ABSTRACT
Background
Elevated serum calcium levels may serve as a useful clinical biomarker of mortality in patients with multiple myeloma(MM). However, the clinical significance of the relationship between serum calcium levels and in-hospital mortality in MM patients admitted to the Intensive Care Unit (ICU) remains unclear.
Objectives
This study aimed to explore the association between serum calcium levels and in-hospital mortality in patients with MM in the ICU.
Methods
Patients with MM were identified from the Medical Information Mart for Intensive Care IV(MIMIC-IV) database. The outcome was in-hospital mortality. Multivariable-adjusted Cox regression analysis, curve fitting, and threshold effects analysis were used to assess the relationship between serum calcium levels and in-hospital mortality in patients with MM in the ICU.
Results
Our study included 262 patients with MM with a mean age of 72.3 ± 11.0 years, 63.4% of whom were male. The in-hospital mortality was 19.5% (51/262). The relationship between serum calcium levels and in-hospital mortality was nonlinear. The effect size on the left and right sides of the inflection point, were 0.270 (HR: 0.270, 95% CI 0.106-0.687, P < 0.05) and 2.104 (HR: 2.104, 95% CI 1.069-4.142, P < 0.05), respectively. The results of the sensitivity analysis remained stable.
Conclusion
Our findings show that a nonlinear relationship exists between serum calcium levels and in-hospital mortality in critically ill patients with MM. A serum calcium level of approximately 8.40 mg/dL was associated with the lowest risk of in-hospital mortality, which increases with rising serum calcium levels, and should be of concern to ICU physicians.
Introduction
Multiple myeloma (MM), a plasma cell tumor that accounts for 1-1.8% of all cancers, is the second most common hematologic malignancy that can originate in the bone [Citation1]. Serum calcium plays an important role in a variety of malignancies, including breast [Citation2], ovarian [Citation3], and prostate cancer [Citation4]. Intracellular calcium ions are key secondary messengers and play an important role in malignant transformation and cancer progression [Citation5]. However, it is based on the tumor hypothesis that serum calcium is elevated due to the action of tumor-derived factors [Citation2]. Myeloma bone disease often causes excessive bone resorption and excessive calcium release, ultimately leading to hypercalcemia (defined as a blood calcium concentration of more than 11.5 mg/dL or 2.85 mmol/L). Some cytokines, including MIP-1, RANKL and DKK1, play an important role in osteoclast bone resorption [Citation6, Citation7].
Seven percent of patients with haematological malignancies who are admitted to the hospital become critically ill [Citation8]. In addition, these patients have a higher mortality rate than the general intensive care population [Citation9–11]. The rising burden of multiple myeloma as a prevalent hematologic disease places tremendous strain on patients, their families, and society. The chronic and aging course of MM has resulted in a significant number of ICU hospitalizations; nevertheless, not all critically ill patients benefit from ICU admission [Citation12]. Therefore, it is important to consider in-hospital mortality after ICU admission. According to the guidelines, relevant tests, such as complete blood count, creatinine, and serum calcium, should be conducted monthly or at least every three months during the follow-up of myeloma patients. This demonstrates the significance of serum calcium in patients with MM [Citation1].
Finding efficient predictors of in-hospital mortality in critically ill patients with MM is clinically important because it allows physicians to better diagnose the disease and communicate with patients and their families in a timely manner, which contributes to the rational allocation of medical resources. Diao et al. [Citation13] reported prognostic factors in patients with MM admitted to the ICU, but the relationship between serum calcium levels and mortality was not significant. Notably, previous findings by Oyajobi et al. [Citation14] showed a strong association between high serum calcium levels and poor prognosis.
To better understand the relationship between serum calcium levels and in-hospital mortality in MM patients in the ICU, we analyzed data extracted from the MIMIC-IV database for all MM patients admitted to the ICU. We aimed to explore the point at which serum calcium levels worsened if they turned out to be an independent predictor of in-hospital mortality.
