ABSTRACT
The simple act of informing patients about side-effects increases the likelihood they will experience them (i.e. the nocebo effect). Explaining this psychological phenomenon could help to reduce side-effect experience, however, it is yet to be explored if this can be applied to clinical settings where new medication is prescribed. In addition, the degree to which a health-care provider empathetically communicates this to patients may have an impact. To investigate this, we carried out 2 × 2 factorial trial to assess the effect of nocebo explanation and empathy (plus their interaction) on side-effect expectations following a fictional GP consultation prescribing a new medication. Overall, 208 participants were randomised to watch one of the four fictive GP consultations and play the role of the patient. In all videos, participants received information about the reason for the consultation, the recommendation of a new fictive medicine, how to take it, benefits and side-effects. The videos differed in whether the GP provided an explanation of the nocebo effect (yes/no) and whether they communicated in an empathetic style (yes/no). After watching the video, participants were asked about their side-effect expectations and rated the quality of the GP’s communication. Two-way ANOVAs revealed no main effect of nocebo explanation on expectation of side-effects warned or not warned about in the consultation. However, there was a main effect of empathy, with participants watching the empathetic consultations having significantly lower expectations of non-warned-about side-effects. There was no significant interaction. Findings suggest that explaining the nocebo effect and GP empathy did little to allay expectations of side-effects that were specifically mentioned in the consultation. However, GP empathy had an effect by helping to reduce additional side-effect expectations participants still had. Future work should extend these findings to real GP consultations where the full dimensions of empathy can be explored.
Introduction
Around 50% of the patients do not adhere to their medication as prescribed (Kleinsinger, Citation2018), adding costs to health services due to the implications for patient health, wasted medication and General Practitioner (GP) visits/hospitalisations (Cutler et al., Citation2018). One of the reasons patients give for not adhering to their medication is a fear of side-effects (Horne, Chapman, et al., Citation2013; Kardas et al., Citation2013). Expectations of side‐effects have been found to be associated with lower medication adherence intentions (Heisig et al., Citation2015) and can lead to the direct experience of side-effects through the nocebo effect, a psychological phenomenon whereby the simple act of informing patients about potential side-effects makes it more likely for them to develop (Barsky et al., Citation2002). This is because negative expectations make patients more likely to attend to new or changed sensations and to (mis)attribute them to their medication (Barsky et al., Citation2002). The experience of side-effects due to negative expectations may occur through perceptual biases, for example people may notice signs that they would have otherwise ignored but that would have occurred anyway (Ross & Olson, 1981). Or it may occur through a response bias, for example, expectations might lower the criterion for labelling a symptom as a side-effect without altering the recipient’s symptom experience (Clark, 1969).
Side-effect expectations can be generated through a variety of sources including patient information leaflets, media reporting and discussion with friends, family and health-care providers (HCPs) (Petrie & Rief, Citation2019). Withholding side-effect information is one way to reduce side-effect expectations and therefore nocebo-induced side-effects (Webster et al., Citation2016). However, this raises important ethical considerations as it does not uphold informed consent or patient autonomy (Cohen, Citation2014). One potential resolution is the use of positive framing whereby the number of people who remain side-effect free is communicated. A review of six studies investigating the use of positive framing to reduce nocebo effects found that all but one study showed a significant framing effect on either side-effect experience, attribution or expectation (Barnes et al., Citation2019). However, positive framing has only been shown to reduce expectations and side-effect experience of those side-effects specifically mentioned (Webster & Rubin, Citation2021; Webster et al., Citation2018). Around 30% of the participants still expect side-effects that have not been warned about (Webster & Rubin, Citation2021). Such alternative methods are needed to help reduce expectations and nocebo-induced side-effects across the board.
One such alternative is to inform patients about the nocebo effect. For example, if people are aware that contextual and psychological factors may cause the experience and exacerbation of symptoms, then they may be less inclined to misattribute symptoms to a new medicine. In addition, explaining why these symptoms occur may remove attention towards them and reduce side-effect expectations (Pan et al., Citation2019). This is supported by two studies which have shown that videos informing participants about the nocebo effect can reduce side-effect reporting to sham infrasound (Crichton & Petrie, Citation2015) and a sham medicine (MacKrill et al., Citation2021). Moreover, MacKrill et al. (Citation2021) have found that explaining the nocebo effect reassures participants and could be useful in reducing side-effect expectations for both warned and non-warned side-effects. There were, however, some limitations as the comparison videos differed on more than one contextual factor, and therefore the study intervention was not a pure comparison of the effect of the nocebo explanation. In addition, the intervention was delivered through an animated video designed to mitigate the influence of negative medication media coverage. There is a need to apply this in a routine clinical setting and solely examine the effects of HCPs explaining the nocebo effect when prescribing patients new medicines to address these shortcomings in the current literature.
