Abstract
Introduction
Research has shown improved health outcomes when patients are involved in managing their health conditions and when their individual needs are considered.
Objectives
This scoping review aimed to map the existing research regarding chronic disease patients’ involvement in their encounters with general practice, with a specific focus on patients with Type 2 diabetes (TD2) or chronic obstructive pulmonary disease (COPD) and from the perspectives of both general practitioners and patients.
Methods
Studies of any design, date, and language were included. A systematic search was conducted using the following databases: Medline, CINAHL, PsycInfo, Scopus, and EMBASE from August until October 2020 and renewed September 2021. Data were systematically charted by the following study characteristics: bibliographic aims; study aims; setting; area of interest; results; conclusion.
Results
Eighteen studies were included; they conducted qualitative methods, surveys or mixed methods. From the patients’ perspectives, the importance of being more involved in treatment discussions during consultations as well as a friendly environment, was underscored. A good relationship and relational continuity make it easier for patients to be more involved in treatment decisions. From the general practitioner (GP) perspectives, they mentioned their high workload, long-standing relationships, knowledge about the patients and prepared patients as factors influencing their ability to involve patients in treatment discussions.
Conclusion
A good GP–patient relationship was considered an important aspect to providing and facilitating for involvement of patients with COPD or TD2.
Scoping review registration: https://osf.io/ynqt2
KEY MESSAGES
Both patients and GPs underscore the importance of a good GP–patient relationship for facilitating involvement of patients with COPD or TD2.
Furthermore, balancing GPs’ professional responsibility of achieving the best health outcome for their patients and respecting patients’ health beliefs is a relevant factor in patient involvement.
Introduction
Globally, there is an increasing interest in patient involvement in healthcare [Citation1,Citation2]. Multiple definitions of patient involvement exist and among those a definition by the British Medical Association: ‘the active participation of citizens, users and careers and their representatives in the development of health care services and as partners in their own health care’ [Citation3]. Research demonstrates improved health outcomes when patients are involved in the management of their own health conditions and when their individual needs are taken into account [Citation4]. Furthermore, the positive influence of patient involvement to treatment and well-being has been established in terms of increased satisfaction [Citation5], higher compliance [Citation6], patient safety [Citation5,Citation7], enhanced psychological well-being [Citation8], improved clinical outcomes and reduced healthcare-system costs [Citation6,Citation9,Citation10]. Moreover, involving patients in treatment decisions benefits healthcare professionals by enhancing their understanding of patients’ health problems, thus contributing to effective management of health delivery by gaining patients’ trust and by enabling them to deliver individualised and tailored healthcare [Citation11].
Worldwide, the number of people living with chronic diseases is rising, and the burden of chronic diseases is increasing rapidly. Globally, approximately one in three adults suffer from one or more chronic diseases [Citation12]. Chronically ill patients tend to have complex pathways characterised by multimorbidity and multiple contacts across the healthcare system. To meet this complexity, general practitioners (GPs) are increasingly given the primary treatment responsibility for patients with chronic disease [Citation13]. Being gatekeepers and the primary contact to healthcare, GPs play an important role in chronically ill patients’ perception of being involved in their treatment and care. However, analyses of chronic diseases patients’ involvement in their encounters with general practice appear to be lacking. We chose to focus on chronic obstructive pulmonary disease (COPD) and type 2 diabetes (TD2) as they are the two most prevalent chronic conditions that are managed by GPs in Western countries [Citation14,Citation15]. In a situation where policymakers continue to push for the adoption of patient involvement in general practice of patients with COPD and TD2 [Citation13], there is an urgent need to remedy the lack of knowledge in this field. This scoping review aimed to map the existing research regarding chronic disease patients’ involvement during their encounters with general practice, with a specific focus on patients with TD2 or obstructive pulmonary disease and from the perspectives of both general practitioners and patients.
