Abstract
Context
Snake envenomation is one of the neglected health problems in Tanzania. Since most people, especially in rural areas, suffer from its burden, their cases are not documented due to reliance on medicinal plants. Despite the pivotal role of medicinal plants in treating snakebites, there is a paucity of information.
Objective
This review documents medicinal plants used to treat snakebites in Tanzania.
Materials and methods
A systematic search using electronic databases such as PubMed, Google Scholar, Scopus, Science Direct and grey literature was conducted to retrieve relevant information on medicinal plants used to treat snakebites in Tanzania. The review was conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The obtained information from 19 published articles was organized and analysed based on citation frequency.
Results
A total of 109 plant species belonging to 49 families are used as snakebite antivenom in Tanzania. Fabaceae had the highest number of medicinal plants (19.3%). The dominant plant growth forms were trees (35%) and shrubs (33%). Roots were the most frequently used plant part (54%), followed by leaves (26%) and bark (11%). Annona senegalensis Pers. (Annonaceae), Dichrostachys cinerea (L.) (Fabaceae), Suregada zanzibariensis Baill. (Euphorbiaceae), Antidesma venosum E.Mey. ex Tul. (Phyllanthaceae), Cissampelos pareira L. (Menispermaceae) and Dalbergia melanoxylon Guill. & Perr. (Fabaceae) were the most cited medicinal plants.
Conclusions
Tanzania has diverse plants used for snakebite treatment; a few have been analysed for their bioactive components. Further study of the phytochemicals may provide scientific information to develop snakebite drugs.
Introduction
Globally, snake envenomation is considered a neglected disease and a significant public health concern (World Health Organization (WHO) Citation2007). About 5.5 million people are envenomed annually, whereas 9% of the cases are reported in Africa (Chippaux Citation1998; Giovannini and Howes Citation2017). Of the reported cases globally, 36% die due to snakebites, and about 7% survive permanent injuries (WHO Citation2007; Omara Citation2020). These figures can be lower than the truth because most snakebite incidences occur in rural areas where there are insufficient health facilities, and most cases are not recorded (Zolfagharian and Dounighi Citation2015; Yirgu and Chippaux Citation2019; Omara Citation2020). In sub-Saharan Africa, about one million cases of snake envenomation are reported annually, causing 2% of death cases and 1% get permanent injuries (Chippaux Citation2015). In East Africa, 108 and 151 cases of snakebite were reported in Uganda (Wangoda et al. Citation2004) and Kenya (Snow et al. Citation1994), respectively. In Tanzania, there are no proper records on snakebite cases despite diverse types of snakes (Chippaux Citation2011; Kipanyula and Kimaro Citation2015).
Venomous snakes are found in most parts of the world, in all climatic conditions except in frozen environments and at higher altitudes (WHO Citation2007; Kasturiratne et al. Citation2008). Africa alone is a home of 400 different snake types, whereby nearly 50% are found in East Africa. Some of them are black mamba (Dendroaspis polylepis Günther (Elapidae)), spitting cobra (Naja nigricollis Hallowell (Elapidae)), Rufous-beaked snake (Ramphiophis rostratus Peters (Psammophiidae)), puff adder (Bitis arietans Parker (Viperidae)) and green mamba (Dendroaspis jamesoni Traill (Elapidae)) (Kipanyula and Kimaro Citation2015; Omara Citation2020). Snakebites are life-threatening due to the scarcity of proven medication. Although antivenom serum has been developed as a lifesaving option, it is associated with the development of immediate or delayed hypersensitivity (anaphylaxis or serum sickness) and does not avert local tissue damage (Maya Devi et al. Citation2002). For example, an antidote such as immunoglobulin G produced in horses could react to serum and cause sickness, renal failure and anaphylaxis (Cannon et al. Citation2008; Giovannini and Howes Citation2017). Still, antivenom administration is considered chiefly a definitive treatment for snakebites. Other treatments include respiratory support therapy, surgical of affected necrosis tissues or even amputation (Cannon et al. Citation2008; de Moura et al. Citation2015).
