Abstract
Objective
This prospective pilot study aimed to evaluate the effects of associating a neodymium:yttrium–aluminum–garnet (Nd:YAG) laser with a vaginal erbium laser (VEL), as a non-ablative photothermal therapy for superficial dyspareunia in postmenopausal women (PMW) suffering from genitourinary syndrome of menopause (GSM).
Methods
Two groups of sexually active PMW reporting superficial dyspareunia were selected: one (15 patients, VEL) was treated using an erbium:yttrium–aluminum–garnet laser crystal (XS Fotona SMOOTH; Fotona, Ljubljana, Slovenia) with a wavelength of 2940 nm; in the other group (15 patients, VEL + Nd:YAG) this treatment was followed by Nd:YAG laser (Fotona SP Dynamis, PIANO mode) treatment. Treatment consisted of three laser applications at 30-day intervals. Symptoms were assessed before, after each laser application and after 1 and 3 months from the end of the treatment, using the subjective visual analog scale (VAS) for superficial dyspareunia.
Results
Both groups showed a rapid and significant improvement of superficial dyspareunia over time (p < 0.001) independently from age and years since menopause. The VEL + Nd:YAG group showed a greater improvement of superficial dyspareunia (p < 0.001); this difference was evident since the first treatment and remained stable over time.
Conclusions
The addition of Nd:YAG to VEL may induce greater improvement in superficial dyspareunia in PMW with GSM.
铒/钕联合激光治疗浅表性性交困难的短期疗效:一项初步研究 摘要
目的:本前瞻性初步研究, 旨在评估钕钇铝石榴石晶体(Nd:YAG)激光与阴道铒激光(VEL)联合治疗(PMW)绝经后泌尿生殖系统综合征(GSM):浅表性性交困难的效果。
方法:选择两组有浅表性交功能障碍的性活跃绝经后妇女PMW患者:一组(15名患者, VEL)使用波长为2940nm的铒钇铝石榴石激光晶体(XS Fotona SMOOTH;Fotona, 卢布尔雅那, 斯洛文尼亚)治疗;在另一组(15名患者, VEL+Nd:YAG)中, 这种治疗随后是Nd:YAG激光(Fotona SP Dynamics, PIANO模式)治疗。治疗包括每隔30天进行三次激光治疗。在每次激光治疗之前、之后以及治疗结束后1个月和3个月后, 使用浅表性交困难主观视觉模拟量表(VAS)评估症状。
结果:随着时间的推移, 两组患者的浅表性交困难均迅速显著改善(p<0.001), 与年龄和绝经后的年数无关。VEL+Nd:YAG组对浅表性交困难的改善更大(p<0.001);这种差异自第一次治疗以来就很明显, 并随着时间的推移疗效稳定。
结论:在VEL中加入Nd:YAG可使伴有泌尿生殖系统综合征的绝经后妇女的浅表性性交困难得到更大的改善。
Introduction
Dyspareunia is the most bothersome symptom in sexually active women suffering from genitourinary syndrome of menopause (GSM). Besides other chronic and generally progressive genital and urinary symptoms associated with estrogen deficiency, dyspareunia severely jeopardizes sexual relationships and quality of life for postmenopausal women (PMW) [Citation1]. In addition to hormonal and non-hormonal therapies [Citation2,Citation3], recently it has been demonstrated that the non-invasive, non-ablative 2940 nm erbium:yttrium–aluminum–garnet (Er:YAG) laser, using the SMOOTH mode (vaginal erbium laser [VEL]), may improve GSM symptoms as well as stress urinary incontinence [Citation4–15]. A large survey conducted in more than 113,000 women showed that the VEL appears to be safe, with a very low risk profile, with transient, mild to moderate minor side effects occurring with very low frequencies [Citation15].
