ABSTRACT
Background
Self-injection, particularly of biologics, has become a mainstay of chronic disease management. Despite labeling requirement for healthcare provider (HCP) training, current injection initiation experiences have been shown to be suboptimal. This study characterizes gaps in training and support during initiation and identifies rationales to inform solutions.
Methods
We enrolled HCPs (n = 18) performing routine biologic initiation and patients (n = 24) currently self-injecting biologics. Participants completed activities through an online, remote ethnography tool. We conducted two focus groups with biologic-naïve patients (n = 5). Data was analyzed using thematic frameworks, Q methodology, and quantitative assessments.
Results
Our results suggest considerable gaps exist. Analysis revealed five common themes that could explain these gaps: 1) minimal biologic-specific professional instruction is provided to HCPs; 2) nuanced injection use-steps are not universally understood; 3) no one stakeholder currently ‘owns’ training; 4) support offered by HCPs and manufacturers is perceived as biased; and 5) emotional burden is not accounted for.
Conclusions
Our study suggests optimizing several elements to facilitate successful initiations, including structured sessions, improved HCP injection device knowledge, demo-device practice, and focus on both emotional and mechanical aspects. Aligning these factors has potential to increase patient confidence, reduce burden on HCPs, and improve probability of success on therapy.
1. Introduction
The rise in multimorbidity has resulted in nearly 40% of patients viewing their treatment burdens as unsustainable[Citation1]. Self-injection, particularly of biologics, has become a mainstay of chronic disease management, partly to address elements of burden associated with in-clinic administration [Citation2,Citation3]. Self-injection is a high-accuracy task, and improper technique may have implications for both clinical outcomes and patient adherence. A systematic review of injection technique in patients with diabetes found that correct technique was associated with improved outcomes in several studies[Citation4]. Similarly, early patient competence with self-injection has been shown to be predictive of adherence to therapy[Citation5]
Human factors engineering focuses on simplifying devices and instructions to eliminate common sources of error[Citation6]. However, patients still make errors with drug delivery devices despite them being ‘simple’ in terms of number of use steps[Citation7]. One study reported that over 84% of patients are not able to properly use autoinjectors (AIs) and over half of those patients routinely miss three or more use steps[Citation8]. Injection products often have a labeling requirement for healthcare provider (HCP) training prior to self-administration [Citation9,Citation10]. However, despite the labeling requirement, HCP training is far from consistent, with more than 40% of physicians acknowledging they do not train patients at all[Citation11]. Moreover, there is currently very little guidance on how HCPs should train patients, as product labels do not specify what constitutes adequate training. This can lead to variability in training practices. One ethnographic study found that some institutions follow extensive, internally developed protocols for training and follow-up, while others barely train and have little to no follow-up at all[Citation12].
Inconsistencies also exist regarding the injection devices themselves, which can create further training challenges. The significant rise in self-injection therapies within the last two decades has placed a plethora of devices on the market, many of which look and function slightly different. Devices not only differ in respect to features (e.g. injection time, audible and visual feedback, safety caps) but also in critical use steps (e.g. method of actuation). It is also not uncommon for patients to be p7rescribed more than one self-injected therapy (either concurrently or in succession), and they may wrongfully attribute the characteristics of one device to another. In fact, studies have already considered the potential for medication errors related to look-alike ‘platform’ devices used for multiple molecules[Citation13].
In terms of content, labeling elements (e.g. prescribing information) relay technical information required to use injection devices and medications safely – the mechanics of self-injection. However, for many patients, knowledge of mechanics alone is not sufficient to relieve persistent apprehension and anxiety associated with self-injection[Citation14]. This emotional angst is well characterized and multifactorial, and includes concerns about incorrect technique, fear of side effects, lack of self-confidence, stigma of illness and social embarrassment, frustration with illness and treatment, and anxiety associated with needles[Citation15]. Although patient satisfaction has been found to be higher when both knowledge and emotional needs are met[Citation16], HCPs may neglect the emotional aspects of training[Citation14], which can cause otherwise capable patients to never start or discontinue self-injection therapies [Citation17,Citation18].
