ABSTRACT
Extreme demand avoidance (EDA) is increasingly described as part of the autism spectrum and is sometimes diagnosed as Pathological Demand Avoidance (PDA). Yet little is known, about the educational experiences of children with and without EDA behaviours. Using an online survey collecting both quantitative and qualitative data, 211 parents reported on the school experiences of their autistic children. 57 parents had a child with an additional diagnosis of PDA (AUT-PDA); 91 had a child with no diagnosis of PDA but, according to parent report, displayed EDA behaviours (AUT-EDA); and 63 had a child with neither a PDA diagnosis nor EDA behaviours (AUT). Results demonstrated that there were few group differences in terms of the frequency of failed school placements and exclusions. However, children in the AUT-EDA/-PDA groups had higher levels of behaviour that challenges, which were particularly high in those with a PDA diagnosis. There were no significant differences in school exclusions, but the fact that these occurred across all groups is of concern. Qualitative results suggested overwhelmingly negative school experiences for all groups but especially the AUT-EDA and AUT-PDA groups. Parents attributed such experiences to misunderstanding of their children’s diagnoses and a lack of targeted support.
Over 20 years ago, Newson and Le Marechal (Citation1998) identified what they considered to be a distinct subgroup of children who had been diagnosed with autism and/or pervasive developmental disorder but seemed to differ from the ‘typical’ presentations of these conditions in their apparent anxiety-driven avoidance of demands. These observations formed the basis of what is now sometimes described as extreme demand avoidance (EDA) or pathological demand avoidance (PDA), the defining feature of which is the continued avoidance of the ordinary demands of life (Christie Citation2007). A prevalence study conducted in the Faroe Islands (Gillberg et al. Citation2015) suggested that one in five autistic people may have PDA in childhood and that just under 0.2% of the population could be described as being autistic with PDA. These are tentative figures, however, as there is no consensus about how PDA should be identified.
PDA is not included as a diagnostic category in the major diagnostic manuals (American Psychiatric Association Citation2013; World Health Organisation Citation2018) nor is it recognised – formally or informally – by many researchers, clinicians and autistic advocates (e.g. Green et al. Citation2018; Green 2020; Milton Citation2013; Moore Citation2020; Woods Citation2017, Citation2020). Green (Citation2020) has expressed concern about the lack of empirical evidence for PDA as an ‘entity’ (Green Citation2020, 74) and the extent to which research and thinking in this area may be considered circular (see also Woods Citation2020). Gore Langton and Frederickson (Citation2018) highlighted that this lack of recognition and understanding may lead to parents of those children who display behaviours associated with PDA (EDA behaviours) to be subject to similar judgements and blame that parents of autistic children have historically experienced (Courcy and des Rivières Citation2017; Langan Citation2011; Silverman and Brosco Citation2007; Waltz Citation2015; Wolff Citation2004).
There is also no consensus about PDA’s relationship to autism (Gillberg et al. 2015). Newson, Le Marechal, and David (Citation2003) originally proposed PDA as separate category within the Pervasive Developmental Disorders, distinct from autism. However, Christie (Citation2007) highlighted the way in which changes to our understanding of autism and Pervasive Developmental Disorders have led to more people viewing Pervasive Developmental Disorders and autism as synonymous and, as such, have started to view PDA as being part of the autistic spectrum. Indeed, the PDA Society (Citationn.d.) state that PDA should not be considered a standalone diagnosis, but a profile seen in some autistic individuals. Nevertheless, Malik and Baird (Citation2018) identify overlaps between traits typically associated with PDA and those associated with many other conditions such as anxiety and mood disorders, conduct disorders and oppositional defiance disorder, raising more questions about the extent to which PDA should be viewed as associated solely with autism.
Despite this lack of formal recognition and the confusion about the relationship between PDA and autism, increasing numbers of families and local authorities, especially in the United Kingdom (UK), are requesting a diagnosis of PDA – either in addition to, or instead of, a diagnosis of autism (Green et al. Citation2018). Indeed, some parents and clinicians stress that it can be difficult to access appropriate educational support without a PDA diagnosis (Sherwin Citation2015). Gore Langton and Frederickson (Citation2018) reported that some parents felt that ‘the identification of PDA was the route to the professional being able to suggest appropriate management strategies’ for daily living (22). It is important to note that ‘appropriate’ support rather than additional support was the focus here, with Gore Langton and Frederickson (Citation2018) highlighting that different strategies are recommended to support those with PDA than are recommended to support autistic students more generally.
The importance of using these different strategies, which include allowing the child increased autonomy and avoiding rewards and sanctions, has been emphasised by some academics and practitioners (Christie Citation2007; Christie et al. Citation2012, Fidler and Christie Citation2019, Newson, Le Marechal, and David Citation2003; Ozsivadjian Citation2020). Others feel there is little empirical evidence for the use of such strategies (Green Citation2020), and still others argue that they are likely to be useful for many autistic people, not just those described as having PDA (Woods Citation2019). Notwithstanding, the discussion highlights the importance of considering the interactions between children and their environment rather than approaching all demand-related difficulties as being due to intrinsic (within-child) factors (Green et al. Citation2018; Green Citation2020; Ozsivadjian Citation2020).
Although the PDA Society (Citation2018) suggests that school difficulties faced by children with EDA behaviours may be more pronounced than those experienced by children without EDA behaviours there is currently limited research to support this claim. In one of the few peer-reviewed studies on this topic, Gore Langton and Frederickson (Citation2016) surveyed 49 parents of children with PDA who reported that their children faced substantial challenges at school. These challenges included high rates of school exclusion, placement breakdown (where pupils move schools due to their educational needs or because they have been excluded) and what Gore Langton and Frederickson (Citation2016) define as ‘problem behaviours’ (255) (e.g. refusing to attend or comply; leaving the classroom or school site; hurting themselves, staff or other pupils). Some of these behaviours could be challenging for teachers (e.g. refusing to attend or comply and hurting staff) whereas others may impact on other children (e.g. hurting other pupils) and some have a direct impact on the children themselves (e.g. hurting self).
Gore Langton and Frederickson’s (Citation2016) study did not distinguish, however, between children with EDA behaviours with or without a formal PDA diagnosis. This distinction is important as there may be differences in the ways that professionals respond to the needs of children with a formal PDA diagnosis which, in turn, may affect their educational experiences. Their study also lacked an autistic comparison group (those without EDA behaviours). Thus, it is unclear whether children with EDA behaviours (with or without a formal diagnosis of PDA) are at particular risk of negative school experiences compared to children with an autism diagnosis alone.
