ABSTRACT
Introduction: Influenza and pneumococcal vaccines are the most regularly prescribed vaccines amongst adults <65 years of age. Pertussis booster vaccines (available as combined diphtheria-tetanus-acellular pertussis, Tdap) uptake is relatively low in many countries in the Asia-Pacific region. Increasing Tdap vaccination is a strategy that may aid healthy aging.
Areas Covered: Epidemiology data, including notification reports from 6 advanced economies in Asia (Australia, Hong Kong, New Zealand, Singapore, South Korea, and Taiwan) were reviewed to assess the pertussis disease burden and identify high-risk groups. Existing Tdap vaccination recommendations were reviewed. Current vaccination practices were discussed to benchmark and identify barriers and success factors for Tdap booster vaccination in older adults.
Expert Opinion: The available evidence supports Tdap vaccination at an individual level for the prevention of pertussis, along with tetanus and diphtheria in those aged 65+ years, together with influenza and pneumococcal vaccination. Data gaps need to be filled to support the development of national/supranational recommendations for pertussis booster vaccination. Groups at higher risk of pertussis infection and its complications, including those with chronic obstructive pulmonary disease and asthma, could be considered as priority groups. Increasing disease awareness and establishing adult vaccination registries could improve vaccine coverage and promote healthy aging.
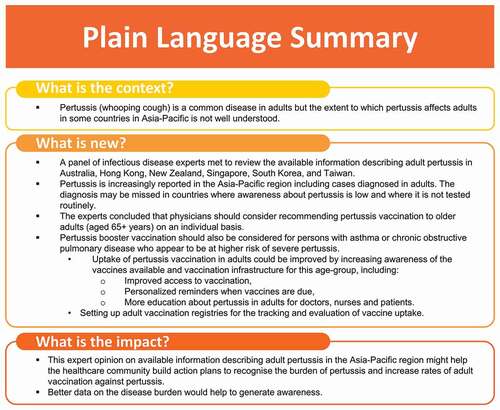
PLAIN LANGUAGE SUMMARY
Pertussis, also called whooping cough, is a common disease in adults. However, how it affects adults in some countries in the Asia-Pacific region is not well understood. In 2019, a panel of experts met to review the available information on adult cases of pertussis in Australia, Hong Kong, New Zealand, Singapore, South Korea, and Taiwan. Here, we present the outcomes of the meeting. Pertussis is increasingly reported in the Asia-Pacific region, including cases diagnosed in adults. The diagnosis may be missed in countries where awareness is still low and/or it is not tested routinely. The experts concluded that physicians should consider recommending pertussis vaccination to older adults (aged 65 or older) on an individual basis, as well as people with asthma or chronic obstructive pulmonary disease, who appear to be at higher risk of severe pertussis. Uptake of pertussis vaccination in adults could be improved by increasing awareness of the vaccines available and vaccination infrastructure for this age-group. Some of the measures proposed were as follows: improved access to vaccination; personalized reminders when vaccines are due; and more education about pertussis in adults for doctors, nursesnurses, and patients. The experts also proposed setting up adult vaccination registries for tracking and evaluation of vaccine uptake. This expert opinion might help the healthcare community build action plans to recognise the burden of the disease and increase rates of vaccination among adults. In addition, better data on the disease burden would help to generate awareness.
© 2021 GlaxoSmithKline Biologicals SA. Published by Informa UK Limited, trading as Taylor & Francis Group.
1. Introduction
As life-expectancy lengthens, the proportion of the global population aged 65+ years is increasing and in 2018, the global population of 65+ year-olds outnumbered the global population of children aged <5 years for the first time [Citation1]. An aging population brings a high cost to healthcare systems as a result of increased susceptibility to infections, chronic degenerative diseases and cancers, as individuals’ age [Citation2]. Enabling life-long well-being has become a key focus for preventative medicine in the 21st century.
Healthy aging is defined by the World Health Organization (WHO) as ‘the process of developing and maintaining the functional ability that enables well-being in older age’ [Citation3], and long term health contributes to improved quality of life and productivity, particularly as the retirement age is extended and a higher proportion of older adults continue to work into later life. Maintaining an adaptive and resilient immune system able to respond to external challenges with appropriate immune responses [Citation4] is crucial to healthy aging. External influences that can positively impact immune fitness include diet, exercise, avoidance of toxins such as smoking, and vaccination [Citation5].
The year 2020 has commenced with the coronavirus disease 2019 (COVID-19) pandemic , which is taking its greatest toll on older adults [Citation6,Citation7]. The current situation illustrates the public health importance of vaccination with clarity. These circumstances may challenge the sense of complacency resulting from the success of vaccines in virtually eliminating some previously disabling or deadly diseases [Citation8].
Preventing infectious disease through vaccination of older adults can have marked benefits in terms of averting acute deterioration in quality of life and reducing hospitalizations and antibiotic use [Citation9]. However, the uptake of vaccines by adult populations is typically low and adult vaccination has rarely, if ever, reached its full potential as a public health intervention [Citation10,Citation11]. Thus, there is an unmet medical need for improved prevention of infectious diseases including pertussis that may impact older adults.
Pertussis (whooping cough) is one of the vaccine-preventable diseases that continues to cause a substantial public health burden in all age-groups. The resurgence in pertussis disease over the last 3 decades coincided with improved disease awareness amongst healthcareprofessionals and the general population, and improved sensitivity of diagnostic tests. Additionally, increased use of acellular pertussis vaccines and waning immunity in older populations are also believed to have contributed to increasing pertussis incidence rates [Citation12,Citation13]. Protection wanes more rapidly following vaccination with acellular pertussis vaccines than after vaccination with whole-cell vaccines and, although effective in preventing disease, it is shown to be less effective in terms of preventing infection and transmission [Citation12,Citation13]. Preventing pertussis in infants too young to be vaccinated, who carry a high disease burden, and in whom pertussis may be fatal, has drawn much attention. Maternal pertussis immunization programs are highly effective in addressing this need [Citation14]. Pertussis, however, remains an under-recognized disease in older adults that can result in hospitalization, rib fractures, incontinence, weight loss, secondary respiratory infection, intra-cerebral hemorrhage, and death [Citation15].
Even though knowledge of the burden of pertussis disease within the Asia-Pacific region is incomplete, understanding the disease burden of pertussis and improving vaccine coverage amongst older adults could provide significant benefits to Asia-Pacific populations in terms of healthy aging.
Here, we review the current recommendations on reduced-antigen-content diphtheria-tetanus-acellular pertussis (Tdap) vaccination and the burden of pertussis amongst older adults using available notification data from 6 countries/regions with advanced economies in the Asia-Pacific, and the high-risk groups that need vaccination. We present the outcomes of an Expert Advisory Panel meeting (held 25 July 2019 in Singapore, sponsored by GlaxoSmithKline Biologicals SA [GSK]) including prioritization of high-risk groups for pertussis vaccination and exploration of barriers and success factors for optimal vaccination coverage. Key conclusions of the Expert Advisory Panel are summarized in .
2. Vaccine preventable disease in older adults
2.1. Burden of vaccine preventable disease and vaccination coverage rates in older adults
Vaccine-preventable infections remain a common cause of morbidity and mortality in older adults. In the United States (US), the number of deaths due to vaccine-preventable diseases in 2009 was 350 times higher in adults than in children [Citation16]. In Australia, the burden of vaccine-preventable diseases in those aged 65+ years increased between 2005 and 2015, primarily due to an increase in cases of influenza and herpes zoster [Citation17]. All deaths due to tetanus over this 10-year period in Australia occurred in persons aged 75+ years. In South Korea, deaths due to infectious diseases decreased over a 32-year period from 1983 to 2015 in all age-groups except 65+ year-olds, in whom the mortality rate per 100,000 population from infectious diseases increased from 135 in 1996 to 307 in 2015 [Citation18].
Vaccines that may be recommended for use in older adults are those targeting pneumococcal disease, influenza, herpes zoster, diphtheria, tetanus, and pertussis.
