Abstract
Introduction
Polysubstance use is a prevalent substance use pattern with adverse effects on psychological distress and diminished treatment outcomes. Although polysubstance use often dominates clinical practice, the trajectories of substance use and psychological distress in the initial phase of treatment have been subject to few empirical investigations.
Material and Methods
141 patients initiating inpatient or outpatient treatment for substance use disorder were followed for 12 months, using multiple assessments. We assessed psychological distress and substance use at baseline and at 3-, 6-, and 12-month follow-up visits. We implemented an SMS tracker of substance use during follow-up to reduce the impact of missing data.
Results
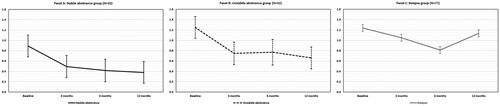
Stable abstinence was associated with a lower baseline SCL-90-R score, as well as a more rapid symptomatic decline during the first 3 months of abstinence. Unstable abstinence was associated with higher GSI scores at baseline, but also with a significant drop in scores across the follow-up period. Relapse was associated with an initial drop in GSI scores, but a subsequent increase in GSI scores at later follow-ups.
Conclusions
Most participants had a rapid reduction of psychological distress during the first 3 months of abstinence. Elevated levels of psychological distress may indicate an increased risk of drug use or relapse and should be monitored carefully. Our findings highlight the importance of early screening for psychological distress in SUD treatment, and advocate the use of tentative diagnostic procedures in the early phase of treatment of PSUD.
1. Introduction
Substance use disorder (SUD) is a debilitating disorder, often resulting in loss of academic achievement, social isolation, and often severe effects on mental and physical health (American Psychiatric Association Citation2013; Martin et al. Citation2014; Kelly, Evans-Whipp, et al. Citation2015; Heradstveit et al. Citation2017). While polysubstance dependence is not in the DSM-5 (Hasin et al. Citation2013), polysubstance use is common in clinical samples (Bhalla et al. Citation2017), and polysubstance use patterns is often seen in patients seeking treatment for mono-drug disorders (Brooner et al. Citation1997; Staines et al. Citation2001; Palamar et al. Citation2018; Timko et al. Citation2018; Choi and DiNitto Citation2019). Polysubstance use disorder (PSUD) in this context refers to the use of multiple substances as part of a pattern of problematic substance use, in which the patient meets criteria for substance use disorder for some, but not necessarily all substances used.
In clinical practice, a quintessential goal of treatment is continued abstinence. Best-practice guidelines suggest appropriating a tailored and personalized approach to treatment, which often entails including a patient’s social, psychological and medical status in the planning of treatment (Kleber et al. Citation2007). SUD-related subjective psychological distress is especially prominent among patients with PSUD, both in clinical and nonclinical samples (Hoxmark et al. Citation2010; Connor et al. Citation2014; Kelly, Chan, et al. Citation2015). PSUD is also associated with poor treatment outcomes, and higher frequencies of comorbid mental disorders, including affective disorders, anxiety, and positive psychotic symptoms (Riehman et al. Citation2002; Bakken et al. Citation2007; Dutra et al. Citation2008; Connor et al. Citation2013; Quek et al. Citation2013; Salom et al. Citation2016). These adverse outcomes have been argued to be a result of dose–response relationship where increasing numbers of substances used result in more adverse effects on psychological health (Andreas et al. Citation2015), an association which might be especially prominent during periods of active drug use (Tomasson and Vaglum Citation1997; Booth et al. Citation2010; Andreas et al. Citation2015).
However, when SUD patients enter treatment, psychological symptoms tend to improve considerably as a result of continued abstinence, especially in the patients with the highest severity of drug or alcohol use disorders (Hoxmark et al. Citation2010). Our group has previously found alleviation of psychological distress, increased quality of life, and improved neurocognitive functioning after 12 months of abstinence (Hagen et al. Citation2017). Reduced psychological distress has also been demonstrated in patients who reduce substance use over 3 years (Booth et al. Citation2010). Abstinence has also been associated with long-term gradual alleviation of mental distress among patients with pSUD at 2-, 6-, and 10-year follow-ups (Tomasson and Vaglum Citation1997; Bakken et al. Citation2007; Andreas et al. Citation2015).
Despite the positive effects of abstinence, recovery is not a stable or static state (De Soto et al. Citation1985). Little is known about the recovery process during the initial phases of abstinence among patients with pSUD (Gossop et al. Citation2006; Dennis et al. Citation2007). Previous studies have demonstrated that recovery from psychological distress may be evident following abstinence periods exceeding 6 months, and that psychological distress may continue to abate across several years (Gossop et al. Citation2006; Andreas et al. Citation2015; Hagen et al. Citation2017).