Materials and methods
MIMIC-IV database
This was a retrospective study based on the MIMIC-IV database (version:1.0) [Citation15], which contains data on over 70,000 patients admitted to Beth Israel Deaconess Medical Center's ICUs in Boston, MA, from 2008 to 2019. The database is accessible to anybody who has passed the Collaborative Institutional Training Initiative exam (Certification number 39050603 for Mao). Considering that this was a retrospective study and all patients in this study were extracted from a public database, informed consent was waived.
Patients
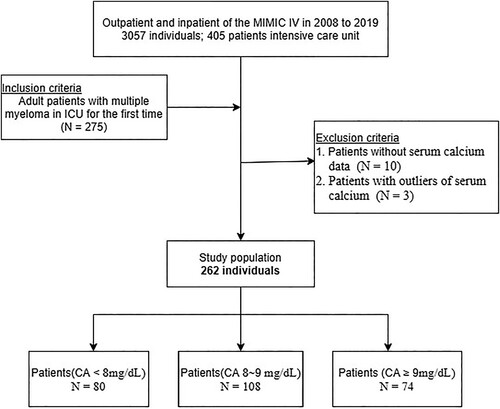
Patients were identified in the MIMIC-IV database from 2008 to 2019. The inclusion criteria were as follows: adult patients with multiple myeloma admitted to the ICU (age ≥18 years); MM defined as ICD-9 codes 20300, 20301, and 20302 or ICD-10 codes C9000, C9001, and C9002. Of the 3057 patients extracted from the MIMIC-IV database, 2052 were excluded because of a lack of recorded ICU admission information. In addition, 130 patients were excluded because of multiple ICU admissions. Thereafter, 10 patients lacking serum calcium records and 3 patients with abnormally elevated serum calcium levels were also excluded. Finally, 262 patients with MM were included in this study (). Survival information was extracted from a table named ‘patients’ from the MIMIC-IV database. Data regarding the length of hospital stay were extracted from the table named ‘admissions’ of the MIMIC-IV database [Citation16].
Covariates
The baseline serum calcium level obtained was the highest calcium value measured within 24 h of ICU admission in the MIMIC-IV database. Normal adult serum calcium levels range from approximately 8.8-10.4 mg/dL. The outcome of this study was in-hospital mortality after admission to the ICU. The variables of enrolled participants in the database included age, sex, ethnicity, the lowest hemoglobin and platelet count, the highest white blood cell (WBC) count, blood urea nitrogen (BUN), creatinine, glucose, lactic dehydrogenase (LDH) levels, and anion gap on the first day of ICU admission. Another factor to consider is the first 24-hour Sequential Organ Failure Assessment (SOFA) score, as well as the Simplified Acute Physiology Score II (SAPSII) score.
Statistical methods
Data for continuous variables were described as mean ± standard deviation (SD) or median and interquartile range (IQR), and data for categorical variables were described as frequencies or percentages. For the analysis of baseline characteristics, data were compared using the Mann–Whitney test for continuous variables and the chi-square test for categorical variables. Patients were divided into three groups based on trichotomous serum calcium levels (CA < 8 mg/dL, 8 mg/dL ≤ CA < 9 mg/dL, CA ≥ 9 mg/dL). To explore the relationship between serum calcium levels and in-hospital mortality after ICU admission, smooth curve fitting was adopted, and univariate and multivariate Cox regression analyses were performed, which used unadjusted and multivariate adjusted models to determine the stability of the relationship. Variables were selected as adjusted if the matched odds ratio changed by at least 10%. Results were adjusted for age and sex in model I; age, sex, race, highest BUN, highest glucose, SOFA and SAPSII in Model II. The results are expressed as hazard ratios (HRs) and 95% confidence intervals (CIs). Threshold effect analyses were conducted to assess the ability of serum calcium levels to predict in-hospital mortality.