Influenza vaccines have long been recommended for the 65+ year-old risk group, yet annual vaccine coverage of adults aged 65+ years was 47.6% in Finland, 55.7% in Spain and 72.6% in the United Kingdom in 2017, and 73.5% in the US in 2014–2015 [Citation19,Citation20]. In Asia-Pacific countries, influenza vaccine coverage is similarly varied; 32.7% of 65+ year-old persons with disabilities in Taiwan [Citation21]; 49.1% of 65–74 year-olds in Hong Kong [Citation22]; and 74.6% of 65+ year-olds in Australia [Citation23]. Tdap booster vaccines for adults have been available for several decades, but vaccination rates in adults of all ages remain suboptimal, even in countries with existing recommendations. For example, in Australia, pertussis booster vaccination uptake amongst adults was 11.3% in 2009 and up to 44.2% in the at-risk groups of parents and family members of newborns, childcare, and healthcare workers [Citation23].
2.2. Pertussis in older adults
Mortality due to pertussis in adults aged 60+ years ranks second only to mortality due to pertussis in infants and young children [Citation24,Citation25]. Despite a sizeable disease burden, few studies describe the burden of pertussis disease in older adults [Citation15]. Studies from Australia, the US and Canada published between 2000 and 2006, found that more than 80% of adults with pertussis experienced paroxysmal cough, and that post-tussive vomiting occurred in approximately 50% of all adults, among whom 27% were aged 65+ years [Citation26–28]. In a Canadian study, pneumonia complicated 9% of the pertussis cases detected in adults aged 50+ years and 34% of women aged 50+ years developed urinary incontinence [Citation26]. A more recent review reported that up to 86% of adults and adolescents experience apnea associated with pertussis, up to 33% experience weight loss, and up to 28% experience urinary incontinence [Citation29]. Up to 12% of adults with pertussis require hospitalization [Citation30], and the risk of hospitalization increases significantly with age [Citation31,Citation32]. Compared to 45–54 year-olds with pertussis, the risk of hospitalization increased 5.4-fold in those aged 65–74 years, and 8.9-fold after the age of 75 years [Citation31]. Older persons who were overweight, who had a history of smoking and pre-existing asthma were also at higher risk for pertussis-related hospitalization [Citation31,Citation32]. Among 41 patients aged 65+ years hospitalized with pertussis in the US, 36.6% had pneumonia, 10% required intensive care, and 90% had at least 1 underlying comorbidity, including asthma (27% of patients), obesity (39%), diabetes (32%), or a cardiac condition (29%). One patient died [Citation25]. When deaths due to pertussis occurred in older adults, intracranial hemorrhage was frequently implicated [Citation33,Citation34].
Pre-existing asthma and chronic obstructive pulmonary disease (COPD) appear to be risk factors for pertussis in all age-groups. Two studies from the US, including a case-control study conducted during a pertussis outbreak in California between 2004 and 2005 and a claims database cohort study, found that asthma was associated with an approximately 1.8 to 3.9- fold increased risk of pertussis [Citation35,Citation36]. The risk of pertussis disease in individuals with COPD was 2.5-fold higher than matched controls without asthma or COPD [Citation36]. A review of the literature found that pertussis symptoms were more severe and hospitalization rates higher in individuals with COPD, asthma, obesity, or immunodeficiency, and in smokers [Citation37]. A study of 26 patients with acute COPD exacerbations in Switzerland found serological evidence of Bordetella pertussis or B. parapertussis infection in 8 patients (31%), suggesting that in this small group, pertussis was an important trigger of COPD exacerbations [Citation38].
Pertussis disease can therefore have marked negative impacts on quality of life and daily functioning in older persons, potentially exacerbating other underlying conditions such as COPD and asthma. Little is known whether pertussis disease can adversely impact other co-morbidities such as cardiovascular disease or diabetes [Citation26,Citation39], or whether pertussis disease contributes to weight loss and increased frailty in older persons. Older adults can serve as a reservoir of pertussis infection and transmission to other age groups, particularly vulnerable infants too young to be vaccinated [Citation40]. Although acellular pertussis vaccines do not completely prevent infection and transmission, cocooning strategies in which parents and caregivers are vaccinated have been shown to reduce infection in infants [Citation41–44].
Several methods for laboratory diagnosis of pertussis infection are available. The time from the onset of a cough to when the patient presents to a healthcare professional is important in the choice of diagnostic test [Citation45]. Culture has high sensitivity when samples are collected during the first 2−3 weeks of cough when bacteria are still present in the nasopharynx, but has low specificity [Citation45,Citation46]. For coughs of less than 3 weeks duration, real-time polymerase chain reaction (PCR) is more sensitive than culture but less specific [Citation45,Citation46]. Both methods can be problematic in adults, who rarely present to a healthcare professional until a cough has persisted for several weeks [Citation45]. Indirect diagnosis can be done by serology testing to detect anti-pertussis toxin (PT) antibodies in serum after 2−3 weeks of cough, and in-house assays developed by reference centers or commercial kits recommended by the WHO are available [Citation47]. The PT antigen is specific to B. pertussis [Citation45]. Diagnosis is based on the identification of a significant rise in anti-PT antibodies in paired serum samples collected during the early phase of the illness versus 1 month later [Citation47]. In a single serum sample, a recent infection is indicated by a high anti-PT antibody concentration in unvaccinated individuals [Citation47]. However, serology testing cannot distinguish between antibodies resulting from natural infection or from vaccination, and cannot be used in people vaccinated within 1 year before contracting infection [Citation47]. Adoption of serology testing together with real-time PCR as diagnostic options in daily practice would be helpful to accurately determine the true incidence of pertussis in adults.
3. Burden of pertussis disease in Asia-Pacific countries
Pertussis notification data from 2001 onwards from government websites of Australia [Citation48], New Zealand [Citation49], Hong Kong [Citation50], Singapore [Citation51], South Korea [Citation52], and Taiwan [Citation53,Citation54] were extracted and reviewed. Additional published information about pertussis epidemiology was interrogated non-systematically for countries with low pertussis notification rates. The diagnosis of pertussis is confirmed by culture, PCR or serological testing in Australia, New Zealand, and Singapore and by culture or PCR in Hong Kong, Taiwan, and Korea [Citation55–60]. For context, the pertussis vaccination schedules for children and adolescents in each country are shown in .
Table 1. Pertussis vaccination schedules in children and adolescents in 6 countries of the Asia-Pacific region
3.1. Australia
Since 2001, pertussis notifications have followed a characteristic cyclic pattern with peaks occurring approximately every 4 years () [Citation48]. Since 2010, between 12,225 and 38,747 pertussis cases have been notified annually. The highest number of notifications was in children between 5–14 years of age who accounted for 27.2–41.8% of notifications each year. Since 2010, the number of pertussis notifications in adults aged 60+ years in Australia has ranged from 1289 cases in 2018, to approximately 5500 cases each during 2010 and 2011, which were outbreak years. Pertussis in 60+ year-olds accounted for between 10.7% and 19.3% of all pertussis notifications between 2010 and 2018. During the 2008–2011 pertussis outbreak in Australia, the mean annual incidence of pertussis in adults aged 65+ years was 86.0 per 100,000 population, with a peak of 124.8 per 100,000 population [Citation61]. A seroprevalence study on a nationally representative sample of sera collected between 1997 and 1998 found that recent pertussis infection was highest in 5 − 25 years and ≥65 years age groups [Citation62]. Approximately 13% of adults ≥65 years of age had titers of anti-PT antibodies indicative of recent infection, likely representing reinfection following waning immunity [Citation62].