However, it is important to appreciate that the patient–HCP relationship can be therapeutic in itself, and such therapeutic alliances are often characterized by HCP empathy (Kornhaber et al., Citation2016). There are four dimensions of empathy; affective (the sensations and feeling that someone gets in response to other’s emotions); moral (internal motivation to empathize); cognitive (the ability to identify and understand others’ perspectives) and behavioural (action-oriented process based on affective and cognitive empathy which is directly oriented to enhance clinical outcome, e.g. making a plan of action and non-verbal facial expression, voice tone, eye contact and posture) (Stepien & Baernstein, Citation2006). HCPs who express empathy foster positive expectations in patients and therefore achieve more effective treatment outcomes than those who communicate more formally without any form of reassurance (Manaï et al., Citation2019). For example, in a classic study by Kaptchuk et al. (Citation2008) patients with irritable bowel syndrome who received empathetic interactions from a HCP while receiving placebo treatment showed greatest improvement compared to those patients who received formal interactions which lacked warmth.
These effects of HCP empathy can also be seen to reduce nocebo effects. For example, Howe et al. (Citation2017) used a histamine skin prick test to induce allergic reactions in participants, who were then provided with an inert cream and instructions to expect either alleviation or worsening of the reaction. At the same time, the HCP administering the treatment was instructed to display either high or low warmth and high or low competence. They found that the impact of expectation was mediated by HCP warmth and competence. Positive expectations accompanied by warmth and competence correlated with the smallest wheal size, and these effects were reversed when the cream was given with low-warmth and competence. More recently, Necka et al. (Citation2021) studied the effect of HCPs facial expressions on pain analgesia following hypothetical painful procedures and found that perceived competence and warmth of the HCP based on their facial expression alone predicted patients’ expectations about post-procedure pain.
As such, not only can negative information itself lead to nocebo effects, the way this information is communicated can also exacerbate these effects. This is especially important for HCPs such as GPs who have direct patient contact, as merely seeing them could elicit nocebo effects (Manaï et al., Citation2019). GPs are often the first port of call for patients and issue a prescription in around two-thirds of their consultations (Duerden et al., Citation2011). Whether the beneficial effects of empathic HCP communication can be applied to reducing nocebo effects to medications prescribed in GP consultations is an important consideration.
To explore the potential for explaining the nocebo effect and HCP empathy to reduce nocebo effects on newly prescribed medications, we carried out a 2 × 2 factorial trial to investigate the main effect of nocebo explanation and empathy (plus their interaction) on side-effect expectations following a fictional GP consultation prescribing a new medication. We hypothesized that the nocebo explanation and HCP empathy would significantly reduce expectations of side-effects that were warned about in the consultation, as well as those not warned about. In addition, we hypothesized that there would be a significant interaction between these two variables with the nocebo explanation accompanied by empathy being the most effective in reducing side-effect expectations.
Methods
Design
A 2 × 2 factorial double-blind randomisation-controlled trial was conducted online. The study was approved by the King’s College London ethics committee (Reference Number: MRSU-19/20–17973).
Participants
Participants were recruited through online adverts on university circular emails, social media and volunteering websites. Participants were eligible to take part if they were aged at least 18 and fluent in English. An estimated sample size of 204 was calculated using G*Power (version 3.1.9.4) on the ability to detect a small-medium effect size (f = 0.20), at 80% power and alpha of p < .05 for a main effects/interaction ANOVA.
Procedure
Study adverts included a link to the study page with the information sheet. This informed participants to play the role of a patient who was experiencing tension-type headaches, and their current medication was not working. It was explained to participants that they would watch one of the four videos depicting a fictitious consultation where they would be prescribed a new fictional medication and that afterwards they would be asked their views regarding the quality of the GP’s communication, and beliefs about the medication being prescribed. Participants were told that the communication style would vary between the four videos, but they did not know how it would vary, or which one they would be allocated to.