Method
Protocol and registration
This scoping review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (Prisma-ScR) [Citation16]. The protocol was registered in the Open Science Framework (osf.io/ynqt2) and remained unchanged during the review.
Eligibility criteria
Studies reporting the involvement of adult patients aged 18 years or older and with TD2 or COPD were included. The core concept examined by this scoping review is patient involvement, defined as active participation in healthcare decision-making, patient involvement in healthcare consultation, factors associated with patient involvement and patients’ preference for involvement. The context is limited to general practice and their encounters with GPs. Studies reporting on patients with mental illness, patients in palliative care, and studies reporting results from multiple diagnoses, populations or age groups and where the results were not stratified were excluded. Studies reporting patient involvement with other healthcare professionals in general practice were excluded. If studies included patients with different diagnoses, patients both over and under 18 years of age, the studies were considered for inclusion only if data was stratified. Similarly, if studies included both a patient perspective and the perspectives of GPs or other healthcare professionals, the studies were included only if the patients and GPs perspectives were presented separately. Literature of any date and language was included.
Information sources and search strategy
Both systematic and explorative literature searches were used to uncover the field of research in the best possible manner. A systematic search was conducted using the following databases: Medline, CINAHL, PsycInfo, Scopus and EMBASE. All databases were searched from August 2020 until October 2020. The search was renewed on 10 September 2021.
The search was performed by the first author and guided by an information specialist. Validated and pre-tested search filters were used as inspiration for developing our matrix [Citation17,Citation18]. The search strategy included subject indexing terms and free-text terms for title, abstract, and keyword searching. The search terms were grouped into three concepts and arranged per the PCC (population, concept, context) framework as recommended for scoping reviews () [Citation19]. The full version of the search is documented as supplementary material. No restrictions were placed in terms of publication year or country. Simultaneously, an explorative chain search was conducted using reference and citation analyses of the publications identified by the systematic search. In addition, reference lists of included studies were screened for relevant articles, and experts’ literature and libraries were also screened.
Table 1. Search matrix.
Study selection
All identified studies were uploaded to Endnote (https://endnote.com/). Doublets were removed prior to importation to the reference programme Covidence.org. Before study selection, the predefined eligibility criteria were pilot-tested in a sample of 50 articles (SBT, MM, and BN). Two authors (SBT and BN) independently screened the remaining titles and abstracts, and disagreements were resolved through discussion or via the involvement of a third author (MM). Eligibility does not necessarily have to be established before the literature search in a scoping review; eligibility criteria can be developed as the knowledge of the identified literature grows [Citation20]; accordingly, the eligibility criteria for this scoping review were adjusted after screening the titles.
Data extraction
Two reviewers (SBT, BN) performed data extraction independently using predefined data-extraction spreadsheets. Discrepancies were negotiated until consensus was reached, with a third reviewer (MM) available to resolve conflicts. Data were systematically charted by the following study characteristics: Bibliographic aims; study aims; setting; area of interest; results; conclusion.
Data synthesis
The included studies’ key findings were descriptively summarised and narratively presented. A textual narrative synthesis was applied as described by Lucas et al. This approach comprises a commentary reporting of study characteristics, context, quality, and findings based on differences and similarities among studies [Citation21]. Thus, the extracted studies were first grouped by the perspectives reported (i.e. perspectives of general practitioners and patients with TD2 or COPD). Afterwards, patterns across the studies were identified and presented descriptively and narratively.
Results
Study selection
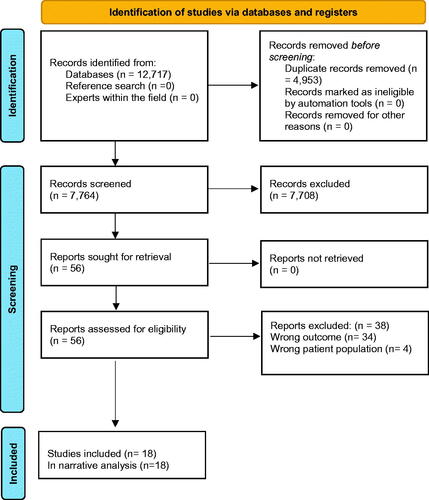
We identified a total of 12,717 studies. After de-duplication, 7764 title abstracts were screened, and 7708 citations were excluded due to wrong outcomes or wrong population, leaving 56 studies for full-text reading, of which 18 studies met the inclusion criteria. The process is illustrated in .
