ABSTRACT
This work aims to understand intra- and interprofessional networks of general practitioners (GPs) and ear, nose, and throat specialists (ENT specialists), and in what manner supervisors in these specialties involve interns in their professional network to help them learn intra- and interprofessional collaboration. An egocentric social network approach was used to collect and analyze quantitative as well as qualitative data. For this, semi-structured interviews were held with ten GP and ten ENT specialists. GPs had significantly more interprofessional contacts than ENT specialists (p < .01), with no significant difference in the network sizes of both professions (p = .37). All supervisors involved interns in their (ego)network actively as well as more passively. They actively discussed how collaboration with other professionals evolved, or passively assumed that an intern would learn from observing the supervisors’ network interactions. Many supervisors considered the interns’ initiative essential in deciding to involve an intern in their network. Although the workplace of GPs differed notably from hospital settings where ENT specialists work, the network sizes of both were comparable. Clerkships at the general practice seemed to provide more opportunities to learn interprofessional collaboration, for example with the medical nurse. Supervisors in both specialties could involve interns more actively in their intra- and interprofessional network while interns could take more initiative to learn collaboration from their supervisors’ network.
Introduction
To prepare medical interns for their future practice, they need to learn how to provide shared care to patients (Shafran, Richardson, & Bonta, Citation2015). This is increasingly important because of an aging population and its associated rise of patients with chronic diseases and multimorbidity which are difficult to solve by one discipline or healthcare professional alone (Boaden & Leaviss, Citation2000). Interprofessional collaboration “means that members of different professional groups with different specialties […], different areas of expertise and work, and a different level of status all work directly together to provide high-quality, patient-oriented care, so that the patient benefits from the specific skills of each individual profession” (Mahler, Gutmann, Karstens, & Joos, Citation2014, p. 7). Intraprofessional collaboration has been described as “cooperation within a profession” (Mahler et al., Citation2014, p. 7); in the healthcare context, this can be seen as collaboration between professionals from different medical disciplines for which the study of medicine is required. Many uncertainties exist about how to teach intra- and interprofessional collaboration and what moment in the educational continuum is most appropriate.
Background
Throughout their curriculum, interns frequently collaborate within their discipline (Beaulieu et al., Citation2009). To learn collaboration with professionals from another medical discipline (intraprofessional) or with another background than medicine (interprofessional) is not easy through formal education (Nisbet, Lincoln, & Dunn, Citation2013). During the last years of medical training, medical interns are mostly educated in different clinical settings during their clerkship rotations (Van Der Hem-Stokroos, Scherpbier, Van Der Vleuten, De Vries, & Haarman, Citation2001). Between these different clinical settings, the contexts in which interns are exposed to intra- and interprofessional collaboration are expected to differ considerably, especially between hospital clerkships and clerkships in general practice (Manca, Breault, Wishart Citation2011; Van Der Zwet et al., Citation2010).
When interns are involved in the professional interactions of their clerkship supervisors, this might provide opportunities to learn, in an informal manner, to collaborate with other professionals (Bell, McAllister, Ward, & Russell, Citation2016; Burford, Citation2012; Nisbet et al., Citation2013). The relevance of interprofessional networks of supervisors for interns has not been dealt with before. Bell et al. (Citation2016) commented on the importance of informal, interprofessional, learning during professional networking, but the focus in their work was on the learning of professionals themselves while collaborating with colleagues in the workplace. We argue that supervisors’ networks constitute a window of opportunity for interns to learn intra- and interprofessional collaboration.
The concept of professional networking occupies an important role when attempting to understand how interprofessional collaboration at the workplace takes place (Bell et al., Citation2016; Van Waes et al., Citation2016; Van Waes, Van den Bossche, Moolenaar, De Maeyer, & Van Petegem, Citation2015). To date, there has been little research on how professional interaction in the learning environment of an intern takes shape. As Van der Hem (Citation2001) has said that clerkships “should offer students the opportunity to learn in situations that resemble their future professional setting as closely as possible” (p. 599), one could argue that interns need to be involved in supervisors’ networks to learn intra- and interprofessional collaboration. Underexplored is how do supervisors envision intra- and interprofessional collaboration and what role-modeling of collaborative relationships looks like (Côté & Laughrea, Citation2014; Hudson & Croker, Citation2018; Passi & Johnson, Citation2016). Also unknown is whether supervisors consider the interactions in their professional networks as learning opportunities for interns. In addition, there is a need to explore what pedagogies supervisors apply to support the learning of intra- and interprofessional collaboration of interns. Finally, intra- and interprofessional learning opportunities in a hospital environment may differ from a general practice setting. Therefore, characteristics of and differences between networks of supervisors in general practice and hospital setting require further investigation.