However, acute-phase data from the early stages of abstinence are still sparse and the interaction between psychological distress and abstinence/recovery remain underexplored. Improved knowledge about the course and timing of symptom alleviation during the recovery of polysubstance abuse could help equip clinicians to better support patients through what is known to be a very vulnerable phase with a high risk of treatment dropout (Stark Citation1992; Passos and Camacho Citation2000). The aim of our study was therefore to provide a detailed account of the trajectory of psychological distress, both during the acute phase of treatment and over 12 months. We hypothesized that greater alleviation of psychological distress would be related to more stable patterns of abstinence.
2. Methods
2.1. Study design and patient characteristics
This study used data from the Norwegian Stayer study, a prospective cohort study of the course and timing of neurocognitive and psychosocial recovery of patients with polysubstance use (Hagen et al. Citation2016). We recruited patients from inpatient treatment facilities (N = 82), outpatient treatment facilities (N = 52), and private treatment facilities (N = 7) in the Stavanger University Hospital catchment area. Both outpatient and inpatient treatment in Norway is regulated by the health authorities through national guidelines, and all patients are provided interdisciplinary services, including psychological, medical and social assistance, in their recovery process. See Andersson, Steinsbekk, et al. (Citation2018) for more details regarding the structure of Norwegian SUD-treatment. To access specialized treatment for SUDs within the Norwegian public health service, patients must fulfill the criteria for a diagnosis F1x.1 – harmful use, or F1x.2 – dependency syndrome, as defined by the ICD-10 (World Health Organization Citation1992). For this study, polysubstance users were defined as patients with SUD, who reported use of multiple substances within the last year before inclusion. The Stayer study was approved by the Regional Ethical Committee (REK 2011/1877).
2.2. Inclusion criteria
Inclusion criteria included: (a) signed written informed consent; (b) polysubstance use as defined by the above diagnostic criteria; (c) participant initiating a course of treatment within the substance abuse treatment services; (d) age >16 years.
2.3. Participant characteristics
A total of 208 patients were recruited consecutively from the Stavanger University Hospital catchment area between March 2012 and January 2016. Patients received NOK 400 in compensation for their time at baseline testing.
Of the 208 patients in the Stayer cohort, 44 patients were omitted from this study because of single-substance use (e.g. alcohol or cannabis) or a nondrug-related addiction (e.g. gambling disorder), leaving 164 patients fulfilling the criteria for the current study. During the follow-up period, 11 (6.7%) patients dropped out of the study, leaving 153 eligible patients. By the 12-month follow-up, 12 of these patients had withdrawn or were unavailable for evaluation, leaving a final study cohort of 141 patients who completed every follow-up (86% of eligible patients).
2.4. Procedures
At baseline, trained members of the Stayer study group performed neurocognitive, psychological, and social functioning assessments of every participant. This comprehensive assessment was repeated at 12 months. Follow-ups at 3 and 6 months comprised a smaller subset of measures assessing substance use and psychological and social functioning. To limit the rate of attrition, comprehensive efforts were made to ensure continued participation (Svendsen et al. Citation2017).
We implemented an SMS tracker in addition to the main follow-ups (Svendsen et al. Citation2017). Participants received an automated text message every two weeks, to which they replied with information about their current substance use and treatment status. This procedure was implemented to inform missing data and increase the temporal density of the data gathered. The automated SMS service contained two items: (1) “How much have you used drugs in the last two weeks?” (Likert scale: 0 = Not at all, 1 = Very little, 2 = Little, 3 = Some, 4 = A lot, 5 = Considerably), and (2) “Are you currently in treatment?” (“yes” or “no”).
2.5. Assessment
We gathered information about demographic variables, clinical history, lifestyle factors, and social functioning using a semi-structured interview. We used the consumption items from the Drug Use Disorders Identification Test (DUDIT-C) and the Alcohol Use Disorders Identification Test (AUDIT-C) (Babor et al. Citation1989; Berman et al. Citation2005) to assess and track substance use. For the DUDIT-C, a cutoff score >1 was used as a definition of current substance use. Although AUDIT-C scores of >3 for women and >4 for men have optimal sensitivity and specificity for problematic alcohol use in the general population (Bush et al. Citation1998), a cutoff score of ≥5 was used as a definition of problematic alcohol use for this study. This higher cutoff score has previously been used to identify unhealthy alcohol use in at-risk populations to limit the risk of false positives (Rubinsky et al. Citation2013; Williams et al. Citation2014).
