Abstract
Objectives: Executive functioning and emotion recognition may be impaired in disruptive youth, yet findings in oppositional defiant disorder (ODD) and conduct disorder (CD) are inconsistent. We examined these functions related to ODD and CD, accounting for comorbid attention-deficit/hyperactivity disorder (ADHD) and internalising symptoms.
Methods: We compared executive functioning (visual working memory, visual attention, inhibitory control) and emotion recognition between youth (8–18 years old, 123 boys, 55 girls) with ODD (n = 44) or CD (with/without ODD, n = 48), and healthy controls (n = 86). We also related ODD, CD, and ADHD symptom counts and internalising symptomatology to all outcome measures, as well as executive functioning to emotion recognition.
Results: Visual working memory and inhibitory control were impaired in the ODD and CD groups versus healthy controls. Anger, disgust, fear, happiness, and sadness recognition were impaired in the CD group; only anger recognition was impaired in the ODD group. Deficits were not explained by comorbid ADHD or internalising symptoms. Visual working memory was associated with recognition of all basic emotions.
Conclusions: Our findings challenge the view that neuropsychological impairments in youth with ODD/CD are driven by comorbid ADHD and suggest possible distinct neurocognitive mechanisms in CD versus ODD.
Introduction
Defiant, aggressive, and antisocial behaviours constitute significant mental problems in youth, causing considerable burden to families and society (Burke et al. Citation2002). Youth showing these behaviours are typically diagnosed with oppositional defiant disorder (ODD), characterised by angry/irritable mood and disobedience, or conduct disorder (CD), involving chronic patterns of violating basic social norms and rights of others (American Psychiatric Association Citation2013). Both disorders are highly comorbid with attention-deficit/hyperactivity disorder (ADHD) and internalising problems, with estimates of comorbidity of up to 35% for both (Loeber et al. Citation2000; Polier et al. Citation2012). It has long been recognised that disruptive behaviour may be associated with impaired executive functioning (i.e. cognitive processes necessary for performing goal-oriented behaviour), which may lead to decreased self-regulation (Hadjicharalambous and Fanti Citation2018). Moreover, disruptive behaviour has been linked to impaired facial emotion recognition (Dawel et al. Citation2012).
Still, our understanding of the specific deficits related to ODD and CD is limited. This may be in part due to the fact that ODD has often been considered as a milder form and possible precursor of CD (Matthys et al. Citation2013), with studies frequently combining both disorders into a single group. Yet, not all youth with ODD will develop CD (Burke et al. Citation2002; Rowe et al. Citation2010), and neurocognitive characteristics in CD may in part differ from those in ODD (Matthys et al. Citation2013). Currently, we lack studies directly comparing youth with ODD-only with those with CD. In addition, studies in ODD/CD have inconsistently controlled for comorbid ADHD and internalising symptoms, and even studies that did have reported mixed results (e.g. Munkvold et al. Citation2014; Griffith et al. Citation2019).
So far, impaired executive functioning has particularly been reported regarding (spatial) working memory and attentional and inhibitory control in disruptive youth (Schoemaker et al. Citation2013; Long et al. Citation2015; Carter Leno et al. Citation2018), showing associations with disruptive behaviour, independent from comorbid ADHD (Hobson et al. Citation2011; Rhodes et al. Citation2012; Johnson et al. Citation2015; Saarinen et al. Citation2015; Schoorl et al. Citation2018; Griffith et al. Citation2019). Other studies, however, found that executive functioning impairments in ODD/CD were explained by comorbid ADHD (Thorell and Wåhlstedt Citation2006; Hummer et al. Citation2011; Munkvold et al. Citation2014).
The ability to recognise emotions in others is vital for successful social behaviour (Collin et al. Citation2013). A hypersensitivity to negative emotions, such as anger, may facilitate ‘hot-tempered’ aggressive responses (Crick and Dodge Citation1994) characteristic of ODD (e.g. ‘often loses temper’), whereas a decreased sensitivity to signs of distress of others, such as sad or frightened facial expressions, relates to an empathy impairment which may particularly exist in antisocial or psychopathic populations (Blair Citation2005). Deficient emotion recognition has most often been found for fear and sadness in CD and antisocial populations (Marsh and Blair Citation2008; Kohls et al. Citation2020), but also for other basic emotions in CD (i.e. disgust, anger, and surprise; Martin-Key et al. Citation2018; Martin-Key et al. Citation2017; Sully et al. Citation2015) and in mixed ODD/CD groups (Fairchild et al. Citation2010; Bours et al. Citation2018); impairments in youth with ODD are still unclear. Emotion recognition deficits have also been reported in ADHD (Collin et al. Citation2013; Waddington et al. Citation2018), although a recent study suggested that emotion recognition deficits in youth with ADHD were specific to those with comorbid CD (Airdrie et al. Citation2018).
Emotion recognition is a complex task that requires attention and working memory (Marsh and Blair Citation2008), and it has been suggested that executive dysfunction may contribute to emotion recognition problems (Van Nieuwenhuijzen et al. Citation2017). While this has been understudied in ODD/CD, impaired sustained attention and response inhibition were associated with worse emotion recognition in youth with ADHD (Shin et al. Citation2008; Sinzig et al. Citation2008), whereas in violent offenders poorer working memory was related to worse emotion recognition (Hoaken et al. Citation2007). Although the effects of executive dysfunction are unclear, studies in CD using eye-tracking found that impaired recognition was not due to a lack of attention to the emotional stimuli (Airdrie et al. Citation2018; Martin-Key et al. Citation2018).
As for ADHD, even fewer studies have considered comorbid internalising symptoms in studies of ODD/CD, although internalising symptoms have been related to impaired attention (Micco et al. Citation2009), working memory (Moran Citation2016), and emotion recognition (Collin et al. Citation2013). However, internalising problems have also been linked to improved response inhibition (Maric et al. Citation2018; Schatz and Rostain Citation2006) and emotion recognition due to heightened threat-sensitivity (Bar-Haim et al. Citation2007), with the latter resulting in a protective role of comorbid internalising problems in individuals with CD (Short et al. Citation2016).