Finally, HCPs themselves may lack the capacity to adequately train patients despite their best intentions. In the current healthcare environment, physicians must contend with shortened time blocks for each patient and decreasing proportions of face-to-face time [Citation19,Citation20]. Time constraint has been cited as a significant barrier to performing in-office inhaler training, with physicians forced to deprioritize training to make room for other tasks[Citation21]. Similarly, in an ethnographic study of biologic initiations, discussion of biologic therapy was often limited in a single visit[Citation22]. HCP experience with injection devices and knowledge of technical nuances may also vary amongst practice specialties according to the prevalence of biologic treatments in clinical guidelines. In a survey of pediatricians on the use of several variants of EpiPen, only 18% of physicians were found to be familiar with and demonstrate correctly at least 1 device[Citation23].
The combination of these barriers to improved injection training suggest a significant need to revisit the paradigm for biologic initiation. The intent of this study was to better understand current practices in biologic initiation and self-injection training, identify areas for improvement, and characterize innovation opportunities for both patients and HCPs.
2. Study design and methods
2.1. Study design
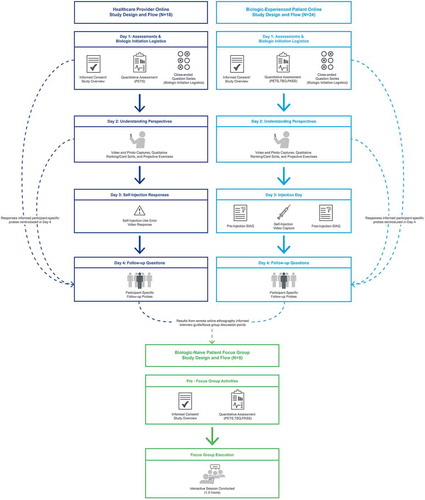
This was a mixed-methods study of HCPs experienced in biologic injection initiation and patients formally diagnosed with one of several chronic diseases treated with self-injection. The primary objective of this study was to characterize gaps in technical training and patient support throughout the biologic initiation phase from the perspective of both patients and HCPs. The secondary objective was to identify the rationales for these training gaps in order to inform effective solutions in future development. Participants completed a series of activities asynchronously through a moderated, online, remote ethnography tool. These activities included closed-ended question series, participant-provided video and photo captures, card sorting, and projective exercises. At the completion of remote ethnography activities, real-time focus group interviews were conducted with self-injection-naïve patients to explore and compare their expectations at initiation to the experiences of current biologic self-injectors. provides a representation of the overall study design and activity sequence. All study procedures were conducted in accordance with the 1964 Declaration of Helsinki and its subsequent revisions. This article describes a non-interventional study and did not involve any new studies of human or animal subjects performed by any of the authors.
2.2. Participant recruiting
Recruiting was performed throughout the United States using commercially available, nation-wide panels of HCPs and patients with chronic disease. Participants completed an informed consent document outlining steps taken to protect their privacy and study logistics (participation time, topics of focus, and required submissions). We excluded participants who expressed discomfort in taking photos and videos. Participants were compensated financially, and both participants and the study sponsor were blinded to each other’s identities.
We recruited HCPs with routine experience (defined as daily or weekly occurrence) training patients to self-inject biologic medications using an AI or prefilled syringe (PFS). We recruited a balanced sample across professional titles (physicians/physician’s assistants, nurses/nurse practitioners, and nurse educators) from the following eight clinical specialties to represent diverse practice settings and varying biologic experience: neurology, rheumatology, gastroenterology, endocrinology, cardiology, allergy/immunology, dermatology, and primary care. In addition to professional title and specialty, recruiting was structured to provide participants with a mix of facility geographies and sizes (measured by number of biologic starts and patients seen per month).
We recruited adult patients (at least 18 years of age) currently self-injecting a biologic at home for the treatment of a chronic disease. The recruiting screener was designed to include patients with a range of biologic experience and number of previous injection therapies. We recruited from the following nine chronic disease areas to account for variability in marketed biologics: psoriasis/psoriatic arthritis (PsO/PsA), rheumatoid arthritis (RA), multiple sclerosis (MS), ulcerative colitis/Crohn’s disease (UC/CD), systemic lupus erythematosus (SLE), migraine, type 2 diabetes, severe asthma, and hypercholesterolemia. Selected chronic disease areas were intentionally aligned to clinical specialties targeted in HCP recruiting to enable comparison and contrasting of experiences in lieu of a more complex, dyadic recruiting strategy. To control for bias toward self-injected medications that are more common or those that have been on the market for longer periods of time, we established medication quotas to ensure diversity within disease areas and avoid over-representation. We also recruited a small sample of adult patients with the aforementioned chronic diseases who were currently managing their diseases with non-biologic therapies. These participants had no prior experience with biologics or self-injections and were recruited as a proxy for biologic-naïve patients who would be newly initiated on self-injection therapy.