Regardless of the funding issues, there is a paucity of snake venom antiserum in most African countries, predominantly rural areas. Tanzania faces a similar problem that makes the rural inhabitants depend on traditional medicines, particularly herbal remedies (Maregesi et al. Citation2013). Other reasons for reliance on traditional medication are distance to medical facilities, poor infrastructure, storage conditions, scarcity of antidotes in hospitals, restricted application, traditional beliefs, and the high cost of antivenom and modern facilities (Giovannini and Howes Citation2017; Steinhorst et al. Citation2021; Kacholi and Amir Citation2022). Therefore, the use of medicinal plants in addressing snakebite problems has been increasing in the modern era due to their safety, effectiveness, cultural preferences, inexpensiveness, abundance and availability (Maregesi et al. Citation2013; Omara et al. Citation2020). Despite the critical role of medicinal plants in combating snakebite problems, there is no specific ethnobotanical study that has compiled data on medicinal plants used to manage snakebites in Tanzania. Thus, this review fills that gap by documenting medicinal plants used in various parts of the country to treat snakebites.
Methods
Description of the country
Tanzania is a country located in East Africa, covering an area of 947,303 km2. It is bordered in the North by Uganda, South by Malawi and Mozambique, Northeast by Kenya, East by the Indian Ocean and Comoro Island, Southwest by Zambia, and West by Burundi, Rwanda and the Democratic Republic of Congo. The country is estimated to have about 56.31 million population, making it the second-most-populous country south of the equator after South Africa. The population comprises over 120 ethnic groups with different beliefs and cultural practices. The great African lakes are partly within this country. Lake Victoria, Africa’s largest lake, is located to the north; Lake Tanganyika, Africa’s deepest lake, is to the west, and Lake Nyasa lies to the south. Africa’s highest mountain, Mount Kilimanjaro, is found on the north-eastern side of the country.
Literature search strategy
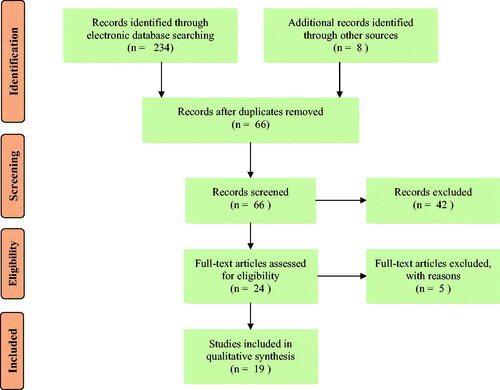
This systematic review has compiled information on ethnomedicinal plants used to treat snakebites in different parts of Tanzania. The study was conducted following the recommendations stated in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Liberati et al. Citation2009). The PRISMA flow diagram is presented in . A web-based literature search was carried out using various electronic databases, including Google Scholar, Web of Science, African Journals Online (AJOL), Science Direct, Scopus, PubMed, Wiley online library and grey literature to access relevant studies. The following search terms and combinations were used to gather relevant studies; medicinal plants, traditional medicines, ethnomedicine, ethnopharmacology, ethnobotany, alternative medicine, antivenin plants, antivenom, antitoxin, antiophidian, snake antidotes, antisera, snakebite, snake envenomation and Tanzania.
All the searches were conducted independently in all the databases, and only articles published and theses or dissertations having any of the above key terms were considered. The studies written in the English language were only searched and considered. Finally, Tanzanian traditional medicinal plants exclusively utilized to treat snakebites were selected. Records from outside Tanzania, ethnoveterinary studies, pharmacological studies and reviewed articles were excluded from the present study. Also, the studies with no scientific names and the plant parts used were excluded. Studies that possessed required information, such as family name, scientific name, local name, growth habits, method of preparation (if available) and route of administration (if available), were extracted. The precision of the botanical names was also searched and confirmed in botanical databases such as International Plant Names Index (https://www.ipni.org) and Tropicos (https://www.tropicos.org).
Data analysis
Microsoft Excel software (Redmond, WA) was employed to analyse the frequency distribution of families, plant parts, growth forms and routes of administration. Moreover, the distribution in regions where the medicinal plants were reported was analysed. The results are presented in figures and tables.
Results and discussion
Distribution of medicinal plants
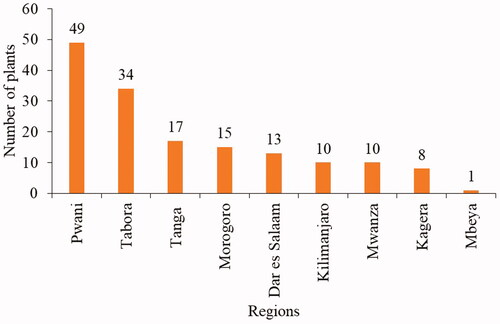
This study has used 19 ethnobotanical studies from nine regions in the country. This indicates that studies on the prevalence of snakebites in different regions of Tanzania are limited (Kipanyula and Kimaro Citation2015). The regions with the highest ethnomedicinal records were Pwani (49 species) and Tabora (34 species). The remaining regions had less than 17 medicinal plants (). The high number of reported antivenin plants in the Pwani and Tabora regions indicates that the locals in the two regions have good indigenous knowledge of the use of plants, and perhaps the regions have many snakebite incidences.