All comparisons were planned, and tests were two-sided, with P < 0.05, indicating statistical significance between two or more groups. All analyses were performed using R 3.3.2 (http://www.R-project.org, R Foundation) and Free Statistics version 1.5 [Citation17].
Results
Baseline characteristics of study subjects
A total of 262 patients with MM admitted to the ICU were identified in the MIMIC-IV database according to the inclusion and exclusion criteria (). summarizes the basic demographic characteristics of the participants stratified by serum calcium levels. The mean age of the participants was 72.3 ± 11.0 years old, of whom 166 (63.4%) were male. The mean serum calcium level on the first day of admission to the ICU was 8.4 ± 0.9 mg/dL. Serum calcium levels were positively associated with hemoglobin, platelets, glucose, and anion gap. The mean SOFA score on the first day of ICU admission was 3.2 ± 2.5, and the mean SAPSII score was 39.2 ± 8.6.
Table 1. Baseline demographic characteristics of the study population stratified by serum calcium.
Association between serum calcium and outcomes
summarizes the univariate analysis of the risk factors associated with in-hospital mortality in patients with critical MM, reported as HRs and 95% CIs. Age, sex, urea nitrogen, glucose, anion gap, SOFA score, and SAPSII score were significantly associated with in-hospital mortality (P< 0.05). Conversely, factors such as hemoglobin, platelets, and other laboratory results, were not significantly associated with in-hospital mortality (). In the multivariate Cox regression analysis (), when serum calcium level was used as a continuous variable, its relationship with mortality was not significant. However, when considered as a categorical variable, a second group of serum calcium (8-9 mg/dL) was used as a baseline reference, and higher serum calcium (≥9 mg/dL category compared with 8-9 mg/dL category) was associated with a higher risk of in-hospital mortality (crude HR: 2.75; 95% CI 1.30-5.81; P < 0.05). The HR for serum calcium level was consistently significant in both models. In model 2, serum calcium level remained significantly associated with an increased risk of in-hospital death after adjusting for age, sex, urea nitrogen, glucose, SAPSII, and SOFA score (adjusted HR: 2.72; 95% CI 1.26-5.88; P < 0.05).
Table 2. Association of covariates and in-hospital morality in patients with MM.
Table 3. Relationship between different serum calcium levels and in-hospital morality in different models.
The nonlinear relationship and sensitivity analysis
Through multivariate Cox regression analysis and smooth curve fitting, we found that the relationship between serum calcium levels and in-hospital mortality in the ICU was nonlinear (). The data were fitted to a piecewise multivariate Cox regression model with two different slopes. In our study, the P-value for the likelihood ratio test was less than 0.001 (); therefore, we used a two-part model to fit the association between serum calcium level and ICU admission mortality in patients with severe MM. We found an inflection point at approximately 8.40 mg/dL. On the left side of the inflection point, the effect size was 0.270 (HR: 0.270, 95% CI 0.106-0.687, P < 0.05), and on the right side of the inflection point, the effect size was 2.104 (HR: 2.104,95% CI 1.069-4.142, P < 0.05).
Figure 2. The nonlinear relationship between serum calcium and in-hospital mortality in Multiple Myeloma in ICU. Adjusted for all covariates as model 2 (Calcium takes the upper limit of 98%).
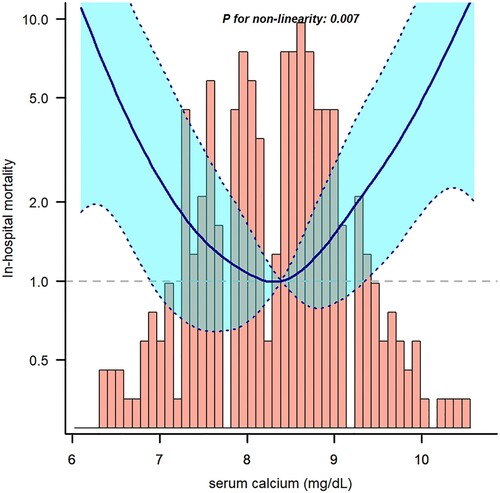
Table 4. Threshold effect analysis of serum calcium level and the in-hospital mortality of MM using Cox regression models.