The neodymium:YAG (Nd:YAG) laser is a solid-state crystal laser-emitting light with a wavelength of 1064 nm that has a deeper optical penetration into tissue. The Nd:YAG laser is one of the most versatile and interesting lasers in dermatological laser medicine, having a wide spectrum of applications. Depending on the wavelength and mode, the Nd:YAG laser can be used for benign pigmented lesions (tattoos, traumatic tattoos, cafe-au-lait macules, lentigines), epilation and vascular lesions (teleangiectasias, hemangiomas). With its long pulses and durations in the range of seconds (PIANO mode), the Nd:YAG laser is ideal for homogeneous bulk heating of the tissues, such as the dermis or the subcutaneous fat. In the PIANO mode, with long pulse duration in the range of seconds, deeper structures can be reached in a very gentle, practically painless way. The PIANO mode has been successfully used for esthetic and dermatological indications, including lichen sclerosus treatment [Citation16,Citation17]. The combination of Er:YAG and Nd:YAG lasers has been demonstrated to be effective for non-invasive dermatologic and esthetic indications [Citation16,Citation18,Citation19]. Therefore, the characteristics of the Nd:YAG laser in the PIANO mode could be of help also in treating the vulva and particularly the posterior commissure in PMW suffering from GSM. The aim of our pilot study was to investigate the efficacy of combined VEL and Nd:YAG laser treatment in PMW suffering from GSM with superficial dyspareunia.
Materials and methods
This pilot, prospective, comparative study was performed in sexually active PMW attending the outpatient Menopause Clinic of Pisa University Hospital. All women were suffering from GSM, with the most bothering symptom being pain at the vaginal opening during intercourse, or superficial dyspareunia. The protocol was revised by a National Independent Advisory Board and approved by the Ethics Committee of the Department of Obstetrics and Gynecology. All patients included were sexually active PMW, with plasma levels of gonadotropin and estradiol in the postmenopausal range (follicle stimulating hormone >40 U/l; estradiol <25 pg/ml), suffering from vaginal atrophy and superficial dyspareunia. All women had to have a negative Pap smear. They were not selected according to previous treatment outcomes. The main goal of the study was the evaluation of laser treatments on superficial dyspareunia. Exclusion criteria were: use of lubricants, local preparations, hormones or other medications to relieve menopausal symptoms in the 3 months prior to inclusion in the study; lesions, scars or infection, active or recent (30 days), of the genitourinary tract; abnormal uterine bleeding; history of photosensitivity disorder or use of photosensitizing drugs; genital prolapse (grade II–III of the classification Pelvic Organ Prolapse Quantification system [POP-Q]); or serious or chronic illness that could interfere with the study.
All procedures were performed in accordance with the ethical standards of the Committee on Institutional Human Experimentation, and with the Helsinki Declaration of 1975, as revised in 1983. All patients gave written informed consent to the study. Thirty women were selected during a screening visit 2–4 weeks prior to the first laser treatment (T0). During this baseline visit, the eligibility of the patient was verified, written informed consent was obtained and clinical information was collected (age, age at menopause and years since menopause [YSM]). Patients were treated with three laser applications (L1, L2, L3) every 30 days, with a screening visit 2–4 weeks prior to the first laser treatment (T0, baseline) and follow-up visits after 1 month (T1) and 3 months (T3) from the last laser application. During every visit and before each laser application, superficial dyspareunia was evaluated by a visual analog scale (VAS) (range 0–10; 0 = total absence of symptoms, 10 = worst possible symptoms). Consecutive patients were included in the study, and they were randomly attributed to two different groups of treatment. The laser procedures were performed in an outpatient clinical setting, without any preparation, anesthesia or post-treatment medications. Before the procedure, the vagina was cleaned with disinfectant solution and dried with a swab.
