Abstract
Surgical site infections (SSIs) are common complications after open heart surgery. Fortunately, most are superficial and respond to minor wound debridement and antibiotics. However, 1–3% of patients develop deep sternal wound infections that can be fatal. Late infections with sternocutaneous fistulas, are encountered less often, but represent a complex surgical problem. This evidence-based review covers etiology, risk factors, prevention and treatment of sternal SSIs following open heart surgery with special focus on advances in treatment, especially negative-pressure wound therapy.
Introduction
Most common surgical site infections (SSIs) following cardiac surgery are of the sternotomy wound and the leg following vein harvesting for coronary bypass grafting; most of them being diagnosed in the first month after surgery. Some SSIs, however, can be diagnosed months or even years after surgery; such as chronic sternocutaneous fistulas (SCFs). Modern care of sternal SSIs following open heart surgery involves effective primary prevention and eradication of infection with a low rate of sequelae. This review will cover both early and late SSIs of the sternum.
Pathogenesis of sternal wound infections
Coagulase-negative staphylococci (CoNS), mostly Staphylococcus epidermidis, are the most commonly reported pathogenic agents associated with SSIs following open heart surgery in recent years, followed by the previously most prevalent bacterial agents Staphylococcus aureus and Gram-negative bacteria.[Citation1,Citation2] Less commonly reported agents include streptococci, anaerobic bacteria such as Propionibacterium acnes, Candida albicans, Aspergillus and Mycobacterium tuberculosis.
CoNS belong to the normal flora of the skin and do not cause harm unless there is a breach in the integrity of the skin.[Citation3] Although many subtypes of CoNS have been identified in humans, only a few have been reported to cause disease, the most well known being S. epidermidis.[Citation3] CoNS are commonly found in the sternal wound before closure and may originate from the patient’s own skin as well as from airborne external contamination during surgery.[Citation3] Mediastinitis caused by CoNS has been reported to be associated with diabetes mellitus, obesity, chronic obstructive pulmonary disease (COPD) and typically present at least 10–14 d postoperatively with sternal dehiscence in combination with only moderate increase in C-reactive protein (CRP) levels.[Citation2]
S. aureus is mainly found in the anterior nares of humans, with around 20% of all people being persistent carriers and nasal carriers have increased risk of sternal SSIs.[Citation4] Staphylococcus aureus does not, however, belong to the normal commensal bacteria of the skin on the sternum. Sternal SSIs caused by S. aureus are considered to be caused by intraoperative contamination of the wound, although they often present 2–4 weeks after surgery or even later.
Gram-negative bacteria do not constitute part of the normal skin flora nor are present in the air of operating rooms (ORs) and sternal SSIs are probably caused by contamination or haematogenous spread from other sites during the postoperative period. Sternal SSIs caused by Gram-negatives are reported to show a fulminant course with high CRP levels, sepsis and have high mortality and complication rate. Most deep Gram-negative deep sternal SSIs present early (within 1–2 weeks) after surgery.[Citation1]
P. acnes is an increasingly recognized pathogen, formerly usually regarded as a harmless contaminant, however, P. acnes has been proposed to have a role in postoperative sternal SSIs.[Citation5] P. acnes is regularly not detected in routine bacterial wound samples unless specifically looked for, since specific anaerobic culture techniques are required and longer time to grow in the laboratory.
Early sternal wound infections
Together with atrial fibrillation, kidney injury and perioperative bleeding, SSIs are among the most important complications related to open heart surgery and often result in early significant morbidity including mortality and increased cost of treatment.[Citation6] The reported incidence of SSIs in the sternotomy wound is up to 9.7%.[Citation7,Citation8] Fortunately most sternal SSIs are superficial and respond to minor wound debridement and antibiotics, however, 1–3% patients develop deep sternal wound infections, which can have severe consequences including increased mortality, morbidity and costs.[Citation9]
Definitions and diagnostic criteria
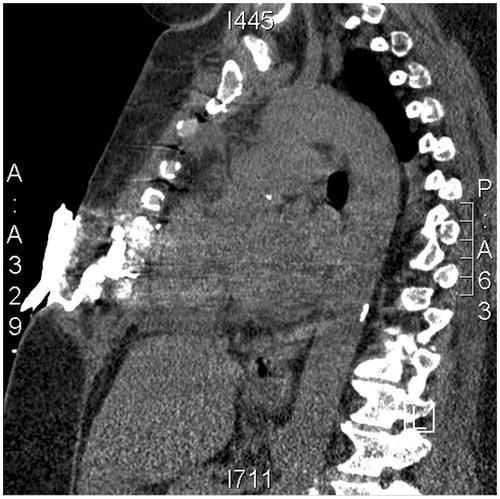
Sternal wound infections can be divided into superficial and deep infections, based on the depth of the infection in the wound. Early infections include both superficial infections, reaching the dermis and subcutaneous tissue, and deep sternal wound infections that reach under the sternum and the anterior mediastinum (). Thus, a DSWI is also often referred to as postoperative mediastinitis. Late infections often comprise a combination of superficial and deep infection and they include osteomyelitis, subcutaneous abscess, and SCF.
Figure 1. (a) Purulent deep sternal wound infection detected one week from surgery. The sternal wires are still in place, (b) the patient after application of a negative wound therapy and (c) one week later. See text for details. Photos: Tomas Gudbjartsson. Published with the courtesy of the Icelandic Medical Journal.

According to the Centre of Disease Control’s (CDC) definition an early superficial infection occurs within 30 d of the operative procedure and involves only skin and subcutaneous tissue of the incision.[Citation10] The CDC definition is presented in .
Table 1. CDC criteria for the diagnosis of DSWI (Horan et al. [Citation10]).
A deep sternal SSIs is specifically defined as an infection that reaches the mediastinum, which is deeper than the sternum. According to CDC, the diagnosis of postoperative mediastinitis requires at least one of the three criteria given in .
The definition of late sternal SSIs is less well defined than that for early infections. There is a large overlap among the various types of late sternal wound infections, including osteomyelitis, subcutaneous abscesses, and chondritis. SCF belongs to this group of late infections and in this review is defined as a draining sinus tract from the sternum to the skin, treated surgically after discharge from hospital with an apparently healed sternotomy wound.
Epidemiology
DSWI most often present as early sternal wound infections, and are the most commonly reported postoperative infections of the sternum. However, although rare, late superficial wound infections can also develop into DSWI. The incidence of DSWI is most often reported to be in the 1–3% range; however, the rates vary considerably due to different patient populations and diagnostic criteria.[Citation8,Citation9]
Superficial sternal wound infections have not been studied as thoroughly as deep infections, due to their much lower morbidity and mortality. The incidence is higher than for DWWI, most often in the 2–6% range.[Citation8,Citation11] These infections are often minor and respond to oral antibiotics or minor wound revision. Risk factors include those for other SSIs, including age and obesity.[Citation8]
Risk factors
A diagnosis of sternal SSIs is most often established in the first days or weeks after the primary operation.[Citation9] Numerous risk factors have been identified; especially for deep SSIs. These can be divided into three categories followed by examples [Citation12,Citation13]:
Preoperative: diabetes mellitus, obesity, peripheral arterial disease, smoking, low left ventricular ejection fraction, chronic renal failure, chronic pulmonary disease.
Perioperative: bilateral use of internal mammary arteries.
Postoperative: longer ventilator support, use of β-adrenergic drugs.
Following the introduction of continuous infusion of insulin during open heart surgery, the importance of diabetes mellitus as an independent risk factor for deep sternal SSIs has diminished.[Citation14] The role of gender as a risk factor for deep sternal SSIs is unclear, female sex has been reported to be associated with both increased risk and reduced risk.[Citation12]
The use of bilateral mammary artery (BIMA) has long been considered a risk factor for deep sternal SSIs when compared to the use of a single left internal mammary artery (LIMA).[Citation15] The decreased vascularization of the sternum following BIMA harvesting is thought to explain the increased SSIs rate.[Citation16] In a recent meta-analysis, the use of BIMA increased the relative risk of deep sternal SSIs by 62% when compared to only LIMA.[Citation15] The risk was most prominent in the elderly and patients with diabetes. The association of sternal wound infections and the use of BIMA was recently challenged in a study with over 1.5 million coronary artery bypass grafting patients were the use of BIMA was not an independent risk factor for DSWI except in patients with chronic complications of diabetes mellitus.[Citation16,Citation17]
The mechanisms by which the risk factors can promote infection are numerous: mechanical force to the wound (e.g. cough related to COPD, re-exploration for bleeding), reduced circulation in the wound (e.g. peripheral arterial disease, diabetes mellitus, smoking, etc.), haematogenous spread (e.g. dialysis for renal failure) and reduced host immunity (e.g. systemic corticosteroids).
Treatment
Once diagnosed, sternal SSIs is initially treated with intravenous antibiotics. First-line antibiotic treatment is commonly intravenous vancomycin, until results from antimicrobial susceptibility tests become available. Cloxacillin and other β-lactamase-resistant staphylococcal antibiotics are commonly used when infection with either S. aureus or CoNS has been established.
In addition to antimicrobial therapy, surgical treatment is generally necessary for deeper sternal SSIs. Although the optimal surgical approach is still debated, at least debridement is necessary. Different approaches can be used to close the wound. Primary intention, i.e. closing of the wound involves drawing the wound edges together. When secondary intention closure approach is applied direct wound closure is not used and instead the wound granulates and heals from below. A more common approach is to use tertiary intention or delayed primary wound closure. The wound is then left open, only debrided and observed and then closed several days later. When wounds are closed with delayed primary closure the sternal halves can usually be re-wired together as in the primary operation – or more securely with the Robicsek technique if there is a risk of fracture of the sternum.[Citation18]
Conventional treatment (CvT)
The earliest treatment for DSWI was revision of the wound, followed by either open wound dressings or closed irrigation. Open wound dressing changes involve frequent changes of paraffin gauzes. The first adjunct therapy was the use of antibiotic irrigation of the wound, or closed irrigation.[Citation19]
Regardless of the method used for treating the infection it is essential to secure the stability of the sternum before delayed primary closure. Cases of right ventricle perforation have been reported due to the sternal halves tearing the ventricle wall.[Citation20] Unclosed wound also impairs pulmonary function, often requiring prolonged intubation of the patient. For delayed closure an unstable sternum can be fixated with a titanium plate.[Citation21]
Soft tissue flap transposition may be required to fill a sternal defect. Use of the omentum as a soft tissue flap is a well-known approach that was first described in 1976.[Citation22] After subtotal sternectomy, followed by transposition of the highly vascularized greater omentum is mobilized to the sternal defect and the wound later closed by delayed primary intention.
A muscle flap is often used instead of an omental flap to fill the sternal defect, most often the pectoralis muscle, but in some cases the rectus abdominis muscle.[Citation23] A particularly difficult problem after reconstruction using muscle flaps is chronic pain and/or sternal instability, which has been reported in over 40% of cases.[Citation31] Abdominal hernias following omental transfer can occur, and may require surgical intervention.
Recurrent sternal SSIs is not uncommon and their treatment can be challenging. They are more frequently seen following irrigation, open wound dressing treatment and other forms of older treatment methods compared to the newer treatment were negative-pressure wound therapy is used.[Citation24–26]
Negative-pressure wound therapy
Negative-pressure wound therapy (NPWT) is a newer treatment modality that can stabilize the sternum and promote granulation of the wound. It was first described in 1999 by Obdeijn et al. that reported successful use of NPWT in three patients with deep sternal SSIs.[Citation27] Since then, numerous studies have provided strong empirical evidence of the usefulness of NPWT for these complex infections.
NPWT promotes wound healing in wounds through removal of debris and excess fluids by creating negative pressure or vacuum, in a well-sealed wound. NPWT increases the perfusion of the wound and facilitates granulation tissue formation. Furthermore, it has been suggested that promotion of wound healing by NPWT occurs by modulation of cytokines to an anti-inflammatory profile, and mechanoreceptor and chemoreceptor-mediated cell signalling, culminating in angiogenesis, extracellular matrix remodelling and deposition of granulation tissue.[Citation28] An NPWT device has four separate elements: (i) a pump that generates negative pressure within a tightly sealed wound, (ii) dressing materials that both fill the wound (usually polyurethane foam) and cover it (adhesive drape), (iii) non-collapsible tubing that removes fluid from the wound, and (iv) a container to collect the fluid and debris that are removed from the wound by the vacuum created in the system. A number of different commercially available NPWT systems are available today.
Treatment of DSWI with NPWT () starts with reasonable debridement of clearly nonviable tissue followed by several layers of paraffin gauze that are placed at the bottom of the sternal wound to prevent injury to the anterior wall of the right ventricle. Polyurethane foam is the cut to fit the wound and covered with a sterile wound drape. Then a tube for transmission of pressure is attached through a hole in the drape (). Studies have shown that the negative pressure applied to the wound increases microvascular blood flow a few centimeters from the wound.[Citation29] Gauze may also be used instead of polyurethane foam with similar results.[Citation30]
Most often the negative pressure in a sternal wound is applied at a continuous pressure of −125 mmHg,[Citation31] but diastasis of the foam has been shown to be more pronounced at pressures less than −100 mmHg.[Citation32,Citation33]
Usually the wound is re-opened after 2–4 d with NPWT. Based on three modalities: (i) clinical observation of the wound during debridement; (ii) infection-related laboratory findings (primary CRP, but also leucocyte counts); and finally, (iii) multiple tissue cultures, the clinician will have the tools to determine whether the wound is sterile and the proliferative stage of wound healing has begun.[Citation34] If the wound has not healed, new foam is placed and negative pressure applied. Most often patients with DSWI require several (often 2–4) dressing changes as part of the NPWT treatment (). This includes the initial debridement with foam placement, subsequent dressing changes, and after the infection has subsided, sternal rewiring with skin closure by delayed primary closure.[Citation35,Citation36]
Complications of negative-pressure wound therapy
Complications related to NPWT are generally minor, usually involving pain at the edges of the wound that most often subsides shortly after initiation of the negative pressure. Light bleeding can also seen due to in-growth of granulation tissue into the foam. Other minor wound complications, that are often preventable, include erosion of the wound edges caused by foam lying over the wound edge onto the healthy skin and pressure sores caused by mislaid evacuation tubes.[Citation37] Major bleeding is the most serious and a potentially fatal complication of NPWT in the sternal wound. It can be seen when the sponge dressings are changed or when negative suction is first introduced to the sponge. There was a concern during the early experience of NPWT for deep sternal SSIs that this could cause rupture of the right ventricle due to displacement of the heart towards the thoracic wall and possible contact of the right ventricle with the edge of the sternum.[Citation20] However, large series has demonstrated very few major bleedings when using proper technique.[Citation40]
Outcome of treatment
Mortality due to DSWIs was 20–45% before more advanced surgical techniques were developed.[Citation38] However, in more recent reports the mortality ranges between 1% and 14%.[Citation35,Citation39,Citation40] Patients treated surgically for DSWIs most often require extended hospital stay with multiple interventions to cure the infection and they do not have improved quality of life after surgery to the same degree as patients without sternal wound infections.[Citation41]
Long-term mortality and morbidity is negatively associated by DSWIs, which is reflected in a long-term study by Braxton et al. where the adjusted hazard ratio for all-cause mortality 10 years after the primary operation in patients with DSWIs was almost doubled.[Citation42] Early sternal SSIs also increase the risk of late chronic infections (SCF).[Citation38]
Advances of NPWT compared to other treatments are improved sternal stabilization and earlier mobilization.[Citation43] It has, however, been debated whether NPWT is truly superior to older techniques in treating patients with DSWI. In a systematic review of randomized trials of NPWT for various acute or chronic wounds Ubbink et al. concluded that there was no evidence to support that NPWT was superior to conventional treatment, and they called for more randomized controlled trials.[Citation44] Unfortunately randomized trials comparing NPWT and conventional treatment are few and concerns about publication bias have been raised.[Citation45] Despite this lack of evidence, currently many institutions prefer NPWT for the treatment of sternal wound infections.
Generally the overall cost of sternal SSIs treatment is no higher with NPWT than with conventional treatment. In a study by Mokhtari et al. from 2008 the total cost of NPWT treatment for sternal SSIs patients was similar to conventional treatment and was 2.5 times higher than for non-SSIs patients.[Citation46] The material cost is greater using NPWT, however, as this technique is less laborious with wound changes only two or three times a week, this results in similar or even reduced total cost.[Citation40] Importantly randomized studies are lacking that prove that NPWT is economically superior to other techniques used for sternal SSIs.
Late sternal wound infections
The most commonly described late sternal wound infection is SCF, an abnormal passage or communication between the sternum and the surface of the skin (). Fistulas following open heart surgery have not received much attention, and most reports are case studies. The incidence in a Swedish University hospital was 0.26% as well as in a nationwide study from Iceland.[Citation47,Citation48] The time to first intervention ranges from a few weeks up to months and even years.
Previous treatment for DSWI, history of previous cardiac operations and advanced age have been shown to be associated with SCF in case series.[Citation25,Citation49] A case–control study found that treatment for early sternal wound infections, renal failure, history of smoking and the use of bone wax were strong independent risk factors for SCF.[Citation47] Bone wax has been shown to both inhibit bone healing and induce chronic inflammation in sternal wounds in a porcine animal model.[Citation50] Foreign objects could also play a role, but in a study of 50 cases of complicated sternal wound reconstructions using titanium plates, there was only one case of SCF.[Citation21]
Previously, there may have been a bias towards publishing cases with rare pathogens in SCFs, but in recent series gram positive cocci have been shown to be most common, followed by gram-negative bacteria and C. albicans.[Citation51]
Treatment and outcome
Treatment of SCF most often entails numerous surgical interventions and prolonged antibiotic treatment. In some cases infections associated with SCF can be treated adequately with antibiotics alone as shown by Tocco et al. where 45 out of 70 patients remitted with medical treatment alone.[Citation51] However, many patients require surgical treatment to eradicate the infection.[Citation47,Citation48,Citation51]
Conventional surgical treatment involves debridement, removal of infected wires, and then closure of the wound. Traditionally, in long-standing SCF a radical excision of parts of the sternum may be needed to eradicate the underlying infection, followed by soft tissue flap surgery to fill up the sternal defect. SCF can become a recurrent problem despite combination of adequate antibiotic therapy with conventional surgical treatment and NPWT.[Citation47] Persistent SCF reduces the patient’s quality of life due to chronic leakage from the wound. The short-term mortality has been shown to be increased and the long-term survival impaired with 58% of patients with SCF being alive at five years compared to 85% in a control group.[Citation47]
Prevention and prophylactic measures
Means to reduce intraoperative wound contamination include measures to reduce airborne contamination in the OR by use of tight scrub-suits and laminar airflow. The use of plastic adhesive drapes on the skin is commonly practiced but can be questioned, since it has not been shown to reduce SSIs and might even increase the recolonization of the skin and wound.[Citation52]
There is evidence that preoperative nasal screening for S. aureus and decolonization can reduce hospital-acquired wound infections. Furthermore, an approach of active surveillance of nasal MRSA, careful contact with carriers, proper hand hygiene, and awareness among staff can reduce transmission and infections with MRSA.[Citation53] Postoperative contamination of wounds through haematogenous spread from intravenous and arterial catheters are best prevented by use of coated catheters, proper hygiene routines among all staff and early removal of all catheters.
The importance of meticulous surgical technique including discriminative use of electrocautery and bone wax, preservation of blood supply to tissues and reduction of bleeding with subsequent reoperation and transfusions is fundamental and well documented.[Citation54] Sternal instability or dehiscence may be a consequence of an SSIs but also by itself promotes bacterial growth. A mechanically rigid fixation of the sternal halves reduces the infection rate. Less than 7 sternal fixation wires has been shown to increase the risk of DSWI, and the standard use of 9 or more wires has even been proposed.[Citation55] Several new techniques with wires (single vs. figure-of-eight), cables, plates or other devices have been published although more evidence from adequately powered, prospective, controlled studies is needed. The technique with lateral reinforcement (Robicsek), however, did not reduce the incidence of sternal wound complications in high-risk patients in a large randomized controlled multicentre trial.[Citation56] Smoking is a risk factor and preoperative cessation of smoking reduces postoperative complications including wound infections.[Citation57] Suboptimal postoperative blood glucose control increases the risk and protocols for avoiding postoperative hyperglycaemia are important and generally implemented.[Citation14]
The SSI rate is reduced to approximately 1/5 by using antibiotic prophylaxis compared to placebo and is recommended for all cardiac surgery.[Citation58] Antibiotics should be present in the tissues before contamination occurs and the first dose given immediately preoperatively. Extending the prophylaxis to more than 48 h has no additional effect and a duration of 24 h may be sufficient. A second- or third-generation cephalosporin is recommended to cover susceptible staphylococci as well as Gram-negative agents. Cloxacillin is also used and despite this very low rates of SSIs caused by Gram-negative are reported with this policy, supporting that intraoperative contamination may be of little importance in Gram-negative infections.[Citation59,Citation2] The use of glycopeptide antibiotics (vancomycin or teicoplanin) has been proposed in settings with high prevalence of MRSA, even though glycopeptides were inferior to beta-lactam antibiotics in a meta-analysis and are reported to increase the risk of acute kidney injury.[Citation60,Citation61]
Local antibiotic prophylaxis using collagen-gentamicin sponge has been evaluated in several studies, including four large randomized controlled trials, retrospective studies and in meta-analyses.[Citation62] In brief, all randomized controlled trials but one,[Citation63] showed a reduction in SWI, including a recent meta-analysis.[Citation62]
In addition to intravenous prophylactic antibiotics and tight per- and postoperative glycemic control local application of vancomycin, seems to reduce the incidence of sternal wound infection after cardiac surgery.[Citation64] There are however concerns regarding potentially high serum levels and the risk of selection of resistant strains to this important antibiotic. The use of antibacterial sutures with triclosan (2,4,4′-trichloro-2′-hydroxy-diphenylether), which is an antibacterial substance which reduces the growth of bacteria by inhibiting the fatty acid synthesis, has been shown in randomized studies to reduce the rate of leg wound infection [Citation65] but not for sternal SSIs.[Citation66,Citation67]
Conclusions
The knowledge of SSIs following open heart surgery has increased over the last decades and much is known about the pathogenesis, prevention and treatment. Furthermore, in modern open heart surgery practice the rate should be low and when an infection occurs, treatment measures should be swift and effective. Using of state of the art techniques, early mortality due to SSIs should be close to none, although long-term survival might still be affected.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Gardlund B, Bitkover CY, Vaage J. Postoperative mediastinitis in cardiac surgery – microbiology and pathogenesis. Eur J Cardiothorac Surg. 2002;21:825–830.
- Friberg O, Svedjeholm R, Kallman J, et al. Incidence, microbiological findings, and clinical presentation of sternal wound infections after cardiac surgery with and without local gentamicin prophylaxis. Eur J Clin Microbiol Infect Dis. 2007;26:91–97.
- Widerstrom M, Wistrom J, Sjostedt A, et al. Coagulase-negative staphylococci: update on the molecular epidemiology and clinical presentation, with a focus on Staphylococcus epidermidis and Staphylococcus saprophyticus. Eur J Clin Microbiol Infect Dis. 2012;31:7–20.
- Munoz P, Hortal J, Giannella M, et al. Nasal carriage of S. aureus increases the risk of surgical site infection after major heart surgery. J Hosp Infect. 2008;68:25–31.
- Unemo M, Friberg O, Enquist E, et al. Genetic homogeneity/heterogeneity of Propionibacterium acnes isolated from patients during cardiothoracic reoperation. Anaerobe. 2007;13:121–126.
- El Oakley RM, Wright JE. Postoperative mediastinitis: classification and management. Ann Thorac Surg. 1996;61:1030–1036.
- Berg TC, Kjorstad KE, Akselsen PE, et al. National surveillance of surgical site infections after coronary artery bypass grafting in Norway: incidence and risk factors. Eur J Cardiothorac Surg. 2011;40:1291–1297.
- Ridderstolpe L, Gill H, Granfeldt H, et al. Superficial and deep sternal wound complications: incidence, risk factors and mortality. Eur J Cardiothorac Surg. 2001;20:1168–1175.
- Steingrimsson S, Gottfredsson M, Kristinsson KG, et al. Deep sternal wound infections following open heart surgery in Iceland: a population-based study. Scand Cardiovasc J. 2008;42:208–213.
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–332.
- Crabtree TD, Codd JE, Fraser VJ Jr., et al. Multivariate analysis of risk factors for deep and superficial sternal infection after coronary artery bypass grafting at a tertiary care medical center. Semin Thorac Cardiovasc Surg. 2004;16:53–61.
- Borger MA, Rao V, Weisel RD, et al. Deep sternal wound infection: risk factors and outcomes. Ann Thorac Surg. 1998;65:1050–1056.
- Sjogren J, Nilsson J, Gustafsson R, et al. The impact of vacuum-assisted closure on long-term survival after post-sternotomy mediastinitis. Ann Thorac Surg. 2005;80:1270–1275.
- Furnary AP, Zerr KJ, Grunkemeier GL, et al. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg. 1999;67:352–360. discussion 60-2.
- Dai C, Lu Z, Zhu H, et al. Bilateral internal mammary artery grafting and risk of sternal wound infection: evidence from observational studies. Ann Thorac Surg. 2013;95:1938–1945.
- Itagaki S, Cavallaro P, Adams DH, et al. Bilateral internal mammary artery grafts, mortality and morbidity: an analysis of 1 526 360 coronary bypass operations. Heart. 2013;99:849–853.
- Kajimoto K, Yamamoto T, Amano A. Coronary artery bypass revascularization using bilateral internal thoracic arteries in diabetic patients: a systematic review and meta-analysis. Ann Thorac Surg. 2015;99:1097–1104.
- Robicsek F, Daugherty HK, Cook JW. The prevention and treatment of sternum separation following open-heart surgery. J Thorac Cardiovasc Surg. 1977;73:267–268.
- Bryant LR, Spencer FC, Trinkle JK. Treatment of median sternotomy infection by mediastinal irrigation with an antibiotic solution. Ann Surg. 1969;169:914–920.
- Sartipy U, Lockowandt U, Gabel J, et al. Cardiac rupture during vacuum-assisted closure therapy. Ann Thorac Surg. 2006;82:1110–1111.
- Cicilioni OJ Jr., Stieg FH 3rd, Papanicolaou G. Sternal wound reconstruction with transverse plate fixation. Plast Reconstr Surg. 2005;115:1297–1303.
- Lee AB Jr., Schimert G, Shaktin S, et al. Total excision of the sternum and thoracic pedicle transposition of the greater omentum; useful strategems in managing severe mediastinal infection following open heart surgery. Surgery. 1976;80:433–436.
- Jurkiewicz MJ, Bostwick J 3rd, Hester TR, et al. Infected median sternotomy wound. Successful treatment by muscle flaps. Ann Surg. 1980;191:738–744.
- Petzina R, Hoffmann J, Navasardyan A, et al. Negative pressure wound therapy for post-sternotomy mediastinitis reduces mortality rate and sternal re-infection rate compared to conventional treatment. Eur J Cardiothorac Surg. 2010;38:110–113.
- Sjogren J, Gustafsson R, Nilsson J, et al. Clinical outcome after poststernotomy mediastinitis: vacuum-assisted closure versus conventional treatment. Ann Thorac Surg. 2005;79:2049–2055.
- Steingrimsson S, Gottfredsson M, Gudmundsdottir I, et al. Negative-pressure wound therapy for deep sternal wound infections reduces the rate of surgical interventions for early re-infections. Interact Cardiovasc Thorac Surg. 2012;15:406–410.
- Obdeijn MC, de Lange MY, Lichtendahl DH, et al. Vacuum-assisted closure in the treatment of poststernotomy mediastinitis. Ann Thorac Surg. 1999;68:2358–2360.
- Glass GE, Murphy GF, Esmaeili A, et al. Systematic review of molecular mechanism of action of negative-pressure wound therapy. Br J Surg. 2014;101:1627–1636.
- Wackenfors A, Gustafsson R, Sjogren J, et al. Blood flow responses in the peristernal thoracic wall during vacuum-assisted closure therapy. Ann Thorac Surg. 2005;79:1724–1730. discussion 30-1.
- Malmsjo M, Gustafsson L, Lindstedt S, et al. The effects of variable, intermittent, and continuous negative pressure wound therapy, using foam or gauze, on wound contraction, granulation tissue formation, and ingrowth into the wound filler. Eplasty. 2012;12:e5.
- Isago T, Nozaki M, Kikuchi Y, et al. Effects of different negative pressures on reduction of wounds in negative pressure dressings. J Dermatol. 2003;30:596–601.
- Mokhtari A, Petzina R, Gustafsson L, et al. Sternal stability at different negative pressures during vacuum-assisted closure therapy. Ann Thorac Surg. 2006;82:1063–1067.
- Borgquist O, Ingemansson R, Malmsjo M. The influence of low and high pressure levels during negative-pressure wound therapy on wound contraction and fluid evacuation. Plast Reconstr Surg. 2011;127:551–559.
- Gustafsson R, Johnsson P, Algotsson L, et al. Vacuum-assisted closure therapy guided by C-reactive protein level in patients with deep sternal wound infection. J Thorac Cardiovasc Surg. 2002;123:895–900.
- Sjogren J, Gustafsson R, Nilsson J, et al. Negative-pressure wound therapy following cardiac surgery: bleeding complications and 30-day mortality in 176 patients with deep sternal wound infection. Interact Cardiovasc Thorac Surg. 2011;12:117–120.
- Gustafsson RI, Sjogren J, Ingemansson R. Deep sternal wound infection: a sternal-sparing technique with vacuum-assisted closure therapy. Ann Thorac Surg. 2003;76:2048–2053. discussion 53.
- Braakenburg A, Obdeijn MC, Feitz R, et al. The clinical efficacy and cost effectiveness of the vacuum-assisted closure technique in the management of acute and chronic wounds: a randomized controlled trial. Plast Reconstr Surg. 2006;118:390–397. discussion 8-400.
- Sarr MG, Gott VL, Townsend TR. Mediastinal infection after cardiac surgery. Ann Thorac Surg. 1984;38:415–423.
- Baillot R, Cloutier D, Montalin L, et al. Impact of deep sternal wound infection management with vacuum-assisted closure therapy followed by sternal osteosynthesis: a 15-year review of 23,499 sternotomies. Eur J Cardiothorac Surg. 2010;37:880–887.
- Tarzia V, Carrozzini M, Bortolussi G, et al. Impact of vacuum-assisted closure therapy on outcomes of sternal wound dehiscence. Interact Cardiovasc Thorac Surg. 2014;19:70–75.
- Jideus L, Liss A, Stahle E. Patients with sternal wound infection after cardiac surgery do not improve their quality of life. Scand Cardiovasc J. 2009;43:194–200.
- Braxton JH, Marrin CA, McGrath PD, et al. 10-year follow-up of patients with and without mediastinitis. Semin Thorac Cardiovasc Surg. 2004;16:70–76.
- Sjogren J, Malmsjo M, Gustafsson R, et al. Poststernotomy mediastinitis: a review of conventional surgical treatments, vacuum-assisted closure therapy and presentation of the Lund University Hospital mediastinitis algorithm. Eur J Cardiothorac Surg. 2006;30:898–905.
- Ubbink DT, Westerbos SJ, Nelson EA, et al. A systematic review of topical negative pressure therapy for acute and chronic wounds. Br J Surg. 2008;95:685–692.
- Peinemann F, McGauran N, Sauerland S, et al. Negative pressure wound therapy: potential publication bias caused by lack of access to unpublished study results data. BMC Med Res Methodol. 2008;8:4.
- Mokhtari A, Sjogren J, Nilsson J, et al. The cost of vacuum-assisted closure therapy in treatment of deep sternal wound infection. Scand Cardiovasc J. 2008;42:85–89.
- Steingrimsson S, Gustafsson R, Gudbjartsson T, et al. Sternocutaneous fistulas after cardiac surgery: incidence and late outcome during a ten-year follow-up. Ann Thorac Surg. 2009;88:1910–1915.
- Steingrimsson S, Sjogren J, Gudbjartsson T. Incidence of sternocutaneous fistulas following open heart surgery in a nationwide cohort. Scand J Infect Dis. 2012;44:623–625.
- Jones G, Jurkiewicz MJ, Bostwick J, et al. Management of the infected median sternotomy wound with muscle flaps. The Emory 20-year experience. Ann Surg. 1997;225:766–776. discussion 76-8.
- Vestergaard RF, Jensen H, Vind-Kezunovic S, et al. Bone healing after median sternotomy: a comparison of two hemostatic devices. J Cardiothorac Surg. 2010;5:117.
- Tocco MP, Ballardini M, Masala M, et al. Post-sternotomy chronic osteomyelitis: is sternal resection always necessary? Eur J Cardiothorac Surg. 2013;43:715–721.
- Webster J, Alghamdi AA. Use of plastic adhesive drapes during surgery for preventing surgical site infection. Cochrane Database Syst Rev. 2007;CD006353.
- Jain R, Kralovic SM, Evans ME, et al. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med. 2011;364:1419–1430.
- Chelemer SB, Prato BS, Cox PM Jr., et al. Association of bacterial infection and red blood cell transfusion after coronary artery bypass surgery. Ann Thorac Surg. 2002;73:138–142.
- Shaikhrezai K, Robertson FL, Anderson SE, et al. Does the number of wires used to close a sternotomy have an impact on deep sternal wound infection? Interact Cardiovasc Thorac Surg. 2012;15:219–222.
- Schimmer C, Reents W, Berneder S, et al. Prevention of sternal dehiscence and infection in high-risk patients: a prospective randomized multicenter trial. Ann Thorac Surg. 2008;86:1897–1904.
- Thomsen T, Villebro N, Moller AM. Interventions for preoperative smoking cessation. Cochrane Database Syst Rev. 2014;3:CD002294.
- Kreter B, Woods M. Antibiotic prophylaxis for cardiothoracic operations. Meta-analysis of thirty years of clinical trials. J Thorac Cardiovasc Surg. 1992;104:590–599.
- Friberg O, Dahlin L-G, Kallman J, et al. Collagen-gentamicin implant for prevention of sternal wound infection; long-term follow-up of effectiveness. Interact Cardiovasc Thorac Surg. 2009;9:454–458.
- Olsson DP, Holzmann MJ, Sartipy U. Antibiotic prophylaxis by teicoplanin and risk of acute kidney injury in cardiac surgery. J Cardiothorac Vasc Anesth. 2014;2015;29:626–631.
- Bolon MK, Morlote M, Weber SG, et al. Glycopeptides are no more effective than beta-lactam agents for prevention of surgical site infection after cardiac surgery: a meta-analysis. Clin Infect Dis. 2004;38:1357–1363.
- Kowalewski M, Pawliszak W, Zaborowska K, et al. Gentamicin-collagen sponge reduces the risk of sternal wound infections after heart surgery: meta-analysis. J Thorac Cardiovasc Surg. 2015;149:1631–1640.
- Bennett-Guerrero E, Ferguson T, Lin M, et al. Effect of an implantable gentamicin-collagen sponge on sternal wound infections following cardiac surgery: a randomized trial. JAMA. 2010;304:755–762.
- Lazar HL, Ketchedjian A, Haime M, et al. Topical vancomycin in combination with perioperative antibiotics and tight glycemic control helps to eliminate sternal wound infections. J Thorac Cardiovasc Surg. 2014;148:1035–1038. 8-40.
- Thimour-Bergstrom L, Roman-Emanuel C, Schersten H, et al. Triclosan-coated sutures reduce surgical site infection after open vein harvesting in coronary artery bypass grafting patients: a randomized controlled trial. Eur J Cardiothorac Surg. 2013;44:931–938.
- Seim BE, Tonnessen T, Woldbaek PR. Triclosan-coated sutures do not reduce leg wound infections after coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2012;15:411–415.
- Steingrimsson S, Thimour-Bergström L, Roman-Emanuel C, et al. Triclosan-coated sutures and sternal wound infections: a prospective randomized clincial trial. Eur J Clin Microbiol Infect Dis. 2015;34:2331–2338.