After reading the information sheet, participants gave their consent and completed the eligibility check. Those that did not consent or who were ineligible were thanked for their interest and exited from the study. The remaining participants completed questions regarding their demographics and perceived sensitivity to medicines before being randomly allocated to one of the four video conditions. Randomisation was carried out by the QualtricsXM program which hosted the study, using simple randomization (1:1:1:1). A timer was placed on the videos to prevent participants skipping the video before it had finished. After watching the video, participants were asked about their side-effect expectations and rated the quality of the GP’s communication. Attention checks were included throughout the study to verify participant’s attention. Participants who failed these were excluded from the study. At the end of the study, participants were debriefed and could enter a prize draw for £50 Amazon vouchers. The study took an average of 7 min to complete.
Materials
GP consultation videos
The videos were recorded using a Sony Cyber-short HX200V camera and uploaded to Qualtrics. The video setting was organised to represent a GP’s office. The desk was oriented towards a white wall surrounded by medical books, a calendar and paperwork. The GP (female) was wearing a white shirt, and a stethoscope was visible either around her neck or on the desk. In all videos, participants received information about the reason for the consultation, the recommendation of a new fictive medicine, how to take it, benefits and side-effects. The three potential side-effects discussed were nausea, dizziness and fatigue. The videos varied in length from 3 to 5 min and could only be played once. The videos differed in whether the GP explained the nocebo effect (yes/no) and whether they communicated in an empathetic style (yes/no). The script and contextual factors of the videos were discussed with the research team until they were approved (see supplementary material) and are briefly described below.
Nocebo explanation
Similar to previous nocebo explanation interventions (Crichton & Petrie, Citation2015; MacKrill et al., Citation2021; Pan et al., Citation2019), in videos 1 and 3, the nocebo effect was explained by comparing it to the more well-known placebo effect, explaining the potential for people to attribute any new symptoms to a new medication and giving a real-life example of the nocebo effect in action for participants to relate to. Videos 2 and 4 only communicated information about the potential for unpleasant side-effects.
Empathetic communication
Videos 1 and 2 conveyed an empathetic style of communication on a moral and behavioural level. Affective and cognitive empathy could not be adequately demonstrated through this format. Moral empathy was demonstrated by showing reassurance towards the participant and asking questions (e.g. ‘Do you know what nocebo effect is?’, ‘Do you have more questions?’, etc.). Behavioural empathy was demonstrated by non-verbal behaviour such as eye contact, adjusted facial expression, open posture in the direction of the camera, talking in terms of ‘we’ and use of a gentle tone of voice. In videos 3 and 4, the GP acted in a more cold and disinterested manner, made less eye contact, sat in a closed and non-camera orientated posture, talked in terms of ‘I’, gave no reassurance and did not ask any questions.
Measures
Control variables
Participants were asked demographic questions regarding their age, gender, ethnicity, level of education, and employment status. Their perceived sensitivity to medicines was measured using the perceived sensitivity to medicines Scale (Horne, Faasse, et al., Citation2013), a 5-item questionnaire rated on a 5-point scale from 1 ‘strongly disagree’ to 5 ‘strongly agree’. Scores range from 5 to 25 with higher scores indicating a greater sensitivity (α = 0.89).
Side-effect expectations
The outcome of side-effect expectations was measured using a six-item scale that represented the six most common nocebo reported side-effects (Wells & Kaptchuk, Citation2012). Of these, three were side-effects that were mentioned in the videos; nausea, dizziness and fatigue, and three were side-effects that were not mentioned in the videos; dry mouth, skin rash, and muscle pain. The selection of side-effects was chosen to resemble a real-life GP’s consultation where the GP may only discuss a few key side-effects. Participants were asked to state how likely they think they would experience each side-effect whilst taking the fictive drug, rated on a 5-point scale from 1 ‘very unlikely’ to 5 ‘very likely’.
Empathy manipulation check
To check that the empathy manipulation worked, we measured the quality of the GP’s empathetic communication through the Consultation and Relational Empathy (CARE) questionnaire (Mercer et al., Citation2004). This is a 10-item questionnaire assessing moral, cognitive, affective and behavioural empathy rated on a 5-point scale from 1 ‘Poor’ to 5 ‘Excellent’. For our study, we selected five items which applied most to our study, as our empathy manipulation was limited to behavioural and moral empathy. These included the items ‘Making you feel at ease’, ‘Explaining things clearly’, ‘Making a plan of action for you’, ‘Showing care and compassion’ and ‘Being positive’. Scores ranged from 5 to 25 with higher scores, indicating better empathetic communication (α = 0.90).