We measured general psychological distress using the Symptoms Checklist 90 – Revised (SCL-90-R), a 90-item self-report measure (Derogatis Citation1994). We scored items on a five-point Likert scale ranging from 0 (Not at all) to 4 (Severe). The checklist yields nine symptom dimension subscales: Somatization, Obsessive-Compulsive Disorder, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, and Psychoticism, in addition to a global severity index (GSI). The SCL-90-R is widely used in clinical practice and research and is a valid instrument for assessing general psychological distress in SUD patients (Bergly et al. Citation2014).
2.6. Data quality and missing data
All 141 participants attended the 12-month follow-up visit. However, 41 patients did not attend the 3- and/or 6-month visits, resulting in missing data.
2.7. Definitions
We used data from the AUDIT-C, DUDIT-C, and the SMS tracker to assess the progression of substance use throughout 12 months. We used SMS data to inform missing data for the 3- and 6-month visits. An answer of ≥1 on the SMS question was used as an indication of drug use. Based on these data, patients were divided into three groups: (1) the Stable abstinence group who reported persistent abstinence over the full 12-month period (i.e. no substance use episodes reported during the follow up time); (2) the Unstable abstinence group who reported abstinence at the 12-month assessment, but also reported substance use episodes during the follow-up period (i.e. score above cutoff on AUDIT-C or DUDIT-C during follow up, but below cutoff on the 12 month-assessment); and (3) the Relapse group who had relapsed at the 12-month evaluation. Relapse was defined as a positive screening with either AUDIT-C or DUDIT-C at the 1-year follow up visit. The inclusion of the category “unstable abstinence” was based on a common clinical observations; patient who manage to recover from their PSUD, both in terms of drug use and successful recovery of social and psychological variables, often have single drug use-episodes during the recovery phase.
2.8. Statistical analysis
We analyzed data using IBM SPSS v. 25 for PC and G*Power 3 (Faul et al. Citation2007). We defined statistical significance as p-values <0.05 (two-tailed). First, assumptions were evaluated using Q-Q plots and inspecting the residuals. We used t-tests to check for gender differences in SCL-90-R scores. Linear regression was used to assess the association between baseline SCL-90-R GSI scores (dependent variable) and age, gender, and age of drug debut (independent variables).
We examined longitudinal data using a linear mixed model (LMM) with maximum likelihood estimation to assess between-group differences on SCL-90-R GSI over the year. We chose LMM to limit the impact of type 1 errors, and fully use the available data. We included random intercept for each patient and slope as they enhanced the model fit (evaluated using Akaike’s information criteria and Schwarz’s Bayesian criterion). The main parameters of interest were the fixed interaction term between progression groups and time. An unadjusted model, with SCL-90-R GSI scores as a dependent variable, and time, progression type (stable abstinence, unstable abstinence, or relapse), and an interaction term (progression type × time) were fitted. We also fitted an adjusted model, which included the fixed variable education (in years). For the repeated measure (SCL-90-R GSI), the unstructured covariance structure was assumed, as this yielded the least amount of error and the best model fit. We calculated the estimated marginal means using Sidak’s adjustment for multiple testing. To gauge within-group differences in SCL-90-R GSI scores between each follow-up visit, separate LMMs were fitted for each group. In these analyses, SCL-90-R was the dependent variable, while time and education (in years) served as fixed effects. We computed within-group pre–post effect sizes using Cohen’s d, with pooled pre- and post-SD adjustment for sample size.
3. Results
3.1. Participant characteristics
summarizes the demographic variables at baseline. Participants were predominantly male, with a mean age of 27.5 (standard deviation [SD] = 7.7) years. Participant age ranged widely (16–51 years). The participants were all polysubstance users, with a mean duration of drug use of 14.5 (SD = 7.8) years. Although the self-reported number of previous treatment attempts varied (range = 0–20), most patients reported one or more previous treatment attempts.
Table 1. Baseline demographic and clinical variables for included patients from the Norwegian Stayer study cohort (N = 141).
3.2. Psychological distress at baseline (SCL-90-R)
Baseline SCL-90-R scores are summarized in . In general, patients reported elevated levels of psychological distress across all indices of the SCL-90-R. No gender differences were evident, but age (β = −0.07; 95% confidence interval [CI]: −0.12– to −0.02; p = 0.006) and years of drug use (β = −0.05; 95% CI: −0.01– to −0.10; p = 0.036) were significantly associated with decreased scores on the SCL-90-R GSI. There were no significant differences between inpatient and outpatient participants in mean SCL-90-R GSI scores.
Table 2. Gender-stratified mean t-scores on ten symptom dimensions, and three global indices on the SCL-90-R (N = 141).
