ABSTRACT
Challenges facing general practice are multiple and extreme. Amongst them is the increasing difficulty of recruiting and retaining General Practitioners (GPs). GPs cite heavy workload, work-related stress, little family time and psychological ill-health as factors influencing their decisions to leave or reduce working hours. Analysis of the literature suggests that these factors, amongst others, are present in GP training and trainees have similar experiences. An in-depth understanding of the challenges trainees in difficulty face is lacking.
Our research aim was to better understand the factors that trainees perceive contribute to their failure to progress in training. A qualitative approach was adopted using semi-structured interviews with GP trainees identified as failing to progress satisfactorily or failing the MRCGP examinations. Interviews were audio-recorded and transcribed. Thematic analysis was used to understand the unique experiences of GP trainees and find common themes.
Twenty-three interview transcripts were analysed. Emergent themes were presented using a framework of three distinct categories to aid data organisation and allocating themes and sub-themes: professional factors, personal factors, and social factors. Difficulties with managing work-load, poor motivation, lack of family time and psychological ill-health were significant themes for many. This study supports the evidence that difficulties facing GPs take root in training. Failure to fully understand trainees’ journeys and associated challenges reduces opportunities to provide bespoke packages of care and remediation that fully address their needs.
Introduction
To complete their training, general practice (GP) trainees in the United Kingdom (UK) must successfully complete the MRCGP examination: the Applied Knowledge Test (AKT), the Clinical Skills Assessment (CSA) and the Workplace-Based Assessment (WPBA)[Citation1]. Minimising the likelihood of failure is an important part of the training, as well as ensuring that enough GPs come through GP training programmes to replace those who leave the profession[Citation2]. Reasons for GP trainees failing the AKT include insufficient knowledge of clinical medicine, poor evidence interpretation, and a lack of understanding about the organisation of primary care[Citation3]. The reasons for GP trainees failing the CSA are similar but also include poor clinical management, data gathering and interpersonal skills [Citation4,Citation5].
Whilst these reasons relate to performance on the day of assessment, research suggests a number of other factors are associated with failure at assessment. These include: GP trainee demographics (non-UK status, black and ethnic minority background and male gender) [Citation6,Citation7]; issues related to day-to-day practice; training and education (heavy workload, reduced work–life balance, poor trainee–trainer relationship) [Citation8–10]; health and well-being (stress, burnout and mental illness) [Citation11,Citation12]; conduct and attitude (motivation, low confidence, poor reflective capacity) [Citation13,Citation14]; and finance [Citation14–16].
Whether these factors cause, or simply correlate with the failure has produced much debate[Citation17]. Nevertheless, remediation interventions continue to focus on further knowledge and skills development[Citation18], rather than address contextual factors surrounding the failure. Although recommended as evidence-based interventions for supporting trainees, there is limited empirical basis for the effectiveness of many remediation interventions over the long term, and even less suggesting they are able to prevent future failure at assessment [Citation9,Citation19]. Given the potential cost to the individual, the training programme, and the wider healthcare system associated with GP trainees who fail to progress in their training, investigating the mechanisms and how they lead to this outcome should be a priority research area.
Whilst knowing factors that predict the likelihood GP trainees failing the CSA is important[Citation20], it is necessary to know the way various factors interact to affect trainees’ study and work[Citation21]. Prediction models help identify trainees who may benefit from additional support at the start of their training[Citation22], but not all trainees who fail are detected this way. Understanding how factors manifest themselves through the eyes of trainees and through everyday experiences may provide a new way for educators to identify ‘at risk’ trainees early in their training.
Research in improved predictions of those who fail has often been driven by the data collected about trainees or a training programme. The aim of this research was to explore how trainees in the UK perceived the factors influencing their ability to pass examinations and how these interact to affect their day-to-day experience of the GP training programme. By exploring the problem of failure to progress in training from the trainee angle, new insights into the way risk factors interact at an individual level (at trainee level or level of the GP trainer, the practice or the training programme) will better inform support interventions for GP trainees.
Methods
Setting
This research was undertaken as part of a larger programme of remediation commissioned by Health Education England East Midlands (HEE-EM) for GP trainees struggling at high-stakes assessments (e.g. AKT or CSA).
