ABSTRACT
Attention-Deficit/Hyperactivity Disorder (ADHD) is a common neurodevelopmental condition. As such most schools, Further Education colleges, vocational training and Higher Education settings will need to support affected children and young people. When young people who require ongoing treatment for ADHD are around 18 years of age, they must transition from child to adult mental health services. However, only a small proportion successfully transition. As significant educational transitions are often happening at the same time, there is a need to consider how education and health service transitions may impact on one another. This paper presents findings from a large UK qualitative study involving 144 semi-structured interviews with young people who had ADHD, parents and health professionals.
Two themes were identified which support the notion that education transition can impact health transition. Firstly, transition to adult health services typically requires continued prescription of ADHD medication, yet many young people stop taking their medication due to a belief that it is only needed for education-based learning. Secondly, if a young person is continuing education post-18, a lack of joined-up planning between education and health (outside of special schools) or consistent support in Higher/Further Education can leave young people with ADHD in limbo between health services and struggling within education.
Given these findings, we recommend regarding multi-agency service statutory health care transition, educational staff training and ongoing oversight of child to adult health service and adult to adult health service transition effectiveness.
Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) is a common neurodevelopmental condition with a worldwide pooled prevalence of 3.4% (CI 95% 2.6–4.5) (Polanczyk et al. Citation2015). This suggests that most schools, Further Education (FE) colleges and Higher Education (HE) settings will include a significant minority of affected children and young people. There is considerable variation in the strengths and difficulties experienced by children with ADHD (Faraone et al. Citation2015), but the core components of the syndrome comprise inattention, hyperactivity and/or impulsivity (American Psychiatric Association Citation2013). Other common problems include difficulties with decision-making, time-management and multi-tasking (Mahdi et al. Citation2017). Those who experience one or more of these difficulties and problems can find aspects of home and school environments challenging. For example, young people with ADHD often struggle to complete academic tasks (Smith et al. Citation2020) and even with medication are at a higher risk of poorer education and health outcomes than those without ADHD (Fleming et al. Citation2017). Diagnosis of ADHD involves a mental health clinician interpreting whether attention span, and activity plus impulsivity levels are within a normal range for developmental stage. This dimensionality (whilst not unique to ADHD) can add to the debate regarding the existence of ADHD and whether medication is necessary, but is not confined to ADHD; for example high blood pressure and obesity are likewise normally distributed (Wedge Citation2015). Further, recent evidence suggests a dose response between the duration of medication and school performance, including academic attainment; those on medication for longer do better at the end of compulsory school (Jangmo et al. Citation2019).
Young people who require ongoing treatment for ADHD into early adulthood must transition from child and adolescent mental health services (CAMHS) or from community paediatrics to adult mental health services (AMHS). These transitions are likely to be impacted by prior education experience because interventions are often tried at school, both before and while on medication. As these young people are between the ages of 17–19 years, and could be early or late in this range, they will often also experience the educational transitions from school to sixth form, FE, vocational training or university settings at around the same time (Ford Citation2020). To better understand the transition from child to adult healthcare, we need to consider other transitions that are occurring for young people at this time and how they may impact one another.
The National Institute for Health and Care Excellence (NICE Citation2019), Department for Education (DfE, Department for Education Citation2015) and Department of Health (DoH) (Department for Education and Department of Health Citation2015) provide guidance for those that work in health and educational settings regarding the support of young people with ADHD. NICE recommends that CAMHS or paediatric services provide diagnosis, transition and symptom change information to schools, colleges and universities, and before prescribing medication review the young person’s mental health, physical health and social circumstances and attempt environmental adaptations such as those that relate to seating, lighting and distractions (NICE Citation2019). NICE also recommends that multi-agency ADHD groups provide training and information for teachers about ADHD and the management of related behaviours (NICE Citation2019).
Young people with ADHD up to 25 years of age may qualify for an education, health and care (EHC) plan if they have complex needs. The Special Educational Needs and Disabilities (SEND) code of practice seeks to ensure those with EHC plans have high quality support in a number of ways, such as involving these young people in discussions about their support and ensuring services, including those who work in education, integrate to provide it (Department for Education and Department of Health Citation2015). The Department for Education (Citation2015) statutory guidance states that all school and college staff are responsible for providing support as soon as safeguarding and welfare problems emerge at any point in a child’s life. As the features of ADHD may undermine young people’s ability to cope with transitions, they are likely to need high quality multi-agency support when moving from one educational setting to another. Therefore, educational and healthcare transitions should be considered together, and the role of education in young people’s experience of their healthcare transition explored.
At its most basic, optimal transition is defined as continuity of care that is supported by a period of joint management, planning meetings, and information sharing (Paul et al. Citation2013; NICE Citation2019) However, only 6% of those who transition from CAMHS to AMHS receive an ‘optimal’ healthcare service transition (Eke et al. Citation2019). Young people with ADHD often ask for medication to help with their educational progress (Newlove-Delgado et al. Citation2018) and pharmacological treatments for ADHD are associated with increases in school performance (Jangmo et al. Citation2019). Undergraduate students report medication helps them academically (Advokat, Lane, and Luo Citation2011), although many young people feel they have limited opportunities to discuss their medical condition and aspects of their learning with teachers (Singh Citation2012). Additionally, many more young adults would like to access ongoing psychological and social support, even if they no longer want or need medication (Janssens et al. Citation2020). The demands on attention and concentration of many courses in HE, training or employment mean that access to medication is important for those who still require it to function.
A minimum estimate for the number of 17–19-year-olds per year with ADHD who require transition to AMHS for ongoing medication in the British Isles lies between 202 and 511 per 100,000 (Janssens et al. Citation2020). With the average annual number of 18-year-olds in the UK predicted to exceed 700,000 per year (Office for National Statistics Citation2018), this results in an estimate of over 1,400 young people with ADHD annually needing service transition for medication.
The transition from post-16 educational settings to HE is a challenge for those with ADHD and for the staff of these institutions (IES Citation2019). Young people diagnosed with ADHD are at greater risk of lower educational attainment than those without ADHD (Jangmo et al. Citation2021). Compared to other young people with SEN, those with ADHD attending FE college are less likely to do academic courses, such as A Levels, and are least satisfied with their school’s support in preparation for adult life (Polat, Kalambouka, and Boyle Citation2001). Support from educational settings may reduce academic failure and drop out, and boost attainment (Kuriyan et al. Citation2013). School counsellors can facilitate the development of successful strategies and interventions such as a transition file to prepare young people for moves between educational settings (Schwiebert, Sealander, and Dennison Citation2011). University health support departments have found clinical transition reports help determine accommodations both from academic and social preparedness perspectives (Wadlington Citation2012). Therefore, optimal transition involves factoring in changes in educational setting, and all stakeholders need to understand the issues that young people with ADHD face during this period of their lives.