2.3. Data collection
At the study outset, all participants completed quantitative assessments and survey questions about their biologic initiation experiences (patients) and facility practices (HCPs). Parallel assessments for patients and HCPs were developed (Supplemental File – Table S1) from the existing Patient Experience with Treatment and Self-Management (PETS) measure to facilitate comparative analysis in the perceived difficulty of treatment management[Citation24]. Patient participants also completed the Self-Injection Assessment Questionnaire (SIAQ) and the Treatment Burden Questionnaire (TBQ) with Patient Acceptable Symptom State (PASS) [Citation25,Citation26]. Assessment data were used during the study as well as for post-hoc analysis of burden of treatment. Patient-provided responses and results of SIAQ, TBQ, and PASS were used to reintroduce participant-specific follow-up probes for a more in-depth understanding. This adaptive approach was used to improve the specificity and fidelity of participant responses after the initial unaided data collection discussed previously.
Patients were asked to passively video record their injections on their scheduled injection days. If scheduled injections did not align with the study fielding, patients verbally walked through the process. The injection recordings were not assessed for correctness but rather to provide insight into the experience and allow researchers to verify participant authenticity. HCP participants were probed with four publicly shared self-injection clips to assess their recognition of correct injection technique. Researchers used search terms including ‘chronic illness’ and ‘self-injection’ to locate public videos on YouTube. Specific clips were chosen as stimuli because each depicted one or more use errors in the self-injection process. Use errors were identified through direct comparison with the corresponding products’ instructions for use. HCPs recorded their live responses to these videos upon initial viewing, and their recognition of use errors was defined as any verbal expression of awareness.
The mixed-method nature of the study design was intended to provide ‘thick’ descriptive data and enable the research team to reach data saturation with a smaller sample[Citation27]. As qualitative data accumulated, researchers evaluated for saturation, taking into consideration the five dimensions suggested by Malterud and colleagues: study aim, sample specificity, use of established theory, quality of dialog, and analysis strategy[Citation28]. Given our narrow study scope, specific participant sample, and robust study design, once themes were repeatedly observed, without the birth of new ideas[Citation29], data saturation was determined, and collection was halted.
Data from biologic-naïve patient participants was collected in two focus groups (n = 2 participants present for each session) and one interview (n = 1 participant) conducted through an encrypted video conferencing platform. All participants completed informed consent prior to the focus group. Each focus group lasted 1.5 hours, and sessions were recorded for later coding and analysis. A single experienced moderator (AR) conducted all sessions. The interview guide used for each focus group was informed by results collected from the remote ethnography study and was developed prior to the first focus group. Activities consisted of structured discussion between participants using prompts, visual stimuli, and probes from the moderator. The moderator encouraged all participants to share responses, consistently rotating the order of speakers and ensuring that all participants were respected and heard[Citation30].
2.4. Data analysis
Video and open-ended submissions were collected, transcribed, and coded by the moderator (AR) and an assistant. Initial coding was executed as participants completed each activity to develop an opening codebook, followed by an iterative process of reviewing and refining coding sequences to develop mutually exclusive themes, similar to what has been described by Baggot and colleagues[Citation31]. Thus, data collection and analysis occurred concurrently. Qualitative data was analyzed using thematic frameworks[Citation32], grouping themes and subthemes to illustrate the reality of biologic initiation from HCP and patient perspectives, as well as the various disconnects observed among the sample groups. Participants completed qualitative ranking through card sorts to generate clusters (factors) of alike perspectives across samples.
Both HCPs and patients completed a card sort regarding perceived importance across 16 injection-related topics. HCPs completed a second card sort involving 25 patient characteristics and the influence on their training approach. We analyzed the card sorting data using Q methodology[Citation33]. Q methodology analysis was performed using Pearson correlation, principle component extraction, and varimax factor rotations. Due to the subjective and exploratory nature of the analysis, various criteria were considered when selecting the number of factors[Citation34]. For the injection-related topics card sorts, factors were extracted using Humphrey’s Law with parallel analysis[Citation35]. Factors were extracted from the patient characteristics card sort using the Kaiser–Guttman rule (eigenvalues >1)[Citation36].
Quantitative analysis was used to identify differentiating variables in the impact of biologic initiation and treatment burden. Given the small sample size, quantitative assessment variables were compared between independent groups using Kruskal–Wallis tests (Wilcoxon tests in the case of a binary independent variable). When appropriate, post-hoc comparisons were calculated using a Dunn test. All analyses used a two-sided Type I error of α = 5%. Quantitative variables were compared against one another using Pearson correlations.