3.3. The course of abstinence and drug use
Over the year, 22.7% (N = 32) reported stable abstinence, 22.7% (N = 32) reported unstable abstinence, and 54.6% (N = 77) reported relapse. Details of alcohol or drug use during the follow-up period are summarized in . In the stable abstinence group, no data were missing by definition. Of the 32 participants in the unstable abstinence group, 59.4% (N = 19) reported a single episode of substance or alcohol use before the 3-month visit, and eight reported a single episode of substance or alcohol episode before the 6-month visit. Five patients who were abstinent at the 12-month evaluation had missing data on the 3-month (N = 1) or 6-month (N = 4) evaluation and had not responded to the SMS tracker. These patients were categorized in the unstable abstinence group because of the uncertain nature of their drug use during follow up. Of the 77 patients categorized as relapsed, 47 had relapsed after 3 months and had continued substance use until the final assessment at 12 months. Ten participants had relapsed after the 6-month visit and had continued substance use until the 12-month evaluation. Six participants relapsed in between the 6-month and the 12-month visits. Lastly, eight participants had a substance use episode in the first 3 months, followed by a time of abstinence and a final relapse before the 12-month assessment. Six participants had missing data on either the 3-month visit (N = 1) or the 6-month visit (N = 5).
Table 3. Substance use during the follow-up period for the different patient groups.
At baseline, there were no significant differences between these groups on demographic variables (data not shown). On the SCL-90-R GSI, no overall significant differences between these groups were evident at baseline. Patients in the relapse group scored significantly higher on the SCL-90-R Depression scale when compared to the Stable abstinence group. No other significant group differences were evident on SCl-90-R at baseline.
3.4. Course of SCL-90-R
All patient groups showed a significant GSI score reduction from baseline to 3-month follow-up in the paired samples t-test (stable abstinence, t = 4.2, p < 0.001, d = 0.66; unstable abstinence, t = 3.7, p = 0.001, d = 0.74; relapse t = 2.2, p = 0.033, d = 0.26). A similar analysis of the development from baseline to 12 months demonstrated a medium reduction in SCL-90-R for the stable abstinence group (t = 4.7, p < 0.001, d = 0.68), a large reduction for the unstable abstinence group (t = 5.8, p < 0.001, d = 1.11), and a small reduction in SCL-90-R GSI score for the relapse group, which did not reach statistical significance (t = 1.5, p = 0.135, d = 0.25). The complete set of stratified mean scores in the SCL-90-R subscales is available in the Supplementary material.
The LMM analysis found a significant main effect of the fixed effects time (F(3, 25) = 25.3, p < 0.001), progression type (F(2, 25) = 13.0, p < 0.001), and the interaction for progression type × time (F(6, 25) = 3.8, p = 0.001). The fixed effects estimates are summarized in . The stable abstinence group (β = −0.35; 95% CI: −0.60 to −0.09; p = 0.007) had significantly lower scores on the SCL-90-R GSI than the relapse group. This was supported by a significant difference (p < 0.001) in the estimated marginal means (EMM) between the two groups (stable abstinence, EMM = 0.55, 95% CI: 0.38–0.71; relapse, EMM = 1.06, 95% CI: 0.95–1.17). The unstable abstinence group did not differ in overall GSI score when compared with the relapse group (B = 0.01, 95% CI: −0.24–0.26; p = 0.931), which was supported by similar EMM between the two groups (unstable abstinence, EMM = 0.86, 95% CI: 0.69–1.03; relapse, EMM = 1.06, 95% CI: 0.95–1.17; p = 0.152). The stable abstinence group had significantly lower EMM scores than the unstable abstinence group (stable abstinence, EMM = 0.55, 95% CI: 0.38–0.71; unstable group, EMM = 0.86, 95% CI: 0.69–1.03; p = 0.033).
Table 4. Fixed effects estimates in linear mixed regression model for SCL-90-R GSI t-score from baseline to 12-month follow-up.
The fixed effect of time was statistically significant, suggesting a general decline in SCL-90-R scores across the entire cohort from baseline to 3 months (β = −0.19; 95% CI: −0.33 to −0.05; p = 0.010), and from baseline to 6 months (β = −0.43; 95% CI: −0.58 to −0.27; p < 0.001). The overall change between baseline and the final 12-month follow-up visit was not significant.
The interaction between progression groups and time suggests that the stable abstinence group did not differ in the development of GSI score over the first 3 months when compared with the relapse group (reference category). However, the unstable abstinence group had a significantly steeper decline in GSI score during this period. The groups did not significantly differ during the baseline to 6-month period. Finally, across the full 12-month follow-up period, both the stable abstinence group (β = −0.41; 95% CI: −0.66 to −0.15; p = 0.002) and the unstable abstinence group (β = −0.49; 95% CI: −0.74 to −0.23; p < 0.001) reported a significantly greater reduction in GSI scores than the relapse group. In an effort to ensure that our results was not impacted by the inclusion of five participants with missing data in the “unstable” group, we replicated the analysis with these participants coded as “abstinent”. This change did not significantly change our results.