The current study aimed to identify possible deficits in executive functions (with a focus on visual working memory, visual attention, and inhibitory control) and emotion recognition in youth with ODD (without CD) and those with CD (mostly comorbid with ODD). We also addressed to which degree these deficits were independent of comorbid ADHD and internalising symptoms. In addition to group comparisons, we analysed dimensional measures of ODD, CD, ADHD, and internalising symptom levels to executive functioning and emotion recognition as well as associations Finally, we explored whether executive functioning was related to emotion recognition performance. Based on previous literature and theory, we expected emotion recognition to be most impaired in relation to CD.
Methods and materials
Participants
We included 178 participants with a primary diagnosis of a disruptive behaviour disorder (n = 44 with ODD, n = 48 with CD of whom n = 8 without and n = 40 with additional ODD, and n = 86 healthy controls) aged 8–18 years. Participants were recruited by nine clinical centres of child- and adolescent psychiatry across Europe (see supplementary information for site details) as part of the multicenter EU-MATRICS and EU-Aggressotype projects (http://www.matrics-project.eu; http://www.aggressotype.eu/). Youth with ODD and CD were recruited from child and adolescent psychiatry departments and patient associations throughout the Netherlands, Germany, Switzerland, Spain, the United Kingdom, and Italy. Healthy controls were recruited mainly through schools. Exclusion criteria for the current study were an IQ <80 in participants with ODD/CD, and presence of any DSM axis I diagnosis in healthy controls, and an IQ <80. Participants using psychotropic medication were required to be at a stable dose during at least two weeks prior to participation in the study, while only at the Nijmegen site participants abstained from taking stimulants on the testing day. After description of the study procedures, informed written consent was obtained from participants and/or their parents or legal guardian, or written or oral assent from children in accordance with national regulations. Each participating centre obtained ethical approval from their local ethics committee.
Clinical measures
Diagnoses of ODD, CD, and comorbid ADHD were based on the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS; Kaufman et al. Citation1997), a well-validated semi-structured interview with participants and their parents based on the DSM-IV. The K-SADS was also used to verify the absence of a DSM axis I diagnosis in healthy controls. We used the K-SADS based number of symptoms of ODD (0–8), CD (0–15), and ADHD (inattention, 0–9 and hyperactivity, 0–9) as continuous measures. T-scores from the broadband internalising scale (anxious-depressed, withdrawn-depressed, and somatic complaints scores) of the Child Behaviour Checklist were used as a continuous measure of internalising problems (Achenbach and Rescorla Citation2001). IQ was estimated based on the block design, similarities, vocabulary, and picture completion subscales of the Wechsler Intelligence Scale for Children (Wechsler Citation2002). Medication use was assessed by parental report.
Neuropsychological testing
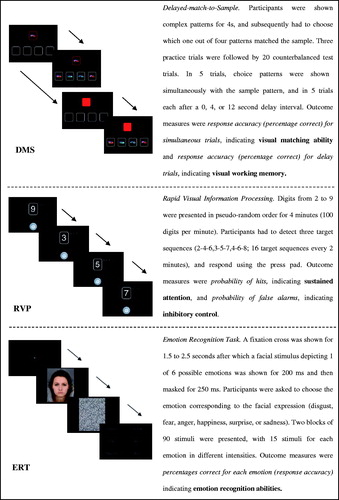
We included three tasks from the Cambridge Neuropsychological Test Automated Battery (CANTAB; Cambridge Cognition, Citation2015), a computerised programme with internal consistency coefficients ranging from .73 to .95 and good validity (Luciana Citation2003): the Delayed-match-to-Sample task (a visual working memory task), the Rapid Visual Information Processing task (a 4-minute visual continuous performance test to assess attentional processes), and the Emotion Recognition Task. See for detailed task descriptions. For the Delayed-match-to-Sample task, our main outcome measure was (i) response accuracy for delay trials (i.e. percentage correct), indicating visual working memory. To investigate if possible group differences in visual working memory were due to attentional or perceptual abilities, we also included (ii) response accuracy for simultaneous trials (i.e. percentage correct), indicating visual matching ability. Rapid Visual Information Processing outcome measures were (i) probability of hits, assessing sustained attention, and (ii) probability of false alarms, assessing inhibitory control (Sahakian et al. Citation1989; Shang et al. Citation2013). For the Emotion Recognition Task, we used response accuracy (i.e. percentage correct) for each emotion (disgust, fear, anger, happiness, surprise, sadness).
Statistical analyses
All analyses were performed using SPSS, release 25 (SPSS, Chicago, IL), using an alpha level of 0.05, unless otherwise stated. The CANTAB outcome measures were checked for outliers (interpreted as indicative of insufficient task effort) and participants were excluded when z-scores were ≥|3.0| on one or more outcome measures of the Delayed-match-to-Sample task (13 participants excluded) and Rapid Visual Information Processing task (6 participants excluded). On the Emotion Recognition Task, participants were excluded when z-scores were ≥|3.0| for at least two emotions (none excluded). As emotions were displayed in random order, we considered an extreme z-score of only one emotion not indicative of insufficient task effort. Raw scores were used as outcome measures in all analyses.
Sample characteristics
Overall differences between ODD, CD, and the healthy control group in age, IQ, number of ODD, CD, and ADHD (inattention and hyperactivity) symptoms, and the CBCL internalising T-score were tested through univariate analyses of variance (ANOVAs). Significant results were followed-up with planned contrasts: all ODD/CD subjects versus controls; ODD (without CD) versus controls; CD (with possible comorbid ODD allowed) vs controls; and ODD versus CD. Differences regarding sex, number of participants with ADHD, and number of participants with clinical levels of internalising symptoms were tested with Chi-square (χ2) tests.
