ABSTRACT
Objectives
To retrospectively investigate the clinical characteristics, prognosis, treatment, and therapy outcome of Chinese patients with primary testicular lymphoma (PTL).
Methods
we collected data of 49 PTL patients from four hospitals over 13 years. The median age was 63 years old. We described the clinical characteristics of the patients including the laterality, serum lactate dehydrogenase (LDH), pathology classification, stage, International prognostic index (IPI) scores and more.
Results
Complete remission (CR) was achieved in 34 patients and partial remission (PR) in 3 patients; Progressive disease (PD) was detected in 11 patients, and 10 patients died. The average progression-free survival (PFS) of all patients was 43.92 months, and the average overall survival (OS) was 47.55 months. The Ann Arbor stage, IPI score, and LDH were associated with OS, while Ann Arbor stage, IPI score, LDH, and histotype were significantly associated with PFS. Chemotherapy and radiotherapy following orchiectomy was associated with a significantly longer PFS.
Conclusion
Most patients can achieve CR after induced therapy or orchiectomy. However, there are many associated prognostic factors.
Introduction
Primary testicular lymphoma (PTL) is a rare non-Hodgkin lymphoma that accounts for 1–2% [Citation1] of all cases of non-Hodgkin’s lymphoma (NHLs) and 3–9% [Citation2] of all testicular malignancies. Most patients are older than 60 years, and the incidence of PTL is low and increase with age. The most common clinical symptom of PTL is painless testicular swelling. The majority of PTL (>80%) are diffuse large B-cell lymphoma (DLBCL) [Citation2]. The central nervous system (CNS) and the contralateral testicle are the most common extranodal sites for relapse.
Most previous studies of PTL are retrospective with a small sample size. To date, the standard treatment for PTL has not been defined due to the rarity of the disease and the lack of prospective controlled studies. Chemotherapy based on cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) combined with radiotherapy (RT) and orchiectomy is mostly recommended. Although about 90% of PTL patients can achieve complete remission (CR) after chemotherapy and orchiectomy, its relapse rate is still very high. The use of the rituximab improved outcomes of CD20-positive B-cell lymphoma significantly [Citation3], but there is still no global consensus regarding its effect on PTL, which is a special extranodal type of lymphoma.
In this retrospective study, we evaluated the clinical features, prognostic factors, and outcomes of 49 PTL cases treated at our hospital and three other hospitals to improve the understanding of PTL and provide a better clinical experience.
Patients and methods
Patients were identified by searching the medical records from four medical institutes in Qingdao and Yantai China for cases of testicular lymphoma occurring from December 2007 to January 2020. Forty-nine patients with primary PTL who were first diagnosed and treated in the four hospitals were included in the study. All patients were followed until December 2020 (or until the date of their death). Data including clinical features, biological features, management methods, and outcomes were analyzed and compared.
Diagnosis, classification, and staging
All patients underwent inguinal orchiectomy, and histopathological diagnosis was PTL according to the 2008 guidelines of the World Health Organization (WHO). They were divided into germinal center B-cell–like (GCB)-type and non-GCB-type according to the expression of antigens MUM-1, CD10, and Bcl-6 based on the Hans algorithm. All patients were staged according to the Ann Arbor criteria [Citation4]. The international prognostic index (IPI) score was also determined so that risk stratification could be done.
Outcome evaluation
Patient treatment response of patients was classified as CR, partial remission (PR), stable disease (SD), or progressive disease (PD), according to the 2014 Lugano classification lymphoma response criteria. CR was defined as the absence of disease signs and symptoms; PR was defined as a >50% reduction in tumor size; SD was defined as less than a partial remission but not progressive disease; and PD was defined as a >50% increase in tumor size or the appearance of any new signs of disease during or at the end of therapy. Every 2–4 cycles during the therapy and 4 weeks after the end of therapy we assessed the efficacy of treatment using contrast-enhanced computed tomography (CT) or positron emission tomography-CT (PET-CT). We evaluated progression-free survival (PFS) and overall survival (OS) based on telephone interviews. PFS was defined as the elapsed time between treatment initiation and tumor progression or death from any causes, and OS was measured from the time of diagnosis to the time of death or the last follow-up.