The adjusted tradjectories of SCL-90-R GSI scores are shown in . Follow-up within-group LMMs revealed that the stable abstinence group saw a significant reduction in SCL-90-R GSI scores between baseline and 3-month follow-up (EMM difference = −0.37; 95% CI: −0.60 to −0.15; p < 0.001), but no significant change between further follow-ups (, Panel A). For the unstable group, a similar development was observed, with a significant change in SCL-90-R GSI score from baseline to the 3-month follow-up (EMM difference = −0.51; 95% CI: −0.86 to −0.15; p = 0.001), but no significant change between remaining visits (, Panel B). For the relapse group, the change from baseline to 3-month visit was also significant (EMM difference = −0.23; 95% CI: −0.44 to −0.02; p = 0.026). This was followed by no significant change from the 3- to 6-month follow-up, but then an increase in SCL-90-R score between the 6- and 12-month follow-ups (EMM difference = 0.31; 95% CI: 0.08–0.53; p = 0.002), setting this group apart from the others (, Panel C).
4. Discussion
This paper investigated changes in psychological distress and substance use over 12 months in a patient cohort with polysubstance use following admission to outpatient or inpatient treatment. In our sample, the initiation of a new treatment series was followed by a significant decline in psychological distress during the first 3 months, regardless of whether patients were still using substances, across all recovery groups. Lasting and stable abstinence during the follow-up period was rare. In a clinical context, these findings highlight the importance of providing close monitoring and support over time for patients who aim to resolve their SUD. Our data clearly illustrate that episodes of drug or alcohol use during recovery are the norm rather than the exception, as more than half of our patients experienced a relapse at some point during the 12 months following admission to treatment.
This study is one of only a limited number of studies that have focused specifically on patients with PSUD. As PSUD is the norm rather than the exception, this means that the findings are likely to be relevant for a large proportion of people in care for any SUD (McCabe et al. Citation2017).
Previous studies have found that higher levels of pretreatment mental distress and psychiatric disorders predict relapse and these leading authors recommend screening for psychological symptoms at the onset of treatment (Andersson, Wenaas, et al. Citation2019). In our sample, however, the relapse and unstable abstinence groups did not significantly differ in initial psychological distress. Both groups demonstrated an initially steep decline in psychological distress over the first 3 months, although this effect was less prominent among the relapse group. A similar pattern was found in a previous study that identified alleviation of mental distress after 1 month of follow-up (Gossop et al. Citation2006). These findings suggest that alleviation of psychological distress is commonplace when initiating a new treatment sequence. This aspect of recovery may be due to abstinence alone. However, psychological (for example personality traits, intelligence or self-efficacy) or demographic factors (for example housing, job security, familial support) may contribute, alongside regression to the mean, to the decline of psychological distress (Daughters et al. Citation2005; Dennis et al. Citation2007; Hoxmark et al. Citation2010).
The decline in psychological distress at 3-month follow-up could be due to a greater degree of abstinence among all of the groups at the beginning of treatment. However, the reduction in psychological distress among the unstable group persisted throughout the 12 months. Only the relapse group had an increase in psychological distress back to baseline levels at the 12-month evaluation. This finding is somewhat surprising, given previous reports that successful abstinence is related to more prominent alleviation of psychological distress and increased quality of life during recovery from SUD or alcohol use disorder (Subbaraman and Witbrodt Citation2014; Andreas et al. Citation2015). Our study suggests that reductions in mental distress may be persistent even if episodes of substance use occur during the recovery process. The current findings are important because they indicate that no abstinence period is without positive effects on the reduction of psychological distress.
The observation that symptoms of psychiatric distress improve with time during treatment for PSUDs has historically been taken as evidence that psychiatric disorders in people with PSUDs are generally substance-induced and need not to be urgently addressed (see Delgadillo et al. Citation2016 for a critique). Patients with high levels of psychological distress have an increased risk of relapse or drug use during the recovery phase (Flynn et al. Citation2004; Andersson, Steinsbekk, et al. Citation2018), or an ongoing need for treatment for psychiatric disorders (Thylstrup et al. Citation2018). Hence, early screening is not without its merits. Indeed, frequent monitoring of drug use and psychological distress may also have clinical value by allowing early identification of relapse episodes and interventions timed to the patient’s specific status concerning drug use and psychological distress (Dennis and Scott Citation2007).