Three outliers in the population for this study, 13, 13.1, and 13.3 mg/dL, were excluded to make the results more representative. However, when a sensitivity analysis was performed, and these three outliers were included in the study, the results were still significantly different (Supplementary Table S1). In addition, we averaged the highest and lowest calcium values from MIMIC IV taken on the first day of ICU admission in patients with MM to further validate the relationship between serum calcium levels and in-hospital mortality, with an effect value of 3.18 (HR: 3.18, 95% CI 1.37-7.41, P = 0.007) (> 9 mg/dL vs. 8–9 mg/dL) (Supplementary Table S2).
Discussion
The results of threshold effect analysis demonstrated that among patients with MM admitted to the ICU, serum calcium values were an independent prognostic factor for MM in-hospital mortality. Furthermore, the study described a nonlinear relationship between serum calcium levels and MM in-hospital mortality in the ICU, and the model was consistent with the trend of the fitted curve. Cheng et al. [Citation18] demonstrated that elevated baseline calcium levels in Chinese patients with newly diagnosed MM predicted their all-cause mortality. In a Mexican study, Maillet et al. [Citation19] included 24 patients with primary MM and demonstrated that serum calcium was an independent factor affecting OS prognosis in Mexican MM patients. Numerous studies have shown that the serum calcium level is a useful clinical biomarker. Diao et al. [Citation13] investigated the prognostic factors of patients with MM in the ICU and concluded that their short-term prognosis depended mainly on the severity of organ failure, infection, and disease status, and they treated serum calcium values as a continuous variable. In contrast, when we treated it as a categorical variable (>9 mg/dL vs. 8-9 mg/dL), it showed a significant relationship with in-hospital mortality, and these results could better serve clinicians by drawing close attention to the serum calcium levels of patients with MM admitted to the ICU.
The SAPSII score is an important component of the Acute Pathology and Chronic Health Evaluation (APACHE II) scoring system, and is primarily used to assess the severity of organ failure. Previous studies have shown APACHE to be an independent prognostic predictor in critically ill patients with malignant hematologic diseases. Meanwhile, SOFA score can be used as a predictor of mortality in critically ill patients [Citation20]. In clinical work, observing the trend of SOFA can better predict the prognosis of patients and help clinicians to adjust the treatment plan appropriately to improve the clinical prognosis [Citation21, Citation22]. Therefore, in our study, we adjusted the SOFA and SAPSII scores for the disease status of patients with MM.
In our study, the in-hospital mortality rate of patients with MM in the ICU (19.4%) was lower than that reported in previous studies. The in-hospital mortality rate in the study by Diao et al. was 29.4% [Citation13], and Azoulay et al. [Citation23] observed a 30-day mortality rate of 57.23% in this group of patients. These differences may be due to different nadir criteria, study populations, study durations, admission and discharge criteria, implementation of end-of-life decisions, and treatment approaches. The relatively low number of patients presenting with complications and organ failure in our study is reflected in the lower SOFA scores of our patients compared to those in several of the aforementioned studies. However, it is important to note that our study included the largest sample size of patients with MM admitted to the ICU.