Statistical analysis
Statistical analyses were performed using SPSS Statistics 18.0 software (IBM Corporation, Armonk, NY, USA). Descriptive analyses were used to characterize the study population. Survival curves were calculated using the Kaplan–Meier method, and differences between groups were compared using log-rank tests. The differences were considered significant at p < 0.05.
Results
Basic clinical characteristics
The cases of 49 patients with a diagnosis of PTL were reviewed in this retrospective study. Overall, 69.39% patients were aged >60 years (range: 30–87years, median age: 63 years). Bilateral testicular involvement was reported only in 3 of 49 patients. Thirty patients had non-GCB subtype based on immunohistochemistry. The Ann Arbor clinical stage was as follows: stage I in 29 (59.18%) patients, stage II in 5 (10.21%) patients, stage III in 6 (12.24%) patients, and stage IV in 9 (18.37%) patients. Thirty-four patients had lower IPI scores (risk stratification was low and intermediate-1). In addition, CNS involvement was reported in three patients. A summary of the main clinical characteristics of all patients is presented in .
Table 1. Clinical characteristics.
Treatment
In our study, 6 patients (12.24%) underwent orchiectomy only as a diagnostic and initial therapy. One patient received conservative treatment (without chemotherapeutic agents) because of advanced age, and 2 patients received chemotherapy alone without orchiectomy. Twenty-nine patients (59.18%) received inguinal orchiectomy and systemic chemotherapy. In addition, 11 patients (22.45%) received systemic chemotherapy and RT after inguinal orchiectomy. Of all patients who received chemotherapy, 1 received rituximab alone; other patients’ chemotherapy regimen contained multiple drugs. The details are presented in and . Four patients received R-hyper CVAD/MA chemotherapy, 23 patients received R-CHOP chemotherapy, 8 patients received R-CHOP combined with higher doses of MTX, and 6 patients received CHOP chemotherapy. Among the whole cohort, prophylactic intrathecal injection (ITH) was performed in 24 patients.
Table 2. Treatment.
Table 3. Chemotherapy regimen.
Outcomes
At a median follow-up time of 39.5 months (range: 2–158 months, average: 48.08 months), only 1 patient was lost to follow-up after orchiectomy. Thus, 48 patients were evaluated for their therapy response. CR was achieved in 34 (70.83%) patients, and PR was achieved in 3 patients. PD was detected in 11 (22.92%) patients, and 10 (20.83%) patients had died at the time of the final follow-up because of PTL progression. The average PFS was 43.92 months (range: 2–158 months), and the average OS was 47.55 months (range: 2–158 months). For all patients, the 3-year OS was 53.06%.
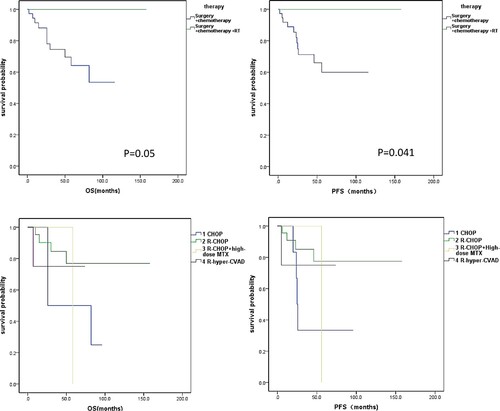
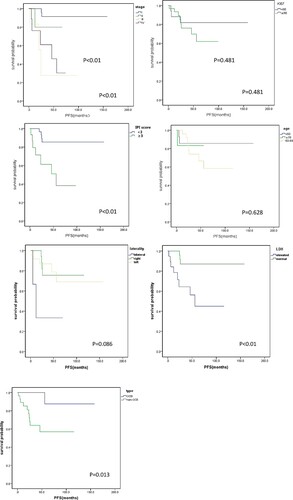
and lists the survival analysis (log-rank test) based on different characteristics for OS and PFS. In our study, we evaluated the influence of age, laterality, histotype, Ann Arbor stage, IPI score, LDH levels, and Ki-67 expression. The results indicated that Ann Arbor stage, IPI score, and LDH were associated with OS, while Ann Arbor stage, IPI score, LDH, and histotype were significantly associated with PFS.