Fifteen patients (VEL group) were treated with VEL Renovalase™ (Fotona SP Dynamis, SMOOTH mode; Fotona, Ljubljana, Slovenia) with a wavelength of 2940 nm. Laser parameters were set as previously reported [Citation7]. The diameter of the laser spot size was 7 mm, with a pulse according to the SMOOTH mode at a frequency of 1.6 Hz and fluence (laser energy emitted per unit area) of 6.0 J/cm2, to achieve a controlled deep thermal effect, without ablation and carbonization of the tissues. A specifically designed glass vaginal speculum was used, and the probe (R11) was inserted into the speculum, without direct contact with the vaginal mucosa. Subsequently, circular treatment of the vaginal wall was performed, with seven pulses given every 5 mm, up to the vaginal vestibule. The procedure was repeated three times. Finally, after removing the speculum, the vestibule and the introitus were treated with the SMOOTH mode using the FS03 probe with a spot size of 7 mm, at a frequency of 1.6 Hz releasing 10 J/cm2. The other 15 women (VEL + Nd:YAG group), after the VEL Renovalase™ treatment, were additionally treated with the Nd:YAG laser (Fotona SP Dynamis, PIANO mode), using the R33 non-contact handpiece with a 9-mm spot size, PIANO pulse mode (5 s) and 90 J/cm2 fluence. Six passes were performed over the posterior commissure with the brushing mode. Both the VEL and Nd:YAG treatments were performed in the same session, with no interval between the exposure to the two energies. After treatment, all patients were advised to practice sexual abstinence for 1 week.
Statistical analysis
All results are reported as mean ± standard deviation. We compared baseline characteristics with a Mann–Whitney U-test to examine between-group characteristics.
We used a linear mixed model for repeated measures over time [Citation20] to analyze the impact of the two different laser interventions on superficial dyspareunia: fixed effects were time, group and interaction between time and group; the dependent variable was the VAS score; and random effects were the subjects. A post-hoc test for the interaction between time and treatment was done using the Bonferroni correction. We also estimated the simple effects of time for different groups to see whether the effect of time is present in each group; then, we did a trend analysis to see how time changes the VAS score and whether the two groups show different trends. No missing data were present in the database.
We calculated the difference between T0 and T3 scores (ΔT0/T3) and we used a multiple linear regression model to study how women’s characteristics (age and YSM) and the treatment may influence ΔT0/T3.
Data were analyzed with the open-source statistical software Jamovi version 1.6.23 (The Jamovi Project, Sydney, Australia). p < 0.05 was considered statistically significant.
Results
There were no significant differences in age (60.00 ± 2.98 years for VEL group vs. 62.3 ± 3.77 years for VEL + Nd:YAG group, p = 0.123), age at menopause (50.2 ± 3.49 years vs. 49.7 ± 3.98 years, p = 0.676) and YSM (9.80 ± 4.44 years vs 12.6 ± 5.55 years, p = 0.219) in the two treatment groups before the study.
The basal VAS scores were similar in the two groups (). shows the VAS score for superficial dyspareunia over time for the groups of treatment. In both groups, the VAS scores showed a significant (p < 0.001) decrease. The L1 score was significantly lower in the VEL + Nd:YAG group versus the VEL group. ΔT0/T3 of the two groups of treatments was significantly different (−3.13 ± 1.25 in VEL group vs. −6.27 ± 1.71 in VEL + Nd:YAG group, p < 0.001)
Figure 1. Mean visual analog scale (VAS) score over time for the two treatment groups. Vaginal erbium laser (VEL) group and VEL + Nd:YAG group VAS scores were compared using the post-hoc test with Bonferroni correction. *p < 0.001 versus T0 of VEL group. **p < 0.001 versus T0 of VEL + Nd:YAG group. §p < 0.001 versus corresponding time of VEL group. L1, L2, L3, laser applications; T0 (baseline), 2–4 weeks prior to first laser treatment; T1, 1 month from last laser application; T3, 3 months from last laser application; VEL + Nd:YAG, neodymium:yttrium–aluminum–garnet.
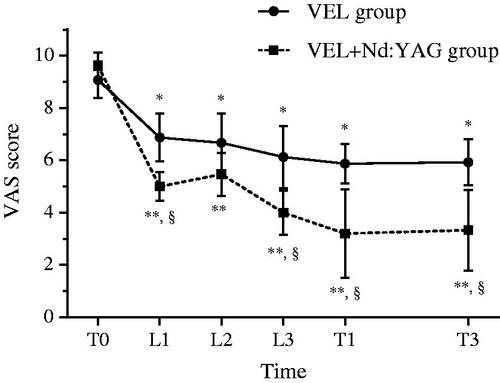
The linear mixed model found R2-marginal of 0.778 and R2-conditional of 0.819. The mixed model analysis found an F test of 61.5 for the effect of group (p < 0.001) and of 112.6 for the effect of time (p < 0.001). The group–time interaction was statistically significant (F-test: 12.7; p < 0.001). Post-hoc comparison of every VAS score measurement over time between the two treatment groups and versus T0 is shown in .