Group comparisons between cases and controls
Repeated measures analyses of covariance (ANCOVAs) were performed separately for the Delayed-match-to-Sample and Emotion Recognition Task, with task condition (i.e. simultaneous/delay condition and emotion, respectively) as within-subject’s variable and diagnostic group (controls; ODD; CD) as between-subject variable. In the case of interactions between task condition and diagnostic group, we subsequently performed univariate analyses for each task condition. For the Rapid Visual Information Processing task, we used a multivariate ANCOVA for the two outcome measures. If the multivariate result was significant, we also interpreted univariate effects.
Significant (univariate) effects were followed by planned contrasts: all ODD/CD versus controls; controls versus ODD; controls vs CD; and ODD versus CD. Age and IQ were included as covariates of non-interest in all analyses. To correct for comorbid ADHD (inattention and hyperactivity) or internalising symptoms we conducted similar additional analyses adding these factors as a covariate (in separate models; described in more detail in the supplementary information).
We corrected for multiple testing by using a corrected alpha-level using the effective number of independent tests (Nyholt Citation2004), resulting in an alpha-level of 0.021 (2.4 effective tests based on 3 original tests; i.e. 2 repeated measures and 1 multivariate ANCOVA). Effect sizes are reported as partial η2, expressing the proportion of explained variance for each variable correcting for the effects of the other variables included, which may be considered as small between 0.01–0.058, medium between 0.059–0.138 and large when >0.139 (Cohen Citation1988).
Dimensional analyses of symptoms
Within-cases (because of the near-zero scores in controls) regression analyses were performed to investigate the contributions of ODD, CD, ADHD (inattention and hyperactivity) counts and internalising symptom severity to executive functioning and emotion recognition. We first specified 2 alternate stepwise models to determine the independent effects of ODD, CD and ADHD counts. In both models, age and IQ were entered in step 1. In the uncorrected model, ODD and CD symptom counts were entered in step 2. In the corrected model, ADHD (inattention and hyperactivity) counts were entered in step 2, and ODD and CD counts in step 3. In the same way, we tested internalising symptoms in separate models (because of a lower sample size). Corrected alpha-levels were again based on the effective number of independent tests (Nyholt Citation2004), here resulting in an alpha-level of 0.0054 (9.2 effective tests; original number of 10 tests).
Association between executive functioning and emotion recognition
To investigate whether Delayed-match-to-Sample (visual matching ability, visual working memory) and Rapid Visual Information Processing (sustained attention, inhibitory control) measures predicted Emotion Recognition, we conducted multiple regression analyses in the combined ODD/CD group. Individual models were specified for each emotion as executive functioning might differentially contribute to recognition of different emotions, with all predictors entered simultaneously to account for each other’s effects (correlations between Delayed-match-to-Sample and Rapid Visual Information Processing task measures were between r = −.25, p = 0.021 and r = .23, p = 0.033). The corrected alpha-level was 0.0096 (5.2 effective tests based on an original number of 6 tests).
Sensitivity analyses
For all case–control as well as within-case analyses, sensitivity analyses were performed adding sex, site, and psychotropic medication use (participants from Nijmegen who were asked to abstain from stimulants were included as not using medication) simultaneously as covariates (in addition to age and IQ) to the models.
Results
All reported results were controlled for age and IQ, and also remained significant after adjusting for sex, site differences, and medication use, unless otherwise stated (see sensitivity analyses in the supplementary information for more details).
Sample characteristics
shows the sample characteristics. The control group consisted of significantly less boys than the CD group, had a higher IQ compared to the full ODD/CD group and ODD and CD groups separately (although IQ was in the normal range in all groups). Although most participants with CD also had a diagnosis of ODD, the ODD group showed more ODD and ADHD inattention symptoms than the CD group. The groups did not differ significantly in the percentage of individuals with a comorbid ADHD diagnosis, which was 52% in the ODD and 37% in CD group. In the ODD and CD groups, respectively 45% and 57% of the participants were using psychotropic medication, mostly stimulants and antipsychotics.
Table 1. Sample characteristics.
Group comparisons between cases and controls
See supplementary information for statistics regarding the additional models including ADHD symptoms or internalising symptom severity.
Delayed-match-to-Sample
The repeated measures ANCOVA yielded significant interactions between diagnostic group and task condition (F(2,160) = 7.5, p < 0.021; adjusted alpha-level) and between age and task condition, (F(1,160) = 6.87, p < 0.021), whereas there was no effect of IQ. Follow-up univariate ANCOVAs for each task condition were performed (). The total ODD/CD group as well as the separate ODD and CD groups showed worse visual working memory (i.e. lower % correct on the delay conditions), compared to the control group, with a significant effect of age (F(1,160) = 13.03, p < 0.021). Although there was no difference between the total ODD/CD group and the control group regarding visual matching ability, performance was significantly worse in the CD group compared to the control and ODD groups. However, group interacted with age, suggesting worse performance particularly in younger participants with CD compared to the ODD and healthy control groups (ODD: visual matching ability 100%, CD: r = 0.35, p = 0.017, healthy controls: r = 0.25, not significant). Visual matching was > 95% in all three groups, indicating a ceiling effect of the task. All effect sizes were in the medium range.
Table 2. Univariate results of executive functioning and emotion recognition followed by planned contrasts.
Group effects remained significant when ADHD symptoms/diagnosis or internalising symptoms were added to the model.
Rapid visual information processing
There was an overall group effect across the Rapid Visual Information Processing outcome measures (F(4,312) = 3.11, p < 0.021; Wilk’s Λ=.925, partial η2= .038), as well as a main effect of age (F(2, 156) = 4.32, p < 0.021; Wilk’s Λ=.945, partial η2= .055) but not of IQ, see for follow-up univariate analyses. The total ODD/CD group as well as the ODD and CD groups separately had significantly worse inhibitory control (i.e. higher probability of false alarms) than the control group, with small-to-medium effects. There was no difference between the ODD and CD groups. No group differences were found for sustained attention, as expressed by the probability of hits.