Figure 1. Pertussis notification data from 6 countries in the Asia-Pacific region Pertussis notification data (number of notifications) from 2001 onwards from government websites of Australia [Citation48], New Zealand [Citation49], Hong Kong [Citation50,Citation63], Singapore [Citation51], South Korea [Citation52] and Taiwan [Citation53,Citation54]. Data presented by age-group where available
![Figure 1. Pertussis notification data from 6 countries in the Asia-Pacific region Pertussis notification data (number of notifications) from 2001 onwards from government websites of Australia [Citation48], New Zealand [Citation49], Hong Kong [Citation50,Citation63], Singapore [Citation51], South Korea [Citation52] and Taiwan [Citation53,Citation54]. Data presented by age-group where available](/cms/asset/3ddec072-ddc2-4c8c-b8fe-1a8f76f9fbab/ierv_a_1990759_f0001_oc.jpg)
The hospital admission rate for pertussis in adults aged 65+ years was 4.9 per 100,000 population between 2006 and 2012, which was higher than any age-group over 4 years [Citation61]. The median length of hospital stay in older adults was 7 days versus 4 days in <6 month-olds and 2 days in those aged 6 months to 4 years [Citation61]. In 2008–2009 during a pertussis outbreak in New South Wales, 13% of all hospitalizations for pertussis were adults aged 60+ years and 4% of all cases required admission to intensive care units [Citation64]. Other surveillance data from New South Wales found that hospitalization rates for pertussis infection in adults were age-dependent, increasing from 0.7 per 100,000 person-years in 45–64 year-olds, to 4.3 per 100,000 person-years in 65–74 year-olds, and 5.4 per 100,000 person-years in 75+ year-olds [Citation32]. Hospitalization rates for pertussis-related illnesses (hospitalized with ICD10 code A37 [whooping cough], or hospital admission for cough or respiratory disease within 1 week before and up to 6 weeks after a pertussis diagnosis) increased similarly with age, from 2.2, to 8.5 to 13.5 per 100,000 person-years in the respective age-groups. The risk of pertussis was higher in adults who were obese, who took medication, or who had pre-existing asthma [Citation32].
3.2. New Zealand
New Zealand pertussis notification data from 2001 to 2017 show a cyclic pattern that is similar to Australia, although the 2 countries differed in the timing of pertussis outbreaks () [Citation49]. Most pertussis notifications in New Zealand between 2001 and 2017 were in adolescents and adults, but the highest incidence was in children <1 year of age at 213 per 100,000 population in 2017. The 2017 incidence of pertussis notifications was 24 per 100,000 population in 60–69 year-olds, and 18.3 per 100,000 population in 70+ year-olds. From 2010, between 9.3% and 16.4% of all pertussis notifications were in adults aged 65+ years. Approximately 4% of patients aged 65+ years with pertussis required hospitalization, compared with 0–1% of patients who were 5–64 years of age. The rate of hospitalization for pertussis was 1.4 per 100,000 person-years in 65+ year-olds, which was higher than in any other age-group over 4 years.
3.3. Hong Kong
Fewer than 50 cases of pertussis were reported annually between 2001 and 2016 (). The number of cases jumped to 110 in 2018, of which 44 were in infants aged ≤6 months [Citation65]. There were 93 cases in adults aged 18+ years recorded in 2017 and 2018, of whom 83% (77 cases) had no or unknown history of pertussis vaccination, including 48% (45 cases) who were not born in Hong Kong, and whose childhood vaccination history was not known [Citation66].
3.4. Singapore
Only 1 or 2cases of laboratory-confirmed pertussis were reported annually in Singapore from 1993 until 2005 [Citation67] (). PCR testing was introduced at the end of 2006, and the annual number of cases increased, but remained <30 per year until 2015. The population incidence of pertussis was estimated to be 0.8 per 100,000 in 2007 and 0.4 per 100,000 in 2014 [Citation51,Citation68], and all cases were reported in children <5 years of age. The low observed incidence is most probably due to a lack of disease awareness in Singapore, leading to low rates of testing and under-reporting [Citation67]. This is supported by data from 2002 that found a 97% seroprevalence rate for anti-PT antibodies in adults 18–45 years of age; evidence of high rates of pertussis infection amongst Singaporean adolescents and adults, none of whom had received an adult pertussis booster dose [Citation69]. Additionally, studies of infants with pertussis admitted to intensive care units showed evidence of transmission from undiagnosed household contacts [Citation70].
Since 2015, pertussis notifications have increased, with 80 cases reported in 2016, 76 in 2017 and 108 in 2018. The first cases in adults aged 65+ years were recorded in 2016, and the proportion of notifications attributable to this age-group has climbed steadily, reaching 16.2% (17 cases) of all cases in 2018. The incidence rate of pertussis in Singapore is highest in infants <1 year of age, ranging from 103.5 to 115.9 per 100,000 populations in 2015–2018. The 2018 incidence rate in adults aged 65+ years was 3.1 per 100,000.
3.5. South Korea
Before 2009, fewer than 20 notifications of pertussis were recorded annually in South Korea, and almost all were in children <1 year of age. After 2009, reporting rates increased in all age-groups. In 2016, there were 39 pertussis notifications among adults aged 60+ years, making up 30.2% of all reports that year. In 2018, the number of cases peaked at 980, of which the majority was in 5–59 year-olds, with 142 cases (14.5%) in adults aged 60+ years.
Published data from South Korea also support significant under-reporting of pertussis [Citation71], with several studies identifying unrecognized infections in adults with prolonged cough () [Citation72–75], and seroprevalence surveys showing high rates of anti-PT antibodies in the absence of recent booster vaccination, consistent with recent infection in adolescents and adults [Citation76–79]. In 2012, a seroprevalence survey of adolescents and adults found that the highest anti-PT seroprevalence (48.1%) was in adults aged 61+ years [Citation77]. Among 412 hospital healthcare workers, anti-PT seroprevalence in 2011 was 33.7% [Citation78]. A 2008 survey of healthy children and adults showed that 57% of participants 51−60 years of age and 55% of those ≥61 years of age had anti-PT titers indicative of seroprotection [Citation79].
Table 2. Prospective studies investigating prolonged cough in adults in South Korea
3.6. Taiwan
Surveillance data from 2001 reported fewer than 100 pertussis cases annually, with no clear cyclic pattern. A report of Taiwan Center for Disease Control and Prevention data between 2003 and 2017 included 668 pertussis cases over this period, with a mean incidence of 0.12 per 100,000 population prior to 2009, and 0.27 per 100,000 from 2009 to 2015 [Citation80]. The majority of cases were in infants <1 year of age, and very few cases were reported in adults aged 40+ years (annual incidence <0.1 per 100,000 population).
Over the last two decades, the number of pertussis cases among young infants has increased, which might suggest increased circulation and resurgence of pertussis in society; however, an increase in cases in adults has not yet been observed, possibly due to under-reporting [Citation76,Citation81]. A small study of 33 patients of all ages presenting to hospital with cough of at least 1 week duration found that 8 (21%) had pertussis as diagnosed by PCR or serology [Citation82]. By contrast, a seroprevalence study of 89 adults with cough duration ≥14 days identified only 1 case of recent pertussis (1.1%) [Citation83].
4. Recommendations for pertussis booster vaccination in adults
The current WHO recommendation concerning pertussis vaccination of adults advises that adult boosters should only be introduced after assessment of local epidemiology, incidence and cost-effectiveness data, and only when high infant coverage rates have been achieved [Citation84]. Globally, 15 countries/regions specifically recommend Tdap vaccination for adults aged 65+ years (Australia, Austria, Bahrain, Belgium, Czech Republic, Germany, Iceland, Ireland, Italy, Liechtenstein, Luxembourg, New Zealand, Slovenia, Taiwan, and the US) [Citation85–89]; 13 of them are national-level recommendations and 8 countries/regions provide vaccine funding. Nine countries/regions recommend a single Tdap booster vaccination for older adults (Australia, Bahrain, Germany, Iceland, Ireland, Luxembourg, Slovenia, and the US), 6 recommend Tdap every 10 years (Italy, Slovenia, Liechtenstein, Belgium [Flanders], Luxembourg, and the Bahamas) [Citation89]. Austria suggests a booster every 5 years, the Czech Republic recommends an interval of 10–15 years, and New Zealand recommends Tdap at age 45 and 65 years. The US Advisory Committee on Immunization Practices updated recommendations for Tdap boosters in adults in 2019 [Citation88]. Either Td or Tdap vaccines may be used for the decennial Td booster, tetanus prophylaxis for wound management, and for additional required doses in the catch-up immunization schedule if a person has received at least 1 Tdap dose. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has updated guidelines for persons with COPD with the US CDC recommendation that adults with COPD receive Tdap vaccination if not vaccinated in adolescence [Citation90].