The simple effects test shows that both treatments had a significant effect on VAS score over time (VEL group and VEL + Nd:YAG group p < 0.001), although for the VEL + Nd:YAG group the effect appears to be larger (VEL group F-test: 25.4; VEL + Nd:YAG group F-test: 99.8). Both curve slopes show significant linear and quadratic trends, but both linear (p < 0.001) and quadratic (p < 0.05) trends of the curves were significantly different ( and ). A cubic trend is similar in the two curves (p = 0.163), demonstrating that the VAS score decreases over time in both groups, with the decrease rate diminishing over time but the flattening out of the trend slightly fluctuating from time to time in both treatments.
Table 1. Characteristics of overall trend of means observed in the two groups.
The multiple linear regression model considering age at treatment, YSM and treatment done as variables showed R2 of 0.55. This model revealed that age at treatment and YSM did not influence ΔT0/T3, while it was related only to the laser treatment performed (). No adverse events related to the procedure were recorded throughout the study period. The most common reactions reported were a transitory warm, not burning, sensation during treatment and, in a few cases, self-limiting leukorrhea for a few days after treatment.
Table 2. Results of multiple linear regression model of the difference between VAS score at T0 and at T3 (ΔT0/T3) corrected for age during treatment, YSM and treatment performed.
Discussion
This is the first study that evaluates the efficacy of the combination of VEL + Nd:YAG laser on superficial dyspareunia in PMW. The results of our pilot, prospective longitudinal study indicate that the association of VEL + Nd:YAG laser induces a more rapid, greater and sustained improvement of superficial dyspareunia than VEL treatment alone.
Both VEL alone and VEL + Nd:YAG treatments are able to decrease superficial dyspareunia. Our study indicates that the effects are independent of age and YSM, implying that laser treatment can be proposed in all PMW suffering from superficial dyspareunia. GSM is chronic, is likely to worsen over time and may interfere with sexual function and quality of life [Citation1]. Non-hormonal moisturizers and lubricants as well as local hormone administration are the treatments of choice [Citation1–3]. Although systemic risks have not been identified with local treatments, many women do not accept protracted daily vaginal treatments, or may present absolute contraindications to hormone use, such as a personal history of estrogen-dependent tumors, as in breast cancer [Citation1–3]. The VEL has been demonstrated in a large, prospective, multicentric study to improve sexuality in PMW suffering from GSM [Citation14]. However, present data show that the VEL + Nd:YAG combination seems to be more effective than VEL alone, particularly on superficial dyspareunia. This effect is evident since the first application of the laser, and the effects are maintained up to 3 months after the end of the treatment. The posterior commissure of the labia majora is formed by their end with the connecting skin between them, which is also the boundary of the perineum. Therefore, use of the Nd:YAG laser is of particular interest for the treatment of the skin, and particularly the dermis, of this region. With long pulse duration in the range of seconds, and a low fluence, the Nd-YAG laser can reach deeper structures, inducing virtually no pain or burning sensation. The results of this pilot study seem to demonstrate that adding treatment of the posterior commissure atrophy with the Nd:YAG long-pulse PIANO mode can be of help in the treatment of superficial dyspareunia.
This study has several limitations. This is a small pilot, comparative study, with no sham group. The study design does not allow us to evaluate the effects of VEL + Nd:YAG treatment with combined hormonal or non-hormonal local or systemic therapies or the stratification of laser effects according to previous treatments or symptom severity and/or duration. In addition, in this short-term study, the treatment duration cannot be evaluated. In a previous long-term study we demonstrated that the effects of VEL alone on GSM symptoms, including dyspareunia, vanish after 1 year [Citation5]. The duration of the outcomes of the VEL + Nd:YAG combination, with or without hormone or non-hormonal therapies, is a matter for future studies.