In this study, 45.4% of participants reported being abstinent 12 months after the onset of treatment. It is sobering to note, however, that only 22.7% of participants, all of whom started a new treatment sequence, managed to stay abstinent throughout the full year. This is supported by clinical observations, and findings from other longitudinal studies investigating the recovery process in these patients (Vaillant Citation1988; Dennis and Scott Citation2007). Indeed, a recent meta-analysis showed that complete remission from substance use is rare, and expected in only 10–15% of cases per year (Fleury et al. Citation2016).
These findings highlight the continued importance of early screening for psychological distress to tailor support and monitoring levels during treatment. This is especially important for patients who report lower rates of symptoms alleviation during the first 3 months of treatment, and thus pose a greater risk of substance use episodes. Still, in clinical practice patients with comparatively mild levels of psychological distress are not guaranteed a stable or even successful recovery. Indeed, patients with PSUD may not only be in need of continued support and monitoring during the recovery phase, but may also need to have easy access to re-admission after episodes of relapse. Finally, our findings also highlight the importance of continued care for patients who have episodes of drug use during treatment, since single episodes of drug use during recovery do not always entail continued substance use. In clinical practice, this new knowledge could inform psychoeducation about the expected mental health benefits of abstinence.
4.1. Strengths and limitations
The major strengths of this study are its prospective design, participants recruited from multiple treatment settings, frequent and repeated assessments during the 12-month follow-up period, and the relatively low level of attrition during follow-up. The study also utilizes validated scales that are common in clinical practice in the follow-up of patients with PSUD.
An important limitation to our study is that some participants missed follow- up visits. Missing data is common in addiction research, and we have used two strategies to handle this issue. First of all, LMM handles missing data well and is an overall better statistical strategy for longitudinal data, as it avoids list-wide deletion or imputation of data, which is common in many SUD studies (McPherson et al. Citation2012). Secondly, the inclusion of an SMS tracker provides strong temporal insights into the SUD status for participants with missing data. This yields a more accurate depiction of drug and alcohol use across the follow-up period. Our relatively low attrition rate (6.7%) also increases the external validity and generalizability of our data. A further limitation of this study is that SUD outcome groups are based on self-report. Self-report has been shown to be a feasible instrument for the study of SUD populations (Secades-Villa and Fernández-Hermida Citation2003). Still, this issue could be at least partly resolved in future studies with somatic screening (e.g. urine samples) and/or collateral information from next-of-kin or treatment practitioners to substantiate group categorization. Lastly, the data is based on a convenience sample, where clinicians asked relevant patients to participate in the study. However, the universal access to health care and treatment in Norway probably allows a more comprehensive sample relative to countries where care is privatized and costly.
Future prospective studies could include an additional measure of psychological distress tolerance to provide further insight into possible the associations between a higher degree of psychological distress and vulnerability to the risk of relapse/increased drug use (Daughters et al. Citation2005).
4.2. Conclusions
Psychological distress in PSUD participants significantly declined during the first 3 months of abstinence in treatment. However, there is no straightforward correlation between abstinence and psychological distress: Short-term alleviation of distress may exist even alongside temporary relapse episodes. Still, our data show that a return to abstinence after using is necessary to attain long-term alleviation of mental distress. These findings argue for the importance of continued follow up when patients relapse during treatment.
Supplemental_materials.docx
Download MS Word (13.7 KB)Acknowledgements
We extend our sincere gratitude to the participants in our study and the staff of the participating clinical services, the KORFOR staff, and in particular, Thomas Solgård Svendsen, Anne-Lill Mjølhus Njaa, and Janne Aarstad, who collected all the initial and follow-up data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington (VA): American Psychiatric Publishing.
- Andersson HW, Steinsbekk A, Walderhaug E, Otterholt E, Nordfjaern T. 2018. Predictors of dropout from inpatient substance use treatment: a prospective cohort study. Subst Abuse. 12:1–10.
- Andersson HW, Wenaas M, Nordfjaern T. 2019. Relapse after inpatient substance use treatment: a prospective cohort study among users of illicit substances. Addict Behav. 90:222–228.
- Andreas JB, Lauritzen G, Nordfjaern T. 2015. Co-occurrence between mental distress and poly-drug use: a ten year prospective study of patients from substance abuse treatment. Addict Behav. 48:71–78.
- Babor TF, de la Fuente JR, Saunders J, Grant M. 1989. AUDIT: the Alcohol Use Disorders Identification Test: guidelines for use in primary health care. Geneva: World Health Organization; p. 894.