Description of included studies
The included studies were published between 2001 and 2020. Four of the 18 studies were undertaken in Australia [Citation22–25], three in the USA [Citation26–28], two in Sweden [Citation29,Citation30], Norway [Citation31,Citation32], UK [Citation33,Citation34], New Zealand [Citation35,Citation36], and Belgium [Citation37,Citation38], and one in Malaysia [Citation39]. For data collection, semi-structured interviews, focus group interviews, telephone interviews, video recordings, and observations were used. Furthermore, the mixed-methods studies included questionnaires, interviews, and observations. The most frequent investigative methods were content [Citation22,Citation29–31] or thematic [Citation23,Citation25,Citation32,Citation34,Citation38] analysis, whereas one study applied a grounded theory approach [Citation28]. Of the included studies, there was an underrepresentation of studies, including patients with COPD because no studies contained knowledge on the involvement of patients with COPD from the patients’ perspectives and only two from GPs’ perspectives [Citation32,Citation36]. The remaining studies reported on the involvement of patients with TD2 from either the patients’ [Citation22,Citation23,Citation26,Citation29,Citation31,Citation33,Citation38] or GPs’ [Citation24,Citation30,Citation32,Citation36,Citation37] views or a combination thereof [Citation25,Citation27,Citation28,Citation34,Citation35,Citation39]. In , the included studies’ characteristics are presented. The studies comprised 1132 participants (843 patients and 289 GPs), with 10–322 patients with TD2 per study and 4–67 GPs. Most studies applied purposive or randomly selected sampling strategies.
Table 2. Study characteristics.
Narrative synthesis
Patients’ perspectives
Patients reported the importance of GPs providing them with sufficient time for consultations and explaining or discussing things with them. It was essential that the GPs were not too rushed and preoccupied with their own agendas under time-pressure constraints [Citation22,Citation23,Citation28,Citation33,Citation34]. The lack of time to deal effectively with patients’ concerns and the beliefs among the patients were repeatedly mentioned [Citation34]. Similarly, the patients stated that an unfriendly environment with poor attention and lack of eye contact with the GP prevented them from asking questions and expressing their concerns during consultations and made the encounters more doctor-centred [Citation29]. The relational continuity of care was important to the patients, who preferred to see the same GP at each consultation. The patients expressed that they would benefit from the continuity in terms of increased familiarity with their circumstances [Citation23,Citation29,Citation33,Citation34]. In addition, the patients considered it problematic if they did not see the same GP every time because seeing the same GP would make it easier for them to discuss their problems and be more involved in treatment decisions [Citation33]. The patients experienced that GPs differ in behaviour and methods of providing care and information, and the patients preferred to build a relationship with their GP to increase their ability to be more active in treatment decision-making [Citation29]. This relationship was considered a partnership defined as when the competence of the GPs and the patients’ knowledge complemented each other [Citation23,Citation28,Citation31,Citation34,Citation38]. The patients wanted to cooperate with their GP but found it highly difficult if their needs were not listened to [Citation31]. Furthermore, patients reported that their GPs paid too little attention to their health beliefs and the opinions and concepts they held on medicine in general, their illness, and medicine-taking [Citation38]. Patients identified key factors associated with more adequate discussion of their visit’s priorities, including GPs’ willingness to be flexible in the flow of discussion topics and the extent to which their GPs listened to their concerns [Citation28]. It was evident that an active patient/provider alliance was important for engaging the patients in the work of disease management but likely also a critical factor in sustaining the long-term collective work that diabetes management requires [Citation23]. Low literacy was mentioned as a barrier to being involved in treatment decisions because the patients believed that they had to accept what has been demonstrated to them [Citation29]. However, identifying visits’ priorities in advance enhanced a proactive and collaborative approach, made it possible for the patients to bring what they wanted to discuss, and did not prevent the GPs from talking about what they wanted to express. Thus, a personalised approach offered by GPs was valued and the patients expressed a wish that the GPs should be better at listening in a more holistic approach [Citation23,Citation31].