In conclusion, this pilot study suggests that treatment with the VEL + Nd:YAG combination is effective as a new non-ablative photothermal therapy for the treatment of superficial dyspareunia. Further larger, long-term and well-controlled studies are required to explore the use of the two complementary laser wavelengths VEL + Nd:YAG in comparison with the VEL and/or different therapeutic options, in order to offer a safe and effective option to treat superficial dyspareunia in GSM patients.
Potential conflict of interest
The authors have no conflict of interest to disclose. The authors alone are responsible for the content and writing of the paper.
Source of funding
Nil.
References
- Portman DJ, Gass MLS, Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–1068.
- Palacios S, Castelo-Branco C, Currie H, et al. Update on management of genitourinary syndrome of menopause: a practical guide. Maturitas. 2015;82(3):308–313.
- The NAMS. Hormone therapy position statement advisory panel. The 2017 hormone therapy position statement of the North american menopause society. Menopause 2017. 2017;24:728–753.
- Elia D, Gambacciani M, Berreni N, et al. Genitourinary syndrome of menopause (GSM) and laser VEL: a review. Horm Mol Biol Clin Investig. 2019 Dec 19;41(1).
- Gambacciani M, Levancini M, Russo E, et al. Long-term effects of vaginal erbium laser in the treatment of genitourinary syndrome of menopause. Climacteric. 2018;21(2):148–152.
- Gambacciani M, Palacios S. Laser therapy for the restoration of vaginal function. Maturitas. 2017;99:10–15.
- Vizintin Z, Lukac M, Kazic M, et al. Erbium laser in gynecology. Climacteric. 2015;18(sup1):4–8.
- Gambacciani M, Levancini M. Vaginal erbium laser as second-generation thermotherapy for the genitourinary syndrome of menopause: a pilot study in breast cancer survivors. Menopause. 2017;24(3):316–319.
- Blaganje M, Šćepanović D, Žgur L, et al. Non-ablative Er:YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2018;224:153–158.
- Lee MS. Treatment of vaginal relaxation syndrome with an erbium:YAG laser using 90° and 360° scanning scopes: a pilot study & Short-term Results. Laser Ther. 2014;23(2):129–138.
- Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: Consensus and controversies. Lasers Surg Med. 2017;49(2):137–159.
- Gambacciani M, Levancini M, Cervigni M. Vaginal erbium laser: the second-generation thermotherapy for the genitourinary syndrome of menopause. Climacteric. 2015;18(5):757–763.
- Gaspar A, Brandi H, Gomez V, et al. Efficacy of erbium:YAG laser treatment compared to topical estriol treatment for symptoms of genitourinary syndrome of menopause. Lasers Surg Med. 2017;49(2):160–168.
- Gambacciani M, Albertin E, Torelli MG, et al. Sexual function after vaginal erbium laser: the results of a large, multicentric, prospective study. Climacteric. 2020;23(sup1):S24–S27.
- Gambacciani M, Cervigni M, Gaspar A, et al. Safety of vaginal erbium laser: a review of 113,000 patients treated in the past 8 years. Climacteric. 2020;23(sup1):S28–S32.
- Vas K, Besenyi Z, Urbán S, et al. Efficacy and safety of long pulse 1064 and 2940 nm lasers in noninvasive lipolysis and skin tightening. J Biophotonics. 2019;12:1–8.
- Bizjak Ogrinc U, Senčar S, Luzar B, et al. Efficacy of non-ablative laser therapy for lichen sclerosus: a randomized controlled trial. J Obstet Gynaecol Can. 2019;41(12):1717–1725.
- Gaspar A. A CASE REPORT: Combined Er:YAG and Nd:YAG laser treatment for non-invasive body contouring. J Laser Heal Acad Artic J LA&HA. 2015;2015:48–50.
- Nghi P-H. Safety and effectiveness of the combined Nd:YAG and Er:YAG laser-assisted TightSculpting® body contouring procedure. J Laser Heal Acad Artic J LA&HA. 2019;2019:11–15.
- Bell ML, Rabe BA. The mixed model for repeated measures for cluster randomized trials: a simulation study investigating bias and type I error with missing continuous data. Trials. 2020;21(1):148.