ADHD symptoms were not associated with overall performance on the Rapid Visual Information Processing task. Internalising symptom severity was related to overall RVP performance in the multivariate ANCOVA. The main group difference became insignificant, as well as the univariate group difference on inhibitory control; there was no association with internalising symptom severity itself.
Emotion recognition task
Type of emotion interacted with diagnostic group (F(10, 845) = 2.49, p < 0.021, adjusted alpha-level) and age (F(5, 845) = 3.86, < 0.021) in the repeated measures ANCOVA. There was no main effect of IQ. Follow-up univariate analyses and contrasts () indicated that the total ODD/CD group performed worse (i.e. lower % correct) in recognising fear, disgust, anger, happiness, and sadness (but not surprise) compared to the control group, with medium-to-large effects. Notably, while the ODD group performed only worse in recognising anger compared to the control group with a small effect, the CD group was worse in recognising all of these five emotions with effects in the medium to large range. Moreover, the CD group performed significantly worse than the ODD group in the recognition of disgust and fear, with small-to-medium effects.
Main effects of age were observed for disgust (F(1,169) = 21.16, p < 0.001), anger (F(1,169) = 5.61, p = 0.019), and sadness (F(1,169) = 37.73, p < .001), but not fear. For happiness and surprise, diagnostic group interacted with age, suggesting worse performance particularly in younger participants with CD (happiness: ODD: r = 0.30, p = 0.54, CD: r = 0.48, p = 0.001, controls: r = 0.21, p = 0.055, surprise: ODD: r = 0.31, p = 0.45, CD: r = 0.56, p < 0.001, controls: r = 0.22, p = 0.041). Surprise also interacted with IQ (ODD: r = −0.10, p = 0.51, CD: r = 0.21, p = 0.15, controls: r = −0.15, p = 0.59), suggesting worse performance in the CD group with lower IQ.
ADHD hyperactivity symptoms were related to emotion recognition in the repeated measures ANOVA, but the group effect remained significant. ADHD inattention symptoms and internalising symptom severity were not associated with emotion recognition
Dimensional analyses of symptoms
All described effects were significant based on the corrected alpha-level of 0.0054, see (ADHD inattention and hyperactivity counts) and Supplementary Table S2 (internalising symptom severity) for statistics.
Table 3. Multiple regression analyses of ODD, CD and ADHD (inattention and hyperactivity) symptom counts as predictors of executive functioning and emotion recognition in ODD/CD cases (N = 86).
ODD, CD, and ADHD symptoms
Delayed-match-to-Sample. Neither ODD, CD, nor ADHD (inattention and hyperactivity) symptom counts were significantly associated with visual matching ability and visual working memory. Higher numbers of CD symptoms where nominally significantly (p < 0.05) associated with lower visual matching ability in the model uncorrected for ADHD symptom counts, showing a small effect size.
Rapid Visual Information Processing. Higher ODD symptom counts were significantly related to worse sustained attention when corrected for ADHD (and nominally significant in the uncorrected model), representing a moderate-to-large effect. After accounting for sex, site differences, and medication use the association became nominally significant. CD counts and ADHD inattention and hyperactivity counts were not significantly associated with sustained attention (albeit effects of CD counts resembled those of ODD counts). None of the symptom dimensions were associated with inhibitory control.
Emotion Recognition Task. Higher CD counts were significantly associated with worse recognition only of disgust, representing a large effect, but not with other emotions before and after adjusting for ADHD symptoms. In addition, there were nominally significant associations between higher ODD symptom counts and poorer recognition of disgust, fear, and sadness, with effects in the small-to-medium range. Higher hyperactivity counts were significantly related to worse recognition of anger, whereas inattention counts were related to better recognition of anger, both with a large effect ().
Table 4. Multiple regression analyses of ODD/CD symptoms and internalising symptom severity as predictors of executive functioning and emotion recognition (N = 82).
Internalising symptom severity
Internalising symptom severity was not significantly associated with any of the outcome measures. However, there was a nominally significant association of higher internalising scores with better visual matching ability and with worse sustained attention, showing medium sized effects.
Association between executive functioning and emotion recognition
As shown in , only better visual working memory was independently related to better recognition of all six emotions, with effects in the medium-to-large range. Furthermore, better inhibitory control was nominally significantly associated with better recognition of disgust with a medium effect size. Sustained attention was not significantly related to emotion recognition.
Table 5. Multiple regression analyses of executive functioning measures as predictors of emotion recognition in youth with ODD/CD (N = 85).
Discussion
The aim of this study was to increase our understanding of executive functioning and emotion recognition in youth with ODD and/or CD by exploring if CD (mostly with comorbid ODD) was associated with similar or unique deficits compared to ODD, while accounting for ADHD and internalising symptoms. We found deficits in visual working memory and inhibitory control both in ODD and CD compared to healthy controls. A key finding was that impaired emotion recognition compared to controls was largely specific to the group with CD (i.e. of fear, disgust, happiness, and sadness; anger recognition was also impaired in ODD without CD). Furthermore, visual working memory was related to worse facial emotion recognition across all six basic emotions. Effect sizes were mostly in the medium-to-large range. Notably, impairments were independent from comorbid ADHD or internalising symptoms. Our results challenge the view that comorbid ADHD drives impairments in neuropsychological functioning in youth with disruptive disorders and suggest possible partly distinct neurocognitive correlates of CD versus ODD.
Our finding of impaired visual working memory both in youth with ODD and those with CD is in line with other studies which found various types of impaired working memory in ODD/CD (Ogilvie et al. Citation2011; Saarinen et al. Citation2015). However, levels of ODD and CD symptoms were not dimensionally related to visual working memory in our study, perhaps due to the restricted range of symptom counts in cases-only analyses. Participants with CD had worse visual matching compared to the healthy control and ODD groups, but as mean performance was still 96% (indicating a ceiling effect), this might not be relevant.