2.5. Participant and public involvement
There was no patient or public involvement in the study design, management, or results generation.
3. Results
3.1. Participant characteristics
A total of 42 participants completed the remote study, including 24 biologic-experienced patients across nine chronic disease areas and 18 HCPs across eight clinical specialties. An additional 10 participants (5 biologic-experienced patients and 5 HCPs) were enrolled but replaced with participants of similar demographics during fielding due to unresponsive communication and lack of progress despite repeated follow-up attempts. Focus groups were held with a total of 5 biologic-naïve patients. A summary of baseline demographics for both biologic-experienced and biologic-naïve patients is presented in and for HCPs in .
Table 1. Patient participant characteristics
Table 2. HCP participant characteristics
3.2. Gaps in technical training and patient support
3.2.1. Time crunch
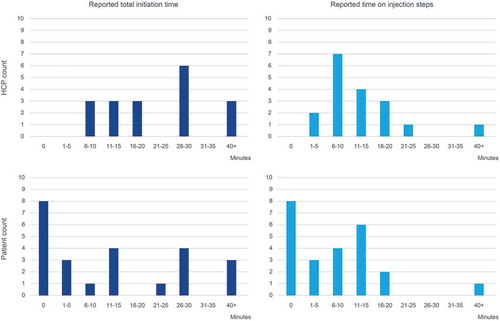
HCPs reported they spent an average of 28 minutes (range: 10–90 minutes, median: 25 minutes) with patients during biologic initiation. Of the total time, an average of 16 minutes (range: 5–70 minutes, median: 12.5 minutes) is spent focused on instruction on injection steps; the remaining time is used for additional topic discussion aside from injection steps. HCPs who reported longer session times did not use additional training materials compared to those HCPs with shorter session times; however, the two highest reporting HCPs offer 2 sessions for in-office biologic initiation, and the time they reported comprised both sessions. Patient participants estimated that the amount of time spent on their biologic initiation was 24 minutes total (range: 1–90 minutes, median: 20 minutes), with 13.5 minutes (range: 1–45 minutes, median: 15 minutes) focused on instruction on injection steps. Both of these times were comparable to those reported by HCP participants, and the patient reporting the highest time also received 2 sessions of in-office biologic initiation ().
3.2.2. Demonstration of injection steps
HCPs reported that their instruction on injection steps begins with a HCP-provided demonstration; 100% (18/18) HCPs report providing some form of visual demonstration, 22% (4/18) consistently use real devices containing medication as props, and 78% (14/18) report using a demo-device or ‘training’ device. Of the 78% (14/18) HCPs who use a demo-device, 67% (12/18) allow the patient to demonstrate their technique back to them. This ‘teach-back’ method allows HCPs to offer just-in-time feedback and corrections during the session (Supplemental File – Table S2). However, 61% (11/18) HCPs reported that a limited number of demo-devices are available in their facility, which precludes patients from taking devices home for subsequent practice (Supplemental File – Table S3). In times when an appropriate demo-device is not available, HCPs reported they may perform a demonstration with a real device containing medication, using the device purely as a prop.
Patient participants reported that their HCPs used demonstrations and demo-devices far less frequently. Of the full sample of patients (n = 24), only 50% (12/24) reported receiving a visual demonstration from an HCP; 29% (7/24) demonstrations were performed with a demo-device and 21% (5/24) with the patients’ real devices containing medication. Of the seven patients who received demonstrations with a demo-device, only 13% (3/24) reported having the opportunity to return the demonstration to their HCP for feedback (i.e. teach-back).
3.2.3. Biologic initiation topics
Beyond demonstration and discussion of injection steps, we also characterized other discussion topics related to biologic initiation (). HCPs reported that the most frequently discussed topics included dosing frequency, overview of device features, post-injection/disposal information, and storage information (94% of HCPs reported they always discuss). In contrast, 50% or fewer HCPs reported discussing topics like managing emotions and injection-related anxiety, differences in new and prior injection devices, traveling with biologics, and lifestyle fit/personal impact. For patients, the frequencies of topics discussed were much more inconsistent, with only one topic (dosing frequency) appearing with greater than 50% discussed during training. For the majority of topics, many patients reported that they either learned the topic on their own or did not learn it all during the initiation phase. Of note, these percentages reflect the full sample of patients (n = 24), of which eight patients uniformly reported that they received no training. When only those patients who received training were considered (n = 16), topics appeared with higher frequencies, although these values were still lower compared to those reported by HCPs (Supplemental File – Table S4).
