillar (r = .661), while reasonableness, finally, can be seen as a subjective interpretation of logic and (at the intuitive level) again, given its ambiguity, is most closely related to benevolence (r = .614).
While benevolence and predictability appeared to stand out as particularly impactful in determining trust, correlations across each of the four pillars were high. Evidently, participants were concerned and affected by the multiple facets of trust and use each of the 4 pillars interconnectedly when arriving at perceptions of trust.
Limitations
While this study certainly covers a reasonably wide range of trust-related factors, it in all likelihood fails to capture trust completely. In this respect, there are likely trust-related factors that are unaccounted for that would influence participants’ willingness to trust their healthcare system. Future research with more comprehensive views of the trust-related factors is important.
Additionally, our interpretative efforts focused on geography as the major link driving international comparisons. This was done to provide a sense of how trust patterns differ, in spite of geographic proximity. Future studies comparing the incidences of COVID-19 cases in a particular country, as well as the mortality rate of one country against another, may have additional relevance. It is also worth noting that the small samples we were able to recruit across different countries certainly bear on the conclusions we can draw from this project. It is entirely possible that any conclusions concerning a particular country reflect idiosyncrasies of the sample, rather than corresponding national attitudes. What we hope the present work does contribute is a robust methodology regarding trust, which can effectively be adapted to sampling across multiple countries, in addition to some preliminary findings about national differences, which could serve to motivate future extensions of this work.
Finally, it is worth again reemphasizing that this data was collected between the first and second waves of the pandemic, and accordingly reflects impressions and perceptions of trust in health systems across the world at a specific point in time. Given the widespread impact of the pandemic on the broad functional nature of health systems, on individual relationships and perceptions of trust, and a variety of other social, political, and macroscopic developments over the past two years, additional research studying the primary underpinnings of trust today would be a valuable extension to this current work.
Supplemental Material
Download MS Word (47.5 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/13548506.2022.2141807
Additional information
Funding
References
- Baier, A. 1986. Trust and antitrust. Ethics 96: 231–260. https://www.jstor.org/stable/pdf/2381376.pdf 2
- Boseley, S. (2020). Herd immunity: Will the UK’s coronavirus strategy work? | world news | The Guardian. The Guardian. https://www.theguardian.com/world/2020/mar/13/herd-immunity-will-the-uks-coronavirus-strategy-work
- Brown, P. R., Alaszewski, A., Swift, T., & Nordin, A. (2011). Actions speak louder than words: The embodiment of trust by healthcare professionals in gynae-oncology. Sociology of Health & Illness, 33(2), 280–295. https://doi.org/10.1111/j.1467-9566.2010.01284.x
- Buchman, D. Z., & Ho, A. (2014). What’s trust got to do with it? Revisiting opioid contracts. Journal of Medical Ethics, 40(10), 673–677. https://doi.org/10.2307/43283152
- Butler, J. K. J. (1991). Toward understanding and measuring conditions of trust: Evolution of a conditions of trust inventory. Journal of Management, 17(3), 643–663. https://doi.org/10.1177/014920639101700307
- Corazzini, J. G. (1977). Trust as a complex multi-dimensional construct. Psychological Reports, 40(1), 75–80. https://doi.org/10.2466/pr0.1977.40.1.75
- Currall, S. C., & Epstein, M. J. (2003). Lessons from the rise and fall of enron. Organizational Dynamics, 32(2), 193–206. https://doi.org/10.1016/S0090-2616(03)00018-4
- Gille, F., Smith, S., & Mays, N. (2015). Why public trust in health care systems matters and deserves greater research attention. Journal of Health Services Research & Policy, 20(1), 62–64. https://doi.org/10.1177/1355819614543161
- Huppert, F. A., Baylis, N., Huppert, F. A., Baylis, N., & Keverne, B. (2004). Well-being: Towards an integration of psychology, neurobiology and social science. Philosophical Transactions of the Royal Society B: Biological Sciences, 359(1449), 1447–1451. https://doi.org/10.1098/rstb.2004.1520
- Hutchinson, M. (2018). The crisis of public trust in governance and institutions: Implications for nursing leadership. Journal of Nursing Management, 26(2), 83–85. https://doi.org/10.1111/jonm.12625
- Lee, S. A. (2020). Coronavirus anxiety scale: A brief mental health screener for COVID-19 related anxiety. Death Studies, 44(7), 393–401. https://doi.org/10.1080/07481187.2020.1748481
- Mayer, R. C., Davis, J. H., & Schoorman, F. D. (1995). An integrative model of organizational trust. The Academy of Management Review, 20(3), 709. https://doi.org/10.2307/258792
- McCurry, J. (2020). Test, trace, contain: How South Korea flattened its coronavirus curve | world news | The Guardian. The Guardian. https://www.theguardian.com/world/2020/apr/23/test-trace-contain-how-south-korea-flattened-its-coronavirus-curve
- Nacoti, M., Ciocca, A., Giupponi, A., Brambillasca, P., Lussana, F., Pisano, M., … Montaguti, C. (2020). At the epicenter of the covid-19 pandemic and humanitarian crises in Italy: Changing perspectives on preparation and mitigation. NEJM Catalyst: Innovations in Care Delivery. https://doi.org/10.1056/CAT.20.0080
- Nefzger, M. D., & Drasgow, J. 1957. The needless assumption of normality in pearson’s r. American Psychologist 12: 623–625. http://0-web.a.ebscohost.com.wam.city.ac.uk/ehost/pdfviewer/pdfviewer?vid=2&sid=16eef70c-3519-40b5-a104-ee2de3c1eeb3%40sdc-v-sessmgr02 10
- Ranney, M. L., Griffeth, V., & Jha, A. K. (2020). Critical supply shortages - The need for ventilators and personal protective equipment during the Covid-19 pandemic. New England Journal of Medicine. Massachussetts Medical Society, 382(18), e41. https://doi.org/10.1056/NEJMp2006141
- Rawlins, B. L. (2008). Measuring the relationship between organizational transparency and employee trust. Public Relations Journal, 2(2), 1–21. http://scholarsarchive.byu.edu/facpub
- Slovic, P. (1993). Perceived risk. Trust, and Democracy.
- White, K. (2017). Trust in healthcare: Making progress. Edelman. Retrieved May 5, 2018, from https://www.edelman.com/post/trust-healthcare-making-progress
- Zaheer, A., McEvily, B., & Perrone, V. (1998). Does trust matter? Exploring the effects of interorganizational and interpersonal trust on performance. Organization Science, 9(2), 141–159. INFORMS. https://doi.org/10.2307/2640350