Tdap recommendations for the 6 Asia-Pacific countries studied here are summarized in . Australia recommends (but does not fund) a single Tdap dose for any adult who wishes to be vaccinated, for travelers and for adults aged 65+ years who have not received a pertussis vaccine in the last 10 years, and decennial Tdap vaccination for healthcare and childcare workers. South Korea recommends a single booster dose for adults aged 18+ if they have not previously received Tdap vaccine. In addition, pregnant women without previous Tdap vaccine are recommended to receive a dose of Tdap vaccine right after or before pregnancy [Citation91–93]. Taiwan recommends Tdap for pregnant women and use of Tdap once instead of the recommended decennial Td vaccination. Tdap is not currently recommended for adults in Hong Kong or Singapore (except pregnant women).
Table 3. Tdap booster recommendations in 6countries of the Asia-Pacific region
5. Barriers and success factors for vaccination of older adults
5.1. Tdap vaccination
Among the countries we studied, awareness of pertussis in adults appears to be highest in Australia, with several studies published [Citation94–96]. We found only one study in the published literature that described barriers and success factors to Tdap vaccination of adults [Citation96]. This study was a market research study of 412 general practitioners (GPs) and 6529 adult consumers in Australia. The discussion of pertussis vaccination during outbreaks or in patients with underlying diseases was uncommon, and that GPs were more likely to recommend vaccination for older adults if they were grandparents of young children. Consumers identified GPs as the most reliable source of information about vaccination, and the lack of GP recommendation and lack of awareness about the need for vaccination as the most common reasons for not being vaccinated [Citation96].
5.2. Learning from influenza vaccination in older adults
In the absence of specific information about factors that influence Tdap vaccine acceptance in Asia-Pacific countries, we looked for parallels between barriers to the uptake of other vaccines and barriers to pertussis vaccination in older adults. Barriers to vaccination of adults in Asia-Pacific countries have been investigated most often in the context of influenza vaccine. Studies in Australia and New Zealand found that the perception of sufficient existing immunity capable of resisting infection was one of the most common reasons cited for not having influenza vaccination, whereas receiving a recommendation from a healthcare professional was associated with vaccine uptake [Citation23,Citation97]. Influenza vaccine uptake was also higher in Singaporean adults with diabetes if they had received a recommendation from their healthcare professional, and uptake was also associated with higher income and cheaper vaccines [Citation98]. A survey of 15 adults aged 65+ years found that in this population, vaccine misconceptions were the most common reasons for not vaccinating, including that vaccination was a cure for influenza instead of for prevention, that vaccination was only needed when traveling, and that the vaccine was too ‘strong’ for older persons [Citation99]. Some reported that they would have been vaccinated if it had been recommended to them by their doctor [Citation99].
A study of influenza vaccine uptake in Taiwan found that vaccination was significantly less likely among individuals who were 85+ years, those with severe disabilities, indigenous persons, and persons hospitalized in the previous year. In Taiwan, where the influenza vaccine is free, the authors recommended an integrated policy for disabled elderly persons, incentives for healthcare providers and caregivers, and media campaigns to improve education about vaccine availability and benefits [Citation21].
In adults in South Korea, uptake of influenza vaccination was associated with a history of prior influenza-like illness, regular exercise, and positive opinions about the vaccine [Citation100]. Reasons for not being vaccinated were time constraints and the perception that good health meant that vaccination was not required [Citation100].
A study of vaccine providers in South Korea identified vaccine hesitancy as the single highest barrier to vaccination, based on fears of side-effects, vaccine safety, and a preference to rely on natural immunity for protection [Citation101]. Low accessibility to clinics in rural areas and lack of time to attend clinics were also contributing factors [Citation101]. During the 2009–2010 influenza pandemic, the most common event triggering vaccination was individual notification from a public health organization. By contrast, confidence in their own health and lack of time were the most common reasons for not being vaccinated [Citation102].
In a Hong Kong study, the strongest barriers to influenza vaccination were a desire to rely on one’s own immunity to prevent infection, a perception of low risk, and concerns around side-effects and vaccine safety and effectiveness [Citation22]. Another study in 65+ year-olds in Hong Kong identified strong cultural perceptions in this age-group that influenced vaccine acceptance and uptake [Citation103]. The study population universally perceived vaccines to be harmful, and this was accompanied by beliefs of low personal risk, lack of promotion by healthcare providers, a perceived risk (catch a disease or ‘unlucky’) associated with attending clinic/hospitals, and a preference for using traditional Chinese medicine.
6. Conclusion
The number of notified pertussis cases has increased in the Asia-Pacific region and the increase is more apparent in countries where awareness of the disease exists as a differential diagnosis to prolonged cough, and where diagnostic practices and reporting systems are well established. The range of pertussis notification rates in the countries we studied was extreme. In countries with available data, hospitalization rates in adults aged 65+ years with pertussis were higher than in adolescents or younger adults. However, data on hospitalization rates were sparse; in adults aged 65+ years, we identified a rate of 4.9 per 100,000 population in Australia and 1.4 per 100,000 in New Zealand [Citation49,Citation61]. The Global Burden of Disease Study reported almost 66 million hospitalizations globally for lower respiratory infections among all ages in 2016 [Citation104]. We estimate that this corresponds to approximately 929 hospitalizations per 100,000 population based on a world population of 7 billion in 2016, substantially higher than the rates we identified for pertussis hospitalization.
Pertussis is a notifiable disease in all 6 of the countries/regions we assessed. Yet, there is evidence of substantial under-diagnosis in Singapore, South Korea, and Taiwan (and probably Hong Kong for which very little data are available) from seroprevalence studies indicating high rates of pertussis infection in adults, with the highest rates in older adults. As a result, there are important data gaps in terms of understanding the age-groups and populations most affected, the incidence of complications, and the economic burden caused by pertussis. Few countries recommend Tdap vaccination for adults and uptake in those countries is sub-optimal. Increasing disease awareness, establishing vaccination registries, and establishing recommendations are key factors to increase Tdap vaccination rates and promote healthy aging. provides a summary of the main findings of this review.
7. Expert opinion
Pertussis is usually considered a childhood disease; however, recent studies also illustrate disease burden in older adults. While most pertussis infections among adults may not result in hospitalization, the risk of hospitalization, death, and complications increases with age and there is a significant impact on the quality of life [Citation31,Citation32,Citation105]. Moreover, older adults can serve as a reservoir of pertussis [Citation40]. There are, therefore, compelling reasons to improve awareness of pertussis, and the need for vaccination.
An increasing number of notifications in Hong Kong, Singapore, South Korea, and Taiwan may be partially attributed to increased accessibility to diagnostic tests such as PCR. Several multiplex PCR manufacturers offer Bordetella pertussis PCR as part of a panel of respiratory pathogens [Citation106,Citation107]. Seroprevalence data show that pertussis is circulating in Singapore and South Korea, while data is lacking for Hong Kong and Taiwan. Despite the increasing number of reported cases, the impact of pertussis amongst older adults and people at risk is largely unknown in Hong Kong, Singapore, South Korea, and Taiwan. Similarly, wider effects of pertussis such as healthcare resource usage, costs to the economy, and unnecessary antibiotic prescriptions that can potentially impact on antimicrobial resistance trends are unquantified in all countries.