Impaired inhibitory control in the ODD and CD groups was also found in previous studies in ODD/CD (Hobson et al. Citation2011; Schoemaker et al. Citation2013; Noordermeer et al. Citation2015). However, when accounting for comorbid internalising symptom severity, our group differences in inhibitory control disappeared, even though internalising symptom severity itself was not associated with inhibitory control.
Internalising symptom severity was neither (positively) associated with other executive functioning measures. Thus, we did not find support for a protective effect of comorbid internalising symptoms, unlike a study in ADHD showing that the presence of comorbid anxiety may ameliorate inhibition deficits (Schatz and Rostain Citation2006). Similarly, another study found that more ODD negative affect symptoms, which can be distinguished from oppositional and antagonistic behaviour symptoms of ODD, were related to better response inhibition in children (Griffith et al. Citation2019). Our null finding may in part be explained by the restricted range of comorbid internalising scores in our sample. Performance may also depend on task properties. Go-no-go and stop signal tasks, often used to measure response inhibition, specifically focus on inhibition of a prepotent response, whereas continuous performance tasks as used in the current study do not induce a prepotent response and may thus rely more on resistance to distractors (Friedman and Miyake Citation2004).
Unlike in previous case–control studies (Baving et al. Citation2006; Hobson et al. Citation2011), sustained attention was not impaired in our participants with ODD and/or CD compared to healthy controls, despite our medium-to-large-sized association with the number of ODD symptoms. Possibly, only the most severe cases show attentional difficulties.
Impaired emotion recognition across a variety of emotions, with strongest effects for fear and disgust but also for anger, happiness, and sadness, may point to a global deficit in emotion recognition in CD (Bowen et al. Citation2013; Sully et al. Citation2015), thus not exclusively involving negative emotions. Our results are consistent with previous findings of impaired recognition of these emotions in CD (Sully et al. Citation2015; Martin-Key et al. Citation2017, Citation2018), and with a meta-analysis identifying a global recognition deficit, with effect sizes for fear and sadness trending towards being larger than for those other emotions in antisocial populations (Dawel et al. Citation2012). Regarding happiness, our results suggest that younger children with CD are more impaired compared to controls than older participants. As happiness recognition develops earliest and with greatest accuracy (Herba and Phillips Citation2004), our results may suggest a developmental delay in the CD group. Although no overall impairment was found, a similar pattern was observed for surprise recognition. Our results indicate more severe deficits in CD than ODD, in line with the suggestion that children with more severe instrumental antisocial behaviours as seen in CD are less sensitive to aversive cues, such as negative facial expressions, and are therefore less able to view the negative consequences of their inappropriate behaviours (classical aversive conditioning, e.g. learning to link hitting someone with the victim’s subsequent distress; Blair Citation2005; Matthys et al. Citation2013).
Only the recognition of anger was impaired in ODD (but also in CD). Although this finding is not in line with a hypersensitivity to negative emotions (Crick and Dodge Citation1994), it is consistent with results from previous research (Fairchild et al. Citation2009, Citation2010, Sully et al. Citation2015). Unlike fear and sadness, displays of anger have been argued not to act as stimuli for aversive conditioning but rather as important signals informing the observer to stop the current behaviour, with dysfunctional anger recognition leading to impaired modulation of social behaviour (e.g. Blair Citation2005). Impaired recognition of anger may thus have clinical implications and perhaps explain why children with ODD/CD are more readily involved in conflicts. Hyperactivity–impulsivity symptoms were also independently associated with worse anger recognition, consistent with several studies suggesting that impaired anger recognition may play a role in the emotion-regulation deficits of children with ADHD (Pelc et al. Citation2006; Chronaki et al. Citation2015). We have no good explanation for the surprising association of inattentive symptoms with better anger recognition in our study, but are aware of one study that also found this (although authors did not elaborate on this finding; Tehrani-Doost et al. Citation2017).
Another central finding in this study was the association between poorer visual working memory and facial emotion recognition. It has been suggested that working memory is integral to emotion recognition (Adolphs Citation2002; Phillips et al. Citation2008) and may be required to link the features of facial expressions with knowledge about the meaning of those features and the emotion they represent (Adolphs Citation2002; Haxby et al. Citation2002). However, part of the association may possibly be attributed to task difficulty as the need for explicit verbal labelling of emotions also taxes working memory (Phillips et al. Citation2008). We found no support for a relation between sustained attention and emotion recognition, in line with results of eye-tracking studies in CD (Airdrie et al. Citation2018; Martin-Key et al. Citation2018).
Important strengths of the current study were (i) the inclusion of a sizeable proportion of children and adolescents (8–18 years) with a diagnosis of CD, (ii) a comparison of youth with ODD without CD and those with CD, (iii) investigating both comorbid inattention and hyperactivity dimensions of ADHD as well as internalising symptoms, and (iv) a joint analysis of executive functioning and emotion recognition tasks. There were also some limitations to the current study. First, almost all participants in the CD group also had ODD; however, youth with only CD rarely exist. Second, to better disentangle effects of ADHD and internalising symptomatology, we would need larger sample sizes with sufficient symptom variation. Therefore, our findings regarding internalising symptoms may best be considered as preliminary. Finally, cases consisted of more males compared to controls, we investigated a wide age range, and a substantial proportion used psychotropic medication. However, we controlled for medication use, and our main findings were independent from sex, age, IQ and site differences.
In conclusion, our study supports deficits in executive functioning and emotion recognition in youth with ODD and/or CD, independent from comorbid ADHD and internalising symptoms. While impairments in executive function were found to be similar in ODD and CD (with ODD), emotion recognition deficits appeared to be largely specific to youth with (comorbid) CD. Moreover, impaired visual working memory was associated with impaired emotion recognition ability. Overall, youth with disruptive behaviour disorders may show behavioural problems due to deficits in multiple neurocognitive processes that relate to self-regulation capacity and emotional dysregulation, as well as insensitivity to emotional expressions of others, which may be especially relevant in CD. Clinically, our results could imply that youth with ODD without CD might benefit from treatment aimed at improving anger recognition and self-control, whilst treatment for CD could target pervasive emotion recognition problems, thus contributing to personalised treatment approaches.