Sample
GP trainees identified as failing to progress by the Professional Support Unit (PSU) at HEE-EM were invited to participate in the research. Criteria for failing to progress, or at risk of failing to progress, were defined as: (i) failing the CSA, or (ii) concerns raised through either the trainee’s educational supervisor or through the Annual Review Competence Progression (ARCP) process, or (iii) identified through a composite risk calculated from their educational supervisor report, multi-source feedback and patient satisfaction questionnaire[Citation22]. Eligible participants were contacted and invited to take part (Supplementary Box 1).
Data collection
Semi-structured interviews were conducted with GP trainees. A topic guide was developed by exploring training experiences (Supplementary Table 1) and included areas such as motivation, work–life balance, and health[Citation23]. Trainees were encouraged to reflect on their experiences. All interviews were digitally recorded and transcribed. Transcripts were excluded if a trainee was not in a formal training programme at the time of interview, if they did not fully engage in the interview process, or did not want the interview to be included in research activities.
Data analysis
All interview data were analysed by hand and the approach followed a three-stage thematic analysis process [Citation24,Citation25] including an initial review and coding of the data, categorising codes into themes, and organising themes into networks[Citation24]. Thematic analyses presented as thematic networks ‘enables a methodical systematisation of textual data, facilitates the disclosure of each step of the analytic process, aids the organisation of an analysis and its presentation, and allows a sensitive, insightful and rich exploration of a text’s overt structures and underlying patterns’[Citation25]. Themes within a thematic network were ordered to represent: (i) basic themes (micro-themes derived from the textual data); (ii) organising themes (principal assumptions of a cluster of basic themes revealing more); (iii) global themes (macro-themes to summarise and make sense of clusters of themes).
Results
Forty-three interviews were undertaken with trainees for over 12 months. Twenty-three were included in the analysis. Of those excluded, 13 were reluctant to fully engage with the process, two were not in training at the time of interview and in five interviews the interviewer did not explore all aspects of the interview schedule. Participant demographics are described in .
Table 1. Participant demographics
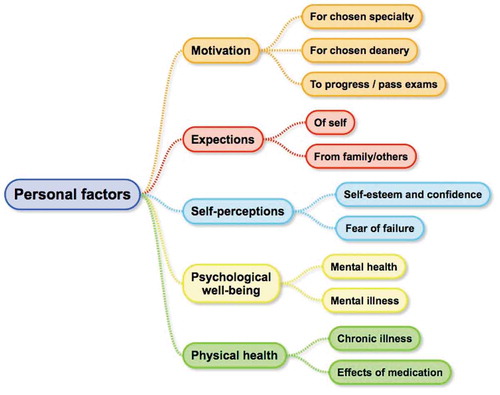
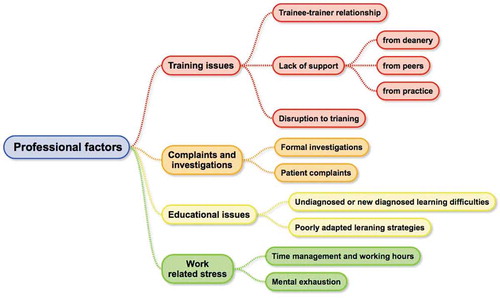
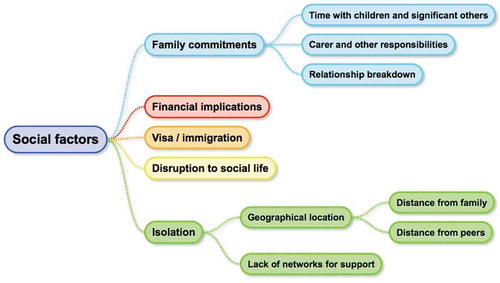
For the scope and purpose of this study, the analysis focused on identifying and describing the factors affecting GP trainee performance. The emergent themes are presented in three (global) categories: personal factors (relating to personal beliefs, perceptions, psychological health and well-being), professional factors (day-to-day work experience, training and development) and social factors (maintaining family life and work–life balance). Supporting quotes were chosen to illustrate sub-themes (organising themes) associated with each global theme, demonstrating the richness of the stories recorded.
Personal factors
Five organising themes () with associated sub-themes emerged from the data relating to personal factors.
Motivation
Trainees’ motivation changed based on their experiences and enjoyment of other specialities, how flexible their posts were and their work–life balance, as experienced at different points in training.
‘I wasn’t really certain about general practice … I probably was leaning towards cardiology more, because I really loved it.’ (Trainee 9)
Trainees describing lacking a clear reason for choosing GP who then went on to fail exams discussed reduced motivation for continuing.