Table 3. Frequency of injection-related content relayed
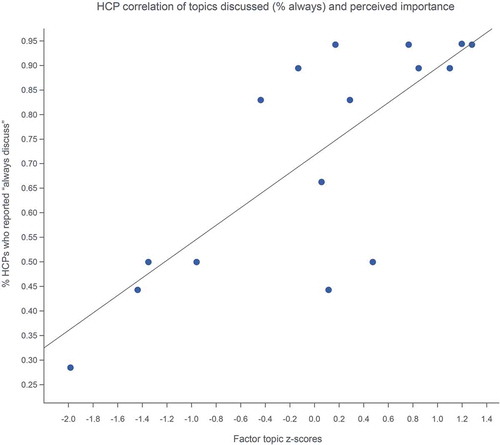
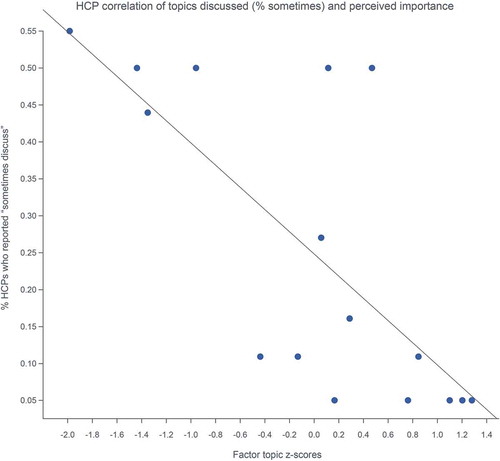
We hypothesized that due to time constraints, HCPs are forced to prioritize aspects of training they perceive as most important. In the HCP topic importance card sort, Q methodology factor rotations revealed only one significant factor, implying that HCPs largely agree on information importance. This factor perceived highest importance in discussing dosing frequency [z-score = 1.2785], device features [z-score = 1.2078], and injection preparation [z-score = 1.2785]. Prescribing information [z-score = −1.9844], lifestyle/personal fit [z-score = −1.4355], and information on traveling [z-score = −1.3597] were topics perceived as least important to discuss with patients (Supplemental File – Table S5). Moreover, consistent topic coverage (% always discuss) was strongly correlated to the factor importance ratings (r = 0.77), indicating that HCPs are more likely to talk about topics they view as important (). Conversely, reduced or infrequent topic coverage (% sometimes discuss) was negatively correlated to factor importance ratings (r = −0.734), suggesting that HCPs skip topics they perceive as less important when faced with time constraints ().
Analysis of the parallel patient topic importance card sort, however, revealed three factors representing three clusters of patient opinion. Of the three factors, both Factors 1 and 3 perceived that reviewing the quick reference guide was of highest importance. Topics distinguishing perceived importance within each group included: Factor 1) injection preparation [z-score = 1.1986] and drug safety [z-score = 1.1972]; Factor 2) establishing medication management routines [z-score = 1.8011] and storage information [z-score = 1.3270]; and Factor 3) dosing frequency [z-score = 1.0278] and device features [z-score = 0.8530] (Supplemental File – Table S6). Qualitatively, patient participants with experience on one biologic therapy tended to cluster toward Factor 1, suggesting that these patients prioritize the technical basics of injection. Patients with experience on more than 1 biologic therapy tended to split between Factor 2 and 3; Factor 2 prioritizes fitting injections into their lifestyle and Factor 3 prioritizes device and dosing differences between new and prior therapies. Compared to HCPs, there seemed to be less association between topic importance and reported frequency for patients. Correlations were seen among Factor 1 prioritizing what was taught by their HCP (r = 0.156), Factor 2 prioritizing what was taught by their HCP (r = 0.252) and what they learned on their own (r = 0.355), and Factor 3 prioritizing what they learned on their own (r = 0.153). To some extent all factors deprioritized what they did not learn (r = −0.0145, −0.583, −0.099, respectively). See Supplemental File – Table S7 for a full breakdown of correlations within the factors.