Future research may distinguish between various subdimensions of ODD (negative affect and oppositional-antagonistic behaviours; Leadbeater and Homel Citation2015) and of CD (callous-unemotional, grandiose-manipulative, daring-impulsive traits; Salekin Citation2016), and focus on the mechanisms related to emotion recognition deficits in ODD and CD. The neuropsychological correlates of disruptive behaviours may also be investigated in the context of other frequently comorbid neurodevelopmental conditions such as tic or autism spectrum disorders (Bours et al. Citation2018; Thériault et al. Citation2018).
Statement of interest
T Banaschewski served in an advisory or consultancy role for Actelion, Lundbeck, Medice, Neurim Pharmaceuticals, Oberberg GmbH, Shire, and Infectopharm. He received conference support or speaker’s fee by Lilly, Medice, and Shire. He received royalities from Hogrefe, Kohlhammer, CIP Medien, Oxford University Press; the present work is unrelated to these relationships. C Arango has been a consultant to or has received honoraria or grants from Acadia, Ambrosseti, Caja Navarra, CIBERSAM, Fundación Alicia Koplowitz, Forum, Instituto de Salud Carlos III, Gedeon Richter, Janssen Cilag, Lundbeck, Merck, Ministerio de Ciencia e Innovación, Ministerio de Sanidad, Ministerio de Economía y Competitividad, Mutua Madrileña, Otsuka, Roche, Servier, Shire, Schering Plough, Sumitomo Dainippon Pharma, Sunovio and Takeda. D Brandeis serves as an unpaid scientific advisor for an EU-funded Neurofeedback trial unrelated to the present work. JC Glennon has acted as a consultant for Boehringer Ingelheim GmbH. B Franke received an educational speaking fee from Shire and Medice. JK Buitelaar has been consultant to/member of advisory board of and/or speaker for Janssen Cilag BV, Eli Lilly, Bristol-Myer Squibb, Shering Plough, UCB, Shire, Novartis and Servier. He is not an employee of any of these companies, nor a stock shareholder of any of these companies. He has no other financial or material support, including expert testimony, patents, and royalties. UME Schulze serves as an unpaid ethics advisor for two EU-funded projects unrelated to the present work. She has received a speaker’s fee from Shire. The other authors do not report any biomedical financial interests or potential conflicts of interest.
Supplemental information
Download MS Word (39.2 KB)Acknowledgements
This paper reflects only the authors’ views, and the European Union is not liable for any use that may be made of the information contained therein.
Additional information
Funding
References
- Achenbach TM, Rescorla LA. 2001. Manual for the ASEBA school-age forms & profiles: an integrated system of multi-informant assessment. Burlington (VT): University of Vermont, Research Center for Children, Youth, & Families.
- Adolphs R. 2002. Recognizing emotion from facial expressions: psychological and neurological mechanisms. Behav Cogn Neurosci Rev. 1(1):21–62.
- Airdrie JN, Langley K, Thapar A, van Goozen SHM. 2018. Facial emotion recognition and eye gaze in attention-deficit/hyperactivity disorder with and without comorbid conduct disorder. J Am Acad Child Adolesc Psychiatry. 57(8):561–570.
- American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders. 5th ed. Washington (DC): American Psychiatric Association.
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. 2007. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 133(1):1–24.
- Baving L, Rellum T, Laucht M, Schmidt MH. 2006. Children with oppositional-defiant disorder display deviant attentional processing independent of ADHD symptoms. J Neural Transm (Vienna). 113(5):685–693.
- Blair RJR. 2005. Responding to the emotions of others: dissociating forms of empathy through the study of typical and psychiatric populations. Conscious Cogn. 14(4):698–718.
- Bours CCAH, Bakker-Huvenaars MJ, Tramper J, Bielczyk N, Scheepers F, Nijhof KS, Baanders AN, Lambregts-Rommelse NNJ, Medendorp P, Glennon JC, et al. 2018. Emotional face recognition in male adolescents with autism spectrum disorder or disruptive behavior disorder: an eye-tracking study. Eur Child Adolesc Psychiatry. 27(9):1143–1157.
- cBowen KL, Morgan JE, Moore SC, van Goozen SH. 2014. Young offenders’ emotion recognition dysfunction across emotion intensities: explaining variation using psychopathic traits, conduct disorder and offense severity. J Psychopathol Behav Assess. 36(1):60–73.
- Burke JD, Loeber R, Birmaher B. 2002. Oppositional defiant disorder and conduct disorder: a review of the past 10 years, part II. J Am Acad Child Adolesc Psychiatry. 41(11):1275–1293.
- Burke JD, Loeber R, Mutchka JS, Lahey BB. 2002. A question for DSM-V: which better predicts persistent conduct disorder – delinquent acts or conduct symptoms? Criminal Behav Ment Health. 12(1):37–52.
- CANTAB® [Cognitive assessment software]. Cambridge Cognition 2015. All rights reserved. www.cantab.com.
- Carter Leno V, Chandler S, White P, Pickles A, Baird G, Hobson C, Smith AB, Charman T, Rubia K, Simonoff E. 2018. Testing the specificity of executive functioning impairments in adolescents with ADHD, ODD/CD and ASD. Eur Child Adolesc Psychiatry. 27(7):899–908.
- Chronaki G, Garner M, Hadwin JA, Thompson MJJ, Chin CY, Sonuga-Barke EJS. 2015. Emotion-recognition abilities and behavior problem dimensions in preschoolers: Evidence for a specific role for childhood hyperactivity. Child Neuropsychology. 21(1):25–40.
- Cohen J. 1988. Statistical power analysis for the behavioral sciences. San Diego (CA): Academic Press.
- Collin L, Bindra J, Raju M, Gillberg C, Minnis H. 2013. Facial emotion recognition in child psychiatry: a systematic review. Res Dev Disabil. 34(5):1505–1520.
- Crick NR, Dodge KA. 1994. A review and reformulation of social information-processing mechanisms in children’s social adjustment. Psychol Bull. 115(1):74–101.
- Dawel A, O’Kearney R, McKone E, Palermo R. 2012. Not just fear and sadness: meta-analytic evidence of pervasive emotion recognition deficits for facial and vocal expressions in psychopathy. Neurosci Biobehav Rev. 36(10):2288–2304.
- Fairchild G, Stobbe Y, Van Goozen SHM, Calder AJ, Goodyer IM. 2010. Facial expression recognition, fear conditioning, and startle modulation in female subjects with conduct disorder. Biol Psychiatry. 68(3):272–279.
- Fairchild G, Van Goozen SH, Calder AJ, Stollery SJ, Goodyer IM. 2009. Deficits in facial expression recognition in male adolescents with early‐onset or adolescence‐onset conduct disorder. J Child Psychol Psychiatry. 50(5):627–636.
- Friedman NP, Miyake A. 2004. The relations among inhibition and interference control functions: a latent-variable analysis. J Exp Psychol Gen. 133(1):101–135.
- Griffith SF, Arnold DH, Rolon-Arroyo B, Harvey EA. 2019. Neuropsychological predictors of ODD symptom dimensions in young children. J Clin Child Adolesc Psychol. 48(1):80–92.
- Hadjicharalambous MZ, Fanti KA. 2018. Self regulation, cognitive capacity and risk taking: investigating heterogeneity among adolescents with callous-unemotional traits. Child Psychiatry Hum Dev. 49(3):331–340.
- Haxby JV, Hoffman EA, Gobbini MI. 2002. Human neural systems for face recognition and social communication. Biol Psychiatry. 51(1):59–67.
- Herba C, Phillips M. 2004. Annotation: Development of facial expression recognition from childhood to adolescence: behavioural and neurological perspectives. J Child Psychol Psychiatry. 45(7):1185–1198.
- Hoaken PNS, Allaby DB, Earle J. 2007. Executive cognitive functioning and the recognition of facial expressions of emotion in incarcerated violent offenders, non-violent offenders, and controls. Aggr Behav. 33(5):412–421.
- Hobson CW, Scott S, Rubia K. 2011. Investigation of cool and hot executive function in ODD/CD independently of ADHD. J Child Psychol Psychiatry. 52(10):1035–1043.
- Hummer TA, Kronenberger WG, Wang Y, Dunn DW, Mosier KM, Kalnin AJ, Mathews VP. 2011. Executive functioning characteristics associated with ADHD comorbidity in adolescents with disruptive behavior disorders. J Abnorm Child Psychol. 39(1):11–19.
- Johnson VA, Kemp AH, Heard R, Lennings CJ, Hickie IB. 2015. Childhood-versus adolescent-onset antisocial youth with conduct disorder: Psychiatric illness, neuropsychological and psychosocial function. PLoS One. 10(4):e0121627.
- Kaufman J, Birmaher B, Brent D, Rao UMA, Flynn C, Moreci P, Williamson D, Ryan N. 1997. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 36(7):980–988.
- Kohls G, Baumann S, Gundlach M, Scharke W, Bernhard A, Martinelli A, Ackermann K, Kersten L, Prätzlich M, Oldenhof H, et al. 2020. Investigating sex differences in emotion recognition, learning, and regulation among youths with conduct disorder. J Am Acad Child Adolesc Psychiatry. 59(2):263–273.
- Leadbeater BJ, Homel J. 2015. Irritable and defiant sub-dimensions of ODD: their stability and prediction of internalizing symptoms and conduct problems from adolescence to young adulthood. J Abnorm Child Psychol. 43(3):407–421.
- Loeber R, Burke J, Lahey B, Winters A, Zera M. 2000. Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry. 39(12), 1468–1484.
- Long EC, Hill J, Luna B, Verhulst B, Clark DB. 2015. Disruptive behavior disorders and indicators of disinhibition in adolescents: The BRIEF-SR, anti-saccade task, and D-KEFS color-word interference test. J Adolesc. 44:182–190.
- Luciana M. 2003. Practitioner review: Computerized assessment of neuropsychological function in children: clinical and research applications of the Cambridge Neuropsychological Testing Automated Battery (CANTAB). J Child Psychol Psychiatry. 44(5):649–663.
- Maric M, Bexkens A, Bögels SM. 2018. Is clinical anxiety a risk or a protective factor for executive functioning in youth with ADHD? A meta-regression analysis. Clin Child Fam Psychol Rev. 21(3):340–353.
- Marsh AA, Blair RJR. 2008. Deficits in facial affect recognition among antisocial populations: a meta-analysis. Neurosci Biobehav Rev. 32(3):454–465.
- Martin-Key NA, Graf EW, Adams WJ, Fairchild G. 2018. Facial emotion recognition and eye movement behaviour in conduct disorder. J Child Psychol Psychiatry. 59(3):247–257.
- Martin-Key N, Brown T, Fairchild G. 2017. Empathic accuracy in male adolescents with conduct disorder and higher versus lower levels of callous-unemotional traits. J Abnorm Child Psychol. 45(7):1385–1397.
- Matthys W, Vanderschuren LJMJ, Schutter DJLG. 2013. The neurobiology of oppositional defiant disorder and conduct disorder: Altered functioning in three mental domains. Dev Psychopathol. 25(1):193–207.
- Micco JA, Henin A, Biederman J, Rosenbaum JF, Petty C, Rindlaub LA, Murphy M, Hirshfeld-Becker DR. 2009. Executive functioning in offspring at risk for depression and anxiety. Depress Anxiety. 26(9):780–790.
- Moran TP. 2016. Anxiety and working memory capacity: a meta-analysis and narrative review. Psychol Bull. 142(8):831–864.