‘I’ve definitely thought about leaving … there’s not a lot of motivation to stay in, I’m definitely having second thoughts about, you know.’ (Trainee 3)
Expectations
Trainees felt burdened by the expectations of others to complete training. A sense of duty or obligation pushed them to continue.
‘I basically tried the sticking to work … see if I could get better without having any time off … I’d be letting down colleagues, letting down family … ’ (Trainee 21)
Self-perceptions
Trainees self-confidence and own judgements about their ability as doctors were low. Some were able to recognise this as a contributing factor to their difficulties, rather than a belief that they lacked the ability to pass.
‘I think it’s probably a lack of confidence on my part … because actually … I’m not much less bright than them … I just didn’t believe in myself … ’ (Trainee 21)
Others were more resigned to failure and described a sense of hopelessness.
‘This failure is something that completely has rocked the boat … personally, mentally it has rocked me … confidence level has plummeted … I’m struggling to make simple decisions, and I’m just hating myself to be in this position’. (Trainee 6)
On the other hand, some trainees retained their self-confidence and perceived themselves as ‘excellent’ trainees despite failure, with concern about reputational damage rather than not progressing.
‘I didn’t prepare for it [CSA], I took it and failed, so I won’t count it as a failure because it was just, you just went to play … but the moment I got into GP everybody started saying I was a star!’ (Trainee 5)
Psychological well-being
A state of heightened anxiety resulted from worry about working in day-to-day practice, along with the prospect of having to study in preparation for the examination re-sit. Following failure, participants reported feeling low and withdrawing from others.
‘I wish I can do something just to have one day without this fear and feeling actually, the one that the CSA has brought on. Just one day where I can rest and relax, be myself.’ (Trainee 6)
Whilst some trainees recognised a deterioration in their mental health and acted appropriately, others were less aware and less able to prioritise their health above their training needs.
‘I think in hindsight I probably should have sought support from my doctor maybe, support from other people … I didn’t do it at the time.’ (Trainee 1)
Physical illness
Newly-diagnosed illnesses were significant challenges, especially when combined with difficulty in getting through the working day whilst studying for re-sits.
‘I guess the fact that it [health problem] came back has made me look more – be more anxious about the future … is my medical condition compatible with what I’m trying to do … being a GP.’ (Trainee 23)
The chronic nature of some illnesses resulted in participants reflecting on what would happen if their conditions deteriorated, especially as they were already struggling to manage their illness alongside studying.
‘it’s a degenerative condition, so it’s not going to get better … it’s ******** … That’s a big unknown for me … that’s something that I’m going to have to deal with and consider.’ (Trainee 10)
Professional factors
Four organising themes () with associated sub-themes were identified within this category.
Training issues
The quality of the trainer–trainee relationship had the most bearing on participants’ training experience. An absent or non-existent relationship with their trainer caused stress, low motivation and risked psychological health.
‘When you have a supervisor who you can share everything [with], it’s like it’s a good chemistry which leads you to favourable results, I think I was lacking that.’ (Trainee 19)
Going beyond lack of support, trainees described destructive and damaging relationships as a significant source of stress.
‘She [supervisor] just has a lot of criticism … I just found it upsetting what she said … she put me off general practice and I had second thoughts about working in general practice for a while … in one of the consultations she just laughed at it, and I found that very insulting.’ (Trainee 3)
Finding and developing a meaningful relationship with a supervisor proved difficult. Trainees felt supervisors rarely engaged with them at key stages of the programme (e.g. at the start and in the first few months). Participants often found trainers did not necessarily appreciate how much or little they actually knew.
‘I was very disappointed for example with my clinical supervisor’s report. My clinical supervisor thought that I was not organised, thought I was late a lot of times, and that I thought was a complete lie.’ (Trainee 20)
Complaints and investigations
Patient complaints, formal investigations, or concerns raised by a colleague caused significant stress. Trainees described eroded confidence, damaged motivation and a fear these would remain with them psychologically and professionally for the rest of their careers.
‘I still carry that aura, of person who done a big mistake … I try to present myself in certain cases, which I’ve done totally right, people still think, he should have done this in a better way … I have to live with it … ’ (Trainee 13)
Educational issues
For those who received a new learning needs diagnosis during the training programme, there was relief as they often long suspected something was wrong. However, there was still an element of fear that the diagnosis would compromise their progress.