General practitioners’ perspectives
GPs mentioned high workload as a major problem affecting their interactions with the patients because building good relationships with patients takes time [Citation25,Citation30]. GPs expressed the negative impact of time constraints on the ideal goal of entirely electing patient priorities; being in a rush, they often had their own agenda overriding the patient’s agendas [Citation28]. A good relationship with patients was considered necessary in relation to involving them in treatment decisions [Citation25,Citation30,Citation32,Citation36,Citation37]. The GPs’ knowledge about their patients appeared to be important in assessing whether they could rely on the patient’s own judgement about the necessity for treatment and hospitalisation. They believed the patients were good at assessing their needs themselves [Citation32]. Some GPs suggested that there should be a personal interest of healthcare providers in care and to show interest to the patients. Furthermore, they proposed avoiding giving instructions to the patients but, rather, having good communication and respecting their concerns; such an approach would be a more helpful way to correct the patients’ understanding of their disease and gain their cooperation [Citation30]. The GPs indicated that they favoured active involvement of the patient’s experiential knowledge due to having lived with the disease not necessarily reflecting a biomedical need but also the requirement for relieving anxiety and meeting challenges in the patients’ social lives [Citation32,Citation35]. Consequently, there could be discrepancies between the GPs’ and patients’ judgments, which the GPs had to balance. According to the GPs, a lack of patients’ consent to treatment or hospital referral seemed particularly challenging [Citation32].
GPs noted that a tool to empower patients to help them formulate their top priorities at consultations would be helpful, and the GPs liked the idea of pre-visit preparation [Citation28]. The GPs acknowledged that there should be potential for flexibility in the application of guidelines and that involving patients in decision-making was an important consideration in delivering high-quality care. However, they believed that it was more caring to insist upon treating a patient’s disease than to respect any patient preference and that they should endeavour to persuade patients to accept their advice. The GPs saw their primary responsibility as doing whatever was necessary to minimise the possibility of achieving less-than-ideal outcomes. GPs often experienced a conflict between the two professional responsibilities of achieving ideal health outcomes for their patients and respecting their patients’ rights to make decisions where compromise is often necessary [Citation32].
Discussion
Main findings
Across studies and perspectives, our findings indicate that time at consultation, relational continuity, and a good GP–patient relationship are important for providing and facilitating patient involvement. These findings align with research showing that continuity in care, a supportive consultation environment with a warm and caring GP, and a good patient–GP interaction is significant in chronic disease management [Citation14,Citation37].
Patients’ perspectives
For the patients, their GP must pay attention to their health beliefs, opinions and concepts they hold about their treatments, illnesses, and medicines, corroborating findings from Kennedy et al. who found that healthcare providers’ understanding of their patients’ healthcare beliefs, values, and preferences is considered important by both patients and healthcare providers. If these providers listen and communicate with patients, they are more likely to develop a shared understanding that may improve future decision-making [Citation40]. This approach is also supported by McMillan [Citation41], who found that the patients’ beliefs and opinions regarding their disease and treatment affect their self-management. Exploring patients’ beliefs and values is crucial to understanding how to provide patient-centred care.