The research questions this study aims to answer are:
In what manner do network characteristics of general practitioners and ear, nose, and-throat specialists who act as supervisors differ?
What are supervisors’ perceptions about the workplace pedagogies they apply when involving interns in their intra- and interprofessional collaboration activities?
Methods
A sequential mixed-methods design was adopted collecting quantitative and qualitative data with the same interview (Creswell & Clark, Citation2011). Qualitative data from the interviews were used to understand how supervisors think about involving interns in their intra- and interprofessional collaborative network. Quantitative (ego)network data were used to understand the intra- and interprofessional network characteristics of interns’ supervisors.
Data collection
Data were gathered among ten general practitioners (GPs) and ten ear, nose, and throat (ENT) specialists who supervise interns during their clerkships of respectively five weeks and two weeks long. Within the time frame in which the study took place, it was not possible to include several different medical specialists. Therefore, the approach of including only one specific specialism, ENT, was adopted. Regarding the extensive curriculum change that occurred during this study at the University Medical Center Utrecht, the research group already had contact with various ENT specialists. Given these practical grounds, ENT specialists were chosen as representative of the specialists. Ten GPs of the four interprofessional academic primary care centers of Utrecht were approached, i.e. the the Leidsche Rijn Julius Gezondheidscentra (LRJG). The ten participating ENT specialists were supervisors of the ENT clerkship in the University Medical Center Utrecht and the, to the University Medical Center Utrecht affiliated, ENT departments in general hospitals.
Based on the literature, a semi-structured interview guide to collect egocentric social network data, which is defined as data on the social interaction between individuals (ego’s) and their contacts (alters), was developed (Côté & Laughrea, Citation2014; Passi & Johnson, Citation2016; Van Waes et al., Citation2016, Citation2015). Interviews lasted between 45 and 60 minutes and were all performed by one researcher (MB). Interviews were audio recorded and fully transcribed. Baseline characteristics were collected during the initial questions. The first step was name-generation (Burt et al., Citation2012; Hogan, Carrasco, & Wellman, Citation2007), to visualize networks during the interviews. Respondents (called “egos”) were asked to nominate all others (called “alters”’), and the discipline this alter belongs to, with whom they had contact with regarding patient care within the last month.
A visually aided data collection tool was used (Hogan et al., Citation2007). Respondents were asked to write the disciplines of the people they worked with within the last month on post-it notes. These post-it notes were stuck on a sheet of A1-sized paper with four concentric rings. The inner ring represented the people closest to the respondent, i.e. their team. For GPs, this concerned the general practice within the health center. The inner ring of ENT specialists encompassed the ENT outpatient clinic and, if present, the ENT ward. The second ring stood for the organization their inner ring was part of, i.e. the healthcare center and the hospital, respectively. The third ring featured connections with other practices, hospitals and organizations outside of the health center, respectively, hospital. This ring concerned a looser form of cooperation, in which integration and interdependence were expected to play a less important role. The fourth ring characterized collaborations in which knowledge interchange takes place on an overarching level. An example is a group of clinicians from different institutions meeting each other to discuss the application of clinical guidelines.
Three different network characteristics were explored to gain insight into supervisors’ professional interactions: the size of their professional networks, the number of different individuals per discipline the physician had contact with within the last month, and the frequency of contact. Network size was defined as the number of different contacts with whom a supervisor interacts. This concerned all different disciplines a GP or ENT specialist had contact with regarding patient care within the last month. For example, the pharmacist, the doctors’ assistant and the speech therapist. In order to improve the pace and reliability of filling in numbers, the frequency of contact has been divided into response categories (Burt & Guilarte, Citation1986). A scale varying from more than three times a day to once a year was used (Van Waes et al., Citation2015).
Once the structure of the ego network was elicited, specific information of one alter from each ring was collected (Hogan et al., Citation2007; Van Waes et al., Citation2016). Open questions were used to gain information about the way in which involvement from the intern takes place during the contact with these alters. Furthermore, respondents were asked what they thought interns could learn from the contacts they had with other professionals. The interview ended with an inventory of their behavior as a role model for collaboration. We asked them for example whether they considered themselves to be a role model and what they considered to be most important for interns to learn.