- Munkvold LH, Manger T, Lundervold AJ. 2014. Conners continuous performance test (CCPT-II) in children with ADHD, ODD, or a combined ADHD/ODD diagnosis. Child Neuropsychol. 20(1):106–126.
- Noordermeer SDS, Luman M, Buitelaar JK, Hartman CA, Hoekstra PJ, Franke B, Faraone SV, Heslenfeld DJ, Oosterlaan J. 2015. Neurocognitive deficits in attention-deficit/hyperactivity disorder with and without comorbid oppositional defiant disorder. J Atten Disord. pii: 1087054715606216. [Epub ahead of print].
- Nyholt DR. 2004. A simple correction for multiple testing for single-nucleotide polymorphisms in linkage disequilibrium with each other. Am J Hum Genet. 74(4):765–769.
- Ogilvie JM, Stewart AL, Chan RCK, Shum DHK. 2011. Neuropsychological measures of executive function and antisocial behavior: a meta-analysis. Criminology. 49(4):1063–1107.
- Pelc K, Kornreich C, Foisy ML, Dan B. 2006. Recognition of emotional facial expressions in attention-deficit hyperactivity disorder. Pediatr Neurol. 35(2):93–97.
- Phillips LH, Channon S, Tunstall M, Hedenstrom A, Lyons K. 2008. The role of working memory in decoding emotions. Emotion. 8(2):184–191.
- Polier GG, Vloet TD, Herpertz-Dahlmann B, Laurens KR, Hodgins S. 2012. Comorbidity of conduct disorder symptoms and internalizing problems in children: Investigating a community and a clinical sample. Eur Child Adolesc Psychiatry. 21(1):31–38.
- Rhodes SM, Park J, Seth S, Coghill DR. 2012. A comprehensive investigation of memory impairment in attention deficit hyperactivity disorder and oppositional defiant disorder. J Child Psychol Psychiatry. 53(2):128–137.
- Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. 2010. Developmental pathways in oppositional defiant disorder and conduct disorder. J Abnorm Psychol. 119(4):726–738.
- Saarinen S, Fontell T, Vuontela V, Carlson S, Aronen ET. 2015. Visuospatial working memory in 7- to 12-year-old children with disruptive behavior disorders. Child Psychiatry Hum Dev. 46(1):34–43.
- Sahakian B, Jones G, Levy R, Gray J, Warburton D. 1989. The effects of nicotine on attention, information processing, and short-term memory in patients with dementia of the Alzheimer type. Br J Psychiatry. 154(6):797–800.
- Salekin RT. 2016. Psychopathy in childhood: toward better informing the DSM-5 and ICD-11 conduct disorder specifiers. Personal Disord. 7(2):180–191.
- Schatz DB, Rostain AL. 2006. ADHD with comorbid anxiety. J Atten Disord. 10(2):141–149.
- Schoemaker K, Mulder H, Deković M, Matthys W. 2013. Executive functions in preschool children with externalizing behavior problems: a meta-analysis. J Abnorm Child Psychol. 41(3):457–471.
- Schoorl J, van Rijn S, de Wied M, van Goozen S, Swaab H. 2018. Boys with oppositional defiant disorder/conduct disorder show impaired adaptation during stress: an executive functioning study. Child Psychiatry Hum Dev. 49(2):298–307.
- Shang CY, Wu YH, Gau SS, Tseng WY. 2013. Disturbed microstructural integrity of the frontostriatal fiber pathways and executive dysfunction in children with attention deficit hyperactivity disorder. Psychol Med. 43(5):1093–1107.
- Shin DW, Lee SJ, Kim BJ, Park Y, Lim SW. 2008. Visual attention deficits contribute to impaired facial emotion recognition in boys with attention-deficit/hyperactivity disorder. Neuropediatrics. 39(06):323–327.
- Short RM, Sonuga‐Barke EJ, Adams WJ, Fairchild G. 2016. Does comorbid anxiety counteract emotion recognition deficits in conduct disorder? J Child Psychol Psychiatr. 57(8):917–926.
- Sinzig J, Morsch D, Lehmkuhl G. 2008. Do hyperactivity, impulsivity and inattention have an impact on the ability of facial affect recognition in children with autism and ADHD? Eur Child Adolesc Psychiatry. 17(2):63–72.
- Sully K, Sonuga-Barke EJS, Fairchild G. 2015. The familial basis of facial emotion recognition deficits in adolescents with conduct disorder and their unaffected relatives. Psychol Med. 45(9):1965–1975.
- Tehrani-Doost M, Noorazar G, Shahrivar Z, Banaraki AK, Beigi PF, Noorian N. 2017. Is emotion recognition related to core symptoms of childhood ADHD? J Can Acad Child Adolesc Psychiatry. 26(1):31–38.
- Thériault MCG, Bécue JC, Lespérance P, Chouinard S, Rouleau GA, Richer F. 2018. Oppositional behavior and longitudinal predictions of early adulthood mental health problems in chronic tic disorders. Psychiatry Res. 2018;266:301–308.
- Thorell LB, Wåhlstedt C. 2006. Executive functioning deficits in relation to symptoms of ADHD and/or ODD in preschool children. Inf Child Develop. 15(5):503–518.
- Van Nieuwenhuijzen M, Van Rest MM, Embregts PJCM, Vriens A, Oostermeijer S, Van Bokhoven I, Matthys W. 2017. Executive functions and social information processing in adolescents with severe behavior problems. Child Neuropsychology. 23(2):228–241.
- Waddington F, Hartman C, de Bruijn Y, Lappenschaar M, Oerlemans A, Buitelaar J, Franke B, Rommelse N. 2018. Visual and auditory emotion recognition problems as familial cross-disorder phenomenon in ASD and ADHD. Eur Neuropsychopharmacol. 28(9):994–1005.
- Wechsler D. 2002. WISC-III Handleiding. London: The Psychological Corporation.