GPs’ perspectives
However, in some of the included studies, the interviewed GPs experienced conflicts between their professional responsibilities of achieving what they consider ideal health outcomes for their patients and respecting their patients’ health beliefs and their rights to be involved in decisions. Abu Hassan et al. found that exploring patients’ concerns and beliefs to treatment is crucial to assist physicians in delivering patient-centred care because negative concerns and beliefs towards treatments or decisions made by the physician might cause barriers to accepting the treatment [Citation42]. Thus, patients’ knowledge and health beliefs and GPs personal knowledge about a specific patient should be acknowledged as a conceptual resource for patient involvement, but how the GPs should balance their own and patients’ preferences should be explored further. However, these aspects apply mainly to patients with TD2 and their GPs because no studies were found reporting on patients with COPD. Only two studies reported on GPs’ perspectives on the involvement of patients with COPD. This literature gap is of concern, given the association between stigma-related experiences and essential patient outcomes and the fact that there are many unmet healthcare needs among patients with COPD [Citation43]. Furthermore, research shows that many people with lung disease have faced stigma due to their condition and research lacks awareness of this aspect [Citation44]. Furthermore, patients with lung disease tend to feel isolated, which makes it even more important to engage patients with COPD to be more involved in treatment decisions [Citation45]. Thus, the included studies indicate that focus and action must be directed towards research exploring patients with COPD perspectives on patient involvement in general practice.
Strengths and limitations
This study was designed and reported in line with the recommendations of the PRISMA-ScR statement [Citation16]. Multiple databases were searched, and a thorough search strategy was designed iteratively by the research team and an information specialist to account for the three different dimensions of the search (patients with TD2 or COPD, patients’ involvement, and general practice). All aspects of data collection, extraction, and analysis were carried out independently by two researchers, with a third party available for mediation in cases of disagreements. The primary limitation of this scoping review is the sparse literature related to our objectives that may be caused by choice to focus on chronic obstructive pulmonary disease (COPD) and type 2 diabetes (TD2) as they are the two most prevalent chronic conditions that are managed by GPs in Western countries [Citation14,Citation15,Citation46–48]. On the other hand, no results were found to suggest that the perspectives of patients with COPD and type 2 diabetes regarding involvement should differ considerably from those of patients suffering from other chronic conditions. The quality of the included studies was not assessed because this is not typically a part of a scoping review due to an effort to maintain a broad perspective and include studies with different methods and designs.
Conclusion
A good GP–patient relationship was considered an important aspect in relation to providing and facilitating for involvement of patients with COPD or TD2. Furthermore, conflicts between GPs’ professional responsibility of achieving the best health outcome for their patients and respecting patients’ health beliefs are relevant factors in patient involvement. The lack of studies investigating patient involvement in general practice of patients with COPD or TD2 may suggest the need for further research. Our findings indicate that the need for future research is vital for patients with COPD.
Authors’ contributions
Design of protocol: SBT, MM, MSR, BN. Search strategy and search: STB, MM, MSR, BN. TiAb screening: SBT, BN. Full text reading: SBT, BN. Data extraction, analysis, and synthesis: SBT, BN. Manuscript: SBT, MM, BN.
PRISMA-ScR-Checklist
Download MS Word (121.4 KB)Supplemental Material: The search strategies applied for the four databases
Download MS Word (25.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability material
Full search string available as supplementary material.
References
- Boote J, Wong R, Booth A. ‘Talking the talk or walking the walk?’ A bibliometric review of the literature on public involvement in health research published between 1995 and 2009. Health Expect. 2015;18(1):44–57. Epub 2012/10/05.
- Pii KH, Schou LH, Piil K, et al. Current trends in patient and public involvement in cancer research: a systematic review. Health Expect. 2019;22(1):3–20. Epub 2018/11/01.
- British Medical Association. Patient and public involvement: a tool kit for GPs. London: British Medical Association; 2015. [cited 2022 November28]. Available from: https://www.bma.org.uk/media/1938/bma-patient-and-public-involvement-2015.pdf
- Kennedy AP, Rogers AE. Improving patient involvement in chronic disease management: the views of patients, GPs and specialists on a guidebook for ulcerative colitis. Patient Educ Couns. 2002;47(3):257–263. Epub 2002/06/29.
- Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making. 2015;35(1):114–131. Epub 2014/10/30.
- Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181(6):566–577.
- Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):Cd001431.
- Bailey RA, Pfeifer M, Shillington AC, et al. Effect of a patient decision aid (PDA) for type 2 diabetes on knowledge, decisional self-efficacy, and decisional conflict. BMC Health Serv Res. 2016;16:10.
- Longtin Y, Sax H, Leape LL, et al. Patient participation: current knowledge and applicability to patient safety. Mayo Clin Proc. 2010;85(1):53–62.
- Wensing M, Grol R. Patients’ views on healthcare: a driving force for improvement in disease management. Dis Manage Health Outcomes. 2000;7(3):117–125.
- Farrell C. Patient and public involvement in health: the evidence for policy implementation: a summary of the results of the health in partnership research programme. London: Department of Health; 2004.
- Hajat C, Stein E. The global burden of multiple chronic conditions: a narrative review. Prev Med Rep. 2018;12:284–293.
- Danske Regioner & PLO. Collective agreement between Danish Regions and General Practice; 2018. [Overenskomst om almen praksis]; [cited 2022 November 24]. Available from: https://www.laeger.dk/sites/default/files/overenskomst_om_almen_praksis_ok18_endelig_udgave.pdf
- Marcussen M, Titlestad SB, Lee K, et al. General practitioners’ perceptions of treatment of chronically ill patients managed in general practice: an interview study. Eur J Gen Pract. 2021;27(1):103–110. Epub 2021/06/04.
- Schermer T, van Weel C, Barten F, et al. Prevention and management of chronic obstructive pulmonary disease (COPD) in primary care: position paper of the European Forum for Primary Care. Qual Prim Care. 2008;16(5):363–377.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473.
- Gill PJ, Roberts NW, Wang KY, et al. Development of a search filter for identifying studies completed in primary care. Fam Pract. 2014;31(6):739–745.
- Rogers M, Bethel A, Boddy K. Development and testing of a medline search filter for identifying patient and public involvement in health research. Health Info Libr J. 2017;34(2):125–133.
- The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers’ manual 2015: methodology for JBI scoping reviews. Joanne Briggs Inst. 2015:1–24. [cited 2022 November 28]. Available from: https://nursing.lsuhsc.edu/jbi/docs/reviewersmanuals/scoping-.pdf
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
- Lucas PJ, Baird J, Arai L, et al. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol. 2007;7(1):4.
- Ball L, Davmor R, Leveritt M, et al. Understanding the nutrition care needs of patients newly diagnosed with type 2 diabetes: a need for open communication and patient-focussed consultations. Aust J Prim Health. 2016;22(5):416–422.
- Burridge LH, Foster MM, Donald M, et al. Making sense of change: patients’ views of diabetes and GP-led integrated diabetes care. Health Expect. 2016;19(1):74–86.
- Shortus T, Kemp L, McKenzie S, et al. ‘Managing patient involvement’: provider perspectives on diabetes decision-making. Health Expect. 2013;16(2):189–198.
- Dao J, Spooner C, Lo W, et al. Factors influencing self-management in patients with type 2 diabetes in general practice: a qualitative study. Aust J Prim Health. 2019;25(2):176–184.
- Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8(5):410–417.
- Heisler M, Vijan S, Anderson RM, et al. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med. 2003;18(11):893–902.
- Grant RW, Altschuler A, Uratsu CS, et al. Primary care visit preparation and communication for patients with poorly controlled diabetes: a qualitative study of patients and physicians. Prim Care Diabetes. 2017;11(2):148–153.
- Abdulhadi N, Al Shafaee M, Freudenthal S, et al. Patient-provider interaction from the perspectives of type 2 diabetes patients in Muscat, Oman: a qualitative study. BMC Health Serv Res. 2007;7(1):162.