Figure 1. OS of patients with primary testicular lymphoma. Kaplan-Meier survival curves by stage, Ki-67, risk-stratification, age, laterality, LDH and type.
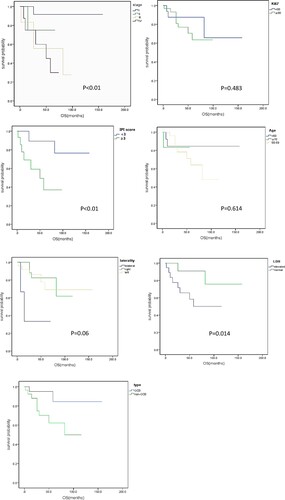
Figure 2. PFS of patients with primary testicular lymphoma. Kaplan-Meier survival curves by stage, Ki-67, risk-stratification, age, laterality, LDH and type.
Among the six patients receiving orchiectomy alone, one was lost to follow-up, and the remaining five patients all had stage I or II disease and achieved CR after orchiectomy. They had no signs of relapse as of the last follow-up. One patient who received prednisone monotherapy ultimately died 2 months after diagnosis. One patient received rituximab monotherapy combined with local radiation after orchiectomy, and also achieved CR without relapse. Four patients were treated with R-hyper CVAD/MA regimen:1of these whom died after undergoing four cycles of therapy because of PTL progression, the remaining patients all achieved CR and did not show relapse as of the last follow-up date.
In total, 11 patients underwent orchiectomy combined with chemotherapy and RT. Twenty-nine patients underwent only orchiectomy and chemotherapy. Survival curves showed that RT had significant effects on patients’ PFS; however, the P-value was 0.05 in the survival curves of OS. Hence, we believe that there were no statistically significant differences. However, the small sample size also has an impact on the outcome. We compared the differences in outcome of the chemotherapy regimen of R-CHOP, CHOP, and R-CHOP combined with high-dose MTX, and the results suggested that there were no significant differences among the three regimens. Nonetheless, if the significance standard were adjusted to P < 0.1, the difference in outcomes between the CHOP and R-CHOP groups would be statistically significant (OS: P = 0.057, PFS: P = 0.074), with patients receiving the R-CHOP regimen having significantly longer PFS and OS. Again, the sample size also had an impact on the result ().
Discussion
PTL is a rare malignancy with poor prognosis and is most common in men over 60 years. Most studies about PTL are retrospective, and prospective controlled studies are lacking because of the lower prevalence of PTL and the age distributions. The most common clinical symptom of PTL is a painless testicular swelling, with no specific presentation. In our study, bilateral testicular swelling was seen in 4.1% (2/49) patients. This proportion was lower than that in other studies and is likely related to the small sample size [Citation5]. Most cases were diagnosed in the early stage of the disease (stage I–II), and patients with isolated bilateral involvement of the testes were considered as having stage I disease, because their prognosis was similar to those with stage I/II disease [Citation6]. Gundrum et al. reported that about 70% patients were in stage IE or IIE at the first diagnosis and had better prognosis than patients in stage III and IV [Citation7]. In our study, 69.38% cases were diagnosed in stage I/II; in addition, they had longer PFS and OS than patients in stage III and IV, which was consistent with other studies. All patients underwent inguinal orchiectomy and the histopathological diagnosis was PTL. The large majority of PTL (>80%) are diffuse large B-cell lymphoma (DLBCL). Rare histologies include mantle cell lymphoma, extranodal NK-cell lymphoma, and peripheral T-cell lymphoma [Citation2]. In our study, all 49 patients had DLBCL, so we cannot comment on patients with different histologies.