3.3. Rationale for training gaps
Qualitative analysis of participant responses revealed several potential reasons for the training gaps presented above. Five consistent themes emerged: 1) HCPs receive minimal biologic-specific professional instruction; 2) nuanced injection use-steps are not universally understood; 3) no one stakeholder currently ‘owns’ the training process; 4) support offered by HCPs and manufacturers is perceived as biased; and 5) the emotional burden of self-injections is not accounted for.
3.3.1. HCPs receive minimal biologic-specific professional instruction
HCPs reported the average professional training they received on a yearly basis is 45 hours; of that, only 6.9 hours are focused on biologic initiation for patients (15.3% of total yearly professional training). Pharmaceutical representatives from specific biologic brands are commonly reported to visit most prescribing facilities on a monthly basis. HCPs indicated such visits are brief (5–30 minutes) but tend to occur during ‘inconvenient’ working hours, when patients are present. HCPs reported that their interactions with representatives are focused on receiving medication samples, new statistical data, and adverse event reporting, rather than current product refreshers and/or training verifications (Supplemental File – Table S8).
Beyond training received during years of formal schooling, only 28% of HCP participants reported ever receiving any form of ‘soft skill’ education (workshops, self-elected courses, employer-provided), and of the facilities represented in the study, only 33% have a clinical educator on staff. As a result, HCPs reported that they undergo a trial-and-error cycle throughout their biologic initiation experiences, using each interaction as a data point to refine their heuristics for managing patients. HCPs reported that maintaining eye contact, offering direct hands-on participation, and communicating with a calm demeanor are successful practices to include during injection training. They have also learned to avoid speaking ‘at’ patients/reading from a script, rushing the session, and overwhelming patients with information (Supplemental File – Table S9). Through this process of trial-and-error, it appears HCPs develop individual heuristics regarding patient characteristics and when more tailored training may be appropriate. In the HCP card sort involving patient characteristics and their influence on training approach, HCPs expressed high consideration for patients’ physical abilities to self-inject (e.g. tremor, limited eyesight), previous injection experience, device type (AI vs. PFS) and anxiety associated with injections. Similarly, the sample collectively neglects characteristics such as patients’ gender, level of education, and BMI. However, HCPs’ mental models for training customization clusters into 6 factors, each placing importance on varying patient characteristics. The distinguishing considerations in each factor for customization were: Factor 1) learning style [z-score = 1.2153] and comorbid conditions [z-score = 1.0564]; Factor 2) number of previous injectables used [z-score = 1.4381] and duration of use [z-score = 1.4171]; Factor 3) reading level [z-score = 1.4913] and social/support needs [z-score = 1.3686]; Factor 4) language barriers [z-score = 0.9798] and ability to use technology [z-score = 0.9798]; Factor 5) demo-device availability [z-score = 1.8194] and caregiver involvement [z-score = 0.9097]; and Factor 6) age [z-score = 0.9798] and resources offered by the drug brand [z-score = 0.9798] (Supplemental File – Table 10).
3.3.2. Nuanced injection use-steps are not universally understood
When presented with videos of self-injections, HCPs in our study had surprisingly little recognition for the use errors that occurred. Use errors in the stimuli included lack of acknowledgment of the injection window, lack of proper skin manipulation (i.e. stretch or pinch), inappropriate injection site (i.e. too close to the navel), and incomplete dose due to leaking (i.e. ‘wet injection’). Overall, with the exception of the incomplete dose error, the majority of HCPs did not recognize these injection-related issues and those who did correctly identify them did not come from any one particular specialty. Notably, of the 12 HCP participants who recognized the wet injection error, 4 rationalized it as a normal occurrence ().
Table 4. HCP live responses to self-injection videos containing use errors
3.3.3. No one stakeholder currently ‘owns’ the training process
Patient participants overwhelmingly held their HCPs responsible (22/24; 92%) for biologic initiation. Patients who did receive instruction from their provider expressed that their in-person training was indispensable. Generally speaking, patients expressed an expectation that their prescriber should be well versed in the self-injection process and able to relay information to patients in layman’s terms. On the other hand, many HCPs view biologic initiation as a joint effort (13/18; 72%) between them and pharmaceutical manufacturers, as they rely on the resources offered by the biologic brand. While HCPs acknowledge their patient-facing responsibility, they do not view themselves as the sole providers of instruction and support (Supplemental File – Table S11).