The current study
The present study sought to extend Gore Langton and Frederickson’s (Citation2016) work by directly comparing the educational experiences of autistic children with and without EDA behaviours, and with and without a PDA diagnosis. To achieve this aim, we developed an online survey for parents and carers of autistic children, asking them to provide information about their children’s diagnoses and to complete questionnaires measuring their children’s autistic features, behaviour that challenges,Footnote1 and current/previous school experiences. Parents were specifically asked whether their child had a formal diagnosis of PDA. They were also asked to complete the Extreme Demand Avoidance Questionnaire (EDA-Q) (O’Nions et al. Citation2014) to measure the degree of EDA behaviours. In so doing, we explored (a) within-child factors by measuring their autistic features and PDA behaviours, and (b) the interactions between the child and their environment by analysing parent comments about their educational environment and experiences.
Method
Participants
An online survey was advertised to parents and carers of autistic children and young people in the UK, via the websites and online forums of local and national autism charities, as well as the PDA Society. To be eligible to participate, respondents needed to reside in the UK and have a school-aged child (4-18 years) with an autism diagnosis. In total, 273 parents completed the survey, of which 62 (23%) were excluded because they either had a child over 18 years (n = 4, 1%) or under 4 years (n = 1, >1%); lived outside the UK (n = 1, >1%), or reported that their child did not have an autism diagnosis (n = 56, 21%).
The remaining 211 respondents were included in the analysis; they comprised 200 biological parents, seven adoptive parents and four grandparents. Most were female (n = 204, 97%), with a mean age of 44 years (range = 27–80 yrs). Full demographics are presented in .
Table 1. Background data on parent respondents from the AUT, AUT-EDA and AUT-PDA groups.
Group allocation
On the basis of parental information regarding PDA diagnosis and level of EDA behaviours (see Measures below), respondents were divided into three groups: (1) an autism (AUT) group (n = 63; 30%), i.e. those with children who had an autism diagnosis but no PDA diagnosis and who scored below the threshold for EDA behaviours on the EDA-Q (O’Nions et al. Citation2014); (2) an AUT-EDA group (n = 91, 43%), i.e. those with children who had an autism diagnosis but no PDA diagnosis and who scored above threshold on the EDA-Q; (3) an AUT-PDA group (n = 57, 27%), i.e. parents with children who had both an autism diagnosis and a PDA diagnosis. As expected, most children in the latter group scored above threshold on the EDA-Q (Mdn=60.00, range = 22–74). The EDA-Q scores of ten children, however, fell below the threshold (Mdn=44.00, range = 22–46). Given that meeting threshold on the EDA-Q is not required for a PDA diagnosis, we have included these ten children in the PDA group. We also conducted analyses excluding these ten children to examine their influence on the results.
Measures
The online survey contained six parts. Parts 1 and 2 collected demographic information about respondents and their children, respectively. Part 3 included ten items assessing parental views on their children’s current and previous educational experiences (taken directly from the Educational Experiences Questionnaire, EE-Q; Gore Langton and Frederickson Citation2016). These focussed on:
number of school exclusions, both fixed term (i.e. exclusion for a fixed period of time due to perceived behavioural problems and formally recorded in school and student records), and informal (i.e. parents asked to collect their child from school for reasons other than illness; not recorded formally as an exclusion);
behaviour that challenges (e.g. refusing to attend or comply; leaving the classroom or school site; hurting themselves, staff or other pupils) displayed by the children during what parents felt was the most difficult term that their child has ever had at school; and
level of support provided by different educational professionals, and how helpful that support was perceived to be (using an open text box).
Part 4 asked parents to complete two standardised questionnaires on their child’s behaviour. First, in the 26-item Extreme Demand Avoidance Questionnaire (EDA-Q) (O’Nions et al. Citation2014), they rated the likelihood of their child displaying each EDA behaviour on a four-point Likert scale, ranging from ‘not true’ (score of 0) to ‘very true’ (score of 3) (note: some items are reverse coded). Higher scores reflect higher levels of EDA behaviours. Scores ≥ 50 for 5- to 11-year-olds, or ≥ 45 for 12- to 17-year-olds are described by O’Nions et al. (Citation2014) as being indicative of PDA. The EDA-Q has good levels of sensitivity (.80) and specificity (.85), and high internal consistency (Cronbach’s α = .93; O’Nions et al. Citation2014); in the current study Cronbach’s α = 0.90.
Second, following Gore Langton and Frederickson (Citation2016), parents completed the 25-item Strengths and Difficulties Questionnaire (SDQ) (Goodman Citation1997), which assessed children’s emotional and behavioural difficulties more generally. Parents rated each item on a three-point scale, ranging from ‘not true’ (score of 0) to ‘certainly true’ (score of 2) (note: again, some items are reverse coded). Higher scores reflect greater emotional and behavioural difficulties (0-13 = ‘typical’, 14-16 = ‘borderline’ and ≥17 = ‘atypical'). This scale has previously been used by researchers to explore behaviours associated with PDA (Gore Langton and Frederickson Citation2016; O’Nions et al. Citation2014). The scale’s reliability with autistic adolescents has been estimated as moderate, with Cronbach’s α ranging from 0.53–0.70 (Simonoff, Jones, and Baird Citation2013). In the current study, reliability estimates were also moderate (α>0.69 for all subscales, except parent-rated peer problems, α = 0.59).
Part 5 asked parents to report on their child’s autistic features using the 65-item Social Responsiveness Scale–2 (SRS-2) (Constantino and Gruber Citation2012). Parents rated their children’s behaviour on a four-point scale, ranging from ‘not true’ (score of 0) to ‘almost always true’ (score of 3). Certain items are reverse coded and then scores are summed to yield a total score. Higher scores reflect greater severity, with T scores ≥66 indicative of an autism profile, and T-scores ≥76 indicative of ‘severe’ difficulties associated with a clinical diagnosis of autism. Internal consistency estimates for the SRS-2 are high (α>0.94) (Bruni Citation2014; Nelson et al. Citation2016); in the current study α = 0.93.
Finally, in Part 6, parents were invited to share ‘anything else you would like to tell us about your child or their experience of education’ in an open text box.
Procedure
Ethical approval was obtained via the Department of Psychology and Human Development at UCL Institute of Education. Responses to the online survey, powered by SurveyMonkey, were collected over six months (January to June 2017).
Data analysis
Quantitative data. First, we sought to compare the behavioural characteristics of children in the three groups. Due to non-normality of distributions, the data did not meet the required assumptions for parametric tests, hence Kruskall-Wallis tests were used for group comparisons (AUT, AUT-EDA, AUT-PDA) on key demographic variables, scores on the EDA-Q, SDQ and SRS-2, and educational experiences. Due to the number of questionnaires used and resulting number of comparisons, a cautious p level of 0.01 was set to reduce the possibility of Type 1 errors, however we also highlight and discuss (tentatively) instances where p <.05. We predicted that higher scores on the EDA-Q would be linked to higher scores on the SDQ, indicating greater emotional and behavioural challenges for children with elevated EDA behaviours. There were no clear predictions regarding the SRS-2, given the ambiguity within the literature about the extent to which PDA is part of the autism spectrum (Gillberg et al. Citation2015).
Second, we compared children’s educational experiences across the three groups. These included frequencies of failed placements, formal exclusions, informal exclusions (which are illegal in the UK and yet still widely used; Atkinson Citation2013), and the extent of behaviour that challenges during the children’s most difficult term at school. We predicted that, compared with children in the AUT group, those with AUT-EDA and AUT-PDA would have poorer educational experiences, including significantly (i) more fixed-term and informal exclusions and (ii) greater levels of behaviour that challenges. We were also interested in the professional support they received and what aspects of this support were helpful. Because of a lack of previous research in this area, no predictions were made concerning potential differences between the AUT-EDA and AUT-PDA groups.
Qualitative data. Parents’ views about professional support were analysed using content analysis (Mayring Citation2015), in which responses were divided into categories. Categories were not pre-defined but arose from the analysis of the data which was undertaken by one researcher (CT). Once the categories were established, the number of responses in each category was recorded.
We also sought to understand parents’ views about their children’s education. To this end, parents’ responses in Part 6 were analysed by three authors (CT, LC, EP) using thematic analysis (Braun and Clarke Citation2006). CT, who led the analysis, is an educator specialising in supporting students who display traits associated with PDA. EP and LC are autism researchers who have not worked directly with children with PDA. An inductive approach was employed, whereby data were coded without reference to any pre-existing coding schemes or preconceptions. Initially, the authors independently familiarised themselves with the data, reading and re-reading the transcripts, and assigning codes to data extracts. They then conferred regularly to discuss preliminary codes, which were completed for each group separately. The authors liaised several times to review themes and subthemes, focusing on semantic (surface-level) features of the data, resolving discrepancies and deciding on the final definitions of themes and subthemes.
Results
Group profiles
Child characteristics. There were no significant differences between the three groups on key parent-reported background variables, including children’s age, gender, reported use of language, and perceived level of cognitive ability (all p values ≥.09; see ). As expected, given the group allocation criteria, there were significant group differences on the EDA-Q (see ). Planned comparisons showed that the EDA-Q scores of the AUT group were significantly lower than those of the AUT-EDA and AUT-PDA groups (ps <.001). There were no significant differences in the latter two groups’ EDA-Q scores (p = 1.00).
Table 2. Child characteristics in the AUT, AUT-EDA and AUT-PDA groups.
Table 3. Behavioural characteristics of the AUT, AUT-EDA and AUT-PDA groups.
There were significant group differences on the SDQ (see ). Planned comparisons indicated that children in the AUT group had lower SDQ scores, reflective of fewer emotional and behavioural difficulties, than children in the other two groups (ps<.001). There was no significant difference in the SDQ scores of the AUT-EDA and AUT-PDA groups (p = 1.00).
Significant group differences were also observed on the SRS-2. Post-hoc analyses showed that the AUT-EDA group had significantly higher scores, reflecting greater autistic features, than the AUT group (p<.001), but this did not reach significance in the AUT-PDA (p = .03) group. There was no significant difference between the SRS-2 scores of the children in the AUT and AUT-PDA groups (p = .89).
Educational placements
There were no significant group differences regarding type of current school placement, reported level of formal educational support received at school (including whether they had a statement of Special Educational Needs or an Education Health and Care Plan; see ), or whether school placement was mainstream without support or included additional support (e.g. with a support assistant) (ps>.20).
Table 4. Details on the children’s educational placements in the AUT, AUT-EDA and AUT-PDA groups.
Exclusions. The fixed term and informal exclusions experienced by children in each group are reported in . Contrary to expectations, there were no group differences in the frequency of fixed-term exclusions (H(2) = 5.77 p = .06, n = 205). Group differences in the frequency of informal exclusions failed to reach the specified level of significance (H(2) = 7.20, p = .03, n = 187).
Table 5. Information ahout the children’s experiences of exclusion for the AUT, AUT-EDA and AUT-PDA groups (note: not all participants provided this information).
Behaviour that challenges. As predicted, the AUT group was generally reported to display fewer specific behavioural difficulties than the other two groups (see ). One exception to this pattern, however, related to hurting or attempting to hurt other pupils and staff: parents reported similar rates of these behaviours among children in the AUT group and those in the AUT-EDA group. On most other variables, parents in the AUT-PDA group reported higher levels of behaviour that challenges than those in the AUT-EDA group who in turn reported higher levels of such behaviour than those in the AUT group. The exceptions here were refusal to attend and hurting or attempting to hurt themselves (where there were no significant differences between the AUT-EDA and AUT-PDA groups).
Table 6. Information about the children’s behaviour that challenges in their most difficult term at school (as identified by parents), for the AUT, AUT-EDA and AUT-PDA groups.Table Footnotea
Supplementary analyses excluding the ten children in the PDA group who did not meet threshold on the EDA-Q revealed an identical pattern of results to those reported above.Footnote2
Professional support
Results of the content analysis on parents’ experiences of professional support for their child are reported in . It is noteworthy that many parents (n = 25) were unable to identify a helpful professional and instead described a lack of professional support. That said, access to diagnosis was the most common comment made about the helpfulness of professionals’ involvement (n = 49), and this was particularly true for the AUT-EDA (n = 21) and AUT-PDA (n = 14) groups. Understanding and helping others to understand EDA behaviours (n = 40), and the provision of practical strategies (n = 38), were the second and third most common comments raised, respectively. The provision of practical strategies was particularly important for the AUT group (n = 18).
Table 7. Information about the support from professionals that parents in the AUT, AUT-EDA and AUT-PDA groups found most helpful. The three most commonly reported professionals are shown here. More detail is available in supplementary material.
Qualitative analysis
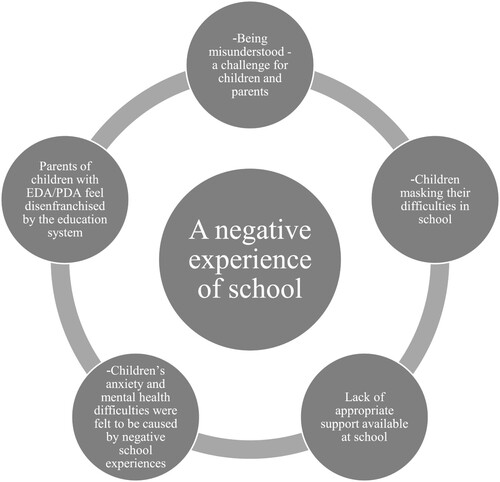
Analyses of the open-ended responses revealed that parents – across all groups – described predominantly negative school experiences for their children, such as ‘a rollercoaster ride through education’ (AUT group). We identified five themes (see ), that were similar across all groups (AUT, AUT-EDA, AUT-PDA). Whilst the themes are presented for the entire sample, we note below any instances of group differences.
Being misunderstood is a challenge for children and parents. Parents perceived their children’s negative educational experiences to be caused, at least in part, by professionals’ lack of understanding of autism and, in some cases, PDA: ‘We are currently very restricted in terms of accessing basic services due to chronic lack of PDA understanding (and ASD!)’ (AUT-EDA). In the few instances in which parents reported a positive experience, they felt their child was understood by school staff: ‘School have got the measure of him and support him brilliantly’ (AUT).
Parents of children with EDA behaviours (with and without a diagnosis of PDA) felt that the schools’ misunderstandings were attributable to their children’s unusual presentation: ‘Because he doesn’t look or behave like a ‘typical’ autistic child, the school have struggled to accept that his behaviour is not deliberate and that his reactions are due to anxiety, not disobedience’. Parents also reported that teachers did not necessarily ‘believe’ in the existence of PDA (AUT-EDA).
For parents whose children displayed elevated levels of demand avoidance (AUT-EDA and AUT-PDA groups), being misunderstood took on a different meaning. Parents described how school staff ‘tried strategies that work with many autistic children but they don’t work with my child’ (AUT-EDA). Another parent described the contrast between the two approaches: ‘When his school tried using strategies that help children with autism, things got worse, anxiety increased and he ended up out of school (signed off with anxiety). Now PDA strategies and support are being used, he is thriving in a large mainstream school’ (AUT-EDA). Indeed, many parents of children in the AUT-EDA and AUT-PDA groups explained how they, themselves, were often made to feel at fault for their children’s behaviour, ‘like a criminal and a liar by the school and the education system’ (AUT-EDA). This apparent parent-blaming caused tensions between parents and the school: ‘School number 4 decided to prosecute me instead of helping us’ (AUT-EDA).
Children masking their difficulties in school. Across all groups, some parents felt that the misunderstanding and mistrust of parents by school staff were rooted in their child’s ability to ‘mask her difficulties in school. School do not see her difficulties cause her anxiety and that could be the cause of the majority of meltdowns after school. They say it’s home but she spends more time in school than with us’ (AUT-EDA). Masking was also believed to be the cause of some children’s needs not being recognised by the school: ‘My daughter totally masked her behaviour at school and right up until the first day she didn’t attend was described as a model pupil. They didn’t understand or believe that she was having often violent meltdowns at home on a nightly basis’ (AUT-EDA).
Parents also described how this masking took its toll on the children (‘my daughter has developed some excellent masking strategies but they drain her of cognitive, social and emotional energy’; AUT) and could have very serious consequences for their mental health (‘Rapid descent into depression, self-harm and suicidal behaviour at start of year 9. Had been masking for many years’; AUT-PDA). This masking seemed to lead to ‘increasing difficulties before/after school’ (AUT-EDA), often resulting in overload (‘He masks his emotions in school but then has overloads at home due to school’; AUT-EDA) and behaviour that challenges (‘My child tries very hard to fit in at school with her peers, almost obsessively so. This results in exhaustion and anxiety at home, and that in turns leads to meltdowns and/or overly rigid or odd behaviour at home, but not at school’; AUT).
Lack of appropriate support available at school. Parents described the ‘constant battle to get support at school’ (AUT-PDA), and the ‘very limited support provided, just enough to make it through the school day but not enough to help with specific areas of difficulty’ (AUT-EDA). Parents provided many potential reasons for this lack of support, including academic achievement (‘because he is achieving reasonably well academically there seems to be very little support available to help him’; AUT), ‘staff shortages’ (AUT-PDA), and a lack of resources (‘school admit struggling but have no more additional resources’; AUT-PDA). Even if several hours of support were provided, parents reported that this support did not necessarily meet their children’s needs: ‘Coping in mainstream even with 32 hours of support is a real struggle most days and school don’t always get it and are not flexible with their approach’ (AUT-PDA).
Children’s anxiety and mental health difficulties were felt to be caused by negative school experiences. Parents described how their children’s mental health issues often resulted from ‘inappropriate, unsupportive early [school] experience[s]’ and caused ‘lasting trauma’ (AUT-EDA). In response to these negative experiences, some parents reported home educating their children, which they felt reduced anxiety: ‘School did not suit him. He is much happier out of it. All the stress of having to deal with the situations gone. Can now concentrate on learning and living’ (AUT). Others echoed this view, suggesting that ‘there has been huge progress in some areas of her development. Her anxiety issues are greatly reduced and so she is more able to complete tasks and concentrate. School was completely wrong for her, home ed is amazing!’ (AUT-EDA).
Educators needing to be flexible in their approach. Some parents of children in the AUT-EDA and AUT-PDA groups questioned whether ‘education’ in any traditional way or sense will ever ‘fit’ my son. Even in a specialist school who understand his complex presentation … everything is still too rigid for him to relax and (mentally/physically) be in a place ready for learning’ (AUT-PDA).
Parents reported some encouraging sentiments, however. For example, some parents of children with a PDA diagnosis felt that their children were able to be engaged in education with the right approach: ‘The mainstream school has had to be very flexible to ensure she keeps attending, and they have offered ‘fun’ sessions to keep her interested’ (AUT-PDA). A greater level of understanding was often the difference between a positive educational experience and a negative one: ‘Her education has been a very varied experience depending on the people who have been around her and their understanding and willingness to support us’ (AUT-PDA).
Discussion
To our knowledge, this is the first study to examine the educational experiences of autistic children with and without elevated EDA behaviours, including those with and without a PDA diagnosis. There were clear parallels in the educational experiences of the AUT, AUT-EDA and AUT-PDA groups, with all reporting overwhelmingly negative school experiences. Notwithstanding these similarities, there were subtle group differences. Quantitatively, these were related primarily to behaviour that challenges. Qualitatively, these were associated with parents’ attributions for their children’s negative school experiences.
Autistic children with an additional PDA diagnosis appeared to be having a more difficult educational experience than those without the diagnosis, even when they displayed similar levels of EDA behaviours (as measured by the EDA-Q). According to their parents, the AUT-PDA group displayed more behaviour that challenges during their most difficult term at school than autistic children without a PDA diagnosis (irrespective of their levels of EDA behaviours). Stuart et al. (Citation2020) identified behaviour that challenges such as aggression, as a ‘last resort’ behavioural response to uncertainty. It is possible that autistic children with an additional PDA diagnosis are responding with aggression when other attempts to reduce uncertainty and control their environment have failed.
While group differences regarding reported exclusions did not reach significance, the high number of fixed term exclusions and the finding that a total of 104 children had been informally excluded from school, is very concerning. Although informal exclusions are not unusual (Atkinson Citation2013; Brede et al. Citation2017; Mccluskey Citation2015; Watling Citation2004), they are illegal in the UK (Deparment for Education, DfE Citation2012). The Department for Education (DfE) in the UK also emphasises that it is unlawful to exclude a child from school due to their special educational needs and that schools have a duty under the 2010 Equality Act to make reasonable adjustments to enable students to access schooling (DfE Citation2012). Nevertheless, disproportionate numbers of pupils with special educational needs are excluded from school (Brede et al. Citation2017; DfE Citation2015; Mccluskey et al. Citation2015; Sproston, Sedgewick, and Crane Citation2017), including high numbers of autistic students (Brede et al. Citation2017). Exclusion from school has been found to be linked to marginalisation (Mccluskey et al. Citation2015) and disrupted education, which can exacerbate existing learning difficulties (Pirrie et al. Citation2011) as well as leading to subsequent social exclusion, unemployment, mental health difficulties and incarceration (Gill, Quilter-Pinner, and Swift Citation2017). As such, the higher rates of informal exclusion of students with a PDA diagnosis have the potential to lead to negative outcomes for these children, not just throughout their education but throughout their life.
It should also be noted that children with an additional PDA diagnosis (the AUT-PDA group) were not alone in experiencing difficulties at school. Parents of those with EDA behaviours (the AUT-EDA group) also reported considerable difficulties. The overwhelmingly negative school experiences reported by the parents of children with EDA behaviours and/or a PDA diagnosis are consistent with existing research in this area. Gore Langton and Frederickson (Citation2016) found that parents of children with PDA reported their children to experience high levels of school exclusions and failed placements, as well as high levels of behaviour that challenges during their most difficult term at school. There have been suggestions that the school difficulties faced by children with EDA are more pronounced than those faced by autistic children without EDA behaviours (PDA Society Citation2018). The current findings provide the first empirical support for this claim.
Parents’ qualitative responses indicated several potential reasons for this pattern. It is important to note that many of these potential factors leading to a negative school experience are factors external to the child and centre instead on the practice and understanding of those around them, particularly the education professionals with whom they interact. Green et al. (Citation2018), Woods (Citation2019) and Ozsivadjian (Citation2020) emphasise the importance of considering the transactional relationship between children and their environment and several aspects of the qualitative findings provide support for this emphasis. First, many parents felt that their children were misunderstood by school staff. A lack of teacher awareness of hidden conditions and disabilities has been raised in the literature with regard to a number of different needs including epilepsy (Bishop and Boag Citation2006), Type 1 diabetes (Fried et al. Citation2018), Attention Deficit Hyperactivity Disorder (ADHD) (Kos, Richdale, and Hay Citation2006) and paediatric brain injury (Linden et al. Citation2013). Brede et al. (Citation2017) also highlight that the hidden nature of some conditions can lead to difficulties being misconstrued as behavioural issues.
Parents in our AUT-EDA and AUT-PDA groups reported that for them and their children, misunderstandings arose due to differences in their children’s presentation, which did not fit the ‘standard’ profile of autistic children. Similar issues have been raised for other minority autistic groups, including girls. Moyse and Porter (Citation2015) found that teachers were unaware of the hidden support needs of autistic girls, which often resulted in them being undersupported in school; Cridland et al. (Citation2014) have also highlighted the need for greater awareness of the needs of autistic girls. These findings suggests that teacher awareness of the varied presentations of autism (including elevated EDA behaviours) may need to be improved, perhaps by adapting teacher training to ensure that teachers are better equipped to understand children’s individual needs and to apply this knowledge in practice.
Second, parents reported their children masking their difficulties at school. Masking (or ‘putting on my best normal’; Hull et al. Citation2017, 2591) is common among autistic children (Cook, Ogden, and Winstone Citation2017) and adults (Hull et al. Citation2017, Citation2020). Here, parents across all three groups reported that masking had a detrimental effect on children’s mental health (see also Cage, Monaco, and Newell Citation2018; Cook, Ogden, and Winstone Citation2017; Lai et al. Citation2017). It is, therefore, imperative that children’s hidden needs are understood both by educators and by the children themselves. Psychoeducation programmes such as PEGASUS (Gordon et al. Citation2015) may also support children and young people to better understand their diagnosis, particularly their profile of strengths and challenges.
Third, parents reported feeling misunderstood, and even blamed, for their children’s difficulties by professionals. Historically, parent blame has been very much part of the discourse surrounding autism (Langan Citation2011; Silverman and Brosco Citation2007; Waltz Citation2015; Wolff Citation2004) and more recent research has reported that parents of autistic children can still feel blamed for their children’s behaviour (e.g. Courcy and des Rivières Citation2017; Neely-Barnes et al. Citation2011; Waltz Citation2015). Gore Langton and Frederickson (Citation2018) suggest that parents of children with EDA may experience similar judgements to those experienced by parents of autistic children before autism became more widely known and understood. The current data suggest that professionals need to work collaboratively with parents to ensure better understanding of children’s complex needs (see also Charman et al. Citation2011). Specialist training for professionals in recognising and meeting autistic children’s varying needs, may also go some way to remedying this issue.
Negative school experiences, across all groups, were reported to have profound consequences, particularly with respect to the children’s mental health. Similar to Brede et al. (Citation2017), many parents in the current study felt that elevated anxiety was a direct consequence of their children’s negative school experiences. While our data cannot demonstrate a causal relationship between anxiety and negative school experiences, elevated anxiety is thought to be a key characteristic of autistic children with EDA behaviours (with or without a diagnosis of PDA; see Christie et al. Citation2012). As such, anxiety might mediate the relationship between EDA behaviours and children’s negative school experiences.
While the data described in this paper cannot speak to the utility of PDA as a diagnostic ‘label’, the findings raise questions about the role the diagnosis plays in enabling school staff to understand and support students who display EDA behaviours. For example, when asked which professional had been the most helpful to them and why, parents (particularly those in the AUT-EDA and AUT-PDA groups) most frequently identified those individuals who had helped them to access a diagnosis for their child. This result concords with the findings of Gore Langton and Frederickson (Citation2018), whose parents felt that their child’s PDA diagnosis led to better support. Given the controversy that exists surrounding the use of PDA as a diagnostic label (Green et al. Citation2018, 2020; Milton Citation2013; Moore Citation2020; Woods Citation2017, Citation2020), an important next step in research will be to examine the extent to which a diagnosis of PDA is perceived as helpful to people and why.
Limitations
There are several limitations of this research. First, the study relied specifically on the views and perspectives of parents, rather than those of educators or, importantly, of children and young people themselves. This was particularly relevant for questions about behaviour that challenges, where parents were identifying the ‘most difficult term’ their children had experienced, an item taken directly from Gore Langton and Frederickson’s (Citation2016) study. Parents’ perception of the most difficult school term may vary from that of the child or their teacher – or even between parents themselves. Caution is warranted when interpreting these particular findings from this questionnaire item. Second, whilst their negative experience of education is consistent with the literature in this area (Ashburner, Ziviani, and Rodger Citation2010; Brede et al. Citation2017; Green et al. Citation2005; Humphrey Citation2015; Humphrey and Symes Citation2010; Rowley et al. Citation2012), the current study, as with previous studies, involved a self-selecting sample. As such, parents whose children have had a more negative experience of education may have been more likely to complete the survey. Nevertheless, there were some respondents who reported having positive schooling experiences. Third, the cross-sectional nature of this study meant that it was not possible to establish causal relationships between EDA behaviours and educational experiences, nor was it possible to establish whether the anxiety reported by many parents was a consequence or a cause of children’s negative school experiences. This is an important direction for future research. Fourth, the SDQ was used to measure children’s emotional and behavioural difficulties in order to facilitate comparison with previous studies of children with EDA behaviours, but caution is warranted given the moderate reliability estimates in our samples. Finally, as we do not have a comprehensive overview of each child’s educational and diagnostic history (or indeed any formal information on their diagnoses), it is not possible to assess to what extent the diagnosis of PDA has enabled, if at all, those children with elevated EDA behaviours to access the support that best meets their needs.
Conclusion
This study highlights the challenges autistic children experience during their education and the particular difficulties that are faced by those with EDA, especially with regard to behaviours that challenge. Further questions remain, however, about whether differential diagnosis can play a role in helping professionals better meet the distinct needs of individual autistic children (see Green et al. Citation2018).
Declaration of interest
One author (CT) provides training and consultancy to schools, colleges and families about supporting the needs of children and young people who display behaviours associated with extreme demand avoidance and volunteers with the PDA Society.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Clare Truman
Clare Truman is a PhD student at the Centre for Research in Autism and Education (CRAE) at the Institute of Education, London. She is a teacher specialising in the education of autistic children who find it difficult to attend school. Her research interests focus on the support needs of children who display extreme demand avoidance and their educational experiences.
Laura Crane
Laura Crane is an Associate Professor at UCL Institute of Education, where she is Deputy Director of the Centre for Research in Autism and Education (CRAE). Her research focuses on understanding the educational experiences of autistic children and young people (in mainstream and special schools), and identifying evidence-based ways to support pupils, their parents and their educators.
Patricia Howlin
Patricia Howlin is Professor of Clinical Child Psychology at the Institute of Psychiatry, Psychology and Neuroscience, King’s College, London. She is a Fellow of the British Psychological Society and Fellow of the International Society for Autism Research. She is currently President of the Society for the Study of Behavioural Phenotypes and was past Chair of the UK Association of Child Psychology and Psychiatry. Her principal research interests focus on the long-term prognosis for individuals with autism spectrum and other developmental disorders and on developing intervention programmes that may help to improve outcomes.
Elizabeth Pellicano
Elizabeth Pellicano is Professor in the Macquarie School of Education at Macquarie University in Sydney and Australian Research Council Future Fellow. She is a developmental cognitive scientist committed to transforming autism science so that it more accurately reflects everyday autistic life. Professor Pellicano trained at the University of Western Australia, before becoming a Junior Research Fellow at the University of Oxford, UK. In 2009, she joined the newly created Centre for Research in Autism and Education (CRAE) at UCL Institute of Education, UK. She became Director of CRAE in 2013 and Professor of Autism Education in 2015.
Notes
1 We define behaviour that challenges as including: refusing to attend or comply; leaving the classroom or school site; and hurting themselves, staff or other pupils. While Gore Langton and Frederickson (Citation2016) describe these as ‘problem behaviours’ (p.255), we have chosen to use the term behaviour that challenges as recommended by NICE (Citation2018) guidelines, emphasising that while the behaviours may challenge others, they may be functional for the individual.
2 Given the fairly large sample, we also conducted supplementary analyses exploring the impact of gender on our results. There were few significant differences between boys, girls and those of other gender identities on most variables, although some differences were noted. First, in the AUT group, only boys experienced informal exclusions, H(2) = 10.60, p = .005. Second, boys in the AUT (H (2) = 9.18, p = .01) and AUT-EDA (H (2) = 8.96, p = .01) groups were more likely than girls and those of other gender identities to hurt or attempt to hurt other pupils.
References
- American Psychiatric Association. 2013. Diagnostic and Statistical Manual of Mental Disorders 5th ed. (DSM-5), Washington, DC: American Psychiatric Association Publishing.
- Ashburner, J., J. Ziviani, and S. Rodger. 2010. “Surviving in the Mainstream: Capacity of Children with Autism Spectrum Disorders to Perform Academically and Regulate Their Emotions and Behavior at School.” Research in Autism Spectrum Disorders 4 (1): 18–27. doi:10.1016/j.rasd.2009.07.002.
- Atkinson, M. 2013. Always Someone Else’s Problem: Office of the Children’s Commissioner’s Report on Illegal Exclusions. London: Office of the Children’s Commissioner for England.
- Bishop, M., and E. M. Boag. 2006. “ Teachers’ Knowledge About Epilepsy and Attitudes Toward Students with Epilepsy: Results of a National Survey.” Epilepsy & Behaviour 8 (2): 397–405.
- Braun, V., and V. Clarke. 2006. “Using Thematic Analysis in Psychology.” Qualitative Research in Psychology 3 (2): 77–101. doi:10.1191/1478088706qp063oa.
- Brede, J., A. Remmington, L. Kenny, K. Warren, and E. Pellicano. 2017. “Excluded from School: Autistic Students’ Experiences of School Exclusion and Subsequent Re-Intergration Into School.” Autism and Developmental Language Impairments 2: 1–20. doi:10.1177/2396941517737511.
- Bruni, T. 2014. “Test Review: Social Responsiveness Scale–Second Edition (SRS-2).” Journal of Psychoeducational Assessment 32: 365–369. doi:10.1177/0734282913517525.
- Cage, E., J. Di Monaco, and V. Newell. 2018. “Experiences of Autism Acceptance and Mental Health in Autistic Adults.” Journal of Autism and Developmental Disorders 48: 473–484. doi:10.1007/s10803-017-3342-7.
- Charman, T., L. Pellicano, L. V. Peacey, N. Peacey, K. Forward, and J. Dockrell. 2011. What is Good Practice in Autism Education? London: Autism Education Trust.
- Christie, P. 2007. “The Distinctive Clinical and Educational Needs of Children with Pathological Demand Avoidance Syndrome: Guidelines for Good Practice.” Good Autism Practice Journal 8 (1): 3–11.
- Christie, P., M. Duncan, R. Fidler, and Z. Healy. 2012. Understanding Pathological Demand Avoidance Syndrome in Children: A Guide for Parents, Teachers and Other Professionals. London: Jessica Kingsley Publishers.
- Constantino, J. N., and C. P. Gruber. 2012. Social Responsiveness Scale. 2nd ed. Los Angeles, CA: Western Psychological Services.
- Cook, A., J. Ogden, and N. Winstone. 2017. “Friendship Motivations, Challenges and the Role of Masking for Girls with Autism in Contrasting School Settings.” European Journal of Special Needs Education 33 (3): 302–315. doi:10.1080/08856257.2017.1312797.
- Courcy, I., and C. des Rivières. 2017. ““from Cause to Cure”: A Qualitative Study on Contemporary Forms of Mother Blaming Experienced by Mothers of Young Children with Autism Spectrum Disorder.” Journal of Family Social Work 20 (3): 233–250. doi:10.1080/10522158.2017.1292184.
- Cridland, E. K., S. C. Jones, P. Caputi, and C. Magee. 2014. “Being a Girl in a Boys’ World: Investigating the Experiences of Girls with Autism Spectrum Disorders During Adolescence.” Journal of Autism and Developmental Disorders 44: 1261–1274. doi:10.1007/s10803-013-1985-6.
- Department for Education. 2012. Exclusion from Maintained Schools, Academies and Pupil Referral Units in England: A Guide for Those with Legal Responsibilities in Relation to Exclusion. London: Department for Education.
- Department for Education. 2015. Permanent and Fixed Period Exclusions in England: 2013 to 2014. London: Department for Education.
- Fidler and Christie. 2019. Collaborative Approaches to Learning for Pupils with PDA: Strategies for Education Professionals. London: Jessica Kingsley Publishers.
- Fried, L., R. Vithiatharan, E. Davis, T. Jones, K. Hancock, K. Runions, D. Cross, etal. 2018. “The school experiences of children and adolescents with type 1 diabetes in Western Australia.” Issues in Educational Research 28 (3): 578–595.
- Gill, K., H. Quilter-Pinner, and D. Swift. 2017. Making the Difference: Breaking the Link Between School Exclusion And Social Exclusion. London: Institute for Public Policy Research.
- Gillberg, C., I. C. Gillberg, L. Thompson, R. Biskupsto, and E. Billstedt. 2015. “Extreme (“Pathological”) Demand Avoidance in Autism: a General Population Study in the Faroe Islands.” European Child and Adolescent Psychiatry 24: 979–984. doi:10.1007/s00787-014-0647-3.
- Goodman, R. 1997. “The Strengths and Difficulties Questionnaire: A Research Note.” Journal of Child Psychology and Psychiatry 38: 581–586.
- Gordon, K., M. Murin, O. Baykaner, L. Roughan, V. Livermore-Hardy, D. Skuse, and W. Mandy. 2015. “A Randomised Controlled Trial of PEGASUS, a Psychoeducational Programme for Young People with High-Functioning Autism Spectrum Disorder.” Journal of Child Psychology and Psychiatry 56: 468–476. doi:10.1111/jcpp.12304.
- Gore Langton, E., and N. Frederickson. 2016. “Mapping the Educational Experiences of Children with Pathological Demand Avoidance.” Journal of Research in Special Educational Needs 16 (4): 254–263. doi:10.1111/1471-3802.12081.
- Gore Langton, E., and N. Frederickson. 2018. “Parents’ Experiences of Professionals’ Involvement for Children with Extreme Demand Avoidance.” International Journal of Developmental Disabilities 64 (1): 16–24. doi:10.1080/20473869.2016.1204743.
- Green, J. 2020. “Commentary: Anxiety and Behaviour in and Beyond ASD; Does the Idea of ‘PDA’ Really Help? – a Commentary on Stuart et al. (2020).” Child and Adolescent Mental Health 25: 74–76. doi:10.1111/camh.12379.
- Green, J., M. Absoud, V. Grahame, O. Malik, E. Simonoff, A. Le Couteur, and G. Baird. 2018. “Pathological Demand Avoidance: Symptoms But Not A Syndrome.” The Lancet: Child and Adolescent Health 2 (6): 455–464. doi:10.1016/S2352-4642(18)30044-0.
- Green, H., A. McGinnity, H. Meltzer, T. Ford, and R. Goodman. 2005. Mental Health of Children and Young People in Great Britain. Hampshire: Palgrave Macmillan.
- Hull, L., M.-C. Lai, S. Baron-Cohen, et al. 2020. “ Gender Differences in Self-Reported Camouflaging in Autistic and non-Autistic Adults.” Autism 24 (2): 352–363. doi:10.1177/1362361319864804.
- Hull, L., K. V. Petrides, C. Allison, P. Smith, S. Baron-Cohen, M. C. Lai, and W. Mandy. 2017. ““Putting on My Best Normal”: Social Camouflaging in Adults with Autism Spectrum Conditions.” Journal of Autism and Developmental Disorders 47: 2519–2534. doi:10.1007/s10803-017-3166-5.
- Humphrey, N.2015. Autism and Education Volume One: Key Perspectives and Themes in Autism Education. London: Sage.
- Humphrey, N., and W. Symes. 2010. “Perceptions of Social Support and Experience of Bullying among Pupils with Autistic Spectrum Disorders in Mainstream Secondary Schools.” European Journal of Special Needs Education 25 (1): 77–91. doi:10.1080/08856250903450855.
- Kos, j. M., A. L. Richdale, and D. A. Hay. 2006. “Children with Attention Deficit Hyperactivity Disorder and Their Teachers: A Review of the Literature.” International Journal of Disability, Development and Education 53 (2): 147–160. doi:10.1080/10349120600716125.
- Lai, M.-C., M. V. Lombardo, A. N. Ruigrok, B. Chakrabarti, B. Auyeung, P. Szatmari, F. Happé, and S. Baron-Cohen. 2017. “Quantifying and Exploring Camouflaging in Men and Women with Autism.” Autism 21 (6): 690–702. doi:10.1177/1362361316671012.
- Langan, M. 2011. “Parental Voices and Controversies in Autism.” Disability & Society 26 (2): 193–205. doi:10.1080/09687599.2011.544059.
- Linden, M. A., H.-J. Braiden, and S. Miller. 2013. “Educational Professionals’ Understanding of Childhood Traumatic Brain Injury.” Brain Injury 27 (1): 92–102. doi:10.3109/02699052.2012.722262.
- Malik, O., and G. Baird. 2018. “Commentary: PDA - What's in a Name? Dimensions of Difficulty in Children Reported to Have an ASD and Features of Extreme/Pathological Demand Avoidance: a Commentary on O'Nions et al. (2017).” Child and Adolescent Mental Health 23: 387–388. doi:10.1111/camh.12273.
- Mayring, P. 2015. “Qualitative Content Analysis: Theoretical Background and Procedures.” In Approaches to Qualitative Research in Mathematics Education. Advances in Mathematics Education, edited by A. Bikner-Ahsbahs, C. Knipping, and N. Presmeg, 365–380. Dordrecht: Springer.