The advantages of this research were the use of appropriate statistical methods to determine the curve relationship of the association between serum calcium levels and in-hospital mortality, instead of a simple straight-line relationship. Two sensitivity analyses were performed based on serum calcium levels. Moreover, we found the inflection point of the smooth curve fitting instead of manual grouping. Such results can prompt ICU physicians to pay attention to serum calcium levels when facing MM, specifically if they are elevated. These results should be interpreted in the context of the following limitations. First, this was a retrospective study, and the diagnosis of multiple myeloma was based on administrative diagnosis codes. Although the first sequence of diagnosis was used in this study, there remained the possibility of misclassifications that could cause false associations. Second, our study was limited to observing patients with MM admitted to the ICU to assess their prognostic survival, and it remains to be tested whether this inflection point can be applied to all MM patients for any period of time. Third, due to the nature of the simulation database, this study lacks some potential variables, such as myeloma parameters, disease status (e.g. bone disease and nephropathy), and treatment information. However, we used severity scoring systems, namely the SOFA score and SAPSII score, to assess the severity and comorbidities of MM, among others. Finally, this study may have been subject to selection bias, as it was a single-institution study.
Conclusions
In summary, our study demonstrated a nonlinear relationship between serum calcium levels and in-hospital mortality in patients with MM. The lowest serum calcium level for in-hospital mortality was approximately 8.40 mg/dL. However, additional prospective cohort studies are necessary to confirm the relationship between serum calcium levels and mortality in MM patients.
Author contributions
YF M conducted data analysis and wrote the manuscript. SM Z conducted data collection and data interpretation. YL G designed the study and reviewed the manuscript.
All authors read and approved the manuscript for publication.
Availability of data and materials
Data in the article can be obtained from mimic-IV database (https://mimic.physionet.org/)
Ethics approval and consent to participate
The establishment of this database was approved by the Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA), and consent was obtained for the original data collection. Therefore, the ethical approval statement and the need for informed consent were waived for this manuscript.
Informed consent statement
There was no requirement of individual informed consent to extract data from the mimic-IV database because mimic-IV database information was publicly available and all patient data were deidentified
List of abbreviations
MM, multiple myeloma; ICU, intensive care unit; SD, standard deviation; IQR, interquartile range; WBC, white blood cell; BUN, blood urea nitrogen; LDH, lactic dehydrogenase; SOFA, Sequential Organ Failure Assessment; SAPS II, Simplified Acute Physiology Score II.
Supplementary materials
The supplemental Word file contains the tables that need to be displayed in the result section of sensitive analysis.
Supplemental Material
Download MS Word (19.4 KB)Acknowledgments
We thank Dr. Liu jie (People's Liberation Army of China General Hospital, Beijing, China) and Dr. Yang Qilin(The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China) for helping in this revision.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Dimopoulos MA, Moreau P, Terpos E, et al. Multiple myeloma: EHA-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up(dagger). Ann Oncol. 2021;32:309–322. doi:10.1016/j.annonc.2020.11.014.
- Thaw SS, Sahmoun A, Schwartz GG. Serum calcium, tumor size, and hormone receptor status in women with untreated breast cancer. Cancer Biol Ther. 2012;13:467–471. doi:10.4161/cbt.19606.
- Schwartz GG, Tretli S, Vos L, et al. Prediagnostic serum calcium and albumin and ovarian cancer: A nested case-control study in the Norwegian Janus Serum Bank Cohort. Cancer Epidemiol. 2017;49:225–230. doi:10.1016/j.canep.2017.07.004.
- Schwartz GG, Skinner HG. A prospective study of total and ionized serum calcium and time to fatal prostate cancer. Cancer Epidemiol Biomarkers Prev. 2012;21:1768–1773. doi:10.1158/1055-9965.EPI-12-0585.
- Huang T, Zhou J, Wang J. Calcium and calcium-related proteins in endometrial cancer: opportunities for pharmacological intervention. Int J Biol Sci. 2022;18:1065–1078. doi:10.7150/ijbs.68591.
- Christoulas D, Terpos E, Dimopoulos MA. Pathogenesis and management of myeloma bone disease. Expert Rev Hematol. 2009 Aug;2(4):385–398.
- Roodman GD, Dougall WC. RANK ligand as a therapeutic target for bone metastases and multiple myeloma. Cancer Treat Rev. 2008;34:92–101. doi:10.1016/j.ctrv.2007.09.002.