It is worth noting that the OS and PFS of patients with PTL gradually improved over the past decades because of the advancements in therapeutic regimens. However, PTL is still a kind of extranodal lymphoma with high relapse rate. To date, several studies have explored the prognostic factors of PTL. For the majority of patients with limited-stage PTL, the IPI is typically < 2; therefore the IPI scores have limited prognostic utility. The MD Anderson Cancer Center have previously reported that Ann Arbor stage III/IV, high LDH, B-symptoms, and higher IPI scores were associated with shorter PFS and OS [Citation8]. Xu et al. reported a large retrospective study of 1169 cases and showed that age, Ann Arbor stage, histologies, and time period of diagnosis were independent prognostic factors [Citation9]. A study including 769 cases based on the SEER databases in 2009 and another study from China including 32 cases conducted in 2011 showed that left testicular involvement was negative prognostic factors for overall survival [Citation7,Citation10], while our study didn’t found that. Collectively, based on our study and other studies, we believe that age, Ann Arbor stage, B-symptoms, mass size, LDH level, and left testis involvement are associated with the outcome of patients with PTL.
Some studies have suggested that PTL patients in stage IE could achieve better outcome by using local treatment regimens like orchiectomy alone or local radiation. In our study, six patients received orchiectomy alone, five of whom achieved CR without relapse. Indeed, the short follow-up time also had an influence on these results. With further developments in medical research, PTL treatment has seen dramatic progress. Despite this, its overall prognosis remains poor, and the relapse rate high, especially CNS relapse, because of the biologic features. Therefore, to ameliorate the high risk of CNS relapse, IT chemotherapy is recommended. In our study, prophylactic ITH was performed in 24 patients, two patients with CNS relapse, we didn’t analyze the effect of ITH on CNS relapse because of the small sample. To date, a combined modality therapy consisting of orchiectomy and chemotherapy is recommended for PTL. Some studies have suggested that combining RT with chemotherapy and orchiectomy can significantly prolong PFS and OS [Citation11], which is similar to our study. The National Comprehensive Cancer Network (NCCN) guidelines [Citation12]have recommended RT to the contralateral testis as a part of treatment to reduce the relapse rate, and many studies have confirmed this opinion so far [Citation11,Citation13]. The ESMO Clinical Practice Guidelines suggest that orchiectomy remains a mandatory step for therapy; 6–8 cycles of R-CHOP given every 21 days is the current standard treatment, and RT to the contralateral testis is strongly recommended [Citation14]. However, in real-life conditions, the final decisions regarding the therapy regimen is made by the patients, and while the treatment regimens are recommended, not all patients follow them. Therefore, there are always some patients that do not agree with the recommendation for contralateral testicular radiation, likely due to the rising cost of treatment or the fears associated with therapy.
Rituximab plus CHOP is one of the most commonly used therapy regimens to date. As is known, the outcome of CD20-positive nodal DLBCL has been improved significantly after the application of rituximab; however, rituximab cannot effectively penetrate the blood-testicle barrier, so its concentration is minimal in the testicles. Conflicts exist about the effective use of rituximab [Citation3,Citation15]. In 2018, a retrospective study of 32 cases from China found that bilateral intervention (contralateral RT or resection) could improve OS and PFS in the rituximab group [Citation16], but in the other that did not use rituximab, patients who performed unilateral or bilateral intervention had a similar OS and PFS. In our retrospective study, we also found differences in the outcome between the R-CHOP and CHOP group, with a P-value >0.05 but <0.1 in the PFS and OS curves. Although we believe this is meaningful, it is also perhaps related to the small sample size of patients that received the CHOP regimen. Use of dose-intensive strategies such as hyper-CVAD are limited because of the usual demographic features of patients with PTL. In our study, only four patients received the hyper-CVAD regimen, illustrative of the limited use of dose-intensive strategies.