‘They labelled me … It [dyslexia] wasn’t actually a massive shock to me, it was actually more of a relief at kind of knowing why I was struggling, cause you’re just sat thinking, is it me? Am I a bit thick? Am I just doing things wrong? … It doesn’t solve the problem, but it gives me a bit more insight.’ (Trainee 11)
Participants generally lacked knowledge and understanding about learning strategies most appropriate for postgraduate training.
‘It’s hard to say how I’ve been studying, I haven’t really studied … in my professional life. I mean, I did some ad-hoc reading around patients … I don’t really have a system of studying … ’ (Trainee 4)
Work-related stress
Workplace stress was common. Trainees described competing daily demands (meetings, home visits, administrative tasks) and the pressure to perform these in the least possible time as unbearable.
‘The most difficult thing is a lot of things to do and you have to fit all these things … you work for long hours, you come back tired … And there’s still more to do. And whatever you do it’s not enough … it never ends.’ (Trainee 18)
After failing the CSA, and against the backdrop of struggling to manage their time, trainees felt anxious about making mistakes, or missing things for fear of being labelled as lacking time management skills. Trainees neglected taking breaks in favour of being seen to carry on.
‘Half the time I don’t really tend to have time to eat … there’s always something to do.’ (Trainee 14)
Trainees described mental exhaustion causing anxiety and tiredness long after they had left for the day. This was often normalised by others as being ‘part and parcel of general practice’. These day-to-day experiences were cited as the first triggers for thinking that their chosen career may not be for them.
‘I was doing so many long ten to twelve hour shifts … on the days I did have off … mentally, I couldn’t focus’. (Trainee 9)
‘It’s a very busy practice … All the partners are full-time, and that’s kind of the ethos that they have … It always feels very busy and stressed.’ (Trainee 14)
Social factors
Five organisational themes () with associated sub-themes were identified within this category.
Family commitments
Despite choosing GP for the perceived career flexibility, participants reported difficulties finding quality time for family.
‘ … I have three children … we’ve been through quite a lot actually, very difficult time. My life has turned out upside down since I started this GP.’ (Trainee 6)
Workload taking a toll on family relationships resulted in further feelings of stress, anxiety and guilt. Participants felt angry at themselves for letting their family down as a consequence of failure in the CSA.
‘I hate myself for wasting my children’s childhood right now, because that’s a time where I should’ve been taking and just having quality time … I hate myself.’ (Trainee 6)
The caring responsibilities of participants were not confined to children, but extended to elderly parents, or other dependents.
‘ … both my parents are disabled and were quite unwell during that year as well, so that was quite a lot of stress added on top.’ (Trainee 11)
Invariably, tensions within the family caused strained relationships with partners, and in some cases led to relationship breakdowns, with inevitable impact on training experience and study.
‘I had a number of sort of issues with my marriage and so on and ended up getting divorced.’ (Trainee Citation15)
Financial implications
The direct costs of failure were significant. In addition, the more hidden costs, including revision courses, required further resourcing, sometimes beyond what participants could afford.
‘Not only is it [CSA] mentally a burden but financially it could be a burden. Because it’s not just the exam, it’s the courses, it’s the booking of accommodation, it’s the transport … all adds up.’ (Trainee 7)
‘I’m basically broke now because of the exams and going part-time and other things. I was in a much happier place before coming to GP.’ (Trainee 6)
The need to ensure sufficient available funds provoked stress, especially among those who had turned to part-time working. The challenge was arguably greatest for participants who were sending money aboard to support family not domiciled in the UK.
‘But I’ve got this sense of financial responsibility to my mum and my younger sisters as well, and I try and send them money every month.’ (Trainee 5)
Visa and immigration status
Non-UK participants felt constantly on-edge as a consequence of their visa requirements and restraints. In many cases, these participants needed to ensure they were always in employment or risk non-renewal of visas, and being asked to leave the UK. Similarly, failure at assessment risked lengthening the training programme, something participants were keen to avoid.
‘I have only fourteen days extra to find a job once my training finishes … I think my training would finish in first week of August and my visa is valid ‘til nineteenth of August 2017 … That’s a pressure.’ (Trainee 16)
Disruption to social life
Failure in the CSA led participants to sacrifice time with family and friends for time working on their portfolios or studying for the re-sit.
‘This weekend I’m probably just going to end up spending working on my e- portfolio … I’d planned to meet up with a friend but had my supervisor meeting and I got told that I needed to do more of my e-portfolio.’ (Trainee 3)
There was a sense of resentment towards the situation and a feeling that this was to be expected by supervisors as a consequence of their predicament. Left unchecked, some participants felt regrets around choosing their career path.