Diversity of medicinal plants
This review reports 109 plant species belonging to 49 families to manage snakebite problems (). Globally, the highest number of medicinal plants used against snakebites was reported from India (Upasani et al. Citation2017), while in sub-Saharan Africa, Ethiopia (Yirgu and Chippaux Citation2019) recorded the highest number of plants, followed by Uganda (Omara et al. Citation2020) and Kenya (Omara Citation2020). This is probably because the highest number of ethnobotanical studies and reviews have been conducted in these countries, making the data more accessible. The majority of the documented plants in this review belong to the family Fabaceae 21 (19.3%), followed by Euphorbiaceae nine (8.3%), Rubiaceae seven (6.4%), Asteraceae and Combretaceae, each with four (3.7% each). The remaining 43 families were represented by less than four species each. The most cited plant species were Annona senegalensis Pers. (Annonaceae), Dichrostachys cinerea (L.) (Fabaceae), Antidesma venosum E.Mey. ex Tul. (Phylanthaceae), Cissampelos pareira L. (Menispermaceae) and Dalbergia melanoxylon Guill. & Perr. (Fabaceae) suggesting considerable potential for possessing snake envenomation bioactive compounds that can be isolated and combined with commercial antiserum to prepare snakebite antidotes. Details on all medicinal plant species with their respective family, local names, growth form, part used and the region in which they were reported are summarized in .
Table 1. List of medicinal plants used for treatment of snakebites in rural communities of Tanzania.
The predominance of the family Fabaceae was similarly reported in Uganda (Omara et al. Citation2020), Ethiopia (Yirgu and Chippaux Citation2019) and India (Upasani et al. Citation2017). This family’s highest usage is associated with richness in terms of species and comprehensive coverage of ecological habitats (Kadir et al. Citation2015; Ajao et al. Citation2019). The family Fabaceae is characterized by active phytochemical compounds such as tannins, phenols and alkaloids (Luís et al. Citation2011; Żarnowski et al. Citation2014). Other families reported in this study were also reported to possess antivenin potential for treating or avoiding snakebites in other countries within and outside Africa. For example, Aristolochiaceae and Lamiaceae in Djibouti (Hasan et al. Citation2016; Yirgu and Chippaux Citation2019), Acanthaceae, Apocynaceae, Asteraceae, Euphorbiaceae, Moraceae, Rubiaceae and Rutaceae in India (Upasani et al. Citation2017), Bangladesh (Hasan et al. Citation2016) and Central America (Giovannini and Howes Citation2017), Euphorbiaceae, Asteraceae, Amaryllidaceae and Solanaceae in Uganda (Omara et al. Citation2020), and Malvaceae, Annonaceae, Combretaceae and Lamiaceae in Kenya (Omara Citation2020).
Growth forms of medicinal plants
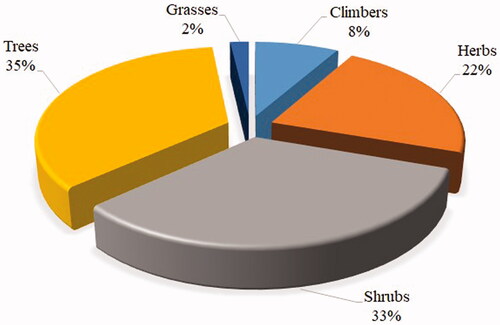
Among the reported medicinal plants in this review, trees (35%) and shrubs (33%) constituted the greatest proportions, followed by herbs (22%), and the remaining growth forms had a small proportion of less than 10% (). The finding is consistent with an ethnobotanical study conducted in Uganda (Omara et al. Citation2020), which reported that trees and shrubs were the most dominant plant growth forms used for making herbal remedies against snakebites. The predominance of trees and shrubs in treating snakebites could be due to their accessibility throughout the year, local socio-cultural beliefs, and the practice of healers in treating snakebites (Asmeron et al. Citation2021; Kacholi and Amir Citation2022). Also, the frequent use of the two growth forms indicates that the locals are conversant with using higher plants in the formulation and preparations of herbal remedies (Kacholi and Amir Citation2022).
Plant parts used
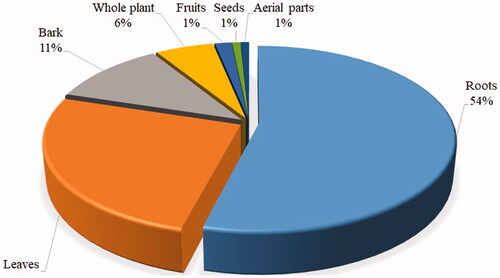
This review observed that locals in Tanzania use different plant parts to treat snakebites. Roots were the most frequently used plant part (54%), followed by leaves (26%), bark (11%) and whole plant (6%). Other parts, such as fruits, seeds and aerial parts, were rarely used (). The common use of roots for treating snakebites was also reported in Kenya (Omara Citation2020), Ethiopia (Yirgu and Chippaux Citation2019), Uganda (Omara et al. Citation2020) and India (Upasani et al. Citation2017). The regular use of roots and leaves in antivenin preparations is a characteristic feature of traditional antivenin therapy (Owuor and Kisangau 2006; Yirgu and Chippaux Citation2019); that is why some of these medicinal plants are named ‘snakeroot’ in some rural communities.
The recurrent use of roots is also reported in treating various ailments in other countries apart from snakebites (Maroyi Citation2013; Jima and Megersa Citation2018; Mathibela et al. Citation2019; Hu et al. Citation2020; Kacholi and Amir Citation2022). Plant roots are believed to possess more bioactive compounds than other parts (Chinsembu Citation2016; Tugume and Nyakoojo Citation2019). The over exploitation of roots for herbal preparations may endanger plants’ existence, especially when uprooting (Kacholi and Mvungi Citation2021). Plants whose roots are preferred for medicinal purposes have been reported to be the most threatened species (Cunningham Citation2001). Thus, this study suggests that local and traditional healers’ awareness of harvesting and conserving medicinal plants is paramount.
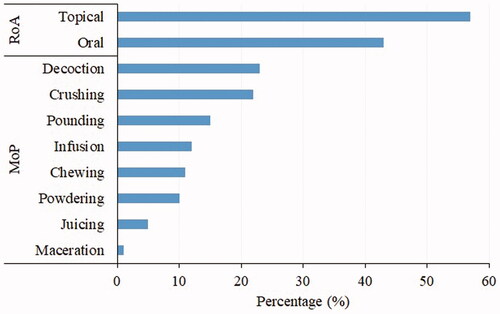
Preparation and administration of remedies
The treatment of snakebite in most of the areas in Tanzania involves mono-preparations of plant extracts, while in a few cases, mixtures of various plants and parts are used to prepare the antidotes. The common mode of preparation of herbal remedies is decoction (23%), followed by crushing (22%) and pounding (15%) (). Other ethnobotanical studies (Yirgu and Chippaux Citation2019; Omara et al. Citation2020) reported decoction as a dominant preparation technique in preparing herbal remedies for snakebite management. On the other side, the most common route of administration of the medicinal plants was topical (57%), followed by oral (43%). Other previous studies showed that herbal remedies could be internal or external, whereas the intake of the plant extract mainly achieves the former, and the latter involves the application of the remedy to the bite site (Snow et al. Citation1994; Omara Citation2020). It should be noted that the study has collected limited information on how remedies are prepared and administered as 35.7% of the reported species lack the information (). Thus, it suggests that a significant effort is still needed to gather information on the mode of preparation and administration route.
Pharmacological evidence against snake venoms
Various pharmacological studies (Núñez et al. Citation2004; Mali Citation2010; Sonibare et al. Citation2016) have proven the wide use of medicinal plants, which revealed that different plant metabolites could antagonize the activity of various crude venoms and purified toxins. For instance, Solanaceae is reported to possess atropine, an alkaloid which inhibits the activity of green and dark mamba (Dendroaspis angusticeps A. Smith (Elapidae) and D. polylepis) venoms by blocking cholinergic nerve terminals (Omara et al. Citation2020). Additionally, the family Aristolochiaceae contains aristolochic acid, an alkaloid that acts similarly to atropine (Kini Citation2005; Kemparaju and Girish Citation2006).
Moreover, the reported species in the present study have been reported elsewhere to have antivenin activities. For instance, the extract from combined roots, bark and leaves of Securidaca longipedunculata Fresen (Polygalaceae) (Sanusi et al. Citation2014), stem bark of Commiphora africana (A.Rich.) Engl. (Burseraceae) (Isa et al. Citation2015), folium extract of Dichrostachys cinerea (L.) Wight et Arn. (Fabaceae) (Agusi and Ogbunachi Citation2018), roots of Capparis tomentosa Lam. (Capparaceae) and Ziziphus mucronata Wild. (Rhamnaceae) (Molander et al. 2014), and those from the whole plant of Euphorbia hirta L. (Euphorbiaceae) inhibit venom activities of N. nigricollis. Also, extracts from leaves and roots of A. senegalensis inhibit venom activities of Echis ocellatus Stemmler (Viperidae), N. nigricollis and B. arietans (Molander et al. 2014), whereas extracts from aerial parts and roots of Cissampelos pareira L. var. orbiculata (DC.) Miq. (Menispermaceae) are reported to neutralize venom activity of Bothrops diporus Cope (Viperidae) (Verrastro et al. 2018). Leaves and roots extracts of Cassia occidentalis L. (Fabaceae) are reported to inhibit venom activities and accelerate wound healing caused by Bothrops moojeni Hoge (Viperidae) (Molander et al. 2014), while the roots and bark extract of Acalypha fruticosa Forssk. (Euphorbiaceae) (Molander et al. 2014), and Paullinia pinnata (Iful 2008; Sanusi et al. Citation2014) are reported to inhibit venom activities of Echis carinatus Schneider (Viperidae). Therefore, the present study highlights the wealthy knowledge locals in Tanzania possess in dealing with snakebites. It also suggests that further pharmacological scrutiny of the recorded medicinal plants is imperative in understanding bioactive compounds that can be used to prepare antivenin in modern science.
Conclusions
This review presents compiled information on medicinal plant species used to treat snakebites in Tanzania. One hundred and nine medicinal plants representing 48 families were documented. Fabaceae and Euphorbiaceae were the families with the highest number of antivenom plants. Trees and shrubs were the most preferred growth forms to prepare herbal remedies for snakebites, and root was the most used plant part. Despite the diversity of plant species used to treat snakebites problems in Tanzania compiled in this review, few have been analysed for their bioactive components and potential for developing modern drugs. Therefore, effort should be geared towards this area to provide scientific information to develop snakebite drugs and solve the major health challenge. We believe that the data presented in this review will provide baseline information for future research on developing modern drugs for treating snakebite.
Author contributions
Conceptualization and data collection, D.S.K. and N.G.M.; data analysis and manuscript writing, D.S.K., O.J.K., N.G.M. and H.A.M.; manuscript revision, D.S.K. and N.G.M.
Disclosure statement
The authors declare that they have no competing interests.
References
- Agusi K, Ogbunachi O. 2018. Effects of ethanolic leaf extract of Euphorbia hirta on Snake Venom Induced Toxicity in Mice. Trop J Appl Nat Sci. 2(2):34–41.
- Ajao AA, Sibiya NP, Moteetee AN. 2019. Sexual prowess from nature: a systematic review of medicinal plants used as aphrodisiacs and sexual dysfunction in sub-Saharan Africa. South Afr J Bot. 122:342–359.
- Amri E, Kisangau DP. 2012. Ethnomedicinal study of plants used in villages around Kimboza forest reserve in Morogoro, Tanzania. J Ethnobiol Ethnomed. 8:1–9.
- Asmerom D, Kalay T H, Araya T Y, Desta DM, Wondafrash DZ, Tafere GG. 2021. Medicinal plants used for the treatment of erectile dysfunction in Ethiopia: a systematic review. BioMed Res Int. 2021:1–12.
- Augustino S, Gillah PR. 2005. Medicinal plants in urban districts of Tanzania: plants, gender roles and sustainable use. Int Forest Rev. 7(1):44–58.
- Augustino S, Hall JB, Makonda FBS, Ishengoma RC. 2011. Medicinal resources of the Miombo woodlands of Urumwa, Tanzania: plants and their uses. J Med Plants Res. 5:6352–6372.
- Cannon R, Ruha A-M, Kashani J. 2008. Acute hypersensitivity reactions associated with administration of Crotalidae polyvalent immune fab antivenom. Ann Emerg Med. 51(4):407–411.
- Chhabra SC, Mahunnah BLA, Mshiu EN. 1987. Plants used in traditional medicine in eastern Tanzania. I. Pteridophytes and angiosperms (Acanthaceae to Canellaceae). J Ethnopharmacol. 21(3):253–277.
- Chhabra SC, Mahunnah RLA, Mshiu EN. 1989. Plants used in traditional medicine in Eastern Tanzania. II. Angiosperms (Capparidaceae to Ebenaceae). J Ethnopharmacol. 25(3):339–359.
- Chhabra SC, Mahunnah RLA, Mshiu EN. 1990a. Plants used in traditional medicine in Eastern Tanzania. IV. Angiosperms (Mimosaceae to Papilionaceae). J Ethnopharmacol. 29(3):295–323.
- Chhabra SC, Mahunnah RLA, Mshiu EN. 1990b. Plants used in traditional medicine in Eastern Tanzania. III. Angiosperms (Euphorbiaceae to Menispermaceae). J Ethnopharmacol. 28(3):255–283.
- Chhabra SC, Mahunnah RLA, Mshiu EN. 1991. Plants used in traditional medicine in eastern Tanzania. V. Angiosperms (Passifloraceae to Sapindaceae). J Ethnopharmacol. 33(1–2):143–157.
- Chhabra SC, Mahunnah RLA, Mshiu EN. 1993. Plants used in traditional medicine in Eastern Tanzania. VI. Angiosperms (Sapotaceae to Zingiberaceae). J Ethnopharmacol. 39(2):83–103.
- Chhabra SC, Mahunnah RLA. 1994. Plants used in traditional medicine by Hayas of the Kagera region, Tanzania. Econ Bot. 48(2):121–129.
- Chinsembu KC. 2016. Ethnobotanical study of medicinal flora utilised by traditional healers in the management of sexually transmitted infections in Sesheke district, Western Province, Zambia. Rev Bras Farmacogn. 26(2):268–274.
- Chippaux JP. 1998. Snake-bites: appraisal of the global situation. Bull World Health Organ. 76(5):515–524.
- Chippaux J-P. 2011. Estimate of the burden of snakebites in sub-Saharan Africa: a meta-analytic approach. Toxicon. 57(4):586–599.
- Chippaux J-P. 2015. Management of snakebites in sub-Saharan Africa. Med Sante Trop. 25(3):245–248.
- Cunningham AB. 2001. Applied ethnobotany: people, wild plant use, and conservation. London: Earthscan.
- de Moura VM, Freitas de Sousa LA, Cristina Dos-Santos M, Almeida Raposo JD, Evangelista Lima A, de Oliveira RB, da Silva MN, Veras Mourão RH. 2015. Plants used to treat snakebites in Santarém, Western Pará, Brazil: an assessment of their effectiveness in inhibiting hemorrhagic activity induced by Bothrops jararaca venom. J Ethnopharmacol. 161:224–232.
- Giovannini P, Howes M-JR. 2017. Medicinal plants used to treat snakebite in Central America: review and assessment of scientific evidence. J Ethnopharmacol. 199:240–256.
- Hasan N, Azam NK, Ahmed N, Hirashima A. 2016. A randomized ethnomedicinal survey of snakebite treatment in southwestern parts of Bangladesh. J Tradit Complement Med. 6(4):337–342.
- Hedberg I, Hedberg O, Madat PJ, Mshigeni KE, Mshiu EN, Samuelsson G. 1983a. Inventory of plants used in traditional medicine in Tanzania. Part II. Plants of the families Dilleniaceae-Opiliaceae. J Ethnopharmacol. 9(1):105–127.
- Hedberg I, Hedberg O, Madati PJ, Mshigeni KE, Mshiu EN, Samuelsson G. 1983b. Inventory of plants used in traditional medicine in Tanzania. Part III. Plants of the families Papilionaceae-Vitaceae. J Ethnopharmacol. 9(2–3):237–260.
- Hilonga S, Otieno JN, Ghorbani A, Pereus D, Kocyan A, de Boer H. 2019. Trade of wild-harvested medicinal plant species in local markets of Tanzania and its implications for conservation. South Afr J Bot. 122:214–224.
- Hu R, Lin C, Xu W, Liu Y, Long C. 2020. Ethnobotanical study on medicinal plants used by Mulam people in Guangxi, China. J Ethnobiol Ethnomed. 16:40.
- Iful ES. 2008. Studies on the antivenom activities of the aqueous extracts of Paullinia pinnata and Detarium microcarpum against Echis carinatus (carpet viper) venom [PhD dissertation]. Jos, Nigeria: University of Jos.
- Isa HI, Ambali SF, Suleiman MM, Abubakar MS, Kawu MU, Shittu M, Yusuf PO, Habibu B. 2015. In vitro neutralization of Naja nigricollis venom by stem-bark extracts of Commiphora africana A. Rich. (Burseraceae). IOSR J Environ Sci Toxicol Food Technol. 9:100.
- Jima TT, Megersa M. 2018. Ethnobotanical study of medicinal plants used to treat human diseases in Berbere district, Bale zone of Oromia regional state, south-east Ethiopia. Evid Based Complement Alternat Med. 2018:1–16.
- Kacholi DS, Amir HM. 2022. Ethnobotanical survey of medicinal plants used by traditional healers in managing gonorrhoea and syphilis in Urambo district, Tabora Region, Tanzania. J Herbs Spices Med Plants. 28(2):179–192.
- Kacholi DS, Mvungi HA. 2021. Plants used by Nyamwezi traditional health practitioners to remedy sexually transmitted infections in Sikonge, Tanzania. J Educ Humanit Sci. 10:89–101.
- Kacholi DS. 2014. Indigenous tree uses, use values and impact of human population on forest size, structure and species richness in Uluguru, Morogoro, Tanzania. Tanz J Sci. 40:34–50.
- Kacholi DS. 2020. Density and aboriginal uses of wild tree species in Milawilila forest reserve in Morogoro region, Tanzania. Tanzania J Sci. 46:85–100.
- Kadir MF, Karmoker JR, Alam M, Jahan SR, Mahbub S, Mia MMK. 2015. Ethnopharmacological survey of medicinal plants used by traditional healers and indigenous people in Chittagong Hill tracts, Bangladesh for the treatment of snakebite. Evid Based Complement Alternat Med. 2015:871675.
- Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, Savioli L, Lalloo DG, de Silva HJ. 2008. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 5(11):e218.
- Kemparaju K, Girish KS. 2006. Snake venom hyaluronidase: a therapeutic target. Cell Biochem Funct. 24(1):7–12.
- Kini RM. 2005. Structure–function relationships and mechanism of anticoagulant phospholipase A2 enzymes from snake venoms. Toxicon. 45(8):1147–1161.
- Kipanyula MJ, Kimaro WH. 2015. Snakes and snakebite envenoming in northern Tanzania: a neglected tropical health problem. J Venom Anim Toxins Incl Trop Dis. 21:32.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. 2009. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 6(7):e1000100.
- Luís Â, Domingues F, Duarte AP. 2011. Bioactive compounds, RP-HPLC analysis of phenolics, and antioxidant activity of some Portuguese shrub species extracts. Nat Prod Commun. 6:1863–1872.
- Mali RG. 2010. Cleome viscosa (wild mustard): a review on ethnobotany, phytochemistry, and pharmacology. Pharm Biol. 48(1):105–112.
- Maregesi S, Kagashe G, Masatu K. 2013. Ethnopharmacological survey of snakebite treatment in Ukerewe Island, Tanzania. Sch Acad J Pharm. 2:381–386.
- Maroyi A. 2013. Traditional use of medicinal plants in south-central Zimbabwe: review and perspectives. J Ethnobiol Ethnomed. 9:31.
- Mathibela MK, Potgieter MJ, Tshikalange TE. 2019. Medicinal plants used to manage sexually transmitted infections by Bapedi traditional health practitioners in the Blouberg area, South Africa. South Afr J Bot. 122:385–390.
- Maya Devi C, Vasantha Bai M, Vijayan Lal A, Umashankar PR, Krishnan LK. 2002. An improved method for isolation of anti-viper venom antibodies from chicken egg yolk. J Biochem Biophys Methods. 51(2):129–138.
- Molander M, Nielsen L, Søgaard S, Staerk D, Rønsted N, Diallo D, Chifundera KZ, Van Staden J, Jäger AK. 2014. Hyaluronidase, phospholipase A2 and protease inhibitory activity of plants used in traditional treatment of snakebite-induced tissue necrosis in Mali, DR Congo and South Africa. J Ethnopharmacol. 157:171–180.
- Núñez V, Otero R, Barona J, Fonnegra R, Jiménez S, Osorio RG, Quintana JC, Díaz A. 2004. Inhibition of the toxic effects of Lachesis muta, Crotalus durissus cumanensis and Micrurus mipartitus snake venoms by plant extracts. Pharm Biol. 42(1):49–54.
- Omara T, Kagoya S, Openy A, Omute T, Ssebulime S, Kiplagat KM, Bongomin O. 2020. Antivenin plants used for treatment of snakebites in Uganda: ethnobotanical reports and pharmacological evidences. Trop Med Health. 48:6.
- Omara T. 2020. Plants used in antivenom therapy in rural Kenya: ethnobotany and future perspectives. J Toxicol. 2020:1828521.
- Owuor BO, Kisangau DP. 2006. Kenyan medicinal plants used as antivenin: a comparison of plant usage. J Ethnobiol Ethnomed. 2:7.
- Ramathal DC, Ngassapa OD. 2001. Medicinal plants used by Rwandese traditional healers in refugee camps in Tanzania. Pharm Biol. 39(2):132–137.
- Ruffo CK. 1991. A survey of medicinal plants in Tabora region, Tanzania. In Traditional medicinal plants, ed. KE Mshigeni, MHH Nkunya, V Fupi, RLA Mahunnah, N Mshiu, 1st ed. Dar es Salaam: Dar es Salaam University Press – Ministry of Health, Tanzania; p. 391–406.
- Salinitro M, Vicentini R, Bonomi C, Tassoni A. 2017. Traditional knowledge on wild and cultivated plants in the Kilombero valley (Morogoro region, Tanzania). J Ethnobiol Ethnomed. 13:17.
- Sanusi J, Shehu K, Jibia AB, Mohammed I, Liadi S. 2014. Anti-snake venom potential of Securidaca longepedunculata leaf and root bark on spitting cobra (Naja nigricollis Hallowel) in envemoned Wister rats. IOSR J Pharm Biol Sci. 9(6):92–96.
- Snow RW, Bronzan R, Roques T, Nyamawi C, Murphy S, Marsh K. 1994. The prevalence and morbidity of snake bite and treatment-seeking behaviour among a rural Kenyan population. Ann Trop Med Parasitol. 88(6):665–671.
- Sonibare MA, Aremu OT, Okorie PN. 2016. Antioxidant and antimicrobial activities of solvent fractions of Vernonia cinerea (L.) Less leaf extract. Afr Health Sci. 16(2):629–639.
- Steinhorst J, Aglanu LM, Ravensbergen SJ, Dari CD, Abass KM, Mireku SO, Adu Poku JK, Enuameh YAK, Blessmann J, Harrison RA, et al. 2021. ‘The medicine is not for sale’: practices of traditional healers in snakebite envenoming in Ghana. PLoS Negl Trop Dis. 15(4):e0009298.
- Tugume P, Nyakoojo C. 2019. Ethno-pharmacological survey of herbal remedies used in the treatment of paediatric diseases in Buhunga parish, Rukungiri district, Uganda. BMC Complement Altern Med. 19(1):353.
- Upasani SV, Beldar VG, Tatiya AU, Upasani MS, Surana SJ, Patil DS. 2017. Ethnomedicinal plants used for snakebite in India: a brief overview. Integr Med Res. 6(2):114–130.
- Verrastro RB, Maria-Torres A, Ricciardi G, Teibler P, Maruñak S, Barnaba C, Larcher R, Nicolini G, Dellacassa EJ. 2018. The effects of Cissampelos pareira extract on envenomation induced by Bothrops diporus snake venom. J Ethnopharmacol. 212:36–42.
- Wangoda R, Watmon B, Kisige M. 2004. Snakebite management: experiences from Gulu regional hospital Uganda. East Cent Afr J Surg. 9:1–5.
- World Health Organization (WHO). 2007. Rabies and envenomings: a neglected public health issue: report of a consultative meeting. Geneva: World Health Organization; p. 32.
- Yirgu A, Chippaux J-P. 2019. Ethnomedicinal plants used for snakebite treatments in Ethiopia: a comprehensive overview. J Venom Anim Toxins Incl Trop Dis. 25:e20190017.
- Żarnowski R, Żarnowska ED, Kozubek A. 2014. Alkylresorcinols in the family Fabaceae. Acta Soc Bot Pol. 70(1):25–29.
- Zolfagharian H, Dounighi NM. 2015. Study on development of Vipera lebetina snake antivenom in chicken egg yolk for passive immunization. Hum Vaccines Immunother. 11:2734–2739.