- Bakken K, Landheim AS, Vaglum P. 2007. Axis I and II disorders as long-term predictors of mental distress: a six-year prospective follow-up of substance-dependent patients. BMC Psychiatry. 7(1):29.
- Bergly TH, Nordfjaern T, Hagen R. 2014. The dimensional structure of SCL-90-R in a sample of patients with substance use disorder. J Subst Use. 19(3):257–261.
- Berman AH, Bergman H, Palmstierna T, Schlyter F. 2005. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res. 11(1):22–31.
- Bhalla IP, Stefanovics EA, Rosenheck RA. 2017. Clinical epidemiology of single versus multiple substance use disorders: polysubstance use disorder. Med Care. 55:2:S24–S32.
- Booth B, Curran G, Han X, Wright P, Frith S, Leukefeld C, Falck R, Carlson R. 2010. Longitudinal relationship between psychological distress and multiple substance use: results from a three-year multisite natural-history study of rural stimulant users. J Stud Alcohol Drugs. 71(2):258–267.
- Brooner RK, King VL, Kidorf M, Schmidt CW, Jr., Bigelow GE. 1997. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch Gen Psychiatry. 54(1):71–80.
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. 1998. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 158(16):1789–1795.
- Choi NG, DiNitto DM. 2019. Older marijuana users in substance abuse treatment: treatment settings for marijuana-only versus polysubstance use admissions. J Subst Abuse Treat. 105:28–36.
- Connor JP, Gullo MJ, Chan G, Young RM, Hall WD, Feeney GF. 2013. Polysubstance use in cannabis users referred for treatment: drug use profiles, psychiatric comorbidity and cannabis-related beliefs. Front Psychiatry. 4:79.
- Connor JP, Gullo MJ, White A, Kelly AB. 2014. Polysubstance use: diagnostic challanges, patterns of use and health. Curr Opin Psychiatry. 27(4):269–275.
- Daughters SB, Lejuez CW, Kahler CW, Strong DR, Brown RA. 2005. Psychological distress tolerance and duration of most recent abstinence attempt among residential treatment-seeking substance abusers. Psychol Addict Behav. 19(2):208–211.
- De Soto CB, O’Donnell WE, Allred LJ, Lopes CE. 1985. Symptomatology in alcoholics at various stages of abstinence. Alcoholism Clin Exp Res. 9(6):505–512.
- Delgadillo J, Bohnke JR, Hughes E, Gilbody S. 2016. Disentangling psychopathology, substance use and dependence: a factor analysis. BMC Psychiatry. 16:281.
- Dennis M, Foss M, Scott C. 2007. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Eval Rev. 31(6):585–612.
- Dennis M, Scott CK. 2007. Managing addiction as a chronic condition. ASCP. 4(1):45–55.
- Derogatis LR. 1994. Symptom checklist-90-R: administration, scoring & procedure manual for the revised version of the SCL-90. Minneapolis (MN): National Computer Systems.
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. 2008. A meta-analytic review of psychosocial interventions for substance use disorders. AJP. 165(2):179–187.
- Faul F, Erdfelder E, Lang AG, Buchner A. 2007. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 39(2):175–191.
- Fleury M.-J, Djouini A, Huỳnh C, Tremblay J, Ferland F, Ménard J.-M, Belleville G. 2016. Remission from substance use disorders: a systematic review and meta-analysis. Drug Alcohol Depend. 168:293–306.
- Flynn HA, Walton MA, Curran G, Blow FC, Knutzen S. 2004. Psychological distress and return to substance use two years following treatment. Subst Use Misuse. 39(6):885–910.
- Gossop M, Marsden J, Stewart D. 2006. Remission of psychiatric symptoms among drug misusers after drug dependence treatment. J Nerv Ment Dis. 194(11):826–832.
- Hagen E, Erga AH, Hagen KP, Nesvag SM, McKay JR, Lundervold AJ, Walderhaug E. 2016. Assessment of executive function in patients with substance use disorder: a comparison of inventory- and performance-based assessment. J Subst Abuse Treat. 66:1–8.
- Hagen E, Erga AH, Hagen KP, Nesvag SM, McKay JR, Lundervold AJ, Walderhaug E. 2017. One-year sobriety improves satisfaction with life, executive functions and psychological distress among patients with polysubstance use disorder. J Subst Abuse Treat. 76:81–87.
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, et al. 2013. DSM-5 criteria for substance use disorders: recommendations and rationale. AJP. 170(8):834–851.
- Heradstveit O, Skogen JC, Hetland J, Hysing M. 2017. Alcohol and illicit drug use are important factors for school-related problems among adolescents. Front Psychol. 8:1023.