‘I didn’t expect this … I would have been frightened off if people had told me that if you are an ST3 this is how you are – your lifestyle is going to be. I would be like, no, I probably don’t want this.’ (Trainee 16)
Isolation
The inability to put down roots as a consequence of having to frequently move was challenging. Every new move brought a sense of ‘starting again’ with respect to friends or acquaintances. A sense of belonging never increased and if anything, was eroded.
‘I don’t really have any friends up here, I don’t really know anyone up here … so it’s kind of like difficult to be an outsider.’ (Trainee 10)
In principle, the idea of moving around to gain exposure to different training experiences was never questioned, but the distances that participants were having to travel was regularly cited as unnecessary. It often meant time away from family, causing a sense of loss and emotional hardship. Participants were convinced this kind of separation impacted on their training, as well as their prospects in the exam.
‘Staying away from the family … it’s a long time. For the first two and a half years, it was alright. But this last six months, it has been really difficult, just staying away has been difficult.’ (Trainee 2)
Discussion
This study found a complex network of factors leading GP trainees to struggle and fail the CSA. These included personal, social and professional factors, none of which operated in isolation. Trainees discussed the emotional turmoil, particularly in the context of having sacrificed so much to arrive at this point. They discussed the psychological impact on their professional identity and the toll failure took on their own self-esteem and psychological well-being. The impact failure had on their motivation to continue with training was apparent, with trainees feeling overwhelmed and burdened by the demands of their programme.
Strengths and limitations
Semi-structured interviews were used to ensure in-depth discussion and a sensitive exploration of the emotions associated with trainees’ experiences and cognitions behind their perception of failure.
One limitation of the research was the sampling method and recruitment. Individuals who fail at assessment may be desperate to participate in anything perceived to help them get through the next exam diet, therefore engagement with this research may have been unconsciously influenced by trainees’ wanting to receive more teaching and feedback on performance. The findings from this research specifically related to the sample population in this study, and may be less generalisable to the wider trainee population. There is evidence of ‘excellent’ trainees who may be exposed to similar challenges yet not succumb to failure or enter into difficulty[Citation26]. Likewise, there was no longitudinal element to this research. The findings relate to a particular point in time rather than a pattern of behaviour and set of circumstances consistent across a number of high-stakes exam failures.
This study explores GP trainees’ experiences of failing the CSA and demonstrates that performance on the day of the exam was likely determined as much by the complex interplay between professional, personal and social factors, as it was individual knowledge or skills alone. This study identified that trainees take exams in the face of challenging training-related issues, difficult personal circumstances, and work-related stress and poor psychological well-being. This is a reminder that sitting professional exams alongside being in employment continues to be a significant challenge for healthcare professionals. The findings confirm trainees who possessed low self-esteem and suffered threats to their psychological or physical health, appeared to have a greater degree of ambivalence towards their chosen speciality after failing the CSA. Finally, this research highlights that failure in the CSA has consequences for the individual far beyond simply the additional study required, but impacts on their friends, family and finances.
The implications of this research are wide-ranging, particularly around ways trainees who fail the CSA could be better supported in future, and policy around the structure of GP training programmes more widely.
The experience of GP trainees who fail the CSA strengthens the case to develop better methods for identifying trainees in difficulty well before they fail at assessment. Traditionally, students and trainees are perceived as homogeneous populations according to their stage of training, academic rank or past performance [Citation7,Citation22,Citation27] Growing evidence demonstrates more heterogeneity among student/trainee populations, each with a different ‘success trajectory’ based on academic and non-academic characteristics. Novel methods using machine learning and artificial intelligence techniques are now being used to give greater precision for detecting those at high risk of failure, for example one US medical school used 53 variables to predict ‘success potential’ in over 1000 students[Citation28]. The use of more ‘dynamic’ variables to predict success, which consider how trainees, trainers and training environments interact on a daily basis is likely to explain a greater proportion of variance.
Seeking support for specified difficulties (such as a learning difficulty) is generally straightforward, though not always timely [Citation29,Citation30]. This research demonstrates the challenge of accessing support for complex difficulties that are not easily labelled. Similar to other educational contexts where individuals who do not present stereotypically, access to support in these instances is often delayed or inadvertently overlooked altogether [Citation31–33].
Whilst classifying challenges across dimensions (personal, professional and social) and identifying relevant interventions for each individual problem is helpful[Citation9], designing and delivering a global support system, and monitoring its effect is probably more important. A multi-disciplinary approach to support is likely to be necessary, where all responsibility does not lie with the GP trainer, but instead, they co-ordinate support, receiving input and feedback from various agencies as required.
The challenges of working in primary care are reported widely [Citation34–36]. The GMC’s 2018 Training Environments Survey identified work-related burnout as prevalent to a high degree among trainees, with well over half feeling worn out at the end of the working day[Citation37]. Whilst a lot of attention has gone to those established in practice, or towards the end of their career[Citation38], this study suggests initiatives to retain GPs should look at those currently in training[Citation39].
To conclude, our findings highlight a lack of sufficient social and emotional support for trainees in a high-demand profession. Structured early support could improve retention and the development of resilient future GPs.
Ethical approval
Ethical approval for this study was granted by University of Leicester, reference number: 7469-rw205-medical education.
Supplemental Material
Download MS Word (17 KB)Acknowledgments
We would like to thank all of the trainees who participated in this study and the staff of the Professional Support and Wellbeing Unit, HEE-EM for their support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Royal College of General Practitioners. MRCGP exam overview. 2020. [cited 2020 Feb]. Available from: https://www.rcgp.org.uk/training-exams/mrcgp-exam-overview.aspx
- Cleland J, Porteous T, Ejebu O, et al. “Should I stay or should I go?”: a qualitative study of why UK doctors retire. Med Ed. 2020;54:821–831.
- Royal College of General Practitioners. Feedback on the January 2018 MRCGP applied knowledge test (AKT32). 2018. [cited 2020 Mar]. Available from: https://www.rcgp.org.uk/training-exams/mrcgp-exam-overview/-/media/9A7EB3A82D7745E0A1614F61129F5DB8.ashx
- Royal College of General Practitioners. MRCGP statistics 2016–2017: annual report on the results of the AKT and CSA assessments 2017. [cited 2020 Mar]. Available from: https://www.rcgp.org.uk/-/media/Files/GP-training-and-exams/Annual-reports/MRCGP-Statistics-2016-17-annual-report-on-AKT-and-CSA-Assessments.ashx?la=en
- Royal College of General Practitioners. MRCGP clinical skills assessment CSA candidate feedback – revised March 2019. [cited 2020 Mar]. Available from: https://www.rcgp.org.uk/training-exams/mrcgp-exam-overview/-/media/B18B21F1C56C49F3A3C3A99C681A8062.ashx
- Woolf K, Potts HWW, McManus IC. Ethnicity and academic performance in UK trained doctors and medical students: systematic review and meta-analysis. Br Med J. 2011;342:d901.
- Shaw B, Fox J, Brown J, et al. An investigation of factors affecting the outcome of the clinical skills assessment (CSA) in general practice specialty training. Educ Prim Care. 2014;25:91–95.
- Galam E, Komly V, Jund J. Burnout among French GPs in training: a cross-sectional study. Br J Gen Pract. 2013;63(608):217–224.
- Patterson F, Knight A, Stewart F, et al. How best to assist struggling trainees? Developing an evidence-based framework to guide support interventions. Educ Prim Care. 2013;24:330–339.
- Jackson D, Davison I, Adams R, et al. A systematic review of supervisory relationships in general practitioner training. Med Ed. 2019;53(9):874–885.
- Kirwan M, Armstrong D. Investigation of burnout in a sample of British general practitioners. Br J Gen Pract. 1995;45:259–260.
- Charles A Looking to the future: general practice through the eyes of GP trainees. The Kings Fund. 2016. [cited 2020 Mar]. Available from: https://www.kingsfund.org.uk/blog/2016/05/general-practice-gp-trainees
- Sagasser MH, Kramer AWM, van der Vluten CPM. How do postgraduate GP trainees regulate their learning and what helps and hinders them? A qualitative study. BMC Med Educ. 2012 [cited 2020 Mar];12(67). Available from https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-12-67
- McLaren P, Patel A, Trafford P, et al. GP trainers’ experience of managing a trainee in difficulty: a qualitative study. Educ Prim Care. 2013;24:363–371.
- Chambers R, Wall D, Campbell I. Stresses, coping mechanisms and job satisfaction in general practitioner registrars. Br J Gen Pract. 1996;46:343–348.