Data analysis
To analyze differences in the sizes of the networks, general statistical procedures were applied. The extracted data were entered in an electronic database (Excel, Microsoft 2010). The Mann-Whitney U test was used to compare the mean of age, mean years of work experience, and mean years of interns’ supervision between the GP and ENT specialists. A probability of less than 0.05 was considered as statistically significant. The main independent variable in this study was profession (GP and ENT specialists). The main dependent variable was network size. Other dependent variables were the number of alters and frequency of contact (only reported on with respect to the visualization). To investigate the window of opportunity supervisors provide to interns to learn intra- and interprofessional collaboration, all contacts of the professional network of a participant were encoded for both types of collaboration. Four groups were created by splitting the contacts per profession into two: one group interprofessional contacts and one for all intraprofessional contacts. An intraprofessional contact was defined as professionals from different medical disciplines for which the study of medicine is required (Mahler et al., Citation2014, p. 7). For example, residents, specialists and committees consisting of only doctors were coded as intraprofessional. Interprofessional was defined as professionals from different disciplines for which the study of medicine is not required. Interprofessional was defined as professionals from different disciplines for which the study of medicine is not required. All different hospital specialists, mentioned by ENT specialists in ring 2, were encoded as ‘specialist’ to allow a meaningful comparison to the network of GPs.
After quantification of data, we performed an analysis of variance (ANOVA) for the variable network size in order to compare the networks of GP and ENT specialists (Van Waes et al., Citation2015). Because the data was not normally distributed, log transformation was applied on the input; on the continuous variable network size (Van Waes et al., Citation2015). Visual inspection of histograms and Q-Q plots underlined that log transformation led to improvement. This finding was also supported by Shapiro-Wilk normality test, which refutes the test of non-normality when log transformation was applied (SW without transformation: W = 0.93, p = .01, SW with log trans-formation: W = 0.97, p = .46).
After log transformation, a one-way ANOVA was carried out on the means of network size per profession based on egocentric network data (Marsden, Citation1993). A one-way ANOVA was also applied to the distribution of interprofessional versus intraprofessional contacts for one profession at a time. ANOVA is used to estimate variance components (Shavelson, Webb, & Rowley, Citation1989). A two-way ANOVA was conducted on the influence of the two different categorical independent variables (profession and type of collaboration) on the continuous dependent variable (network size). Profession included two levels (GP and ENT specialists) and type of collaboration consisted also of two levels (intra- and interprofessional). The interaction effect between profession and interprofessional or intra-professional contacts on network size was thus tested. The software program R (version 3.3.3) was used to analyze the quantitative data. The authors are willing to share the R code with annotation upon reasonable request.
For the qualitative analysis, transcripts were imported into analysis software (QSR NVivo 11). The inductive data analysis took place after the quantitative analysis. An expert in qualitative analysis (FP) was asked for feedback on our process of analysis at different moments in time. Initially, open codes based on the topics covered in the interviews were developed through the coding of two interviews by two different researchers (EdG, JF). After discussions, a first draft of the coding scheme was developed. With this second coding scheme, three interviews were double-coded (EdG, JF). The coding was again discussed in the team. The coding of these transcripts was overlapping sufficiently to decide, based on the recommendation of the expert in qualitative analysis (FP) to code the remaining transcripts by a single researcher (JF). The analysis through axial and selective coding was led by the lead author (EdG) and carried out with frequent in-between discussions of the qualitative researchers (JF and EdG). The whole team of authors was asked for feedback on the final results and clarifications were carried out when necessary. All researchers agreed on the final analytical framework and the results.
Ethical considerations
Ethics approval for the study was received from the ethical review board of the Dutch Society for Medical Education (NVMO). The purpose of the study, potential risks, and benefits were explained through information letters and written informed consent of the participants were obtained in advance.
Results
Baseline characteristics
There was no significant difference between the mean age (43.0 ± 7.1 vs 41.7 ± 8.9, p = .58), work experience in years (9.3 ± 4.9 vs 9.2 ± 10.1, p = .25) and teaching experience in years (6.1 ± 4.5 vs 8.9 ± 9.6, p = .74) of the participating ten GPs and ten ENT specialists. lists the minimum, maximum, mean, median and standard deviation of the baseline characteristics.
Table 1. Baseline characteristics of the twenty participants (in years). Min = Minimum. Max = Maximum, M = Mean, SD = Standard Deviation
Network size
Data on a total of 492 ties were collected. The mean network sizes between the two professions were compared. The network of a GP consisted of, on average, 22 contacts (intra- and interprofessional), whereas the ENT specialist had a mean number of 20 contacts in his network (). A one-way ANOVA did not show a significant difference between those network sizes, F (1, 18) = 0.84, p = .37. The average network size per ring illustrated GPs have more contacts in the second and third ring of collaboration, while ENT specialists have a larger number of contacts in the first and fourth ring ().
Table 2. Descriptive statistics of network size. M Intra = Mean number of intraprofessional contacts, M Inter = Mean number of interprofessional contacts, M total = Mean number of contacts, SD = Standard Deviation
Based on mean frequencies of their interprofessional contacts, GPs interacted most frequently with doctors’ assistants in the first ring of collaboration, the pharmacist in the second ring and outpatient clinic assistants of the hospital in the third ring. The main interprofessional contacts of ENT specialists were, respectively, outpatient clinic assistants, surgery assistants, and speech therapists. Looking at intraprofessional contacts, colleague GPs in the general practice and diverse hospital specialists were most regularly contacted by the GPs. In ENT specialists, most intensive intraprofessional contacts were colleague specialists in the hospital, especially the anesthetist, and GP outside the hospital. The division of the contacts in the two types of collaboration (intra- and interprofessional) demonstrated that GP and ENT specialists both had more interprofessional than intraprofessional contacts (). A network overview of the GP and ENT specialist was created to give an idea of the kind of contacts the network of the supervisors exists of ().
Figure 1. Network overview of a general practitioner The inner ring represents the people closest to the GP: the contacts within the general practice. The second ring stands for the organization the inner ring is part of: the healthcare center. The third ring featured connections with other practices, hospitals and organizations outside of the health center. The fourth ring characterized collaborations in which knowledge interchange takes place on an overarching level. Pharmacists are shown in different rings because pharmacists may work within the healthcare center (second ring) and different pharmacists work outside the center (third ring)
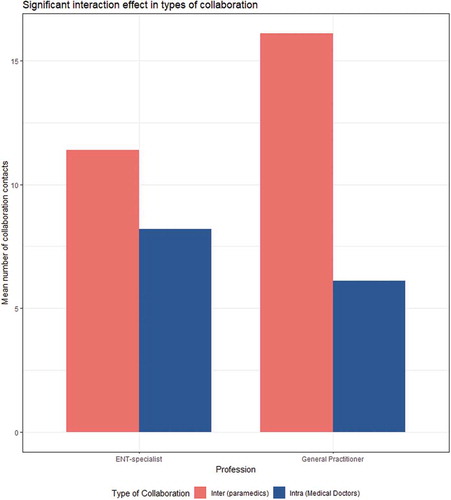
Analysis of variance on the type of collaboration for GPs supported a major significant difference, F (1, 18) = 26.22, p < .001. No significant difference was identified between the types of collaboration for ENT specialists,F (1, 18) = 4.343), p = .052. A two-way ANOVA showed a significant interaction effect between profession and type of collaboration, F (1, 36) = 8.154, p < .01. The interaction effect is visualized in .
Figure 3. Significant interaction effect in types of collaboration. On the x-axis the two different type of professionals and their type of collaboration (intraprofessional in dark gray and interprofessional in light gray). On the y-axis the mean number of collaboration contacts
The qualitative analysis provided insight in what supervisors want interns to learn and what they consider a supervisors’ role to be in giving support to interns. It also showed what pedagogies supervisors apply to support the learning of interns.
What should interns learn during the clerkship?
Supervisors mentioned a wide spectrum of topics which they consider to be the most important for interns to learn during the clerkship. They wanted to teach them more about their profession, medical knowledge, how to behave in the workplace and about intra- and interprofessional collaboration. Concerning this last topic, supervisors mentioned that it is important to know what knowledge other professionals in the healthcare system have and why this is relevant for doing your job and good patient care. As such, they saw changes in their work environment and the increase in the importance of intra- and interprofessional collaboration resulting from those changes.
Well, as I said, I think it’s good to know how it works and that it works like this or doesn’t work like that. And how important it can be to know one another that you know who to ask, that it really makes a difference when you have close contacts and are approachable. […] And that it benefits patient care. (GP respondent 7)
Well, that you understand that there is no more working solo, that you really need knowledge from other people, that you need other specialists as well to achieve your objective. Especially when it concerns sleep apnoea syndrome or some other sleeping disorder that belongs, well, partly to pulmonary medicine, partly to ENT and partly to neurology. Oh sure, it’s great when interns get that. (ENT respondent 1)
Approaches in involving interns
Supervisors applied different pedagogies in supporting the learning process of interns. Concerning intra- and interprofessional collaboration, supervisors often relied on implicit pedagogies. Supervisors let interns listen to the conversations they have with other professionals in their network, putting their telephone on the speaker and stimulate, more or less explicit, that interns observe what other professionals at the workplace are doing and in what manner this is relevant for their work as a specialist. Occasionally, supervisors discussed these interactions with the interns, primarily concerning the medical issues that came forward during that interaction but also about intra- and interprofessional collaboration in general. In several interviews, respondents mentioned that looking back, to discuss with interns their intra- and interprofessional collaborations would have been a good idea, but that practical obstacles were standing in the way, primarily when the intern was not easily available for discussion.
Well okay, in this case it’s about how to approach a specialist. Like, if I have a specific question, how do I manage to get the answer? How can I do that in my own way, or if I want to get something done, how can I achieve that? Naturally, there are different approaches, different forms of communication. […] If an intern had the chance to listen in, it would be a learning opportunity for them. (GP respondent 10)
I think this is also something they could learn from, that it can be very useful to see patients together with some kind of supportive or paramedical staff because they look at it in a completely different way so that you, as a doctor, get insights that you might not have noticed otherwise. […] See how we do this, and discuss what we find valuable about doing like that, you know? (ENT respondent 11)
Supervisors did allow interns to have their own intra- and interprofessional interactions. GPs mention this more often than ENT specialists. However, both, GP and ENT specialists, added to this, that this depends heavenly on how competent the supervisor thinks the intern is.
What I also do when an intern clearly knows what he is doing, […], then I let him get on with it. If the intern thinks the patient should be referred to the hospital, and I agree, I let him handle the communication and refer the patient. (GP respondent 8)
Occasionally, I tell the intern, “Well, go ahead, make that appointment.” When I think it’s all going well, then I say, “Do what needs to be done, together with the assistant. As long as you arrange this and that.” (ENT respondent 4)
Reasons for not involving interns in their interaction with others in their network were that supervisors thought that the clerkship did not have intra- or interprofessional collaboration as a learning goal or was too brief for paying attention to those learning goals. Also, practical or logistical reasons were standing in the way of focusing on collaboration. ENT specialists, more than GPs, considered the involvement of interns during supervisors’ interactions in their network as not useful for learning which might be related to the shorter duration of their clerkships. Especially interactions with professionals outside the strictly medical work (ring 4) were not considered useful for interns.
Well, I don’t know if that would be useful. For now, I wouldn’t think of taking the intern with me to those meetings. I think it’s more interesting for them to watch an operation or do consultations, those kinds of things. Even when the meetings are part of the job. (ENT respondent 11)
Role of the supervisor
Supervisors from both professions did not consider themselves as role models concerning intra- or interprofessional collaboration. Even though supervisors were convinced that being able to collaborate intra- and interprofessionally is very important, most of them thought that interns will learn this without explicit actions by them, as supervisors. They used words such as ‘watch’, ‘observe’ but without an indication of what their role is in making the watching or the observation possible.
I think that she learns passively, by observing how things go, not by me making it a real task or by involving her actively. Could do it, though. (GP respondent 20)
The intern not being present seems to be a major barrier for learning intra- and interprofessional collaboration. When the intern is elsewhere, he or she does not see how it works. Most supervisors did not consider it their responsibility to get the interns involved. The interns’ initiative was considered essential. Supervisors thought that interns should create their own learning opportunities.
No, in general no telephone calls, unless the calls are about a patient who the intern has seen in the hospital. But in general the intern won’t be involved. No. Just maybe if the intern is here, with me, in the room. However, if the intern is somewhere else, certainly not. (ENT respondent 15)
Well, yes, you could discuss it afterwards. […] I think that they can learn [from that]. But I have to say that in daily practice I don’t do this very often because the intern is in her own room and doing her own things. (GP respondent 6)
But I think that’s often on the intern’s own initiative, if I’m very honest. Well, you know, if the intern is interested and takes part in the conversation, then he is automatically involved and I don’t mind that. But if that intern is sitting on the other side of the table in the lunch room and doesn’t hear it, then I won’t actively say to him, oh yeah you’ve seen that patient too, or something. (GP respondent 14)
One of the ENT specialists considered intra- and interprofessional important but did attribute their limited involvement of interns to their specific discipline. Other disciplines were more suitable for learning about such collaboration.
Yes, that’s actually not something I consciously transfer to them because I think it’s a health sector [thing, the idea that] you have to do things together, you have to work across borders. […] It’s not something that I explicitly discuss with the intern. […] As an ENT, relatively speaking you are out in the back of beyond, purely because it is a very defined area. So I think we’re not the [best] example. […] If you could only see all the people we work with so very intensively. Often it’s very brief contact, and yes, they don’t always see that. […] But yes, it’s something that does go on in the healthcare sector, so I suspect that they really should be exposed to it. (ENT respondent 1)
Discussion
The study provides insight into the professional networks of intern supervisors. The mean network size did not differ between GP and ENT specialists, despite the fundamental differences in context. In both learning environments, the hospital and the general practice, there seem to be opportunities for interns to learn intra- and interprofessional collaboration. A clerkship in the general practice, nevertheless, provides a significantly higher number of learning opportunities for interprofessional collaboration.
This study nuances previous findings of network size and intra- and interprofessional collaboration. Preliminary work in this field revealed that social networks of physicians merely consisted of other physicians (intraprofessional) (West, Barron, Dowsett, & Newton, Citation1999). Physicians tended to form connections with people who are like them instead of connecting with diverse professions (Tasselli, Citation2014; West et al., Citation1999). A study by Creswick, Westbrook, and Braithwaite (Citation2009), noted that physicians in the emergency department sporadically forge communication ties with members of other professions (interprofessional), whereas they were very likely to contact members of the same profession. This is important since the current complexity of work tasks in healthcare need collaboration across levels of care. As healthcare labor is divided into tasks assigned to different people, different professionals depend on each other in their work. The necessity of intra- and interprofessional collaboration is endorsed in several significant studies (Beaulieu et al., Citation2009; Tasselli, Citation2014). Findings in more recent literature meet this need and are consistent with our results. For instance, a recent study discovered that physicians in a team of healthcare professionals of a hospital burn unit were involved in a higher percentage of interprofessional than intraprofessional contacts (Shoham, Harris, Mundt, & McGaghie, Citation2016). With a percentage of 90%, they even computed substantial higher values for interprofessional collaboration compared to our results. The network size of the physicians involved in their study was in line with our results, as a mean of 20 contacts was found (Shoham et al., Citation2016). Another example is the study of Pomare, Long, Ellis, Churruca, and Braithwaite (Citation2018), in which was shown that the staff of two youth mental health service centers tends to collaborate with colleagues outside of their professional group.
The qualitative findings help us understand better whether opportunities were seized. Van Der Hem-Stokroos (Citation2001) has concluded that ‘learning during a clerkship occurs rather haphazardly’ (p. 599) and the same appears to be true for learning intra- and interprofessional collaboration. Our results suggest that the opportunities interns have to get hands-on experience with intra- or interprofessional collaboration varies substantially from intern to intern, depending on how knowledgeable the supervisor thinks the intern is. Supervisors in our study, irrespective of their work in general practice or the hospital, indicated that their main consideration to let them handle things on their own with contacts from within their network was closely related with this assessment.
In our study, several respondents indicated that learning intra- and interprofessional learning should not be a main goal during the clerkships. This aligns with ideas about clerkships as the place where undergraduate students are expected to master the basic clinical skills, not more (Van Der Hem-Stokroos et al., Citation2001). In his work about interprofessional shadowing, Daniel Shafran (Citation2015) refers to the debate on the optimal timing for interprofessional education. These authors took the middle ground, stating that “interprofessional education experiences should be undertaken early in medical school to foster positive attitudes toward and healthy relationships with collaborating healthcare professionals and should be continued through later stages of training to harness its more practical benefits” (p.88). In our results, it has become clear that interns, at least during these two types of clerkships have opportunities to develop these positive attitudes to a certain degree but it remains open for discussion whether such a small step is sufficient, as these clerkships are occurring in the fifth year of the curriculum.
Limitations
This study should be interpreted within the context of its strengths and potential limitations. The study set up we used was based on the work of Waes and colleagues. (Citation2015). Their study looked into education science faculty members. Faculty members, however, turned out to have relatively few contacts. For example, they reported mean network sizes varying from 6 to 12 contacts. Our mean network size differed between 20 to 22 contacts. For this reason, we obtained a less in-depth view of the networks in the same period. As a solution, only one alter from each ring was questioned in-depth to receive some profound details. As a result, the richness of our qualitative data could have been larger. A strength of this study is the use of a visually aided data collection tool which was an innovative way to elicit physicians’ networks during interviews. Respondents enjoyed the use of visualization during name generation and various respondents commented on how they currently realized how broad their network was and how they never considered their network in such a fashion. The significant results of the statistical analyses support the findings based on the graph (). Although the sample size remains a limitation, this gave us confidence to support our claims with inferential statistics. We do suggest further research with more data.
The findings of the ENT network cannot be generalized in the same way as results from a survey of multiple different specialists would have done. This limitation emphasizes the importance of ongoing research to explore the relevance of our findings beyond the networks that we measured. Hospital specialists focus primarily on the medical problem whereas GPs also look at problems evoked by social interactions. Therefore, a comparison of GPs, who are connected with the social domain, with one kind of hospital specialists is a first step.
Study contribution
This study contributes to the understanding of how supervisors of a clerkship provide a window of opportunity for interns to learn intra- and interprofessional collaboration at the workplace. The qualitative findings help us understand better what aspects are relevant with respect to the opportunities that the supervisors’ network provide for learning intra- and interprofessional collaboration. The results indicate the importance of more active pedagogies as well as initiative of the intern to use the opportunities provided to learn intra- and interprofessional collaboration. We may need to expand our focus to include the way interns experience their supervisors’ contacts. This study described an interview-based data collection based on participants’ perceptions of their network. A useful complement to our knowledge about professional networks could be to observe collaboration at the workplace itself. Closely following subjects over a period to investigate with whom professionals interact is called work shadowing (Quinlan, Citation2008). Unlike interviews, work shadowing is less dependent on the accuracy of reporting relationships. Work shadowing could be a design to collect professionals’ network data for future research.
Concluding comments
This study aimed to explore and compare the characteristics of the professional network of interns’ supervisors. Furthermore, knowledge about opportunities for learning collaboration in the different workplaces was acquired. The size of the overall network of GP and ENT specialists are similar. However, at least for these types, the number of interprofessional contacts in comparison to intraprofessional contacts vary. During a clerkship at the general practice, more opportunities for interprofessional collaboration are present in comparison to a clerkship in the ENT department of the hospital. These findings suggest an important role for the general practice as an interprofessional learning environment. Whether interns will be able to profit from these opportunities, both in general practice and in the hospital, to learn collaboration depends on the pedagogies that supervisors utilize. Our study suggests that important gains are possible when supervisors involve interns in a more active manner in their own intra- as well as interprofessional interactions. Supervisors underline however that interns should take more initiative to learn intra- and interprofessional collaboration.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Beaulieu, M., Samson, L., Rocher, G., Rioux, M., Boucher, L., & Del Grande, C. (2009). Investigating the barriers to teaching family physicians’ and specialists’ collaboration in the training environment: A qualitative study. BMC Medical Education, 9. doi:10.1186/1472-6920-9-31
- Bell, E., McAllister, S., Ward, P. R., & Russell, A. (2016). Interprofessional learning, impression management, and spontaneity in the acute healthcare setting. Journal of Interprofessional Care, 30, 553–558. doi:10.1080/13561820.2016.1198310
- Boaden, N., & Leaviss, J. (2000). Putting teamwork in context. Medical Education, 34, 921–927. doi:10.1046/j.1365-2923.2000.00794.x
- Burford, B. (2012). Group processes in medical education: Learning from social identity theory. Medical Education, 46, 143–152. doi:10.1111/j.1365-2923.2011.04099.x
- Burt, R. S., & Guilarte, M. G. (1986). A note on scaling the general social survey network item response categories. Social Networks, 8, 387–396. doi:10.1016/0378-8733(86)90004-3
- Burt, R. S., Meltzer, D. O., Seid, M., Borgert, A., Chung, J. W., Colletti, R. B., … Margolis, P. (2012). What’s in a name generator? choosing the right name generators for social network surveys in healthcare quality and safety research. BMJ Quality & Safety, 21, 992–1000. doi:10.1136/bmjqs-2011-000521
- Côté, L., & Laughrea, P. (2014). Preceptors’ understanding and use of role modeling to develop the CanMEDS competencies in residents. Academic Medicine, 89, 934–939. doi:10.1097/ACM.0000000000000246
- Creswell, J., & Clark, V. (2011). Desiging and conducting mixed methods research. Thousand Oaks, CA: Sage.
- Creswick, N., Westbrook, J. I., & Braithwaite, J. (2009). Understanding communication networks in the emergency department. BMC Health Services Research, 9. doi:10.1186/1472-6963-9-247
- Hogan, B., Carrasco, J. A., & Wellman, B. (2007). Visualizing personal networks: Working with participant-aided sociograms. Field Methods, 19, 116–144. doi:10.1177/1525822X06298589
- Hudson, J. N., & Croker, A. (2018). Educating for collaborative practice: An interpretation of current achievements and thoughts for future directions. Medical Education, 52, 114–124. doi:10.1111/medu.13455
- Mahler, C., Gutmann, T., Karstens, S., & Joos, S. (2014). Terminology for interprofessional collaboration: Definition and current practice [Begrifflichkeiten für die zusammenarbeit in den gesundheitsberufen – Definition und gängige praxis]. doi:10.3205/zma000932
- Manca, D. P., Breault, L., & Wishart, P. (2011). A tale of two cultures: Specialists and generalists sharing the load. Canadian Family Physician, 57(5), 576–584.
- Marsden, P. V. (1993). The reliability of network density and composition measures. Social Networks, 15, 399–421. doi:10.1016/0378-8733(93)90014-C
- Nisbet, G., Lincoln, M., & Dunn, S. (2013). Informal interprofessional learning: An untapped opportunity for learning and change within the workplace. Journal of Interprofessional Care, 27, 469–475. doi:10.3109/13561820.2013.805735
- Passi, V., & Johnson, N. (2016). The hidden process of positive doctor role modelling. Medical Teacher, 38, 700–707. doi:10.3109/0142159X.2015.1087482
- Pomare, C., Long, J. C., Ellis, L. A., Churruca, K., & Braithwaite, J. (2018). Interprofessional collaboration in mental health settings: A social network analysis. doi:10.1080/13561820.2018.1544550
- Quinlan, E. (2008). Conspicuous invisibility: Shadowing as a data collection strategy. Qualitative Inquiry, 14, 1480–1499. doi:10.1177/1077800408318318
- Shafran, D. M., Richardson, L., & Bonta, M. (2015). A novel interprofessional shadowing initiative for senior medical students. Medical Teacher, 37, 86–89. doi:10.3109/0142159X.2014.929099
- Shavelson, R. J., Webb, N. M., & Rowley, G. L. (1989). Generalizability theory. American Psychologist, 44, 922–932. doi:10.1037/0003-066X.44.6.922
- Shoham, D. A., Harris, J. K., Mundt, M., & McGaghie, W. (2016). A network model of communication in an interprofessional team of healthcare professionals: A cross-sectional study of a burn unit. Journal of Interprofessional Care, 30, 661–667. doi:10.1080/13561820.2016.1203296
- Tasselli, S. (2014). Social networks of professionals in health care organizations: A review. Medical Care Research and Review, 71, 619–660. doi:10.1177/1077558714557079
- Van Der Hem-Stokroos, H. H., Scherpbier, A. J. J. A., Van Der Vleuten, C. P. M., De Vries, H., & Haarman, H. J. (2001). How effective is a clerkship as a learning environment?. Medical Teacher, 23, 599–604. doi:10.1080/01421590127200
- Van Der Zwet, J., Hanssen, V. G. A., Zwietering, P. J., Muijtjens, A. M. M., Van Der Vleuten, C. P. M., Metsemakers, J. F. M., & Scherpbier, A. J. J. A. (2010). Workplace learning in general practice: Supervision, patient mix and independence emerge from the black box once again. Medical Teacher, 32, e294–e299. doi:10.3109/0142159X.2010.489128
- Van Waes, S., Moolenaar, N. M., Daly, A. J., Heldens, H. H. P. F., Donche, V., Van Petegem, P., & Van den Bossche, P. (2016). The networked instructor: The quality of networks in different stages of professional development. Teaching and Teacher Education, 59, 295–308. doi:10.1016/j.tate.2016.05.022
- Van Waes, S., Van den Bossche, P., Moolenaar, N. M., De Maeyer, S., & Van Petegem, P. (2015). Know-who? linking faculty’s networks to stages of instructional development. Higher Education, 70, 807–826. doi:10.1007/s10734-015-9868-8
- West, E., Barron, D. N., Dowsett, J., & Newton, J. N. (1999). Hierarchies and cliques in the social networks of health care professionals: Implications for the design of dissemination strategies. Social Science & Medicine, 48, 633–646. doi:10.1016/S0277-9536(98)00361-X