Attention check
During the study, we used three questions to check participants had paid attention to the video consultations. These were ‘Can Parosin be taken during pregnancy? (Yes)’, ‘Is reducing fever a benefit of Parosin? (No)’ and ‘Parosin are small white round pills? (Yes)’. During the side-effect expectation and empathy measures, we also included two items that asked participants to select a certain response option. Those who failed the attention checks were withdrawn from the study.
Statistical analysis
All data were analysed using SPSS version 26. Responses of ‘Prefer not to say’ and ‘don’t know’ were treated as missing data and excluded from the analyses. Chi-square and Fisher exact tests were carried out to analyse any differences in the distribution of gender, ethnicity, education level and employment status by experimental condition. One-way ANOVAs were used to assess any baseline differences in age or perceived sensitivity to medicine. To check if empathy manipulation had worked, we carried out a one-way ANOVA to compare the differences in mean empathy scores between the four experimental conditions. A significant result was followed up with post hoc multiple-comparison tests using the Bonferroni correction. To assess the main effect of the nocebo explanation, empathetic communication and their interaction on expectations of mentioned and non-mentioned side-effects we carried out two-way ANOVAs, whilst controlling for perceived sensitivity to medicine which was correlated with side-effect expectations.
Results
Participant characteristics
Participants were recruited from 17 April 2020, to 24 June 2020. A final sample of 208 participants took part in the study (see for participant flow through the study). The mean age of the participants was 30.63 years (SD = 12.15). Most of the participants were female (72.9%), White (79.1%) and had achieved a higher education qualification (79.5%). A similar proportion of participants were currently students in full-time education (44.2%) or employed (44.7%). Mean ratings on the perceived sensitivity to medicines scale were relatively low (M = 11.61). For full participant characteristics and break down between the four video conditions see . There was no difference in the distribution of participant characteristics between the four conditions, p > .176.
Table 1. Baseline Characteristics of Participants.
Empathy manipulation check
There was a significant difference in the empathy ratings between the conditions, F(3, 204) = 45.543, p < .001. Post hoc multiple-comparison tests using Bonferroni showed that the Empathy and Nocebo (M = 18.35, SD = 4.56) and Empathy only (M = 17.46, SD = 4.52) consultations were rated significantly higher in empathy than the Nocebo only (M = 10.96, SD = 4.34) and no Nocebo or Empathy (M = 10.84, SD = 3.89) consultations (p < .001). There was no significant difference in scores between the two empathetic consultations themselves (p = .299), or the two non-empathetic consultations (p = .889).
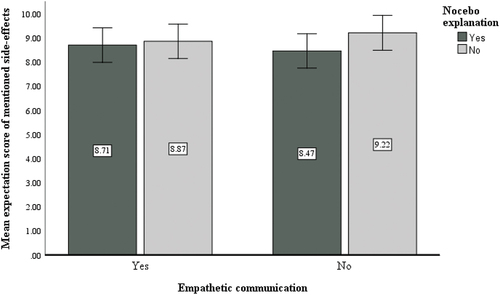
Expectations of side-effects mentioned in the video consultations
Mean expectation scores of mentioned side-effects were similar between the four conditions (see ). Results showed that there was no main effect of empathetic communication, F(1,203) = .022, p = .881; nocebo explanation, F(1,203) = 1.558, p = .213; or an interaction effect between these two conditions, F(1,203) = .671, p = .414 on side-effect expectation scores.
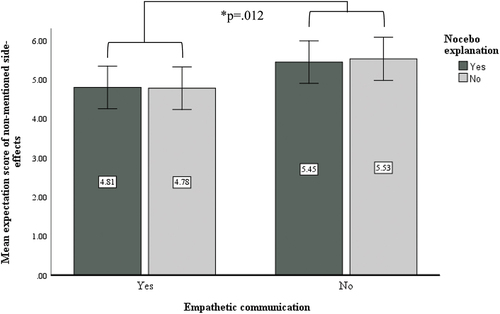
Expectations of side-effects not mentioned in the video consultations
Mean expectations scores of non-mentioned side-effects are shown in . Results showed there was a significant main effect of empathetic communication, F(1,203) = 6.360, p = .012. Participants who were randomised to the empathetic consultations had significantly lower expectations of non-mentioned side-effects (M = 4.80) than those who watched the non-empathetic consultations (M = 5.49). There was no main effect of nocebo explanation, F(1,203) = .012, p = .912 or an interaction effect between the nocebo explanation and empathetic communication, F(1,203) = .035, p = .851 on side-effect expectation scores.