- Gordon AC, Oakervee HE, Kaya B, et al. Incidence and outcome of critical illness amongst hospitalised patients with haematological malignancy: a prospective observational study of ward and intensive care unit based care. Anaesthesia. 2005;60:340–347. doi:10.1111/j.1365-2044.2005.04139.x.
- Lloyd-Thomas AR, Wright I, Lister TA, et al. Prognosis of patients receiving intensive care for lifethreatening medical complications of haematological malignancy. Br Med J (Clin Res Ed). 1988;296:1025–1029. doi:10.1136/bmj.296.6628.1025.
- Peters SG, Meadows III JA, Gracey DR. Outcome of respiratory failure in hematologic malignancy. Chest. 1988;94:99–102. doi:10.1378/chest.94.1.99.
- Yau E, Rohatiner AZ, Lister TA, et al. Long term prognosis and quality of life following intensive care for life-threatening complications of haematological malignancy. Br J Cancer. 1991;64:938–942. doi:10.1038/bjc.1991.430.
- Azoulay E, Recher C, Alberti C, et al. Changing use of intensive care for hematological patients. Intensive Care Med. 1999;25(12):1395–1401.
- Diao X, Cai R, Luo J, et al. Prognostic factors for patients with multiple myeloma admitted to the intensive care unit. Hematology. 2020;25:433–437. doi:10.1080/16078454.2020.1845502.
- Oyajobi BO. Multiple myeloma/hypercalcemia. Arthritis Res Ther. 2007;9(Suppl 1):S4, doi:10.1186/ar2168.
- Goldberger AL, Amaral LA, Glass L, et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation. 2000;101:E215–E220. doi:10.1161/01.cir.101.23.e215.
- Johnson AE, Stone DJ, Celi LA, et al. The MIMIC Code Repository: enabling reproducibility in critical care research. J Am Med Inform Assoc. 2018 Jan 1;25(1):32–39.
- Xiao Z, Gong R, Chen X, et al. Association between serum lactate dehydrogenase and 60-day mortality in Chinese Hakka patients with acute myeloid leukemia: A cohort study. J Clin Lab Anal. 2021 Dec;35(12):e24049, doi:10.1002/jcla.24049. Epub 2021 Oct 28. PMID: 34708888; PMCID: PMC8649362.
- Cheng J, Zhang W, Zhao Y, et al. Association of serum calcium levels with renal impairment and all-cause death in Chinese patients with newly diagnosed multiple myeloma: a cross-sectional, longitudinal study. Nutr Metab (Lond). 2021;18:19, doi:10.1186/s12986-020-00525-0.
- Maillet D, Montiel-Cervantes L, Padilla-González Y, et al. Serum calcium is an independent prognostic factor of overall survival in Mexican patients with multiple myeloma. Rev Invest Clin. 2012 Jan-Feb;64(1):17–24.
- Haddadi A, Ledmani M, Gainier M, et al. Comparing the Apache II, Sofa, Lod, and SAPS II scores in patients who have developed a nosocomial infection. Bangladesh Crit Care J. 2014;2(1):4.
- Choi JY, Jang JH, Lim YS, et al. Performance on the APACHE II, SAPS II, SOFA and the OHCA score of post-cardiac arrest patients treated with therapeutic hypothermia. Plos One. 2018;13:e0196197, doi:10.1371/journal.pone.0196197.
- Cour M, Bresson D, Hernu R, et al. SOFA score to assess the severity of the post-cardiac arrest syndrome. Resuscitation. 2016;102:110–115. doi:10.1016/j.resuscitation.2016.03.001.
- Hampshire PA, Welch CA, McCrossan LA, et al. Admission factors associated with hospital mortality in patients with haematological malignancy admitted to UK adult, general critical care units: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care. 2009;13:R137, doi:10.1186/cc8016.