- Mccluskey, Gillean, Sheila Riddell, Elisabet Weedon, and Mariela Fordyce. 2015. “Exclusion from School and Recognition of Difference.” Discourse: Studies in the Cultural Politics of Education 37: 1–11. doi:10.1080/01596306.2015.1073015.
- Milton, D. 2013. ‘Nature’s Answer to Over-Conformity’: Deconstructing Pathological Demand Avoidance, Autism Experts Online. Accessed 05.05.20. https://kar.kent.ac.uk/62694/.
- Moore, A. 2020. “Pathological Demand Avoidance: What and Who Are Being Pathologised and in Whose Interests?” Global Studies of Childhood 10 (1): 39–52. doi:10.1177/2043610619890070.
- Moyse, R., and J. Porter. 2015. “ The Experience of the Hidden Curriculum for Autistic Girls at Mainstream Primary Schools.” European Journal of Special Needs Education 30 (2): 187–201. doi:10.1080/08856257.2014.986915.
- Neely-Barnes, S. L., H. R. Hall, R. J. Roberts, and J. C. Graff. 2011. “Parenting a Child With an Autism Spectrum Disorder: Public Perceptions and Parental Conceptualizations.” Journal of Family Social Work 14 (3): 208–225. doi:10.1080/10522158.2011.571539.
- Nelson, A. T., C. Lopata, M. A. Volker, M. L. Thomeer, J. A. Toomey, and E. Dua. 2016. “Exploratory Factor Analysis of SRS-2 Teacher Ratings for Youth with ASD.” Journal of Autism and Developmental Disorders 46: 2905–2915. doi:10.1007/s10803-016-2822-5.
- Newson, E., and K. Le Marechal. 1998. Pathological Demand Avoidance Syndrome, presented at Durham Conference Psychobiology of Autism: current research and practice. Accessed 04.05.20. https://www.autismeastmidlands.org.uk/wp-content/uploads/2016/10/PDA-discriminant-functions-analysis.pdf.
- Newson, E., Kate Le Marechal, and C. David. 2003. “Pathological Demand Avoidance Syndrome: A Necessary Distinction Within the Pervasive Developmental Disorders.” Archives of Disease in Childhood 88: 595–600. doi:10.1136/adc.88.7.595.
- NICE. 2018. Learning disabilities and behaviour that challenges: service design and delivery: NICE guideline NG93, London: National Institute for Health and Care Excellence (NICE).
- O’Nions, E., P. Christie, J. Gould, E. Viding, and F. Happe. 2014. “Development of the ‘Extreme Demand Avoidance Questionnaire’ (EDA-Q): Preliminary Observations on a Trait Measure for Pathological Demand Avoidance.” Journal of Child Psychology and Psychiatry 55 (7): 758–768. doi:10.1111/jcpp.12149.
- Ozsivadjian, A. 2020. “Editorial: Demand Avoidance — Pathological, Extreme or Oppositional?” Child and Adolescent Mental Health 25: 57–58. doi:10.1111/camh.12388.
- PDA Society. 2018. Being Misunderstood: Experiences of the Pathological Demand Avoidance Profile of ASD. Accessed 05.05.20. https://www.pdasociety.org.uk/resources/2018-summary/.
- PDA Society. n.d. Diagnosing PDA available online at https://www.pdasociety.org.uk/what-is-pda-menu/diagnosing-pda/.
- Pirrie, A., G. Macleod, M. A. Cullen, and G. McCluskey. 2011. “What Happens to Pupils Permanently Excluded from Special Schools and Pupil Referral Units in England?” British Educational Research Journal 37: 519–538. doi:10.1080/01411926.2010.481724.
- Rowley, E., S. Chandler, G. Baird, E. Simonoff, A. Pickles, T. Loucas, and T. Charman. 2012. “The Experience of Friendship, Vicitimization and Bullying in Children with an Autism Spectrum Disorder: Associations with Child Characteristics and School Placement.” Research in Autism Spectrum Disorders 6 (3): 1126–1134. doi:10.1016/j.rasd.2012.03.004.
- Sherwin, J. 2015. Pathological Demand Avoidance Syndrome: My Daughter Is Not Naughty. London: Jessica Kingsley Publishers.
- Silverman, C., and J. P. Brosco. 2007. “Understanding Autism: Parents and Pediatricians in Historical Perspective.” Archives of Pediatrics and Adolescent Medicine 161 (4): 392–398. doi:10.1001/archpedi.161.4.392.
- Simonoff, E., C. R. G. Jones, and G. Baird. 2013. “The Persistence and Stability of Psychiatric Problems in Adolescents with Autism Spectrum Disorders.” Journal of Child Psychology and Psychiatry 54 (2): 186–194. doi:10.1111/j.1469-7610.2012.02606.x.
- Sproston, K., F. Sedgewick, and L. Crane. 2017. “ Autistic Girls and School Exclusion: Perspectives of Students and Their Parents.” Autism & Developmental Language Impairments 2), doi:10.1177/2396941517706172.
- Stuart, L., V. Grahame, E. Honey, and M. Freeston. 2020. “Intolerance of Uncertainty and Anxiety as Explanatory Frameworks for Extreme Demand Avoidance in Children and Adolescents.” Child and Adolescent Mental Health 25: 59–67. doi:10.1111/camh.12336.
- Waltz, M. M. 2015. “Mothers and Autism: The Evolution of a Discourse of Blame.” AMA Journal of Ethics 17 (4): 353–358. doi:10.1001/journalofethics.2015.17.4.mhst1-1504.
- Watling, R. 2004. “Helping Them Out.” Emotional and Behavioural Difficulties 9 (1): 8–27. doi:10.1177/1363275204038258.
- Wolff, S. 2004. “The History of Autism.” European Child & Adolescent Psychiatry 13 (4): 201–208. doi:10.1007/s00787-004-0363-5.
- Woods, R. 2017. “Pathological Demand Avoidance: My Thoughts on Looping Effects and Commodification of Autism.” Disability and Society 32 (5): 753–758. doi:10.1080/09687599.2017.1308705.
- Woods, R. 2019. “ Demand Avoidance Phenomena: Circularity, Integrity and Validity – a Commentary on the 2018 National Autistic Society PDA Conference.” Good Autism Practice 20 (2): 28–40.
- Woods, R. 2020. “Commentary: Demand Avoidance Phenomena, A Manifold Issue? Intolerance of Uncertainty and Anxiety as Explanatory Frameworks for Extreme Demand Avoidance in Children and Adolescents – a Commentary on Stuart et al. (2019).” Child and Adolescent Mental Health. 68–70.
- World Health Organisation. 2018. ICD-11 International Classification of Diseases for Mortality and Morbidity Statistics Eleventh Revision. Geneva: World Health Organisation.