A better understanding of the burden of pertussis disease is key to driving a change in vaccination policy. Seroprevalence data and studies of prolonged cough indicate that pertussis is circulating in older adults in the Asia-Pacific region and that the infection rate is considerably underestimated. Although many pertussis infections in adults are asymptomatic, underestimation of infection inevitably leads to underestimation of the burden of disease. More epidemiological data are required from countries in the Asia-Pacific to understand the incidence of pertussis, particularly in specific populations such as 65+ year-olds and other at-risk groups. In settings where there is low disease awareness amongst healthcare professionals, pertussis is not diagnosed, and notification data are unable to fill existing data gaps. An important goal in these settings is to increase disease awareness through education campaigns and data from epidemiological studies conducted locally. Studies that assess the excess burden of diseases/conditions potentially associated with pertussis infection in the adult population or in specific risk groups, e.g., cardiorespiratory disease, stroke, during pertussis epidemics could be conducted locally and without the need to capture all pertussis cases. In addition, to adequately capture the burden of pertussis disease in adults, it is important that appropriate diagnostic laboratory methods for adult populations are used i.e., serology testing in addition to culture or real-time PCR methods [Citation45,Citation47].
The current level of evidence in the countries we studied is considered strong enough to support ‘individual’ recommendations (physician to patient) for pertussis vaccination of adults aged 65+ years, but existing evidence is not strong enough to support a recommendation for Tdap vaccination amongst all adults and high-risk groups. The addition of a Tdap booster dose in 65+ year-olds makes sense from the perspective of medical need and practical implementation. Age itself is a risk for severe pertussis disease, and Tdap vaccination could be easily added to existing platforms for influenza, herpes zoster, and pneumococcal vaccination in this age-group. Tdap also provides booster vaccination against diphtheria and tetanus. In Australia, 90% of deaths due to tetanus in the last 30 years have been in adults aged 65+ years [Citation108]. A seroprevalence study in South Korea in 2007–2008 showed that 92.0% of adults aged 61+ years had anti-tetanus antibody concentrations below the protective level of 0.1 IU/ml [Citation109]. Tdap booster vaccination at age 65+ years would have the added benefit of boosting tetanus immunity in older populations in whom protection against tetanus has waned.
Other known risk groups for pertussis that could be considered for Tdap vaccination are those with underlying multi-morbidities such as asthma and COPD [Citation32,Citation35,Citation110]. It is reasonable to consider that patients with chronic respiratory diseases might be at higher risk of severe pertussis disease and of exacerbations of underlying disease, and judicious vaccination of such individuals appears reasonable. Pertussis in persons with these conditions can trigger exacerbations of their pre-existing illness [Citation111], resulting in hospitalization and antibiotic use. Patients with cancer receiving chemotherapy and patients with chronic kidney disease are priority groups for influenza vaccination because they are at high risk of severe or fatal influenza [Citation112]. We speculate that impaired immunity could also potentially lead to more severe pertussis disease, although this needs to be confirmed. Patients with cancer and patients with renal disease could be candidates for timed Tdap vaccination linked to current recommendations in these groups for pneumococcal and hepatitis B vaccination, for example, priorf to commencing chemotherapy or prior to commencing dialysis [Citation113]. The wider impact on older adults in terms of frailty and the consequences of complications including, cardio-respiratory events and cerebral hemorrhage need further elucidation. This information will be important in undertaking cost-effectiveness analysis of adult pertussis booster vaccination in the Asia-Pacific.
Success factors and barriers to Tdap vaccination in healthy adults are summarized in .. Important barriers to vaccination included lack of awareness about the disease and low disease prioritization amongst recommending and funding bodies, which translated to lack of funding for vaccination. Limited access to vaccination arising from low awareness and lack of prioritization of vaccination by healthcare professionals was an issue in some countries, as well as views among adults that vaccines are not required for healthy aging and perceptions that a ‘strong’ immune system is sufficient to prevent infection. Lack of time to attend vaccination visits among adults was important in some countriesand was linked to the absence of regular or scheduled interactions with healthcare providers, and uncertainty as to who was the vaccinator. Unlike influenz which follows a seasonal cycle and an annual vaccination pattern, the lack of seasonality of pertussis vaccination was also considered a barrier to vaccine uptake.
Figure 2. Current barriers and suggested solutions to improve Tdap vaccination amongst healthy adults

To overcome these issues, the Advisory Board identified vaccination infrastructure as a key factor for the success of Tdap uptake in adults. This should include setting up registries for adult vaccination, identifying target populations for vaccination, and using personalized reminders as a tool to inform adults when vaccination is due. Further education is needed for healthcare professionals and the general public in terms of increasing disease awareness. Vaccination recommendations and funding from governments were seen as critical, which could be combined with incentives for vaccination or penalties for non-compliance.
The published information around influenza vaccine acceptance in Asia-Pacific countries shows many common barriers and success factors for adult vaccination to those identified by the Advisory Board with respect to Tdap vaccination uptake. Strategies to promote vaccine uptake need to be tailored to account for the specific individualities of population groups. However, overriding common factors for success in all countries are the need for education of healthcare professionals and patients around disease awareness and the benefits of vaccination, and the critical influence that primary healthcare providers have in promoting vaccination to their patients. In Australia, where Tdap recommendations are in place, market research data showed gaps between recommendation, awareness, and vaccination coverage, highlighting that the presence of official recommendations (i.e., Australian Technical Advisory group on Immunisation) alone is insufficient to achieve the maximum public health benefit [Citation96]. It needs active recommendation by healthcare professionals.
Lessons learnt from influenza and pneumococcal vaccination programs can be applied to pertussis implementation [Citation114]. Successful implementation of Tdap vaccination will require strategies that are adapted to the local setting and the target group. For example, in Hong Kong, education of older adults is needed to counteract traditionally held beliefs about vaccines and the capability of the immune system, and vaccine delivery outside of hospitals and clinics may be needed to improve uptake. In South Korea, increased accessibility to vaccine centers is needed in rural areas, and education that prioritizes vaccination such that busy adults make time to be vaccinated is needed. It is important that Tdap vaccination should not create yet another visit to the healthcare provider but should be provided within existing structures.
In the next 5 years, we foresee the development of a ‘Healthy Aging Vaccination Package,’ a portfolio approach that will increase awareness of the role of vaccines in staying healthy while growing old [Citation10]. Such a package could include currently available Tdap, influenza, herpes zoster, and pneumococcal vaccines, with the inclusion of new vaccines targeting diseases of importance for older adults as they become available. These could include vaccines against bacteremia (e.g. Escherichia coli, Staphylococcus aureus), respiratory infections such as respiratory syncytial virus, improved pneumococcal vaccines, and others. Currently available Tdap vaccines can be added with relative ease to existing immunization schedules and should be included in a vaccination package for older persons.
Childhood immunization registries have existed in many countries for decades, but as yet, registries to record adult immunization are lacking. In all countries, establishing an immunization registry for all vaccine recipients, including adults, is critical for providing the foundation on which to assess data on vaccine coverage, evaluate the performance of the vaccine and the success of the vaccination program.
Unfortunately, the current vaccination uptake for ‘established’ vaccines among adults is low, so there is still a need to improve the general awareness about vaccine-preventable diseases and use of vaccines in this population. Disease awareness in the general public and among healthcare professionals is needed to underpin any further strategies to address and achieve this goal.
BOX 1 Conclusions and recommendations of the Expert Advisory Panel
Article highlights
Burden of pertussis has been increasing in older adults, but the true burden is not well understood in countries in the Asia-Pacific region
There is a need for evidence generation on the risk and burden as well as impact of pertussis among older adults.
Increasing awareness on pertussis would be helpful to capture the disease burden and experts proposed measures to increase awareness about vaccination and suggested tracking and evaluating vaccine uptake.
Based on currently available data, vaccination against pertussis for older adults (aged 65 or older) at individual level is recommended as well as patients with COPD or asthma.