- Hoxmark E, Benum V, Friborg O, Wynn R. 2010. Reduction in mental distress among substance users receiving inpatient treatment. Int J Ment Health Syst. 4(1):30.
- Kelly A, Chan GC, Mason WA, Williams JW. 2015. The relationship between psychological distress and adolescent polydrug use. Psychol Addict Behav. 29(3):787–793.
- Kelly A, Evans-Whipp T, Smith R, Chan G, Toumbourou J, Patton G, Hemphill S, Hall W, Catalano R. 2015. A longitudinal study of the association of adolescent polydrug use, alcohol use and high school non-completion. Addiction. 110(4):627–635.
- Kleber H, Weiss R, George T, Kosten T, Rounsaville B, Ziedonis D, Disorders W. 2007. Treatment of patients with substance use disorders. 2nd ed. Am J Psychiatry. 164(4 Suppl):5–123.
- Martin CS, Langenbucher JW, Chung T, Sher KJ. 2014. Truth or consequences in the diagnosis of substance use disorders. Addiction. 109(11):1773–1778.
- McCabe SE, West BT, Jutkiewicz EM, Boyd CJ. 2017. Multiple DSM-5 substance use disorders: a national study of US adults. Hum Psychopharmacol. 32(5):e2625.
- McPherson S, Barbosa-Leiker C, Burns GL, Howell D, Roll J. 2012. Missing data in substance abuse treatment research: current methods and modern approaches. Exp Clin Psychopharmacol. 20(3):243–250.
- Palamar JJ, Le A, Mateu-Gelabert P. 2018. Not just heroin: extensive polysubstance use among US high school seniors who currently use heroin. Drug Alcohol Depend. 188:377–384.
- Passos SR, Camacho LA. 2000. Factors associated with immediate dropout of outpatient treatment for drug abuse in Rio de Janeiro. Soc Psychiatry Psychiatr Epidemiol. 35(11):513–517.
- Quek LH, Chan GC, White A, Connor JP, Baker PJ, Saunders JB, Kelly AB. 2013. Concurrent and simultaneous polydrug use: latent class analysis of an Australian nationally representative sample of young adults. Front Public Health. 1:61.
- Riehman KS, Iguchi MY, Anglin MD. 2002. Depressive symptoms among amphetamine and cocaine users before and after substance abuse treatment. Psychol Addict Behav. 16(4):333–337.
- Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. 2013. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res. 37(8):1380–1390.
- Salom CL, Betts KS, Williams GM, Najman JM, Alati R. 2016. Predictors of comorbid polysubstance use and mental health disorders in young adults-a latent class analysis. Addiction. 111(1):156–164.
- Secades-Villa R, Fernández-Hermida JR. 2003. The validity of self-reports in a follow-up study with drug addicts. Addict Behav. 28(6):1175–1182.
- Staines GL, Magura S, Foote J, Deluca A, Kosanke N. 2001. Polysubstance use among alcoholics. J Addict Dis. 20(4):57–73.
- Stark M. 1992. Dropping out of substance abuse treatment: a clinically oriented review. Clin Psychol Rev. 12(1):93–116.
- Subbaraman MS, Witbrodt J. 2014. Differences between abstinent and non-abstinent individuals in recovery from alcohol use disorders. Addict Behav. 39(12):1730–1735.
- Svendsen TS, Erga AH, Hagen E, McKay JR, Njå ALM, Årstad J, Nesvåg S. 2017. How to maintain high retention rates in long-term research on addiction: a case report. J Soc Work Pract Addict. 17(4):374–387.
- Thylstrup B, Bloomfield K, Hesse M. 2018. Incremental predictive validity of the Addiction Severity Index psychiatric composite score in a consecutive cohort of patients in residential treatment for drug use disorders. Addict Behav. 76:201–207.
- Timko C, Han X, Woodhead E, Shelley A, Cucciare MA. 2018. Polysubstance use by stimulant users: health outcomes over three years. J Stud Alcohol Drugs. 79(5):799–807.
- Tomasson K, Vaglum P. 1997. The 2-year course following detoxification treatment of substance abuse: the possible influence of psychiatric comorbidity. Eur Arch Psychiatry Clin Neurosci. 247(6):320–327.
- Vaillant GE. 1988. What can long-term follow-up teach us about relapse and prevention of relapse in addiction? Addiction. 83(10):1147–1157.
- Williams EC, Rubinsky AD, Chavez LJ, Lapham GT, Rittmueller SE, Achtmeyer CE, Bradley KA. 2014. An early evaluation of implementation of brief intervention for unhealthy alcohol use in the US Veterans Health Administration. Addiction. 109(9):1472–1481.
- World Health Organization. 1992. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization.