ABSTRACT
Background
Previous research has found a relationship between students’ gender and attitudes surrounding peer physical examination, but relationship between patient gender and confidence/comfort is less clear. We explored whether patient gender affects medical students’ levels of confidence and comfort in clinical examination skills.
Methods
An electronic survey and focus groups were conducted with medical students from one UK institution. Students reported levels of confidence/comfort when carrying out clinical examinations on men/women. An inductive thematic analysis was performed.
Results
Of a total of 1500 students provided with the opportunity to participate, ninety (6%) responded. For cardiovascular and respiratory examinations, confidence/comfort were higher when examining male-presenting patients. The opposite was true for mental state examinations. Barriers to confidence/comfort included perceiving males as a norm, difficulty navigating breasts, tutors’ internalised gendered attitudes and a wider sociocultural issue. Facilitators of confidence/comfort included students relating to patients, embodying a professional role, gender blindness, and authentic clinical environments. Fewer than 20% (n = 18) of students felt they had enough opportunity to practice clinical skills on women, versus 90% (n = 82) on men.
Conclusion
Our study identified an area where students’ confidence and comfort in clinical examinations could be enhanced within medical education. Changes were implemented in the institution under study’s vocational skills teaching, which is rooted in general practice. Information on gender and clinical skills was provided within course handbooks, time was scheduled to discuss gender and clinical skills in small group settings, and equitable gender representation was ensured in clinical assessment.
Introduction
Gender bias costs lives: in the last decade, deaths of more than 8200 women in England and Wales could have been prevented had they received the same standard of care as men, equating to two preventable gender gap-related deaths daily [Citation1]. In healthcare, gender bias is attributable to both gender blindness [Citation2], the false assumption of women’s and men’s health situations being the same where there are differences, and the converse, the assumption of differences where there are none [Citation3].
Gender bias’s implications on patient care [Citation2,Citation3] are multifaceted. Gender-stereotyping may result in doctors attributing coronary heart disease symptoms to psychological causes in women, increasing mortality [Citation4]. Gendered communication styles lead to a reduced awareness of mental health pathology in men [Citation4]. Gendered social expectations see the normalisation of menstrual pain resulting in an endometriosis diagnosis taking an average of 7 years [Citation5]. Medical education, too, can be androcentric [Citation4,Citation6,Citation7] – resources, including textbooks and CPR dummies [Citation8,Citation9] centre on the male body. Although progress has been made regarding the participation of women in clinical trials [Citation10] and the Scottish Government ‘Women’s Health Plan’ [Citation11] and England’s ‘Women’s Health Strategy’ [Citation12] aim to combat biases, inequalities remain; men still overrepresented in trials [Citation13,Citation14] and research into how sex and gender bias may be reduced is lacking [Citation15].
Gender bias in healthcare, whether implicit or explicit, is perpetuated by healthcare professionals. The education and training that they receive, thus, may be paramount in combating gender bias, for, when doctors are gender aware, they can contribute to equity and equality [Citation4]. Gender equality is the absence of discrimination based on gender, whilst gender equity is the identification of gender differences and rectification of gender imbalance [Citation16].
The importance of medical education is emphasised by the UK government’s pledge for women’s health-specific assessments to become mandatory in medical training, as part of its first women’s health strategy for England [Citation12]. The strategy also commits to commission research by the National Institute for Health and Care Research (NIHR) on women’s health and establishes a new policy research unit on reproductive health [Citation12]. The strategy lends a specific focus to primary care and general practice – pledging to expand general practice capacity, establish women’s health hubs, piloted in one primary care network and commissioning research into healthcare professionals’ perspectives of listening to women in primary care [Citation12]. In medical education, primary health care too has been highlighted as a discipline of specific suitability to communicate the importance of gender issues to students, due to its multidisciplinary character [Citation17].
A scoping review on interventions to reduce gender disparities in clinical care found only 22 studies, of which only two were based in primary care [Citation15]. Primary care, however, may provide a unique opportunity for educational interventions which address gender disparities in the curriculum. Indeed, at the institution under study, all early years’ clinical skills and all communication skills are general practice. Furthermore, previous research also advocates that general practice may have an integral role in promoting professionalism [Citation18], which is closely intertwined with issues concerning gender equity [Citation19]. Additionally, many of the health impacts of gender bias are often first encountered in primary care, including, but not limited to, domestic violence, reproductive healthcare services and cardiovascular health [Citation15].
Whilst there has been considerable research regarding gender discrimination within medicine [Citation20–27], there has been less research examining the impact of patient gender on medical student comfort and confidence when practising clinical skills. Given this, we asked: ‘Does patient gender affect medical students’ levels of confidence and comfort in undertaking clinical examination skills, and, if so, why?’.
outlines key terminology in this study and emphasises the limitation in only identifying gender as perceived gender-presentation of individuals as male and female, thereby limiting applicability of the work.
Table 1. Definitions of terms used in this study.
Methods
Research approach
A mixed methods study design was used, consisting of an anonymous online questionnaire and focus groups. A multi-paradigmatic approach was adopted – quantitative aspects were interpreted using a post-positivist approach and qualitative aspects using a socio-constructivist ontology and interpretivist epistemology. We understand gender as a concept for which individuals possess personal mental constructs influenced by subjective social experiences [Citation28,Citation29].
Study context and study population
All medical students at one UK institution were eligible for inclusion. The institution has a 5-year integrated syllabus with the option to undertake an intercalated degree after year 3.
Sample selection and recruitment
Students were invited to participate through the institution’s digital learning environment. Links were provided to a questionnaire, and contact details given if students wished to be part of a focus group. Participation was non-incentivised and voluntary.
Surveys were sent out once to students via Moodle, the institution’s online learning environment and via year group social media pages. This study was done as a part of a student selected component, with only 1 week for data collection, and all survey responses dated between 28/01/2020 and 3/02/2020, which was a major limitation to recruitment attempts.
Ethical considerations
Ethical approval was granted by the institution’s Ethics Committee (approval number: 200,190,082). Written informed consent was obtained from participants.
Data collection
The questionnaire consisted of quantitative Likert scales and qualitative open text items. Questions were constructed with reference to issues highlighted by existing literature and teaching staff, in line with guidelines for developing questionnaires for educational research [Citation30]. Face validity was assessed by independent faculty. No formal reliability analysis was conducted.
Examinations included in the questionnaire were those that are taught as a part of a peer-based examination in the institution under study – cardiology, respiratory, gastrointestinal, neck, neurology, ENT, back MSK, upper limb MSK, lower limb exams and mental health history. Those that are taught on models as opposed to peers, such as the genitourinary exam, were excluded from this research.
Students were also asked how much the following factors influence their confidence examining patients – age, religion, ethnicity, weight, sexuality and whether they are transgender.
Additional qualitative data to explore students’ perspectives were gathered through two semi-structured hour-long focus groups, each composed of five students. Focus group question stems (Supplementary Materials I) were drawn with reference to existing literature [Citation31,Citation32] and issues highlighted by teaching staff. Focus groups were conducted by two medical students not otherwise involved in the study – it was hoped that, as fellow medical students, they would be viewed as insiders in relation to the study topic by participants, facilitating richer responses. Recordings were transcribed verbatim by the research team and anonymised. Focus group and survey data were analysed separately, then triangulated.
Data analysis
Quantitative Likert scale data were analysed using descriptive statistics in Microsoft Excel.
Qualitatively, separate inductive thematic analyses were performed on textual survey responses and focus group transcripts using Braun and Clarke’s framework [Citation33] to identify themes relating to students’ experiences of gender regarding clinical examinations. The authors familiarised themselves with data and generated initial descriptive codes through manual coding (MP and MB), leading to the creation of a codebook, which was used to recode all data (MP and MB). Codes were abstracted to themes (MP, MB and CH), data were triangulated and presented narratively as a whole (all authors).
Theoretical framework
Theoretical framework Sensitising concepts that informed data analysis are the facets of gender bias in medicine described by Verdonk et al – gender blindness, androcentrism and gender role ideology (4) (). These sensitising concepts were applied as lenses to the thematic analysis to deepen understanding of data [Citation37]. This approach has been described by Varpio et al. as a theory-informing inductive data analysis[Citation38].
Table 2. Verdonk’s facets of gender bias [Citation4].
Reflexivity
Researchers kept reflexive journals to explore implicit assumptions and internalised beliefs that influenced interpretation [Citation39]. As a medical student, MP is a member of the community under study. The rest of the research team consists of educational researchers (MB), medical school academics (CH) and clinical academics (LC, LH). CH, LC and LP have teaching roles in the medical school under study. To minimise potential issues with insider research, member-checking was carried out with focus group participants to ensure agreement with the representation of views within the study’s results – no new points or disagreements were raised.
Results
Study demographics
A total of 1500 students were provided with the opportunity to participate. Ninety students (6%) responded. Ten students took part in two focus groups (five students per group) (). Participants were predominantly female, which is representative of the gender ratio of medical students within the institution under study (60% F: 40% M).
Table 3. Participant demographics.
Survey Likert scale responses
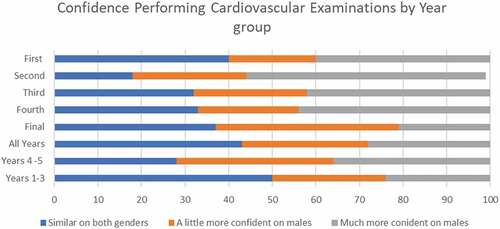
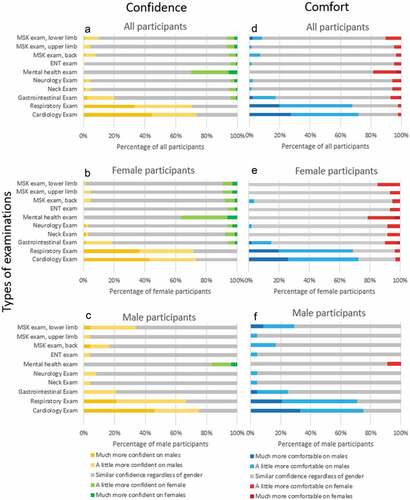
Certain examinations showed gender variations (). The greatest differences were within respiratory and cardiology examinations, where participants felt more confident and comfortable on male-presenting patients. Indeed, not a single participant felt more confident on women for these examinations (yellow and blue bars, ). The converse was observed for the mental state examination, the only examination where male students reported being more confident examining women than men. Similar trends were seen regardless of the participants’ own genders in cardiorespiratory examinations, unlike previous literature which suggests that female students are more likely to correctly perform cardiovascular examinations on women [Citation40]. However, it is important to note that this study measured perceived ability (i.e. self-confidence), which does not necessarily correlate with actual performance.
Figure 1. Online survey answers to the questions ‘How confident do you feel in carrying out:’ (a-c) and ‘How comfortable do you feel in carrying out:’ (d-f). Participant answers are presented for all participants (a and d), female participants (b and e), and male participants (c and f). There were not sufficient participants of non-binary genders to allow production of charts for non-binary participants.
Only 8% (n = 5) of participants in years 1–3 felt that they had had enough opportunity to practice all clinical examinations on women, whereas 87% (n = 53) felt they had had enough opportunity to practice clinical examinations on men. This may indicate that perceived opportunity to practice may be linked to the reduced confidence and comfort felt by students when examining female patients. Fisher’s exact test gave a P-value of 0.0000000000004148.
Including data from year 4 and 5 participants, who are ward-based and have the opportunity to practice on patients of all demographics, the figures rose to 19% (n = 17) and 90% (n = 80) for examining women versus examining men, respectively. This suggests that students may not be comfortable to take advantage of these learning opportunities, perhaps due to earlier male-centric teaching. Fisher’s Exact Test gave a P-value of 0.0000000000000951.
Perceived confidence was highest in year 1, dropped in year 2, then rose over the next 4 years (), but the proportion of people more confident on males was still higher in year 5 than year 1.
Qualitative questionnaire and focus group data
Thirty-four descriptive open codes were identified after triangulating qualitative survey and focus group responses. Thematic sufficiency, Page 3 of 3 ‘the stage at which categories appear to manage new data without requiring further modifications’ [Citation40], was achieved after 90 survey responses and two focus groups involving 10 participants. Two major themes and nine categories were identified ().
Table 4. Major themes, categories and corresponding codes obtained from inductive qualitative analysis of open-text responses in the electronic questionnaire and two focus groups.
Theme 1: Barriers to developing equal confidence and comfort in carrying out examinations in male and female patients
(a) Males as standard:
Participants felt they had more opportunities to practice on males and that resources favoured males as a normative standard.
I think when it comes to respiratory and cardio exams we are often taught with male patients and models. Anatomy textbooks have a tendency to use male bodies as the standard which also makes this hard. (P41, F, Y5)
Students vocalised a need for more teaching on women. Given a lack of focus within teaching, formative and summative examinations were sometimes the first-time students were required to examine a female patient.
In my very first station for the mock OSCE … it was CV exam and it was a woman and they’d never even discussed how to approach it so I just assumed they would just give you a male patient because they just teach them. They didn’t. And I kind of freaked out … (P4, F, Y3)
(b) Difficulty navigating breasts:
Proposed reasons for medical students’ differing confidence and comfort levels often involve variations in anatomy, with teaching not providing clear guidance on how to vary techniques based on differences.
I wouldn’t know what to do with the breasts! (P24, F, Y2)
It’s all males we learn with so it’s difficult to know how to manage and where to position. (P3, F, Y2)
Some participants juxtaposed the professional responsibilities of a doctor with the limited clinical skills teaching received regarding examining women.
Despite the fact that we are expected to deal with the female body of patients in a professional behaviour as doctors it is perceived that we will not be able to do this with our peers as medical students. (P65, M, Y2)
Participants desired clear, practical advice regarding the examination of women.
Frank explanation by a doctor telling you how to handle it (I was told to ask the woman to move her breast out the road for you and it has helped a great deal). (P68,F, Y5)
(c) Tutors’ internalised gendered attitudes
Participants vocalised how tutors’ behaviours reinforced the narrative that males were a normative standard.
[In clinical skills] it is always the males that are encouraged to volunteer. I have had … tutors in the past be a bit skittish about using females, which doesn’t help us and it can be detrimental to female health. (P8, F, Y2)
I know many females who wouldn’t have minded being the patient but often find it is the tutors too awkward to ask the girls. (P49, F, Y3)
Participants wanted staff to be trained regarding any biases they may have.
… giving training to all staff who teach clinical skills … on how to approach this subject correctly, not using language that assumes that women/females will not want to be simulated patients or even encouraging them to do so (without pressuring them). (P65, M, Y2)
(e) A wider socio-cultural issue
Many students referenced experiences outside of medical school as influencing their comfort and confidence.
Social norm suggests it is more acceptable for a male to be topless therefore when practising we always practise on male colleagues. (P80, F, Y3)
Some students also made stereotyped generalisations about the nature of patients, for example:
… female patients are typically more co-operative, and this makes it easier. (P16, M, Y2)
(f) Intersections of identities
Some patients’ characteristics, across both genders, amplified student discomfort. Students felt less confident examining overweight patients and more confident on underweight patients.
Overweight patients are challenging to examine regardless of gender. (P25, F, Y5)
For an underweight person it will be easier to feel things on their body (P64, F, Y3)
Students preferred patients who were not of a similar age to them, as distance in age was felt to facilitate professional practice.
… examin[ing] a patient at my same age or a bit younger I feel uncomfortable as I could feel attracted by him. (P29, F, Y3)
Religion and ethnicity also influenced comfort and confidence. Some students felt less confident examining patients of ethnicities different to their own.
[I am] worried about being insensitive if e.g. a woman wears religious garments such as hijab. (P31, F, Y5)
Ethnicity plays a role [in confidence and comfort] because I am used to see[ing] white people. (P29, F, Y3)
LGBTQIA+ patients were also identified as an area of lesser confidence, due to perceived gaps in teaching.
We have been taught next to nothing on transgender medicine. (P75, F, Y3)
Theme 2: Facilitators of developing equal confidence and comfort in carrying out examinations in male and female patients
(a) Relating to patients
Students felt more confident examining patients of the same gender although treating men as the norm within clinical skills meant some female medical students also felt more at ease examining men.
As a female I find it easier to connect with another female, however, in [the] case of respiratory and cardiac exam males are easier to examine as we were made to practice on males. (P18, F,Y2)
(b) Role as a professional
Participants dissociated themselves from discomfort by emphasising their professional role as a future doctor.
I remind myself I should be as professional as possible so I shouldn’t feel uncomfortable. (P29, F, Y3)
(c) Gender blindness
Some students attributed their comfort in examining all genders to ‘not seeing’ gender within clinical skills.
Gender does not matter in an examination. (P35, F, Y5)
(d) Authentic clinical environments
Students noted that differences were alleviated by the placement environment, which offered a more authentic way to practice.
When initially being taught particular examinations especially respiratory and cardio[vascular] examinations, we would always practise on male students. I have gained confidence in examining women since then on hospital placements. (P5, F, Y5)
Discussion
Our data suggest that patient gender can impact medical students’ levels of confidence and comfort. The described barriers and facilitating factors to equal comfort and confidence in examination skills may provide guidance for educators contemplating how gender disparities within examination skills may be addressed.
Students surveyed perceived clinical skills instruction as androcentric, centring upon the male body. The portrayal of men as the norm has been previously noted within medical textbooks, which frequently underrepresent women in all areas bar those with sex-specific content and promote traditional gender stereotypes [Citation41]. This study adds to these findings by moving beyond textbooks to considering the bodies students practice on, demonstrating how students may internalise what is presented to them within teaching sessions as the ‘norm’. This suggests that there is scope for demonstrating examination skills on willing female students as, in doing so, examinations on women may become more ‘normalised’ for students. Students’ desire for learning how to handle sex-specific differences in anatomy is supported by previous research, which shows that emphasis on sex-specific examination manoeuvres, such as lifting the left breast to facilitate mitral valve auscultation, may begin to address gender bias [Citation42].
Students perceived tutors as reinforcing stereotypes related to gender. In this way, gender attitudes can become part of the ‘hidden curriculum’ within medical education – the ‘set of influences that function at the level of organisational structure and culture’ [Citation43], which represent unintended learning experiences [Citation43]. This reported gender bias may be a form of benevolent sexism [Citation20], which, although well intentioned, propagates stereotypes [Citation44]. Achieving gender-sensitivity within medical education must, therefore, address both implicit bias within curricula, e.g. through adaptation of content, language and representation of women in education resources [Citation20], and the implicit biases held by educators, e.g. through implicit bias education programmes [Citation45] and systemic action [Citation46]. Importantly, just as the barriers to gender equity are intersectional [Citation47], approaches to addressing biases should be intersectional, as evidenced by participants also emphasising weight, gender identity and ethnicity/religious attire.
All placements and teaching described by the early years students in this study are part of the clinical skills and vocational studies teaching, which is GP-led at our institution. This emphasises how teaching-interventions may also be suitably placed in primary care. Since data collection took place for this study, GP teaching in the later years has increased for all students, and a special GP track has been developed in parallel. Further research is required to investigate the impact of the changes made to GP teaching at our institution in response to this study, in both preclinical and clinical phases.
Gender blindness was apparent in several students’ accounts, who related disregarding gender to achieving greater comfort and confidence in examination skills. Although well intentioned, Risberg et al.’s theoretical model illustrates that gender-blindness prevents gender equity in medicine, which requires that doctors recognise differences in experience and biology when they exist [Citation4,Citation48]. Students perceiving ‘gender blindness’ as a promoter of gender equity rather than as a contributor to gender inequity show a need for education regarding gender within medical institutions. Risberg et al.’s model recommends reflections on gender-based attitudes alongside ‘consciousness-raising activities’ to combat gender-blindness [Citation48].
Limitations
The low response rate of 6% may limit the validity and generalisability of the results. Despite significant P-values when performing Fisher’s test, given the small sample size, confidence intervals should be interpreted with caution. The study was timebound utilising only the original data set for analysis. Although thematic sufficiency was achieved, it is important to acknowledge that further research may reveal new themes. In particular, the focus groups consisted of early years students, reflecting the concurrent exam period for later years. Survey data, however, showed that later years also showed a gap in confidence and comfort (). Further research ought to ensure all years are reflected in focus groups. Further research is required to determine if the confidence and comfort gap identified in later years by the survey is perpetuated by similar or emerging themes. The complex issues of ‘how many qualitative interviews are enough?’ is explored by Baker [2012, Citation49] with the conclusion being that ‘it depends’ and that practical issues can be legitimate factors in deciding, including the amount of time available. The qualitative data offers richness and, according to Charmaz (2014), ‘reveals participants’ views, feelings, intentions and actions as well as the contexts and structures of their lives’ [Citation50]. Morse (1995) emphasised the importance of data richness and variation over quantity which can lead to the development of a plausible and convincing theory [Citation51].
Participants were from a single institution, which may limit transferability. There may be a selection bias in the demography of our sample, given the over-representation of women; however, this is a recognised phenomenon [Citation52], and we sampled a breadth of student experience from all years. Furthermore, triangulation of data deepened the analysis and is likely to have enhanced transferability.
Although well aligned with the study’s research question, this study only investigated student perceptions of confidence and comfort in carrying out examinations – how this translates to practice is a necessary direction for future research. Other areas for future research may concern specific examinations which show differences in confidence or comfort but do not feature prominently within our results, such as mental state examinations. Furthermore, additional examinations such as the genitourinary exam could be included, as well as histories as well as examinations. Multi-institutional research, and evaluation of gender equity changes implemented by institutions, would also be worthwhile.
A major limitation is that this study only identifies gender as the perceived gender-presentation of individuals as male and female, which limits the applicability of this work. Given that gender is not a binary issue, a further area of study is transgender identities and to include comfort and confidence working with non-binary and transgender patients. Although students were asked about the areas of intersection in this study – age, religion, ethnicity, weight, sexuality and whether they are transgender – these topics warrant exploration in their own right, rather than solely as secondary questions.
Recommendations to promote gender equity
Previous research has emphasised a need to clarify how gender issues may be integrated into the curriculum [Citation4] – our research suggests examination skills training as a key domain in which gender can be explicitly discussed and that vocational skills, or equivalent GP-based teaching, may be a relevant part of the curriculum to implement such changes. We offer the following practical proposals to promote gender equity (), drawn from changes established at the institution at which this research was conducted.
Table 5. Practical proposals to promote gender equity.
Conclusion
This study set out to investigate whether the gender of an individual to be examined influences medical students’ levels of confidence and comfort when carrying out various types of examinations and, if so, why this was the case.
Recommendations for change include the need for additional information on gender and clinical skills and the promotion of resources which feature all genders. Differences in gender, and gender biases, must be explicitly acknowledged and discussed throughout medical school curricula as the ability of medical students to understand clinical presentations in all genders is essential to ensuring that the doctors of tomorrow are adequately prepared for clinical practice. Although clinical ability is not in direct question, addressing confidence and comfort is a learner-centric response and these recommendations may help medical schools meet their dual obligations to patients and learners. This aligns with the Scottish Government’s Women’s Health Plan long-term aim to improve awareness and education among healthcare professionals of sex-related differences in presentation and management of heart disease in women of all ages [Citation11] and changes such as ensuring gender-representation in OSCEs align with England’s Women’s Health Strategy’s aim that women’s health-specific assessments are to become mandatory in medical training [Citation53].
In making such changes, medical education can begin to move away from the androcentric status quo that has negatively impacted patient outcomes for generations.
Supplemental Material
Download MS Word (13.8 KB)Acknowledgments
We would like to acknowledge Professor Susan Jamieson and Professor Matthew Walters for their comments during the write up process; Dr Zoe Noonan for ensuring that OSCEs were gender aware; Dr Sharon Sneddon for her support in developing the survey; Rebecca Galloway and Laura McCafferty for facilitating the focus groups; Isobel Walker for her illustrations (although these were not used in the final manuscript, we want to recognise her expertise and time) and to all survey and focus group participants.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/14739879.2022.2129460
Additional information
Funding
References
- Foundation BH. Bias and biology: how the gender gap in heart disease is costing women’s lives. 2019.
- Hamberg K. Gender bias in medicine. Women’s Health. 2008;4(3):237–243.
- Ruiz MT, Verbrugge LM. A two way view of gender bias in medicine. J Epidemiol Community Health. 1997;51(2):106–109.
- Verdonk P, Benschop YW, de Haes HC, et al. From gender bias to gender awareness in medical education. Adv Health Sci Educ Theory Pract. 2009;14(1):135–152.
- Excellence Nifha C. Endometriosis: diagnosis and management. 2017.
- Gishen F, Lokugamage A. Diversifying the medical curriculum. BMJ. 2019;364:l300.
- Burrage H. Health education: the androcentric agenda. Journal of the Institute of Health Education. 1986;24(3):106–111
- Mendelsohn KD, Nieman LZ, Isaacs K, et al. Sex and gender bias in anatomy and physical diagnosis text illustrations. JAMA. 1994;272(16):1267–1270.
- Parker RB, Larkin T, Cockburn J. Gender bias in medical images affects students’ implicit but not explicit gender attitudes. AERA Open. 2018;4(3):2332858418798832
- Bushnell C, McCullough LD, Awad IA, et al. Guidelines for the prevention of stroke in women. Stroke. 2014;45(5):1545–1588.
- Minister for Public Health WsHaS. Women’s health plan A plan for 2021-2024. Edinburgh: Scottish Government; 2021.
- Care DoHaS. Women’s health strategy for England. 2022.
- Feldman S, Ammar W, Lo K, et al. Quantifying sex bias in clinical studies at scale with automated data extraction. JAMA Network Open. 2019;2(7):e196700–e.
- Maas AHEM, van der Schouw YT, Regitz-Zagrosek V, et al. Red alert for women’s heart: the urgent need for more research and knowledge on cardiovascular disease in women: proceedings of the workshop held in Brussels on gender differences in cardiovascular disease, 29 September 2010. Eur Heart J. 2011;32(11):1362–1368.
- Berner AM, Lund J, Saunders CL. Tackling the complexity of gender bias in primary care. Br J Gen Pract. 2021;71(708):296–297.
- WHOROf E. Gender: definitions 2020 [ Available from]: http://www.euro.who.int/en/health-topics/health-determinants/gender/gender-definitions.
- Weisman CS, Rich DE, Rogers J, et al. Gender and patient satisfaction with primary care: tuning in to women in quality measurement. J Womens Health Gend Based Med. 2000;9(6):657–665.
- Johnston JL, Cupples ME, McGlade KJ, et al. Medical students’ attitudes to professionalism: an opportunity for the GP tutor? Educ Primary Care. 2011;22(5):321–327.
- Shaw MK, Chandratilake M, Ho M-J, et al. Female victims and female perpetrators: medical students’ narratives of gender dynamics and professionalism dilemmas. Adv Health Sci Educ. 2020;25(2):299–319.
- Cheng L-F, Yang H-C. Learning about gender on campus: an analysis of the hidden curriculum for medical students. Med Educ. 2015;49(3):321–331.
- Samuriwo R, Patel Y, Webb K, et al. ‘Man up’: medical students’ perceptions of gender and learning in clinical practice: a qualitative study. Med Educ. 2020;54(2):150–161.
- Oancia B, Carry C, Johnson C. The influence of gender and specialty on reporting of abusive and discriminatory behaviour by medical students, residents and physician teachers. Med Educ. 2000;34(4):250–256.
- Han H, Kim Y, Kim S, et al. Looking into the labyrinth of gender inequality: women physicians in academic medicine. Med Educ. 2018;52(10):1083–1095.
- Babaria P, Bernheim S, Nunez-Smith M. Gender and the pre-clinical experiences of female medical students: a taxonomy. Med Educ. 2011;45(3):249–260.
- Broad J, Matheson M, Verrall F, et al. Discrimination, harassment and non-reporting in UK medical education. Med Educ. 2018;52(4):414–426.
- Jendretzky K, Boll L, Steffens S, et al. Medical students’ experiences with sexual discrimination and perceptions of equal opportunity: a pilot study in Germany. BMC Med Educ. 2020;20(1):56.