This expert opinion might help the healthcare community build action plans to achieve these goals
Declaration of interest
P Buchy, J Chen, M Nissen and KB Oh are employees of the GSK group of companies and hold shares in the GSK group of companies. LH Nam, CH Chiu, JY Heo, M Ip, KS Jung, R Menzies and R Pearce received a fee from the GSK group of companies for their attendance at the advisory board meeting. LH Nam received honoraria for talks from Sanofi Pasteur outside of the submitted work. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Acknowledgments
The authors would like to thank Sanjoy Datta and Elisa Turriani for their attendance at the advisory board meeting and Sanjoy Datta for his review of the manuscript. The authors would also like to thank Business & Decision Life Sciences platform for editorial assistance and manuscript coordination, on behalf of GSK. Janne Tys coordinated manuscript development and editorial support and Joanne Wolter provided medical writing support.
Additional information
Funding
References
- United Nations. Department of economic and social affairs [internet]. world population prospects: 2019. highlights. [ cited 2019 Jul 12]. Available from https://population.un.org/wpp/Publications/Files/WPP2019_10KeyFindings.pdf
- Cristea M, Noja GG, Stefea P, et al. The impact of population aging and public health support on EU labor markets. Int J Environ Res Public Health. 2020;17:4.
- World Health Organization. The global strategy and action plan on ageing and health [internet]. [ cited 2020 Jan 08]. Available from http://www.who.int/ageing/global-strategy/en/
- Building a resilient immune system: Interview with Prof. Philip calder (part 1) 2 Nov 2016. Kristina Campbell immune health, news watch. Available from https://www.gutmicrobiotaforhealth.com/en/building-resilient-immune-system-interview-prof-philip-calder-part-1/ Accessed 2020 Jan 08)
- Building a resilient immune system: Interview with Prof. Philip calder (part 1) 2 Nov 2016. Kristina Campbell immune health, news watch [internet]. [ cited 2020 Jan 08]. Available from https://www.gutmicrobiotaforhealth.com/en/building-resilient-immune-system-interview-prof-philip-calder-part–1/
- Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323(18):1775–1776.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062.
- Janko M. Vaccination: a victim of its own success. Virtual Mentor. 2012;14(1):3–4.
- Lang PO, Aspinall R. Vaccination in the elderly: what can be recommended? Drugs Aging. 2014;31(8):581–599.
- Doherty TM, Del Giudice G, Maggi S. Adult vaccination as part of a healthy lifestyle: moving from medical intervention to health promotion. Ann Med. 2019;51(2):128–140.
- Tan L. Adult vaccination: now is the time to realize an unfulfilled potential. Hum Vaccin Immunother. 2015;11(9):2158–2166.
- Cherry JD. Adult pertussis in the pre- and post-vaccine eras: lifelong vaccine-induced immunity? Expert Rev Vaccines. 2014;13(9):1073–1080.
- Esposito S, Stefanelli P, Fry NK, et al. Pertussis prevention: reasons for resurgence, and differences in the current acellular pertussis vaccines. Front Immunol. 2019;10:1344.
- Amirthalingam G, Campbell H, Ribeiro S, et al. Sustained effectiveness of the maternal pertussis immunization program in England 3 years following introduction. Clin Infect Dis. 2016;63(suppl 4):S236–S243.
- Kandeil W, Atanasov P, Avramioti D, et al. The burden of pertussis in older adults: what is the role of vaccination? A systematic literature review. Expert Rev Vaccines. 2019;18(5):439–455.
- Ga P, Rm J, IG O. Trends affecting the future of vaccine development and delivery: the role of demographics, regulatory science, the anti-vaccine movement, and vaccinomics. Vaccine. 2009;27(25–26):3240–3244.
- Australian Institute of Health and Welfare. The burden of vaccine preventable diseases in Australia. Cat. no. PHE 263. Canberra: AIHW; 2019.
- Choe YJ, Choe SA, Cho SI. Trends in infectious disease mortality, south korea, 1983-2015. Emerg Infect Dis. 2018;24(2):320–327.
- Williams WW, Lu PJ, O’Halloran A, et al. Surveillance of vaccination coverage among adult populations -– United States, 2015. MMWR Surveill Summ. 2017;66(11):1–28.
- Nuffieldtrust. Adult flu vaccination coverage [Internet]. [ cited 2020 Feb 26]. Available from https://www.nuffieldtrust.org.uk/resource/adult-flu-vaccination-coverage
- Chang YC, Tung HJ, Hsu SW, et al. Use of seasonal influenza vaccination and its associated factors among elderly people with disabilities in Taiwan: a population-based study. PLoS One. 2016;11(6):e0158075.
- Sun KS, Lam TP, and Kwok KW, et al. Seasonal influenza vaccine uptake among Chinese in Hong Kong: barriers, enablers and vaccination rates. Hum Vaccin Immunother. 2020:16(11) ;1675–1684.
- Australian Institute of Health and Welfare 2011. Adult vaccination survey: summary results. cat. no. PHE 135. Canberra: AIHW; 2009.
- Guimaraes LM, Carneiro EL, Carvalho-Costa FA. Increasing incidence of pertussis in Brazil: a retrospective study using surveillance data. BMC Infect Dis. 2015;15:442.
- Mbayei SA, Faulkner A, Miner C, et al. Severe pertussis infections in the United States, 2011-2015. Clin Infect Dis. 2019;69(2):218–226.
- De Serres G, Shadmani R, Duval B, et al. Morbidity of pertussis in adolescents and adults. J Infect Dis. 2000;182(1):174–179.
- Thomas PF, McIntyre PB, Jalaludin BB. Survey of pertussis morbidity in adults in western Sydney. Med J Aust. 2000;173(2):74–76.
- Lee GM, Lett S, Schauer S, et al. Societal costs and morbidity of pertussis in adolescents and adults. Clin Infect Dis. 2004;39(11):1572–1580.
- Kilgore PE, Salim AM, Zervos MJ, et al. Pertussis: microbiology, disease, treatment, and prevention. Clin Microbiol Rev. 2016;29(3):449–486.
- Kretsinger K, Broder KR, Cortese MM. et al. Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among health-care personnel. MMWR Recommendations and Reports: morbidity and Mortality Weekly Report Recommendations and Reports/Centers for Disease Control. 2006;55( RR-17):1–37.
- Karki S, McIntyre P, Newall AT, et al. Risk factors for pertussis hospitalizations in Australians aged 45 years and over: a population based nested case-control study. Vaccine. 2015;33(42):5647–5653.
- Liu BC, McIntyre P, Kaldor JM, et al. Pertussis in older adults: prospective study of risk factors and morbidity. Clin Infect Dis. 2012;55(11):1450–1456.
- Rothstein E, Edwards K. Health burden of pertussis in adolescents and adults. Pediatr Infect Dis J. 2005;24(5 Suppl):S44–47.
- Mertens PLJM, Borsboom GJJM, Richardus JH. A pertussis outbreak associated with social isolation among elderly nuns in a convent. Clin Infect Dis. 2007;44(2):266–268.
- Capili CR, Hettinger A, Rigelman-Hedberg N, et al. Increased risk of pertussis in patients with asthma. J Allergy Clin Immunol. 2012;129(4):957–963.
- Buck PO, Meyers JL, Gordon LD, et al. Economic burden of diagnosed pertussis among individuals with asthma or chronic obstructive pulmonary disease in the USA: an analysis of administrative claims. Epidemiol Infect. 2017;145(10):2109–2121.
- Jenkins VA, Savic M, and Kandeil W. Pertussis in high-risk groups: an overview of the past quarter-century. Hum Vaccin Immunother. 2020;16(9):;2609–2617.
- Bonhoeffer J, Bar G, Riffelmann M, et al. The role of Bordetella infections in patients with acute exacerbation of chronic bronchitis. Infection. 2005;33(1):13–17.
- Ridda I, Heywood AE, Hueston L, et al. The burden of pertussis in patients with and without recurrent ischaemic vascular events. Infect Disord Drug Targets. 2014;14(2):101–109.
- Bisgard KM, Pascual FB, Ehresmann KR, et al. Infant pertussis: who was the source? Pediatr Infect Dis J. 2004;23(11):985–989.
- Rowe SL, Tay EL, Franklin LJ, et al. Effectiveness of parental cocooning as a vaccination strategy to prevent pertussis infection in infants: a case-control study. Vaccine. 2018;36(15):2012–2019.