3.3.4. Support offered by HCPs and manufacturers is perceived as biased
HCPs reported they feel their facilities and the medication brands offer ample support to patients. However, we observed major disconnects between the support patients receive and the support they perceive as valuable. Throughout the study activities, HCPs routinely minimized the difficulty of the injection experience and the value of demo-devices for patient training. This was apparent through numerous uses of phrases such as ‘self-explanatory,’ ‘incredibly simple,’ ‘straight-forward,’ and ‘easy.’ In general, HCPs viewed demo-devices in the context of one-time, in-office use, and did not consider that they could be employed beyond the initial training session. In contrast, patients noted that demo-devices would be useful to have at home to reinforce proper injection technique and set expectations for their actual injections (Supplemental File – Table S12).
HCPs reported they view materials offered by the biologic brands as sufficient and frequently refer patients to these sources. However, the majority of patient participants (15/24; 63%) expressed that the materials offered by biologic brands have shortcomings (Supplemental File – Table S13). They often reported that this information is ‘basic’ and ‘biased’ (7/15; 46%), displays an overwhelming amount of content and legal jargon (4/15; 27%), and lacks authenticity (4/15; 27%). Although this comparison did not reach statistical significance, when considering a holistic view of medical information, the PETS subscale assessment for medical information detected that HCPs find the process of locating and understanding medical information more difficult than patients do (median PETs: 20.5 vs. 17.5; p = 0.081). Notably, PETs scores were more consistent for HCPs, whereas the patients were much more variable, ranging from 14 to 22 (Supplemental File – Figure S1).
3.3.5. The emotional burden of self-injection is not accounted for
Considering all aspects of training, a third of patients within our study (8/24; 33%) reported they received no formal training with an HCP at all. These patients were found to have a significantly higher perceived burden of treatment as measured by TBQ compared to those who did receive training (median TBQ: 105 vs. 51; p = 0.008). TBQ scores were very consistent for patients who did not receive training, whereas the range in scores was more variable in patients who did receive formal training (Supplemental File – Figure S2). This may reflect the observed variability in content and quality of training previously discussed. Perceived ease of use with self-injection, as measured by SIAQ subscale, was also significantly higher in patients who received formal training (mean SIAQ: 6.25 vs. 8.73; p = 0.042) (Supplemental File – Figure S3).
Patients who did receive formal training were not spared from uncertainty about self-injection, however. Regardless of training experience, patients recalled a lack of preparedness and appropriate expectations about their injections once they were alone at home (10/24; 42%). They reported errors and near misses (4/24; 17%), negative physical feedback (9/24; 38%), including pain, bruising, and bleeding, and general feelings of emotional overwhelm (19/24; 79%) in their early injection experiences. Patients reported they do not vocalize these issues due to feelings of guilt associated with disease progression, prior negative experience with injectables, and embarrassment about injection anxiety/needle related fears (Supplemental File – Table S14).
3.4. Biologic-naïve focus groups
In general, the biologic-naïve patient group expressed acceptance that they may eventually require self-injection therapies for treatment – one participant described it as ‘inevitable.’ Patients had realistic expectations about who would train them (5/5 reported HCP, specifically the clinic’s nurse), where they would be trained (5/5 reported a clinical office), and what they might learn (technical steps, injection sites, adverse reactions). However, in certain instances, participants presented what we considered to be ‘high’ expectations, given the experiences/practices reported in the remote portion of our study. Expectations for total training time ranged from minutes to hours. Although patients found it difficult to establish specific time requirements for training, they agreed that visual demonstrations, repeated practice, and verbal discussion must be included in the session, however long that may take. Patients with no prior injection experience still preferred hands-on training, some even noting preference toward using a ‘dummy’ device to establish an expectation for required activation pressure and device handling. When asked to select between watching a demonstration done by a doctor or practicing the injection with a demo-device (resettable, no needle, no medication), 4/5 preferred practicing with a demo-device. The biologic naïve group also reported that not receiving any formal training would be unacceptable (Supplemental File – Table S15).
4. Discussion
4.1. Gaps in technical training and patient support
4.1.1. Time crunch
Our study suggests there are considerable gaps in technical training and patient support during biologic initiation, and inconsistencies in formal demonstration and verbal discussion of proper injection device use. Responses from both HCPs and patient participants support the hypothesis that when device training does occur in an office setting, it is typically a time-constrained, single-instance event. The average time spent on biologic initiation described in our study is consistent with the ranges reported elsewhere for typical visit durations [Citation19,Citation20,Citation22], with the highest reported times encompassing more than one training session. This single-session approach may have several limitations. Prior research suggests patients may be overwhelmed during a single visit, and providing information in an incremental and iterative fashion could reduce this emotional burden[Citation22]. Moreover, several studies have found that incorporating spaced repetition of training over time can enhance retention [Citation37,Citation38]. These multiple training sessions may provide ‘over-learning’ beyond what is required for initial proficiency, which may reduce knowledge and skill decay over time[Citation39]. Overall, distributing training in shorter, more frequent intervals is likely optimal, as it provides patients adequate time to absorb and retain information for the duration of their therapies.