- Wiskin CMD, Allan TF, Skelton JR. Gender as a variable in the assessment of final year degree-level communication skills. Med Educ. 2004;38(2):129–137.
- Crotty M. The foundations of social research: meaning and perspective in the research process. London: SAGE Publications Ltd; 1998.
- Denzin NK, Lincoln YS. The sage handbook of qualitative research. 5th ed. California: SAGE Publications; 2017.
- Artino AR, La Rochelle JS, Dezee KJ, et al. Developing questionnaires for educational research: AMEE Guide No. 87. Med Teach. 2014;36(6):463–474.
- Vnuk AK, Wearn A, Rees CE. The influence of students’ gender on equity in peer physical examination: a qualitative study. Adv Health Sci Educ. 2017;22(3):653–665.
- Dabson AM, Magin PJ, Heading G, et al. Medical students’ experiences learning intimate physical examination skills: a qualitative study. BMC Med Educ. 2014;14(1):39.
- Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE Guide No. 131. Med Teach. 2020;42(8):846–854.
- Tsouroufli M, Rees CE, Monrouxe LV, et al. Gender, identities and intersectionality in medical education research. Med Educ. 2011;45(3):213–216.
- Dictionary OE. Gender, n. 2020 [ Available from]: https://www.oed.com/viewdictionaryentry/Entry/77468
- Dictionary OE. Sex, n. 2020 [ Available from]: https://www.oed.com/viewdictionaryentry/Entry/176989.
- Bowen GA. Grounded theory and sensitizing concepts. Int J Qual Methods. 2006;5(3):12–23.
- Varpio L, Paradis E, Uijtdehaage S, et al. The distinctions between theory, theoretical framework, and conceptual framework. Acad Med. 2020;95(7):989–994.
- May TP B. Reflexivity and the practice of qualitative research. In: Flick U, editor. The SAGE handbook of qualitative data analysis. London: SAGE Publications Ltd; 2014. p.108–122.
- Varpio L, Ajjawi R, Monrouxe LV, et al. Shedding the cobra effect: problematising thematic emergence, triangulation, saturation and member checking. Med Educ. 2017;51(1):40–50.
- Parker R, Larkin T, Cockburn J. A visual analysis of gender bias in contemporary anatomy textbooks. Soc sci med. 2017;180:106–113.
- Chakkalakal RJ, Higgins SM, Bernstein LB, et al. Does patient gender impact resident physicians’ approach to the cardiac exam? J Gen Intern Med. 2013;28(4):561–566.
- Brown MEL, Hafferty FW, Finn GM. The hidden curriculum and its marginalisation of longitudinal integrated clerkships. Educ Primary Care. 2020;31(6):337–340.
- Glick P, Fiske ST. The ambivalent sexism inventory: differentiating hostile and benevolent sexism. J Pers Soc Psychol. 1996;70(3):491–512.
- Sukhera J, Watling C. A framework for integrating implicit bias recognition into health professions education. Acad Med. 2018;93(1):35–40.
- Fallin-Bennett K. Implicit bias against sexual minorities in medicine: cycles of professional influence and the role of the hidden curriculum. Acad Med. 2015;90(5):549–552.
- Brown MEL, Hunt GEG, Hughes F, et al. ‘Too male, too pale, too stale’: a qualitative exploration of student experiences of gender bias within medical education. BMJ Open. 2020;10(8):e039092.
- Risberg G, Johansson EE, Hamberg K. A theoretical model for analysing gender bias in medicine. Int J Equity Health. 2009;8(1):28.
- Baker S, Edwards R. How many qualitative interviews is enough. 2012.
- Charmaz K. Grounded theory in global perspective: reviews by international researchers. Qual Inq. 2014;20(9):1074–1084.
- Morse JM. The significance of saturation. Qual Health Res. 1995;5(2):147–149.
- Smith G. Does gender influence online survey participation?: a record-linkage analysis of university faculty online survey response behaviour’. San Jose, California: San Jose State University SJSU ScholarWorks Faculty Publications; 2008. ERIC Document Reproduction Service No ED 501717
- Wise J. Women’s health: specific assessments to become mandatory in medical training. BMJ. 2022;378:o1820.