In conclusion, PTL is a rare malignancy with high mortality. Most patients are >60 years old, and the available dose-intensive strategies are limited in this age group. R-CHOP-based chemotherapy combined with inguinal orchiectomy and RT are recommended. Immunomodulators like lenalidomide and the inhibitor of Bruton’s tyrosine kinase ibrutinib are being gradually used on patients with PTL, but further prospective studies are needed to better understand PTL and validate therapeutic options.
Compliance with ethical standards
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Vitolo U, Chiappella A, Ferreri A J, et al. First-line treatment for primary testicular diffuse large B-cell lymphoma with rituximab-CHOP, CNS prophylaxis, and contralateral testis irradiation: final results of an international phase II trial. J Clin Oncol. 2011;29(20):2766–2772.
- Cheah C Y, Wirth A, Seymour J F. Primary testicular lymphoma. Blood. 2014;123(4):486–493.
- Deng L, Xu-Monette Z Y, Loghavi S, et al. Primary testicular diffuse large B-cell lymphoma displays distinct clinical and biological features for treatment failure in rituximab era: a report from the international PTL consortium. Leukemia. 2016;30(2):361–372.
- Cheson B D, Fisher R I, Barrington S F, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059–3068.
- Chen B, Cao D H, Lai L, et al. Adult primary testicular lymphoma: clinical features and survival in a series of patients treated at a high-volume institution in China. BMC Cancer. 2020;20(1):220–230.
- Go R S, Gundrum J D. Uncertainty and discordance in the staging and prognosis of diffuse large B-cell lymphoma with isolated bilateral testicular involvement. Am J Hematol. 2009;84(11):762–763.
- Gundrum J D, Mathiason M A, Moore D B, et al. Primary testicular diffuse large B-cell lymphoma: a population-based study on the incidence, natural history, and survival comparison with primary nodal counterpart before and after the introduction of rituximab. J Clin Oncol. 2009;27(31):5227–5232.
- Mazloom A, Fowler N, Medeiros L J, et al. Outcome of patients with diffuse large B-cell lymphoma of the testis by era of treatment: the M. D. Anderson Cancer Center experience. Leuk Lymphoma. 2010;51(7):1217–1224.
- Xu H, Yao F. Primary testicular lymphoma: A SEER analysis of 1,169 cases. Oncol Lett. 2019;17(3):3113–3124.
- Cao B, Ji D M, Zhou X Y, et al. A clinical analysis of primary testicular diffuse large B-cell lymphoma in China. Hematology. 2011;16(5):291–297.
- Conrad A L, Go R S. Contralateral testicular relapse after prophylactic radiation in a patient with primary testicular diffuse large B-cell lymphoma. Eur J Haematol. 2009;83(6):603–605.
- Zelenetz A D, Gordon L I, Wierda W G, et al. Diffuse large B-cell lymphoma version 1.2016. J Natl Compr Cancer Netw. 2016;14(2):196–231.
- Ollila T A, Olszewski A J. Radiation therapy in primary testicular lymphoma: does practice match the standard of care?. Leuk Lymphoma. 2019;60(2):523–526.
- Vitolo U, Seymour J F, Martelli M, et al. Extranodal diffuse large B-cell lymphoma (DLBCL) and primary mediastinal B-cell lymphoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v91–v102.
- Kridel R, Telio D, Villa D, et al. Diffuse large B-cell lymphoma with testicular involvement: outcome and risk of CNS relapse in the rituximab era. Br J Haematol. 2017;176(2):210–221.
- Ma R Z, Tian L, Tao L Y, et al. The survival and prognostic factors of primary testicular lymphoma: two-decade single-center experience. Asian J Androl. 2018;20(6):615–620.