The meaning of transitions in terms of the lives of young people, the nature of the institutions they engage with, and how policy makers can allocate resources efficiently, are a worthy topic of research (Bynner Citation2001). The perspectives of practitioners, carers and young people are all important (Kern Citation2011) and the importance of advocacy for young people with ADHD has been highlighted (Ascherman and Shaftel Citation2017). However, a systematic review of child to adult health care transitions found that detailed descriptions of transition processes were limited and called for more youth and parent feedback (Phabinly et al. Citation2017).
CATCh-uS was a UK mixed methods NIHR study carried out between 2016 and 2019 (Janssens et al. Citation2020) that explored the transition of young people with ADHD from child to adult health services. CATCh-uS included a qualitative stream to explore how stakeholders (young people, parents, clinicians and General Practitioners (GPs)) experienced healthcare transitions, and to identify factors that influence the quality and experience of transition. As part of an overarching theme which recognised that successful transition depended on how invested stakeholders were in the ongoing treatment for young adults, we identified two sub-themes which highlighted the influence of education transition on health transition (Janssens et al. Citation2020). To raise further awareness of these findings, in this paper, we expand our description of these two themes, discuss the findings within educational policy contexts and suggest recommendations to improve interactions between education and health care systems to support young people with ADHD to successfully transition between education institutions, employment and health services.
Methods
The methodology for this stream of the CATCh-uS study is described in detail elsewhere (Janssens et al. Citation2020) and summarised briefly below.
Participants
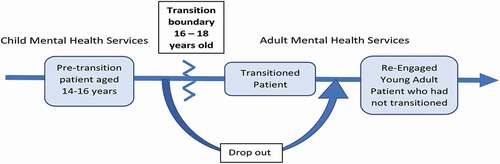
The CATCh-uS study recruited three key stakeholder groups: health professionals, young people with ADHD and parents. The health professionals were clinicians from specialist child and adult health services, and primary care (GPs), who all supported young people with ADHD. The young people with ADHD were at three different stages of transition; before (pre-transition), those who transitioned successfully (defined as a referral being made, accepted, and first adult service appointment attended (Janssens et al. Citation2020)) and those who re-engaged with services after a gap of at least one year (see ).
Figure 1. Three groups of young people representing different stages in the transition process (adjusted from Janssens et al. Citation2020)
Ethical approval for the qualitative stream of the CATCh-uS study was granted by National Research Ethics Service South Yorkshire Ethics Committee: Yorkshire & The Humber (Research Ethics Committee (REC) Reference: 15/YH/0426) and the University of Exeter Medical School Research Ethics Committee (REC Application Number: 15/07/070). Given the potential vulnerability of participants the interviewers were conducted by researchers with current Good Clinical Practice training certificates, and NHS research passports. Before interviews, the interviewer (HE/AP/AJ/TND) discussed the study with the participant who was then given the opportunity to ask any questions. Once the participant had decided to continue with the interview, they were asked to sign the consent form. Parents of young people 15 years old or younger were asked to consent for participation of their child, and assent was also sought from the young person.
Sampling and recruitment strategy
CATCh-uS used purposive sampling to ensure that a breadth of experiences were represented with recruitment of parents and young people 1) from different geographical locations and NHS Trusts with a range of adult ADHD service provision; 2) both males and females; 3) with and without co-morbidities; 4) living with or away from parents; 5) in and out of education settings. The NHS trusts’ provision for adults with ADHD ranged from no formal service to highly specialist clinics taking regional and national referrals. The sampling frame for paediatricians, and child or adult mental health practitioners mirrored the geographical and service spread, while that for General Practitioners (GPs) also sought differing practices e.g., working in student practices, special interest in ADHD, and roles e.g. mental health, and commissioning (Newlove-Delgado et al. Citation2019). CATCh-uS aimed to conduct 20–25 interviews from each stakeholder group to reach saturation (Guest, Bunce, and Johnson Citation2006), but included a mid-recruitment break to assess ‘saturation level’.
CATCh-uS data collection
CATCh-uS used semi-structured interviews based on topic guides which were informed by NICE transition guidelines, the CATCh-uS project Patient and Public Involvement (PPI) group and existing research (Janssens et al. Citation2020). These were adjusted to reflect the stakeholder group so that the interviews with young people and parents covered current and future medication use and contact with services, while those with practitioners covered pre-transition dropout, questions of who was involved in transition, transition re-entry, and management of young people in transition in primary care.
The focus was not on young people’s experiences of education. Only one question in the young people pre-transition topic guide referred to school. They were asked, ‘Do you think you will still need help or support for your ADHD after you leave school?’ Yet, in response to other questions, for example about when and how they were diagnosed, what kind of support they received and what made YP decide to try and get help as an adult, parents and all three groups of young people frequently mentioned school.
Clinicians working in child services and adult services were asked about their experiences of working with schools or the education system during the service transition, through the following questions: ‘Who is usually involved in the transition process?’, ‘what would transition for your ADHD patients look like in an ideal world?’, and probing questions: ‘Is there any involvement from non-health services, e.g. education or social services’?” The topic guide for GPs did not contain any questions mentioning education although this was a topic they raised (Newlove-Delgado et al. Citation2019), for example in answer to the question ‘what role do you have in that transition or in supporting that patient?’ Interviews were recorded and transcribed verbatim. Quotes are highlighted in italics and are labelled with stage of transition for young people’s interviews.
CATCh-uS analysis
Data analysis used a thematic qualitative analysis following a Framework Analysis (FA) approach (Gale et al. Citation2013). Interviews from all seven groups were double coded and the summaries of each code and emerging themes were created. The analysis team (AJ, AP, HE, TND and SB) worked systematically through the texts to identify topics and patterns; through FA an additional layer was added resulting in separate summary matrices for each stakeholder group (except for GPs, who were recruited later and analysed separately). These were used to compare and contrast, identify patterns or links, and to provide explanations of the findings (Ritchie, Lewis, and Elam Citation2003). This approach is open to external scrutiny and is replicable due to the systematic nature of the process.
Extracting the findings of relevance to education institutions
Building on the identified themes from the CATCh-uS analysis as reported in the report for the NIHR (Janssens et al. Citation2020) SBC and SBM completed a critical review of all stakeholder’s matrices (resulting from the FA) with a focus on education in the broad sense, including aspects such as behaviour at school, teachers’ support and dealing with homework. This material was narratively synthesised and presented with the objective of contributing knowledge for the educational and policy contexts.
Results
CATCh-uS interviewed a total of 64 young people (see ), 36 of whom disclosed comorbidities, 25 reported none and 3 were unknown. These comorbid difficulties included Autism Spectrum Disorder (ASD), Anxiety, Depression, Dyslexia, Dyspraxia, Learning Disability, Cerebral Palsy, Obsessive Compulsive Disorder (OCD), Tourette’s syndrome, and behavioural difficulties. Twenty-eight interviews took place with parents (27 mothers and 3 fathers, as some were joint interviews) who had children with ADHD from all three stages of transition. CATCh-uS interviewed 52 clinicians; 22 were from young person’s services (15 paediatricians, 7 psychiatrists); 16 from adult mental health services; and 14 GPs. The GPs included two working in university student practices, two who had a mental health lead role or special interest, and one who had an additional commissioning role, while the adult mental health practitioners had a range of roles (7 psychiatrists, 2 psychologists, 1 nurse prescriber, 1 mental health nurse, 5 unknown).
Table 1. Young people with ADHD participant details
Perspectives of transition from child to adult health services which referenced aspects of education were common and clearly articulated across the different groups interviewed, although to a lesser extent by GPs and clinicians working in adult services. The following two themes were identified (see ): ADHD – medication: a means to an end and The influence of educational setting upon health service transition.
Table 2. Themes and key elements
Theme 1. ADHD – medication: a means to an end
Most young people interviewed were prescribed medication to treat their ADHD. The beneficial effects of, adjustment to and withdrawal of medication and their links to education were discussed in many interviews.
Young people often reflected on the link between taking medication and improved concentration and academic achievement. Many young people reported a need to take medication for its educational benefits. One 16-year old schoolboy stated: ‘To help me get qualifications, get the grades I need, help me concentrate. Because I don’t take them at weekends.’ (Pre-service transition) and a 21-year old male in voluntary work said: ‘ … I mainly took them just for school because I wanted to be able to concentrate, sit down and be able to work.’ (Re-engaged with services). Additionally, one parent of a 16-year old schoolboy reported that their child’s college insisted they take medication, ‘They’ve actually said that they don’t want him in the college if he’s not medicated.’ (Pre-service transition). One 17-year old employed female decided to not apply to university, as she had not found a medication that would help her in that environment, I don’t think I’d cope with that learning … If I’d found an ADHD medication that works by now then maybe I would be considering it. (Transitioned)
Many of those young people with ADHD who were studying and taking exams and other assessments at sixth form or FE college wanted to continue their medication. As this would take them beyond the boundary for child health services, to continue accessing medication they would need to transition to adult mental health services. This desire to continue medication was encapsulated by this 18-year old female HE student,
Because I get quite bad stress anyway so around say exam time obviously I have to be taking those tablets [for ADHD] because I have to be on the ball like revising and everything, A Levels have been pretty horrible and intense so I have to be taking them. (Transitioned)
Young people’s relationship with medication and learning was described as being ‘invested’ by one adult clinician,,
It’s really interesting, young people, they need to be invested in their medication, so if they are going on to higher education or they have an apprenticeship then they are more invested, they are more likely to keep taking it.
Clinicians working in children’s services often introduced aspects of education as factors in their decisions regarding medication dosage levels and withdrawal, which seemed to match the perspective of young people that medication was for learning. For example, ‘I had a few kids who had twice the dose for school-work days and half a dose for recreation or weekend days’, and ‘ … we do obviously give drug holidays for weekends and children that are doing well during half-term and things, let them run a bit wild when it doesn’t matter, they’re not learning anything.’ The withdrawal of medication process was exemplified by this clinician, ‘ … once they are past GCSEs and they have done their exams then we would try to wean the medication down and see how they manage without it, but over a long period of time.’
Young people who had recently transitioned to adult ADHD services reported seeing a future where symptoms would improve once formal education was over, as this 21-year old male voluntary worker put it,
Like I say, for the sake of school, that’s what I was taking them for really. So, I was kind of excited, well not excited, but waiting to finish school so I wouldn’t have to take them. (Re-engaged with services)
GPs also discussed how adjustment of dosage reflected the changing demands of a young person’s educational provision or setting, for example,
… so sometimes they go on holiday or students will often take it at times of stress when they’ve got to revise or have got a lot of coursework and then don’t take it then for two or three weeks or months … So I give them the option – We can taper it off and you can see how you are without it.
One 27-year old male, who had just finished university, felt that based on his experiences, young people with ADHD would benefit from continued healthcare support for their ADHD, including medication. His perspective was that consistent support would help them overcome challenges related to transitioning into different educational settings. He explains,
More than just it being difficult to concentrate, it’s the other stuff that goes along with the attention deficit disorder that makes it quite tricky. So I think that just having the support would be enough to make kids go, “Yeah, I’m going to go to college. I’m going to do really well. I’m going to go to university.” Because I’ve done fucking well at university, and I think other kids could do better. (Re-engaged with services)
Theme 2. The influence of educational setting upon health service transition
Transition from child to adult health services typically took place while the young people were attending an educational setting. Practitioners often highlighted consequences of transitions and links to aspects of education that young people or their parents did not. These related to inconsistencies in transition approaches and the added complication of temporary relocations for post-18 education provision.
Transition inconsistencies
This clinician working in children’s services highlighted how in some cases young people have to fend for themselves in the transition process,
… so many catastrophic changes happened at 16 to 18. Parents are kicked out by statute; they [young people] become legally responsible for their misdemeanours. So, a lot of my kids graduated to prison. … I think it’s true of virtually every case I ever saw, that transition was particularly difficult.
The important role played by FE college or school sixth form staff in the lead-up to the transition to adult services was emphasised by a 21-year old unemployed male when he said,
So although SENCo [special educational needs co-ordinator] at school is great, you don’t have that support outside school … my teacher for seven years prior to being sixth form head … he knew a lot about me and my ADHD. Yes. He was quite helpful. (Transitioned).
Clinicians and others stated that school staff played a limited role or no role and were perceived not to be involved during transfer to adult services. A child clinician stated,
… the kids that I see that are on medication but have no other specific needs, they are not in special school, I would lead on [transition] and there’s nobody else particularly [in education or elsewhere] who would be following these kids up or who need to know about it, … it’s simply a case of telling the GP and referring on to the adult services.
Some clinicians viewed joint handovers including school staff as an ideal, however special schools, who support those with particular needs not always seen in mainstream education settings, were reported to manage transitions well for complex cases, as this child clinician stated,
So for those young people who are at special schools there’s a whole process that is led by the school and it is a multiagency process. But I think the less complex a young person, the less considered the process is.
This clinician working in children’s services highlighted that the lack of joint handovers related to NICE guidelines and education,
I will put in one particular bugbear which is that they [NICE guidelines] don’t cover education which is just a massive limitation of their usefulness.
Added complication of leaving home for education
Young people who relocated were often left in limbo between services, particularly if going to university when the potential for two addresses could result in interruptions to their medication and inconsistent support that could undermine their ability to cope. Clinicians described relocations to continue their studies as adding a layer of complexity to transition,
Because there’s obviously a danger of it [service transition] crashing. …, the additional complication which I haven’t found a solution for is, the majority of these young people are moving on to some sort of out of town experience, ideally college or university. So, there’s often an address move to temporary student accommodation and then introduces the whole layers of complexity of who is going to prescribe then? (GP)
So, a lot of people turn up [at university] having not transitioned to adult services … And then of course you get some people who just rock up having been at university for two months and say, ‘I’ve run out of my medication; can I have some more? (GP)
In some cases, young people were held up by a lack of coordination within funding administration. Gap years too could make transition more challenging,
It took me about a year and a half to transfer this seventeen-and-a-half-year-old referred this one about six months ago and they still haven’t received the confirmation of funding from our CCG [clinical commissioning group] (clinician working in children’s services)
… this child to adult bit, we’ve often a gap in the middle where they’ve been on a gap year or something, can make it much harder to get everything set up as soon as possible when they get to university. (GP)
Across different sample groups, participants reported that the support within universities for young people with ADHD varied.
… ultimately at university it wasn’t the GPs that supported me, they just gave me the diagnosis and the prescription for the medication, but it was my university that then acted upon that, gave me a learning assessment and helped me speak to my tutors and get a learning support plan put in place. (Re-Engaged with services)
So far, I haven’t successfully had any engagement with a [university] Student Health Service that have taken on the supervision of this [relocating to university and service transition]. (clinician working in children’s services)
Discussion
Our expansion of the CATCh-uS study findings highlight how education transition and health transition can influence each other.
Beliefs regarding medication only needed for school-based learning
There were reports from all key stakeholders about the importance of continuing medication where appropriate to benefit young people’s learning, which has also been reported by teachers and others (Jangmo et al. Citation2019; Keilow, Holm, and Fallesen Citation2018; Prasad et al. Citation2013; Wilson et al. Citation2006). While underlining the importance of access to ADHD medication for young people who can benefit from it, NICE (Citation2020) state healthcare professionals should review medications and their discontinuation yearly including its impact on education; as shown in our findings this may perpetuate a potentially misleading belief that drug treatment is only necessary for school. Analysis of the role of information provision in relation to the CATCh-uS study data suggested that this mistaken belief could contribute to difficulties associated with the premature stopping of medication for some young people (Price et al. Citation2019), especially as many daily tasks for individuals of any age who have ADHD require sustained attention, concentration and self-organisation. This finding is supported by other studies including Schaefer et al. (Citation2017).
Research suggests that young people adhere (or not) to medication because of its perceived benefits (Marrero et al. Citation2020). Young people’s attitudes to medication are diverse (Gallichan and Curle Citation2008) and they have been shown to weigh-up the burden of treatment against the benefits to their schoolwork (Eccleston et al. Citation2019). There seems much to be gained for these young people from receiving support that includes information, and discussions that consider their perspectives about their self-care, including medication (Eccleston et al. Citation2019), to which those in education could contribute. Medication has benefits beyond learning in educational settings; studies report substantially reduced levels of suicidal behaviour (Chen et al. Citation2014), depression (Chang et al. Citation2016), substance misuse (Chang et al. Citation2014; Montano and Young Citation2012), road traffic accidents (Chang et al. Citation2017), and convictions and violent reoffending (Lichtenstein and Larsson Citation2013) among young adults with ADHD who continue their medication compared to those that stop it.
Many of the young people interviewed in the CATCh-uS study had a mindset that medication was beneficial for learning, reflecting on aspects such as improved concentration and academic achievement. In some cases, the data suggested young people have felt pressured to take medication while at school or college. This indicates that medication is often seen as essential to ensure continuity of learning into FE college, university and training. In addition, prescribing medication for school days and not for weekends or holidays seems to assume that no learning takes place at these times, which for most sixth form, FE college, university and training courses is not the case. Therefore, along with a balanced discussion of individual preference and need, the potential benefits of medication for and beyond their formal education should be communicated to young people with ADHD.
Unmet needs and inconsistent support
The CATCh-uS study demonstrated a lack of ‘optimal’ health care transition for young people with ADHD. The themes expanded in the current paper indicate that young people with ADHD can find themselves left with unmet needs for healthcare support with negative implications for their educational progress or entry to employment (Jangmo et al. Citation2021). The person-environment-fit theory (Eccles and Midgley Citation1989) posits that if a young person is frequently in an environment where their needs are not met, the resulting mismatch is likely to lead to demotivation, thereby increasing the risk of, or exacerbating, educational failure, existing mental health difficulties and unacceptable behaviours. A worryingly high proportion of young people in prisons have ADHD, while studies suggest an excess of convictions among those who stop their ADHD medication compared to those who continue it (Young et al. Citation2018).
The healthcare transition from CAMHS to AMHS has been recognised as ‘a priority for action’ by the DfE and DoH (Department for Education and Department of Health Citation2015). Educational staff are an important constituent of the pathway to meeting the needs of young people with mental health issues (Department for Education Citation2017). However, only those young people who healthcare practitioners regard as having a significant health need or have an EHC plan formally qualify for transition support between educational settings (Department for Education and Department of Health Citation2015). The IES report for the Office for Students (OfS) highlights that HE faces a number of challenges in supporting young people with disabilities (including those with ADHD), with one provider stating their disability service and academic staff need training and development to support those with ADHD amongst others (IES Citation2019). Given the healthcare transition challenges perhaps it is unsurprising that when compared with their non-ADHD peers, young people with ADHD in the UK are less likely to enrol at university, and if they do enrol, are likely to graduate later (Jangmo et al. Citation2021). Research has found that university students do experience inconsistent waiting times for treatment (Sedgwick Citation2018), but we lack data on the experience of this particular group of young adults with ADHD. With no statutory guidance focussed on education to meet the transition needs of all those with ADHD from the DfE or the OfS, it is clear from the experience of those interviewed for the CATCh-uS study, who returned to services after a period without support, that young people with ADHD who have ongoing treatment needs merit improved support and guidance.
Recommendations on how health service transitions should take place have already been proposed (Young et al. Citation2016), with the importance of personalisation identified (Sansosti et al. Citation2017). These recommendations put the responsibility on clinicians to initiate contact with educational settings when the young people’s circumstances change. However, our findings indicate that clinicians are rarely in direct contact with schools or colleges. The perspectives from the interviews of young people and parents indicate these discussions would have helped them achieve smoother transitions. The benefits of a single point of contact through transition have previously been outlined (Poulton Citation2017).
There appears to be a need for an evidence based multi-agency service transition model or protocol with clear leadership responsibilities that includes roles for educational staff in settings such as sixth forms, FE colleges and universities for adoption across the UK. This should build upon NICE guidelines (NICE Citation2019) and be published as statutory guidance jointly by the DfE, OfS and NICE. This guidance could be configured and if necessary resourced so there is no additional burden on existing staff workloads or educational setting finances. Perhaps, as our data suggests, the approach taken in special schools where young people are often supported into their twenties with better coordination between health, social care and education could be explored to understand how to translate these models to mainstream education settings (recommendation 1 in ). Special school placement may imply particular needs that are not always seen in mainstream education setting, examination of their strengths to inform mainstream education (Black Citation2019) and greater commonality of educational provision in mainstream and special schools has been suggested (Norwich Citation2008). Sadly, collaboration between the two is rarely seen (Ofsted Citation2005).
Table 3. Recommendations
Research into areas of service transition best practice, e.g., processes adopted by special schools, should be conducted to inform how education could and should best support young people with ADHD to improve transitions. Health economics analyses could also assist in making the case for resource for such practice. The engagement in multi-agency coordination by special schools draws parallels with the successful integration of services that should result from EHC plans. Young people with a range of conditions and their parents have reported satisfaction with EHC plans (Department for Education Citation2017). The educational transition to university and adjustment to new social and learning expectations is significant for many students (Meehan and Howells Citation2019). Therefore it is crucial that those with ADHD benefit from greater coordination between health services and education to increase the level of support at this challenging time.
Further research on the perspectives of young people with ADHD (medicated and unmedicated) along with their parents and carers, education staff and practitioners that explicitly focusses on transition experiences while in school, college or HE is recommended. It might be useful to consider an economic evaluation with a societal perspective. As well as consideration of young people with ADHD’s world in a holistic way that the wider ecological approach to needs management informs, with different factors impacting on complex transitions at different levels. For example, with education appearing in terms of staff (micro), relationship effects (meso), funding (macro) and transitions as environmental change over time (chrono) (O’Toole, Hayes, and Mhathúna Citation2014). Furthermore, many young people with other recognised special educational needs are not being supported effectively in mainstream schools (National Audit Office Citation2019) and poor transitions in health and education risk diffracting social and academic trajectories further. Thus, research could extend to other mental health conditions beyond ADHD, and the impact of child to adult health care transitions on young people’s learning.
We appreciate that is not straightforward for those working in education to understand and support those with ADHD. There are many variables to consider including the effects of medication on learning and behaviour (Jangmo et al. Citation2019, Citation2021) as well as the timing and implications of health service transitions, and the implications of relocations.
A narrative synthesis based on these same parent and young people interviews on the role of information in transition (Price et al. Citation2019) highlighted the importance of making information available and communicating it to young people and their parents or carers. In addition to understanding the importance of continued access to medication to assist learning, data from young people and their parents indicates the important role educators and or SENCos can have. Young people with ADHD indicated they value having someone in education who knows them well, and this role could include signposting them to ADHD support and resources beyond school and college (recommendation 2 ). Here we emphasise that these results suggest that the education and health sectors need to work together to decide and facilitate who is best to lead ongoing support for these young people. In addition, specific staff in all education settings need to be trained to help identify, prepare, and support these young people through education as they navigate health service transitions. This would include managed handovers from one education setting to the next and engaging with parents or carers, as well as being a point of contact for practitioners.
Further, oversight of service transition effectiveness would seem to be essential to improve and maintain their quality (recommendation 3 in ). Perhaps the ‘deep dive’ work by Ofsted (Citation2019) where schools are being evaluated as part of multi-agency mental health support for children aged 10–15 could be used to inform transition approaches. Whether or not universal structural changes and oversight take place, smoother transitions would also be supported by better mutual understanding between education staff and clinicians of the different transition processes involved in health and education. Ideally, regular discussion between clinicians and educators would support improved joint working and smoother educational and health care transitions.
A key strength of this study is that the CATCh-uS recruited a wide range of participants who provided detailed accounts of their experiences relating to ADHD and service transition (Patton Citation1999). The accounts from clinicians provided data that helped to corroborate young people’s accounts. However, the focus of the CATCh-uS study was transition between health services, and these accounts were not subject to a detailed examination that a researcher with a planned topic guide focussed on education processes would have undertaken. As they were collected during research focussed on child to adult health service transitions, they may also not relate to the experiences of young people with ADHD who do not need or want to transition to adult ADHD service, and may reflect only part of the education experience of these young people. Furthermore, the transition process was examined by interviewing at three stages of health care transition. A longitudinal study following individual young people through the whole process may provide even richer data. Lastly, the experiences and perspectives of educators were not captured in this study which further research should explore.
Conclusions
The wellbeing of young people with ADHD is often intertwined with access to education and health care institutions. This research provides evidence of links between healthcare transitions and educational processes, the perceived association between medication and academic learning and attainment, inconsistent coordination between health and education providers, and health transitions often complicated by educational relocations. Improved implementation of health care transition approaches with coordinated support from trained educators could reduce the challenges faced by young people with ADHD, leading to improved educational and occupational outcomes. Improving health care transitions and ensuring educational providers coordinate with healthcare services to support young people with ADHD is an important priority for them and their parents and carers.
Acknowledgments
The authors would like to thank: the CATCh-uS parent advisory group, the Study Steering Committee, the parents, young people, clinicians and GPs who participated in interviews, and the NHS Trusts who facilitated recruitment. This work would not have been possible without your help.
Disclosure statement
Tamsin Ford received an honorarium for presenting the results of the CATCh-uS study to the Nurses Training forum funded by Takeda in March 2019. The authors declare there are no other known conflicts of interest.
Additional information
Funding
Notes on contributors
Simon Benham-Clarke
Simon Benham-Clarke is a researcher who focusses on education and mental health to improve outcomes for young people.
Tamsin Ford
Tamsin Ford is a child and adolescent psychiatrist who research focuses on interventions and services to optimize the mental health of children and young people.
Siobhan B Mitchell
Siobhan B. Mitchell is a Research Fellow at the University of Exeter working in the Children & Young People–s Mental Health Research Collaboration with a research focus on child and adolescent development and mental health.
Anna Price
Tamsin Newlove-Delgado has a background in child and adolescent psychiatry and public health, and experience in applied epidemiology and mixed methods health services research. She was a co-investigator on CATCh-uS.
Tamsin Newlove-Delgado
Sharon Blake is an experienced qualitative researcher with an interdisciplinary background (law, social science, health). She has worked with youth with ADHD both in the criminal justice and care systems.
Sharon Blake
Dr Helen Eke is a Postdoctoral Research Fellow on the NIHR South West Peninsula Applied Research Collaboration (PenARC) Child Health and Maternity Programme based at the University of Exeter.
Helen Eke
Darren A. Moore is a Senior Lecturer in Education at the University of Exeter. His research interests focus on mental health in education, including SEND, behaviour, school attendance and implementation.
Darren A Moore
Abigail Emma Russell is a Senior Lecturer in Child Health. Her research focusses on neurodevelopmental disorders and school attendance, as well as understanding and preventing mental health difficulties in young people.
Abigail Emma Russell
Astrid Janssens is a psychologist and anthropologist and works in partnership with patients and relatives to create health research.
References
- Advokat, C., S. M. Lane, and C. Luo. 2011. “College Students with and without ADHD: Comparison of Self-Report of Medication Usage, Study Habits, and Academic Achievement.” Journal of Attention Disorders 15 (8): 656–666. doi:https://doi.org/10.1177/1087054710371168.
- American Psychiatric Association. 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. (eds, 5th). Washington, D.C: American Psychiatric Association.
- Ascherman, L., and J. Shaftel. 2017. “Facilitating Transition from High School and Special Education to Adult Life.” Child and Adolescent Psychiatric Clinics of North America 26 (2): 311–327. doi:https://doi.org/10.1016/j.chc.2016.12.009.
- Black, A. 2019. “Future Secondary Schools for Diversity: Where are We Now and Were Could We Be?” Review of Education 7 (1): 36–87. doi:https://doi.org/10.1002/rev3.3124.
- Bynner, J. 2001. “British Youth Transitions in Comparative Perspective.” Journal of Youth Studies 4 (1): 5–23. doi:https://doi.org/10.1080/13676260120028529.
- Chang, Z., B. M. D’Onofrio, P. D. Quinn, P. Lichtenstein, and H. Larsson. 2016. “Medication for Attention-Deficit/Hyperactivity Disorder and Risk for Depression: A Nationwide Longitudinal Cohort Study.” Biological Psychiatry 80 (12): 916–922. doi:https://doi.org/10.1016/j.biopsych.2016.02.018.
- Chang, Z., P. D. Quinn, K. Hur, R. D. Gibbons, A. Sjölander, H. Larsson, and B. M. D’Onofrio. 2017. “Association between Medication Use for Attention-Deficit/Hyperactivity Disorder and Risk of Motor Vehicle Crashes.” JAMA Psychiatry 74 (6): 597–603. doi:https://doi.org/10.1001/jamapsychiatry.2017.0659.
- Chang, Z., P. Lichtenstein, L. Halldner, B. D’Onofrio, E. Serlachius, S. Fazel, N. Långström, and H. Larsson. 2014. “Stimulant ADHD Medication and Risk for Substance Abuse.” Journal of Child Psychology and Psychiatry, and Allied Disciplines 55 (8): 878–885. doi:https://doi.org/10.1111/jcpp.12164.
- Chen, Q., A. Sjölander, B. Runeson, B. D’Onofrio, P. Lichtenstein, and H. Larsson. 2014. “Drug Treatment for Attention-deficit/hyperactivity Disorder and Suicidal Behaviour: Register Based Study.” BMJ: British Medical Journal 348: g3769–g3769. doi:https://doi.org/10.1136/bmj.g3769. Accessed 29 April 2021.
- Department for Education and Department of Health. 2015. “Special Educational Needs and Disability Code of Practice: 0 to 25 Years Statutory Guidance for Organisations Which Work with and Support Children and Young People Who Have Special Educational Needs or Disabilities.” London: DfEand DoH. Accessed 9 May 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/398815/SEND_Code_of_Practice_January_2015.pdf
- Department for Education. 2015. “Supporting Pupils at School with Medical Conditions Statutory Guidance for Governing Bodies of Maintained Schools and Proprietors of Academies in England.” London: DfE. Accessed 9 May 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/803956/supporting-pupils-at-school-with-medical-conditions.pdf
- Department for Education. 2017. “Experiences of Education, Health and Care Plans. A Survey of Parents and Young People.” London: DfE. Accessed 9. May 2020. https://www.gov.uk/government/publications/education-health-and-care-plans-parents-and-young-people-survey
- Eccles, J. S., and C. Midgley. 1989. “Stage Environment Fit: Developmentally Appropriate Classrooms for Early Adolescents.” In Research on Motivation in Education, edited by R. E. Ames and C. Ames, 139–186. Vol. 3. New York, NY: Academic Press.
- Eccleston, L., J. Williams, S. Knowles, and L. Soulsby. 2019. “Adolescent Experiences of Living with a Diagnosis of ADHD: A Systematic Review and Thematic Synthesis.” Emotional and Behavioural Difficulties 24 (2): 119–135. doi:https://doi.org/10.1080/13632752.2019.1582762.
- Eke, H., T. Ford, T. Newlove-Delgado, A. Price, S. Young, C. Ani, K. Sayal, R. Lynn, M. Paul, and A. Janssens. 2019. “Transition between Child and Adult Services for Young People with Attention-Deficit Hyperactivity Disorder (ADHD): Findings from a British National Surveillance Study.” The British Journal of Psychiatry 217 (5): 616–622. doi:https://doi.org/10.1192/bjp.2019.131.
- Faraone, S. V., P. Asherson, T. Banaschewski, J. Biederman, J. K. Buitelaar, J. A. Ramos-Quiroga, L. A. Rohde, E. J. Sonuga-Barke, R. Tannock, and B. Franke. 2015. “Attention-deficit/hyperactivity Disorder.” Nature Reviews. Disease Primers 1: 15020. doi:https://doi.org/10.1038/nrdp.2015.20.
- Fleming, M., C. A. Fitton, M. F. C. Steiner, J. S. McLay, D. Clark, A. King, D. F. Mackay, and J. P. Pell. 2017. “Educational and Health Outcomes of Children Treated for Attention-Deficit/Hyperactivity Disorder.” JAMA Pediatrics 171 (7): e170691. doi:https://doi.org/10.1001/jamapediatrics.2017.0691.
- Ford, T. 2020. “Transitional Care for Young Adults with ADHD: Transforming Potential Upheaval into Smooth Progression.” Epidemiology and Psychiatric Sciences 29: e87. doi:https://doi.org/10.1017/S2045796019000817.
- Gale, N., G. Heath, E. Cameron, S. Rashid, and S. Redwood. 2013. “Using the Framework Method for the Analysis of Qualitative Data in Multi-disciplinary Health Research.” BMC Medical Research Methodology 13 (1): 1–8. doi:https://doi.org/10.1186/1471-2288-13-117.
- Gallichan, D. J., and C. Curle. 2008. “Fitting Square Pegs into Round Holes: The Challenge of Coping with Attention-Deficit Hyperactivity Disorder.” Clinical Child Psychology and Psychiatry 13 (3): 343–363. doi:https://doi.org/10.1177/1359104508090599.
- Guest, G., A. Bunce, and L. Johnson. 2006. “How Many Interviews are Enough? an Experiment with Data Saturation and Variability.” Field Methods 18 (1): 59–82. doi:https://doi.org/10.1177/1525822X05279903.
- IES. 2019. “Review of Support for Disabled Students in Higher Education in England, Report to the Office for Students by the Institute for Employment Studies and Researching Equity, Access and Participation.” October 2019.
- Jangmo, A., A. Stålhandske, Z. Chang, Q. Chen, C. Almqvist, I. Feldman, C. Bulik, et al. 2019. “Attention-Deficit/Hyperactivity Disorder, School Performance, and Effect of Medication.” Journal of the American Academy of Child and Adolescent Psychiatry 58 (4): 423–432. doi:https://doi.org/10.1016/j.jaac.2018.11.014.
- Jangmo, A., R. Kuja-Halkola, A. Pérez-Vigil, C. Almqvist, C. Bulik, B. D’Onofrio, P. Lichtenstein, et al. 2021. “Attention-deficit/hyperactivity Disorder and Occupational Outcomes: The Role of Educational Attainment, Comorbid Developmental Disorders, and Intellectual Disability.” PLoS ONE 16 (3): e0247724. doi:https://doi.org/10.1371/journal.pone.0247724.
- Janssens, A., H. Eke, A. Price, T. Newlove-Delgado, S. Blake, C. Ani, P. Asherson, et al. 2020. “The Transition from Children’s Services to Adult Services for Young People with Attention Deficit Hyperactivity Disorder: The CATCh-uS Mixed-methods Study.” Southampton (UK): NIHR Journals Library; 2020 Nov. PMID: 33211453.
- Keilow, M., A. Holm, P. Fallesen, and N. Hadjikhani. 2018. “Medical Treatment of Attention Deficit/Hyperactivity Disorder (ADHD) and Children’s Academic Performance.” PLoS ONE 13 (11): e0207905. In N Hadjikhani (Eds). doihttps://doi.org/10.1371/journal.pone.0207905.
- Kern, D. 2011. “Early Identification of ADHD: Methods, Benefits, and a Standard Performance Metric for School Districts.” Wilmington University (Delaware).
- Kuriyan, A., W. Pelham, B. Molina, D. Waschbusch, E. Gnagy, M. Sibley, D. Babinski, et al. 2013. “Young Adult Educational and Vocational Outcomes of Children Diagnosed with ADHD.” Journal of Abnormal Child Psychology 41 (1): 27–41. doi:https://doi.org/10.1007/s10802-012-9658-z.
- Lichtenstein, P., and H. Larsson. 2013. “Medication for Attention Deficit-hyperactivity Disorder and Criminality.” The New England Journal of Medicine 368 (8): 776.
- Mahdi, S., M. Viljoen, R. Massuti, M. Selb, O. Almodayfer, S. Karande, P. J. De Vries, L. Rohde, and S. Bölte. 2017. “An International Qualitative Study of Ability and Disability in ADHD Using the WHO-ICF Framework.” European Child & Adolescent Psychiatry 26 (10): 1219–1231. doi:https://doi.org/10.1007/s00787-017-0983-1.
- Marrero, R., A. Fumero, A. De Miguel, and W. Peñate. 2020. “Psychological Factors Involved in Psychopharmacological Medication Adherence in Mental Health Patients: A Systematic Review.” Patient Education and Counseling 103 (10): 2116–2131. doi:https://doi.org/10.1016/j.pec.2020.04.030.
- Meehan, C., and K. Howells. 2019. “In Search of the Feeling of ‘Belonging’ in Higher Education: Undergraduate Students Transition into Higher Education.” Journal of Further and Higher Education 43 (10): 1376–1390. doi:https://doi.org/10.1080/0309877X.2018.1490702.
- Montano, C., and J. Young. 2012. “Discontinuity in the Transition from Pediatric to Adult Health Care for Patients with Attention–Deficit/Hyperactivity Disorder.” Postgraduate Medicine 124 (5): 23–32. doi:https://doi.org/10.3810/pgm.2012.09.2591.
- National Audit Office. 2019. “Support for Pupils with Special Educational Needs and Disabilities in England.”
- Newlove-Delgado, T., S. Blake, T. Ford, and A. Janssens. 2019. “Young People with Attention Deficit Hyperactivity Disorder in Transition from Child to Adult Services: A “Qualitative Study of the Experiences of General Practitioners in the UK.” BMC Family Practice 20 (1): 159. doi:https://doi.org/10.1186/s12875-019-1046-0.
- Newlove-Delgado, T., T. Ford, R. Garside, R. Garside, and O. C. Ukoumunne. 2018. “Prescribing of Medication for Attention Deficit Hyperactivity Disorder among Young People in the Clinical Practice Research Datalink 2005–2013: Analysis of Time to Cessation.” European Child & Adolescent Psychiatry 27: 29–35 27 (1): 29–35. doi:https://doi.org/10.1007/s00787-017-1011-1.
- NICE. 2019. “Attention Deficit Hyperactivity Disorder: Diagnosis and Management.” Accessed 11 March 2021. https://www.nice.org.uk/guidance/ng87/chapter/Recommendations#service-organisation-and-training
- NICE. 2020. “Treatment Attention Deficit Hyperactivity Disorder (ADHD).” Accessed 8 May 2020. https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/treatment
- Norwich, B. 2008. “Special Schools: What Future for Special Schools and Inclusion? Conceptual and Professional Perspectives.” British Journal of Special Education 35 (3): 136–143. doi:https://doi.org/10.1111/j.1467-8578.2008.00387.x.
- O’Toole, L., N. Hayes, and M. Mhathúna. 2014. “A Bio-ecological Perspective on Educational Transition.” Procedia - Social and Behavioral Sciences 140: 121–127. doi:https://doi.org/10.1016/j.sbspro.2014.04.396.
- Office for National Statistics. 2018. “Population Estimates for UK, England and Wales, Scotland and Northern Ireland.” Office for National Statistics.
- Ofsted. 2005. “Inclusion: Does It Matter Where Pupils are Taught?” www.ofsted.gov.uk
- Ofsted. 2019. “Guidance for Joint Targeted Area Inspections on the Theme: Children’s Mental Health A ‘Deep Dive’ Theme for Joint Targeted Area Inspections.” Accessed 3 May 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/820890/Guidance_for_joint_targeted_area_inspections_on_the_theme_childrens_mental_health.pdf
- Patton, M. 1999. “Enhancing the Quality and Credibility of Qualitative Analysis.” Health Services Research 34 (5): 1189. Pt 2.
- Paul, M., T. Ford, T. Kramer, Z. Islam, K. Harley, and S. P. Singh. 2013. “Transfers and Transitions between Child and Adult Mental Health Services.” British Journal of Psychiatry Supplement 54 (s54): 36–40. doi:https://doi.org/10.1192/bjp.bp.112.119198.
- Phabinly, G., M. McManus, K. Rogers, and P. White. 2017. “Outcome Evidence for Structured Pediatric to Adult Health Care Transition Interventions: A Systematic Review.” The Journal of Pediatrics 188: 263–269. doi:https://doi.org/10.1016/j.jpeds.2017.05.066.
- Polanczyk, G. V., G. A. Salum, L. S. Sugaya, A. Caye, and L. A. Rohde. 2015. “Annual Research Review: A Meta-analysis of the Worldwide Prevalence of Mental Disorders in Children and Adolescents.” Journal of Child Psychology and Psychiatry, and Allied Disciplines 56 (3): 345–365. doi:https://doi.org/10.1111/jcpp.12381.
- Polat, F., A. Kalambouka, and W. Boyle. 2001. “Post-16 Transitions of Pupils with Special Educational Needs.” Centre for Formative Assessment Studies School of Education University of Manchester.
- Poulton, A. 2017. “Transition in ADHD: Attention to the Lifespan.” Australasian Psychiatry 25 (2): 126–129. doi:https://doi.org/10.1177/1039856216671665.
- Prasad, V., E. Brogan, C. Mulvaney, M. Grainge, W. Stanton, and K. Sayal. 2013. “How Effective are Drug Treatments for Children with ADHD at Improving On-Task Behaviour and Academic Achievement in the School Classroom? A Systematic Review and Meta-Analysis.” European Child & Adolescent Psychiatry 22 (4): 203–216. doi:https://doi.org/10.1007/s00787-012-0346-x.
- Price, A., T. Newlove-Delgado, H. Eke, M. Paul, S. Young, T. Ford, and A. Janssens. 2019. “In Transition with ADHD: The Role of Information, in Facilitating or Impeding Young People’s Transition into Adult Services.” BMC Psychiatry 19 (1): 404. doi:https://doi.org/10.1186/s12888-019-2284-3.
- Ritchie, J., J. Lewis, and G. Elam. 2003. “Designing and Selecting Samples.” In Qualitative Research Practice. A Guide for Social Science Students and Researchers, edited by J. Ritchie and J. Lewis, 77–108. Thousand Oaks, CA: Sage.
- Sansosti, F., F. Cimera, L. Koch, P. Rumrill, L. C. Koch, and P. D. Rumrill. 2017. “Strategies for Ensuring Positive Transition for Individuals with Attention-Deficit/Hyperactivity Disorder.” Journal of Vocational Rehabilitation 47 (2): 149–157. Edited by Lynn C. Koch and Phillip D. Rumrill. doihttps://doi.org/10.3233/JVR-170891.
- Schaefer, M., A. Rawlinson, S. Wagoner, S. Shapiro, J. Kavookjian, and W. Gray. 2017. “Adherence to Attention-deficit/hyperactivity Disorder Medication during the Transition to College.” Journal of Adolescent Health 60 (6): 706–713. doi:https://doi.org/10.1016/j.jadohealth.2016.12.011.
- Schwiebert, V., K. Sealander, and J. Dennison. 2011. “Strategies for Counselors Working with High School Students with Attention-Deficit/Hyperactivity Disorder.” Journal of Counseling & Development 80 (1): 3–10. doi:https://doi.org/10.1002/j.1556-6678.2002.tb00160.x.
- Sedgwick, J. 2018. “University Students with Attention Deficit Hyperactivity Disorder (ADHD): A Literature Review.” Irish Journal of Psychological Medicine 35 (3): 221–235. doi:https://doi.org/10.1017/ipm.2017.20.
- Singh, I. 2012. VOICES Study: Final Report. London, UK.
- Smith, Z., J. Langberg, C. Cusick, C. Green, and S. Becker. 2020. “Academic Motivation Deficits in Adolescents with ADHD and Associations with Academic Functioning.” Journal of Abnormal Child Psychology 48 (2): 237–249. doi:https://doi.org/10.1007/s10802-019-00601-x.
- Wadlington, C. 2012. “A Nationwide Survey of Disability Support Personnel regarding Transition, Documentation, and Services for Postsecondary Students with Invisible Disabilities.” Texas Woman’s University.
- Wedge, M. 2015. “A Disease Called Childhood: Why ADHD Became an American Epidemic.” Avery.
- Wilson, H., D. Cox, R. Merkel, M. Moore, and D. Coghill. 2006. “Effect of Extended Release Stimulant-based Medications on Neuropsychological Functioning among Adolescents with Attention-deficit/hyperactivity Disorder.” Archives of Clinical Neuropsychology 21 (8): 797–807. doi:https://doi.org/10.1016/j.acn.2006.06.016.
- Young, S., G. Gudjonsson, P. Chitsabesan, B. Colley, E. Farrag, A. Forrester, J. Hollingdale, et al. 2018. “Identification and Treatment of Offenders with Attention-deficit/hyperactivity Disorder in the Prison Population: A Practical Approach Based upon Expert Consensus.” BMC Psychiatry 18 (1): 281. doi:https://doi.org/10.1186/s12888-018-1858-9.
- Young, S., M. Adamou, P. Asherson, D. Coghill, B. Colley, G. Gudjonsson, C. Hollis, et al. 2016. “Recommendations for the Transition of Patients with ADHD from Child to Adult Healthcare Services: A Consensus Statement from the UK Adult ADHD Network.” BMC Psychiatry 16 (1): 301. doi:https://doi.org/10.1186/s12888-016-1013-4.