- Forsyth K, Plotkin S, Tan T. Wirsing von König CH. Strategies to decrease pertussis transmission to infants. Pediatrics. 2015;135(6):e1475–82.
- Centers for Disease Control and Prevention. Pregnancy and whooping cough. Surround babies with protection. 2017. [Internet]. [ cited 2021 May 6]. Available from https://www.cdc.gov/pertussis/pregnant/mom/protection.html.
- World Health Organization. WHO SAGE pertussis working group. Background paper. 2014. [Internet]. [ cited 2021 May 22]. Available from https://www.who.int/immunization/sage/meetings/2014/april/1_Pertussis_background_FINAL4_web.pdf?ua=1.
- Cherry JD, Tan T, Wirsing von König CH, et al. Clinical definitions of pertussis: summary of a global pertussis initiative roundtable meeting, February 2011. Clin Infect Dis. 2012 Jun;54(12):1756–1764.
- Centers for Disease Control and Prevention. Pertussis (whooping cough). Diagnosis confirmation. [Internet]. [ cited 2021 May 5]. Available from https://www.cdc.gov/pertussis/clinical/diagnostic-testing/diagnosis-confirmation.html.
- Thisyakorn U, Tantawichien T, Thisyakorn C, et al. Pertussis in the association of Southeast Asian Nations: epidemiology and challenges. Int J Infect Dis. 2019 Oct;87:75–83.
- Australian Government. Department of health, national notifiable disease surveillance system [internet]. [ cited 2019 Jun 24]. Available from http://www9.health.gov.au/cda/source/rpt_5_sel.cfm.
- The Institute of Environmental Science and Research - Public Health Surveillance. annual surveillance summary [Internet]. [ cited 2019 Oct 22]. Available from https://surv.esr.cri.nz/surveillance/annual_surveillance.php
- The Government of the Hong Kong Special Administrative Region – Department of Health - Centre for Health Protection. Statistics on communicable diseases [internet]. [ cited 2019 Jun 14]. Available from https://www.chp.gov.hk/en/static/24012.html.
- Ministry of Health Singapore. Communicable disease surveillance in Singapore [internet]. [ cited 2019 Jun 14]. Available from https://www.moh.gov.sg/resources-statistics.
- South Korean Ministry of Welfare and Health - Korea Centers for Disease Control & Prevention. Infectious disease portal [internet]. [ cited 2019 Jun 14]. Available from http://www.cdc.go.kr/npt/biz/npp/ist/bass/bassSexdstnAgeStatsMain.do
- Taiwan Centers for Disease Control. Taiwan national infectious disease statistics system [internet]. [ cited 2019 Dec 11]. Available from https://nidss.cdc.gov.tw/en/SingleDisease.aspx?dc=1&dt=3&disease=033
- Taiwan Centers for Disease Control. Disease surveillance express [internet]. [ cited 2020 Jan 06]. Available from https://www.cdc.gov.tw/En/Category/MPage/3AqyaZ-ycOjQyRx3LoC8vw
- Australian Government Department of Health. Pertussis case definition [Internet]. [ cited 2021 Jun 18]. Available from https://www1.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-nndss-casedefs-cd_pertus.htm.
- Institute of Environmental Science and Research. New Zealand. pertussis [internet]. [ cited 2021 Jun 18]. Available from https://surv.esr.cri.nz/episurv/CaseReportForms/Pertussis-Dec2017.pdf.
- National Centre for Infectious Diseases. Pertussis [Internet]. [ cited 2021 Jun 18]. Available from https://www.ncid.sg/Health-Professionals/Diseases-and-Conditions/Pages/Pertussis.aspx.
- Centre for Health Protection. Communicable disease surveillance case definitions [Internet]. [ cited 2021 Jun 18]. Available from https://cdis.chp.gov.hk/CDIS_DINS_ONLINE/document/previewPDF?id=3639967.
- Taiwan Centers for Disease Control. Pertussis [Internet]. [ cited 2021 Jun 18]. Available from https://www.cdc.gov.tw/File/Get/hXlOZtreRs3dNqSHcgjomg. Accessed 2021 Jun 18
- Korea Centers for Disease Control and Prevention. Pertussis integrated management guidelines [Internet]. [ cited 2021 Jun 22]. Available from https://www.google.be/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiRgaDK7KrxAhWUA2MBHWmCASkQFjAAegQIBRAD&url=http%3A%2F%2Fwww.busancidc.or.kr%2Fboard%2FdownFileD.do%3Fno%3D24%26view%3Dview%26idx%3D254&usg=AOvVaw3_q4MbUe5B-hqThtWl1YbF.
- Pillsbury A, Quinn HE, McIntyre PB. Australian vaccine preventable disease epidemiological review series: pertussis, 2006-2012. Commun Dis Intell Q Rep. 2014;38(3):E179–194.
- Cagney M, MacIntyre CR, McIntyre P, et al. The seroepidemiology of pertussis in Australia during an epidemic period. Epidemiol Infect. 2006;134(6):1208–1216.
- Wong K. An update on infectious diseases in hong kong. 16th annual scientific meeting. Stanley Ho centre for emerging infectious diseases, CUHK 11 June 2019 [Internet]. [ cited 2020 Aug 17]. Available from http://www.cuhk.edu.hk/med/ceid/images/asm/16_asm/Dr%20KH%20WONG.pd
- Spokes PJ, Quinn HE, and McAnulty JM. Review of the 2008-2009 pertussis epidemic in NSW: notifications and hospitalisations N S W Public Health Bull . New South Wales public health bulletin. 2010;21(7–8):167–173.
- Siu P, Cheung E. Pregnant Hongkongers urged to get whooping cough vaccine as number of cases in city almost doubles leaving some infants in intensive care. South China Morning Post 9 Jan 2019 [Internet]. [ cited 2020 Feb 24]. Available from. https://www.scmp.com/news/hong-kong/health-environment/article/2181416/pregnant-hongkongers-urged-get-whooping-coughaccessed
- Hong Kong Center for Health Protection. Scientific Committee on Vaccine Preventable Disease. Scientific committee on vaccine preventable diseases consensus recommendations on pertussis vaccination for pregnant women in hong kong. [ cited 2020 Jun 16]. Available from https://www.chp.gov.hk/files/pdf/recommendations_on_pertussis_vaccination_for_pregnant_women_in_hk_formatted.pdf
- Goh A, Chong CY, Tee N, et al. Pertussis–an under-diagnosed disease with high morbidity in Singapore children. Vaccine. 2011;29(13):2503–2507.
- Ministry of Health, Singapore. Communicable diseases surveillance in Singapore, 2007 [Internet]. [ cited 2020 Feb 21]. Available from https://www.moh.gov.sg/resources-statistics/reports/communicable-diseases-surveillance-in-singapore-2007.
- Wilder-Smith A, Ng S, Earnest A. Seroepidemiology of pertussis in the adult population of Singapore. Ann Acad Med Singapore. 2006;35(11):780–782.
- Kowalzik F, Barbosa AP, Fernandes VR, et al. Prospective multinational study of pertussis infection in hospitalized infants and their household contacts. Pediatr Infect Dis J. 2007;26(3):238–242.
- Choe YJ, Kim JW, Park YJ, et al. Burden of pertussis is underestimated in South Korea: a result from an active sentinel surveillance system. Jpn J Infect Dis. 2014;67(3):230–232.
- Lee SY, Han SB, Kang JH, et al. Pertussis prevalence in Korean adolescents and adults with persistent cough. J Korean Med Sci. 2015;30(7):988–990.
- Park S, Lee MG, and Lee KH, et al. A multicenter study of pertussis infection in adults with coughing in Korea: PCR-based study Tuberc Respir Dis . . 2012;73(5): 266–272
- Kwon HJ, Yum SK, Choi UY, et al. Infant pertussis and household transmission in Korea. J Korean Med Sci. 2012;27(12):1547–1551.