- Milbank D, Ryall S, Lisman E. Trainees in difficulty or a system in difficulty. BMJ Careers. 2016 [cited 2020 Mar]:i246. Available from: http://careers.bmj.com/careers/advice/Trainees_in_difficulty%E2%80%94or_a_system_in_difficulty%3F
- Linton S. Taking the difference out of attainment. Br Med J. 2020;368:m438.
- Cleland J, Leggett H, Sandars J, et al. The remediation challenge: theoretical and methodological insights from a systematic review. Med Educ. 2013;47(3):242–251.
- Lacasse M, Audétat MC, É B, et al. Interventions for undergraduate and postgraduate medical learners with academic difficulties: a BEME systematic review. BEME Guide no. 56. Med Teach. 2019;41:981–1001.
- Patterson F, Kerrin M, Baron H, et al. Exploring the relationship between general practice selection scores and MRCGP examination performance. Final Report to General Medical Council. 2015. [cited 2020 Mar]. Available from: https://www.gmc-uk.org/-/media/documents/Exploring_the_Relationship_between_Recruitment_Scores_and_MRCGP_Examination_Performance_v5.4.pdf_63533914.pdf
- Woolf K, Cave J, Greenhalgh T, et al. Ethnic stereotypes and the underachievement of UK medical students from ethnic minorities: a qualitative study. Br Med J. 2008;337:a1200.
- Naidoo S, Lopes S, Patterson F, et al. Can colleagues’, patients’ and supervisors’ assessments predict successful completion of postgraduate medical training? Med Ed. 2017;51(4):423–431.
- Patel R, Tarrant C, Bonas S, et al. Medical students’ personal experience of high-stakes failure: case studies using interpretative phenomenological analysis. BMC Med Educ. 2015;15(1):86.
- Braun V, Clarke V. Teaching thematic analysis. Psychologist. 2003;26:120–123.
- Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res. 2001;1(3):385–405.
- Howe A, Smajdor A, Stockl A. Towards an understanding of resilience and its relevance to medical training. Med Ed. 2012;46(4):349–356.
- Crane R, Haig P, Scallan S. Failure to secure a training post in an applicant’s first choice deanery: a significant risk factor for difficulties during training. Educ Prim Care. 2013;24:372–373.
- Baron T, Grossman RI, Abramson SB, et al. Signatures of medical student applicants and academic success. Plos One. 2020 [cited 2020 Apr];15:e0227108.
- Shrewsbury D. Dyslexia in general practice education: considerations for recognition and support. Educ Prim Care. 2016;27(4):267–270.
- Asghar ZB, Siriwardena AN, Elfes C, et al. Performance of candidates disclosing dyslexia with other candidates in a UK medical licensing examination: cross-sectional study. Postgrad Med J. 2018;94(1110):198–203.
- Henderson P. Are there delays in reporting dyslexia in university learners? Experiences of university learning support staff. J Furth and High Educ. 2017;41(1):30–43.
- Mowlem F, Agnew-Blais J, Taylor E, et al. Do different factors influence whether girls versus boys meet ADHD diagnostic criteria? Sex differences among children with high ADHD symptoms. Psychiatry Res. 2019;272:765–773.
- Murray AL, Booth T, Eisner M, et al. Sex differences in ADHD trajectories across childhood and adolescence. Dev Sci. 2019;22(1):e12721.
- Hall LH, Johnson J, Watt I, et al. Association of GP wellbeing and burnout with patient safety in UK primary care: a cross-sectional survey. Br J Gen Prac. 2019;69(684):e507–514.
- Thompson M, Walter F. Increases in general practice workload in England. Lancet. 2016;387(10035):2270–2272.
- Hobbs R, Bankhead D, Mukhtar T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet. 2016 [cited 2020 Mar]. Available from: www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)00620-6/fulltext
- General Medical Council. Training environments 2018: key findings from the national training surveys. 2018. [cited 2020 Apr]. Available from: https://www.gmc-uk.org/-/media/documents/training-environments-2018_pdf-76667101.pdf
- Smith F, Lachish S, Goldacre MJ, et al. Factors influencing the decisions of senior UK doctors to retire or remain in medicine: national surveys of the UK-trained medical graduates of 1974 and 1977. BMJ Open. 2017;7(9):e017650.
- Verma P, Ford JA, Stuart A, et al. A systematic review of strategies to recruit and retain primary care doctors. BMC Health Serv Res. 2016;16(1):126.