Discussion
We carried out 2 × 2 factorial trial to assess the potential for nocebo explanation and empathy (plus their interaction) to reduce side-effect expectations following a fictional GP consultation prescribing a new medication.
Explaining the nocebo effect had no effect on expectations of side-effects that were warned or not warned about in the consultation. This could be because side-effect information (from a trusted source) was included alongside this explanation (as would be expected in GP consultations) and therefore likely fresh in participants’ minds contributing towards a recency bias. In addition, our nocebo explanation may not have been as reassuring or in-depth as that portrayed via the medium of video by Crichton and Petrie (Citation2015) and MacKrill et al. (Citation2021). It is difficult to include this level of verbal and visual information in time-limited consultations with a lack of available visual aids, and this could limit the effectiveness of such interventions in these settings. Alternatively, perhaps the nocebo explanation works by reducing the misattribution mechanism, by encouraging patients to evaluate their attributions when they experience symptoms, rather than altering expectations themselves (which is what we measured). As such, they might still expect symptoms but upon experiencing them attribute them to another cause. This is supported by Pan et al. (Citation2019) who found that explaining the nocebo effect via a leaflet reduced side-effect reporting to a sham headache medicine, but only marginally altered expectations. Understanding the mechanisms through which explaining the nocebo effect can help to reduce side-effect experience is important.
We found no effect of empathy manipulation on expectation of side-effects that had been warned about, however it did reduce expectations of side-effects that had not been communicated in the consultation. It may be that when side-effect risk is directly communicated, it matters more ‘what’ is said rather than ‘how’ it is. Whereas, when side-effect information is not communicated, empathy may help to reassure and reduce expectations of side-effects as a whole. Again, however, because of the timing of measuring expectations, the communicated side-effect information was still easy to recall. It would be interesting to extend these findings to real GP consultations to see if the effects of empathy come into play later when patients have had the opportunity to reflect on consultations.
We know that HCP empathy reduces patient anxiety and leads to significantly better clinical outcomes (Derksen et al., Citation2013). Here, we show that this could be partially explained by helping to reduce nocebo effects to prescribed medications. With calls for GP surgeries to still offer remote consultations after the pandemic (RCGP, Citation2021), it is important to understand the effect this has on HCPs ability to demonstrate empathy and the potential knock-on implications this could have on patients’ health. It is also important to note that there are racial/ethnic group disparities in patients’ perceived quality of care from HCPs and perceived racial/ethnic discrimination at least partly underlies this relationship (Benjamins et al., Citation2019). It is possible that a lack of empathy shown by HCPs in such situations may be contributing to health inequalities in BAME groups through the nocebo effect.
There are some limitations to be considered with this work. First, the study was based on a fictitious scenario, and whether these findings can be generalised to real GP consultations’ and patients’ actual experience to newly prescribed medication needs to be assessed. For example, the dependent variable only considers expectation, not the real feeling surrounding actual medication taking behaviour, which may be less impacted by the nocebo effect explanation. Second, the majority of our sample were young, White, well-educated women and therefore not representative of the demographics of the population that most commonly seek medical care. Third, although our empathy manipulation was successful, it only altered the behavioural and moral aspects of empathy and was delivered online. It is possible that empathy manipulations involving affective and cognitive aspects, and which are delivered through human interaction may more strongly impact side-effect expectations. Fourth, our study did not include a manipulation check of the nocebo effect explanation to see if participants understood and believed in the existence of the nocebo effect as this would have inadvertently prompted all participants about the nocebo effect, potentially confounding the results. As such we cannot be certain if this manipulation was successful. Finally, the gender of observers or providers can impact the experience of nocebo effects in pain (Aslaksen et al., Citation2007). As our study only portrayed a female HCP, and the majority of participants matched this gender, it is possible that we may not find the same effect of empathy for male participants. We could not reliably assess this in our data due to the lack of balance in gender of participants and a limited sample size to carry out such tests of interaction. In addition, as female HCPs are often thought of as being more empathetic than their male counterparts (Howick et al., Citation2017), these findings may not translate to male HCPs. It is important that the effect of HCP’s gender and whether this matches patients’ gender on nocebo responses to prescribed medicines are investigated further.