- Abdulhadi NM, Al-Shafaee MA, Wahlstrom R, et al. Doctors’ and nurses’ views on patient care for type 2 diabetes: an interview study in primary health care in Oman. Prim Health Care Res Dev. 2013;14(3):258–269.
- Oftedal B, Karlsen B, Bru E. Perceived support from healthcare practitioners among adults with type 2 diabetes. J Adv Nurs. 2010;66(7):1500–1509.
- Laue J, Melbye H, Halvorsen PA, et al. How do general practitioners implement decision-making regarding COPD patients with exacerbations? An international focus group study. Int J Chron Obstruct Pulmon Dis. 2016;11(1):3109–3119.
- Dambha-Miller H, Silarova B, Irving G, et al. Patients’ views on interactions with practitioners for type 2 diabetes: a longitudinal qualitative study in primary care over 10 years. Br J Gen Pract. 2018;68(666):e36–e43.
- Pooley CG, Gerrard C, Hollis S, et al. ‘Oh it’s a wonderful practice… you can talk to them’: a qualitative study of patients’ and health professionals’ views on the management of type 2 diabetes. Health Soc Care Community. 2001;9(5):318–326.
- Dowell A, Stubbe M, Macdonald L, et al. A longitudinal study of interactions between health professionals and people with newly diagnosed diabetes. Ann Fam Med. 2018;16(1):37–44. Epub 2018/01/10.
- Halliwell J, Mulcahy P, Buetow S, et al. GP discussion of prognosis with patients with severe chronic obstructive pulmonary disease: a qualitative study. Br J Gen Pract. 2004;54(509):904–908.
- Wens J, Vermeire E, Royen PV, et al. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: a qualitative analysis of barriers and solutions. BMC Fam Pract. 2005;6(1):20.
- Vermeire E, Van Royen P, Coenen S, et al. The adherence of type 2 diabetes patients to their therapeutic regimens: a qualitative study from the patient’s perspective. Pract Diab Int. 2003;20(6):209–214.
- Syed A, Don ZM, Ng CJ, et al. Using a patient decision aid for insulin initiation in patients with type 2 diabetes: a qualitative analysis of doctor-patient conversations in primary care consultations in Malaysia. BMJ Open. 2017;7(5):e014260.
- Kennedy BM, Rehman M, Johnson WD, et al. Healthcare providers versus patients’ understanding of health beliefs and values. Patient Exp J. 2017;4(3):29–37.
- McMillan SS, Kendall E, Sav A, et al. Patient-centered approaches to health care: a systematic review of randomized controlled trials. Med Care Res Rev. 2013;70(6):567–596.
- Abu Hassan H, Tohid H, Mohd Amin R, et al. Factors influencing insulin acceptance among type 2 diabetes mellitus patients in a primary care clinic: a qualitative exploration. BMC Fam Pract. 2013;14:164.
- Rose S, Paul C, Boyes A, et al. Stigma-related experiences in non-communicable respiratory diseases: a systematic review. Chron Respir Dis. 2017;14(3):199–216.
- Berger BE, Kapella MC, Larson JL. The experience of stigma in chronic obstructive pulmonary disease. West J Nurs Res. 2011;33(7):916–932.
- BREATHE the Lung Association. Stigma report. www.lung.ca; 2018. [cited 2022 November 28]. Available from: https://nb.lung.ca/sites/default/files/StigmaReport.pdf
- Bos-Touwen ID, Trappenburg JCA, van der Wulp I, et al. Patient factors that influence clinicians’ decision making in self-management support: a clinical vignette study. PLoS One. 2017;12(2):e0171251.
- Heltberg A, Andersen JS, Kragstrup J, et al. Social disparities in diabetes care: a general population study in Denmark. Scand J Prim Health Care. 2017;35(1):54–63.
- Ahnfeldt-Mollerup P, Søndergaard J, Barwell F, et al. The relationships between use of quality-of-care feedback reports on chronic diseases and medical engagement in general practice. Qual Manag Health Care. 2018;27(4):191–198.