- Park S, Lee SH, Seo KH, et al. Epidemiological aspects of pertussis among adults and adolescents in a Korean outpatient setting: a multicenter, PCR-based study. J Korean Med Sci. 2014;29(9):1232–1239.
- Son S, Thamlikitkul V, Chokephaibulkit K, et al. Prospective multinational serosurveillance study of Bordetella pertussis infection among 10- to 18-year-old Asian children and adolescents. Clin Microbiol Infect. 2019;25(2):250e251–250 e257.
- Lee SY, Han SB, Bae EY, et al. Pertussis seroprevalence in Korean adolescents and adults using anti-pertussis toxin immunoglobulin G. J Korean Med Sci. 2014;29(5):652–656.
- Choi WS, Kim SH, Park DW. Seroprevalence of pertussis in healthcare workers without adult pertussis vaccine use at a university hospital in Korea. J Korean Med Sci. 2018;33(50):e321.
- Lee S, Choi U, Kim J, et al. Immunoassay of pertussis according to ages. Korean J Pediatr infect Dis. 2021;19(2): 55–60
- Chang IF, Lee PI, Lu CY, et al. Resurgence of pertussis in Taiwan during 2009-2015 and its impact on infants. J Microbiol Immunol Infect. 2019;52(4):542–548.
- Lin YC, Yao SM, Yan JJ, et al. Epidemiological shift in the prevalence of pertussis in Taiwan: implications for pertussis vaccination. J Med Microbiol. 2007;56(Pt 4):533–537.
- Hu JJ, Lu CY, Chang LY, et al. Survey of pertussis in patients with prolonged cough. Journal of microbiology, immunology, and infection = Wei mian yu gan ran za zhi. 2006;39(1): 54–58
- Koh MT, Liu CS, Chiu CH, et al. Under-recognized pertussis in adults from Asian countries: a cross-sectional seroprevalence study in Malaysia, Taiwan and Thailand. Epidemiol Infect. 2016;144(6):1192–1200.
- Pertussis vaccines: WHO position paper - September. 2015. Week Epidemiol Rec 2015; 90(35): 433–458
- Australian Technical Advisory Group on Immunisation (ATAGI). Australian Immunisation Handbook, Australian Government Department of Health, Canberra, 2018.[Internet]. [ cited 2020 Feb 24]. Available from https://immunisationhandbook.health.gov.au/
- Kingdom of Bahrain Ministry of Health. Immunizations. [Internet]. [ cited 2020 Jun 25]. Available from https://www.moh.gov.bh/HealthInfo/Immunizations?lang=en
- European Centre for Disease Prevention and Control. ECDC Vaccine schedules in all countries of the European Union. [Internet]. [ cited 2020 Jun 25]. Available from https://vaccine-schedule.ecdc.europa.eu/
- Havers FP, Moro PL, Hunter P, et al. Use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccines: updated recommendations of the advisory committee on immunization practices - United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(3):77–83.
- New Zealand Immunisation Advisory Centre. [Internet]. [cited 2020 Jun 25]. Available from https://www.immune.org.nz/hot-topic/pharmac-announces-immunisation-schedule-1-july-2020.
- Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2021 report). [Internet]. [cited 2021 Jan 25]. Available from https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf
- Recommended immunization schedule for adults in Korea, by the Korean society of infectious diseases, 2012. Clin Exp Vaccine Res. 2014;3(1):110–112.
- Singapore Ministry of Health. 21 Oct 2017 Annex A. summary of national adult immunisation schedule (NAIS) iinternetinternet]. [ cited 2020 Feb 21]. Available from https://www.moh.gov.sg/news-highlights/details/moh-establishes-national-adult-immunisation-schedule-extends-use-of-medisave-for-vaccines-under-the-schedule
- Taiwan Centers for Disease Control. Recommended schedule for adult vaccination. [Internet]. [ cited 2020 Aug 17]. Available from https://www.cdc.gov.tw/File/Get/KaYmM41oLshy3-WfBrUTsQ.
- Clarke M, Thomas N, Giles L, et al. Community awareness and predictors of uptake of pertussis booster vaccine in South Australian adults. Vaccine. 2015;33(51):7337–7343.
- Ridda I, Gao Z, Macintyre CR. Attitudes, knowledge and perceptions towards whooping cough and pertussis vaccine in hospitalized adults. Vaccine. 2014;32(9):1107–1112.
- Bayliss J, Randhawa R, and Oh KB, et al. Perceptions of vaccine preventable diseases in Australian healthcare: focus on pertussis. Hum Vaccin Immunother. 2020;17(2): ;344–350.
- Brunton C, Weir R, Jennings L, et al. Knowledge and attitudes about influenza vaccination amongst general practitioners, practice nurses, and people aged 65 and over. N Z Med J. 2004;118(1214):U1434.
- Tan EK, Lim LH, Teoh YL, et al. Influenza and seasonal influenza vaccination among diabetics in Singapore: knowledge, attitudes and practices. Singapore Med J. 2010;51(8):623–630.
- Teo LM, Smith HE, Lwin MO, et al. Attitudes and perception of influenza vaccines among older people in Singapore: a qualitative study. Vaccine. 2019;37(44):6665–6672.
- Kee SY, Lee JS, Cheong HJ, et al. Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J Infect. 2007;55(3):273–281.
- Park B, Choi EJ, Park B, et al. Factors influencing vaccination in Korea: findings from focus group interviews. J Prev Med Public Health. 2018;51(4):173–180.
- Heo JY, Chang SH, Go MJ, et al. Risk perception, preventive behaviors, and vaccination coverage in the Korean population during the 2009-2010 pandemic influenza A (H1N1): comparison between high-risk group and non-high-risk group. PLoS One. 2013;8(5):e64230.
- Siu JY. Perceptions of Seasonal Influenza and Pneumococcal Vaccines Among Older Chinese Adults. Gerontologist.2018;61(3):439–448 .
- Troeger C, Blacker B, Khalil IA, GBD 2016. Lower Respiratory Infections Collaborators.Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-20161990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Infect Dis. 2018;18(11):1191–1210.
- Ridda I, YinJK JK, King C, et al. The importance of pertussis in older adults: a growing case for reviewing vaccination strategy in the elderly. Vaccine. 2012;30(48):6745–6752.
- Oh SC, Park SM, and Hur J, et al. Effectiveness of rapid multiplex polymerase chain reaction for early diagnosis and treatment of pertussis. J Microbiol Immunol Infect. 2020;54(4):687–692 .
- Parcina M, Schneider UV, Visseaux B, et al. Multicenter evaluation of the QIAstat Respiratory Panel-APanel—A new rapid highly multiplexed PCR based assay for diagnosis of acute respiratory tract infections. PLoS One. 2020;15(3):e0230183.
- Australian Institute of Health and Welfare 2018 [Internet]. Tetanus in Australia. [ cited 2020 Feb 28]. Available from https://www.aihw.gov.au/getmedia/f877a2da-23e3-4516-948f-df05ca7ceb43/aihw-phe-236_Tetanus.pdf.aspx
- Lee S, Kim J, Ahn J, et al. Immunoassay of Diphtheria and Tetanus according to Ages Infect Chemother. 2012;44(2):62–66.
- Hashemi SH, Nadi E, Hajilooi M, et al. High seroprevalence of bordetella pertussis in patients with chronic obstructive pulmonary disease: a case-control study. Tanaffos. 2015;14(3):172–176.
- Blasi F, Bonanni P, Braido F, et al. The unmet need for pertussis prevention in patients with chronic obstructive pulmonary disease in the Italian context. Hum Vaccin Immunother. 2020;16(2):340–348.
- Buchy P, Badur S. Who and when to vaccinate against influenza. Int J Infect Dis. 2020;93:375–387.
- ATAGI. Australian Technical. Advisory Group on Immunisation (ATAGI). Australian Immunisation Handbook. Canberra: Australian Government Department of Health; 2019.
- Bach AT, Kang AY, Lewis J, et al. Addressing common barriers in adult immunizations: a review of interventions. Expert Rev Vaccines. 2019;18(11):1167–1185.