Conclusion
Explaining the nocebo effect and GP empathy did little to allay expectations of side-effects that were specifically mentioned in the consultation. However, GP empathy had an effect beyond this, helping to reduce additional side-effect expectations that participants had. Future work should extend these findings to real GP consultations with more representative populations where the full dimensions of empathy and patient/provider gender can be explored.
Acknowledgments
This study was funded by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between Public Health England, King’s College London and the University of East Anglia. The views expressed are those of the author(s) and not necessarily those of the NIHR, Public Health England or the Department of Health and Social Care.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Aslaksen, P. M., Myrbakk, I. N., Høifødt, R. S., & Flaten, M. A. (2007). The effect of experimenter gender on autonomic and subjective responses to pain stimuli. Pain, 129(3), 260–268. https://doi.org/10.1016/j.pain.2006.10.011
- Barnes, K., Faasse, K., Geers, A. L., Helfer, S. G., Sharpe, L., Colloca, L., & Colagiuri, B. (2019). Can positive framing reduce nocebo side effects? current evidence and recommendation for future research. Frontiers in Pharmacology, 10, 167–167. https://doi.org/10.3389/fphar.2019.00167
- Barsky, A. J., Saintfort, R., Rogers, M. P., & Borus, J. F. (2002). Nonspecific medication side effects and the nocebo phenomenon. Journal of the American Medical Association, 287(5), 622–627. https://doi.org/10.1001/jama.287.5.622
- Benjamins, M. R., Middleton, M., & Koniaris, L. G. (2019). Perceived discrimination in medical settings and perceived quality of care: A population-based study in Chicago. PloS One, 14(4), e0215976. https://doi.org/10.1371/journal.pone.0215976
- Cohen, S. (2014). The nocebo effect of informed consent. Bioethics, 28(3), 147–154. https://doi.org/10.1111/j.1467-8519.2012.01983.x
- Crichton, F., & Petrie, K. J. (2015). Health complaints and wind turbines: The efficacy of explaining the nocebo response to reduce symptom reporting. Environmental Research, 140, 449–455. https://doi.org/10.1016/j.envres.2015.04.016
- Cutler, R. L., Fernandez-Llimos, F., Frommer, M., Benrimoj, C., & Garcia-Cardenas, V. (2018). Economic impact of medication non-adherence by disease groups: A systematic review. BMJ Open, 8(1), e016982. https://doi.org/10.1136/bmjopen-2017-016982
- Derksen, F., Bensing, J., & Lagro-Janssen, A. (2013). Effectiveness of empathy in general practice: A systematic review. British Journal of General Practice, 63(606), e76–84. https://doi.org/10.3399/bjgp13X660814
- Duerden, M., Avery, T., Millson, D., & Smart, S. (2011). Quality of GP Prescribing. King’s Fund Report, March 2011.
- Heisig, S. R., Shedden Mora, M. C., Hidalgo, P., & Nestoriuc, Y. (2015). Framing and personalizing informed consent to prevent negative expectations: An experimental pilot study. Health Psychology, 34(10), 1033–1037. https://doi.org/10.1037/hea0000217
- Horne, R., Chapman, S. C. E., Parham, R., Freemantle, N., Forbes, A., Cooper, V., & Xia, Y. (2013). Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PloS One, 8(12), e80633. https://doi.org/10.1371/journal.pone.0080633
- Horne, R., Faasse, K., Cooper, V., Diefenbach, M. A., Leventhal, H., E, L., & Petrie, K. J. (2013). The perceived sensitivity to medicines (PSM) scale: An evaluation of validity and reliability. British Journal of Health Psychology, 18(1), 18–30. https://doi.org/10.1111/j.2044-8287.2012.02071.x
- Howe, L. C., Goyer, J. P., & Crum, A. J. (2017). Harnessing the placebo effect: Exploring the influence of physician characteristics on placebo response. Health Psychology, 36(11), 1074–1082. https://doi.org/10.1037/hea0000499
- Howick, J., Steinkopf, L., Ulyte, A., Roberts, N., & Meissner, K. (2017). How empathic is your healthcare practitioner? A systematic review and meta-analysis of patient surveys. BMC Medical Education, 17(1), 136. https://doi.org/10.1186/s12909-017-0967-3
- Kaptchuk, T. J., Kelley, J. M., Conboy, L. A., Davis, R. B., Kerr, C. E., Jacobson, E. E., Kirsch, I., Schyner, R. N., Nam, B. H., Nguyen, L. T., Park, M., Rivers, A. L., McManus, C., Kokkotou, E., Drossman, D. A., Goldman, P., & Lembo, A. J. (2008). Components of placebo effect: Randomised controlled trial in patients with irritable bowel syndrome. BMJ, 336(7651), 999–1003. https://doi.org/10.1136/bmj.39524.439618.25
- Kardas, P., Lewek, P., & Matyjaszczyk, M. (2013). Determinants of patient adherence: A review of systematic reviews. Frontiers in Pharmacology, 4, 91. https://doi.org/10.3389/fphar.2013.00091
- Kleinsinger, F. (2018). The unmet challenge of medication nonadherence. The Permanente Journal, 22(3), 18–033. https://doi.org/10.7812/tpp/18-033
- Kornhaber, R., Walsh, K., Duff, J., & Walker, K. (2016). Enhancing adult therapeutic interpersonal relationships in the acute health care setting: An integrative review. Journal of Multidisciplinary Healthcare, 9, 537–546. https://doi.org/10.2147/JMDH.S116957
- MacKrill, K., Morrison, Z., & Petrie, K. J. (2021). Increasing and dampening the nocebo response following medicine-taking: A randomised controlled trial. Journal of Psychosomatic Research, 150, 110630. https://doi.org/10.1016/j.jpsychores.2021.110630
- Manaï, M., van Middendorp, H., Veldhuijzen, D. S., Huizinga, T. W. J., & Evers, A. W. M. (2019). How to prevent, minimize, or extinguish nocebo effects in pain: A narrative review on mechanisms, predictors, and interventions. Pain Reports, 4(3), e699–e699. https://doi.org/10.1097/PR9.0000000000000699
- Mercer, S. W., Maxwell, M., Heaney, D., & Watt, G. C. (2004). The consultation and relational empathy (CARE) measure: Development and preliminary validation and reliability of an empathy-based consultation process measure. Family Practice, 21(6), 699–705. https://doi.org/10.1093/fampra/cmh621
- Necka, E. A., Amir, C., Dildine, T. C., & Atlas, L. Y. (2021). Expectations about pain and analgesic treatment are shaped by medical providers’ facial appearances: Evidence from five online clinical simulation experiments. Social Science & Medicine, 281, 114091. https://doi.org/10.1016/j.socscimed.2021.114091
- Pan, Y., Kinitz, T., Stapic, M., & Nestoriuc, Y. (2019). Minimizing drug adverse events by informing about the nocebo effect—an experimental study. Frontiers in Psychiatry, 10504. https://doi.org/10.3389/fpsyt.2019.00504
- Petrie, K. J., & Rief, W. (2019). psychobiological mechanisms of placebo and nocebo effects: pathways to improve treatments and reduce side effects. Annual Review of Psychology, 70(1), 599–625. https://doi.org/10.1146/annurev-psych-010418-102907
- RCGP. (2021). GP Consultations Post-COVID Should Be a Combination of Remote and Face to Face, Depending on Patient Need, Says College. https://www.rcgp.org.uk/about-us/news/2021/may/gp-consultations-post-covid.aspx
- Stepien, K. A., & Baernstein, A. (2006). Educating for empathy. A review. Journal of General Internal Medicine, 21(5), 524–530. https://doi.org/10.1111/j.1525-1497.2006.00443.x
- Webster, R. K., & Rubin, G. J. (2021). Predicting expectations of side-effects for those which are warned versus not warned about in patient information leaflets. Annals of Behavioral Medicine, 55(22), 1253–1261. https://doi.org/10.1093/abm/kaab015
- Webster, R. K., Weinman, J., & Rubin, G. J. (2016). A systematic review of factors that contribute to nocebo effects. Health Psychology, 35(12), 1334–1355. https://doi.org/10.1037/hea0000416
- Webster, R. K., Weinman, J., & Rubin, G. J. (2018). Positively framed risk information in patient information leaflets reduces side effect reporting: a double-blind randomized controlled trial. Annals of Behavioral Medicine, 52(11), 920–929. https://doi.org/10.1093/abm/kax064
- Wells, R. E., & Kaptchuk, T. J. (2012). To tell the truth, the whole truth, may do patients harm: the problem of the nocebo effect for informed consent. The American Journal of Bioethics, 12(3), 22–29. https://doi.org/10.1080/15265161.2011.652798