4.1.2. Demonstration of injection steps
Both HCPs and patients reported that visual demonstrations were utilized during injection training, although there was significant discordance on the frequency at which those tools were employed. According to HCPs in our study, visual demonstrations are uniformly used, with most participants relying on demo-devices. This was not consistent with patient responses, as only half reported experience with visual demonstrations and a select few with demo-devices. Although we specifically enrolled HCPs from facilities where biologic training is routine, supplies of demo-devices were consistently reported to be limited. Beyond forgoing any potential benefit demo-devices may provide[Citation40], the absence of trainers forced some HCPs to rely on actual devices for injection training. As the real device is not actuated under these circumstances, this training method does not adequately represent key use steps associated with the injection itself, including proper pressure required for device activation, audiovisual device feedback (e.g. ‘clicks’ and viewing window changes), and appropriate holding time to allow for complete medication administration. Perhaps equally important, lack of availability of demo-devices restricts patients to a single demonstration or ‘practice’ session before self-injecting actual medication, as HCPs in our study reported they do not allow patients to take demo-devices home with them. This has similar implications to those discussed above, as single-session training sessions are limited when compared to use of spaced repetition.
When used beyond the initial training session, demo-devices may serve as a form of ‘just-in-time’ (JIT) training. JIT training provides the opportunity for ‘rolling refreshers’ on how to perform a procedure in real-time just prior to actual performance[Citation41]. This technique has been used successfully in areas analogous to injection where infrequent, accuracy-based tasks must be completed correctly, including cardiopulmonary resuscitation, lumbar puncture, intubation, cardiac surgery, and transvenous pacemaker placement [Citation42–46]. JIT may become increasingly important as the industry continues to develop injection products that are dosed infrequently. Although literature suggests patients prefer less frequent dosing for convenience [Citation47,Citation48], it is unclear how longer dosing intervals will impact patient education and retention of critical device-related information between administrations. Application of JIT principles has potential to offer real-time tips and recommendations that patients may forget from previous training or actual use.
Teach-back was another method employed by HCPs in our study. When delivered correctly, teach-back is an effective adult learning principle used to confirm understanding and facilitate patients’ role in their own training [Citation49,Citation50]. This method is widely used in practice, and the inclusion of teach-back in clinical counseling has been associated with increased patient satisfaction in medical education and disease management[Citation51]. While clearly successful, implementation of this practice is not ubiquitous. A cross-sectional analysis of diabetic patients in the U.S. described that only 25% of patients reported teach-back experience during their care[Citation49]. In our sample, an even smaller proportion of patients (13%) reported having experienced teach-back during biologic initiation, despite the majority of HCPs reporting they utilize it. This disconnect may suggest there is opportunity to better employ teach-back principles, possibly via other mediums than strictly in-person training.
4.1.3. Biologic initiation topics – frequency
Although we did not enroll HCP-patient dyads, our study results still suggest a major disconnect between the topics HCPs routinely discuss and what patients retain. HCPs reported they frequently discuss numerous topics during biologic initiation; however, patients expressed they learned far less during their training. One possible explanation for this information loss is memory decay, the natural physiological process of how retention of new information decays in the brain, which is consistent with evidence presented by the neuropsychologist, Roy Kessels. Kessels reported that 40–80% of medical information presented by HCPs is forgotten immediately, and of the information remembered, only half is remembered correctly[Citation52]. The concept of memory decay is well established in the literature, dating back to the works of Ebbinghaus in 1880, and has been since replicated by modern authors [Citation53,Citation54]. More recently, training decay has been recognized as relevant to combination products, resulting in the establishment of FDA working groups to set guidelines for testing devices[Citation37].
Another possible explanation is that some topics are truly more likely to be discussed during biologic initiation compared to others. Ignoring the difference in absolute frequencies reported by HCPs and patients, topics such as dosing frequency, injection preparation , drug safety information/side effects, and overview of device features were consistently among the most discussed, while managing emotions/injection-related anxiety and lifestyle fit/personal impact were consistently among the least. This finding is consistent with those observed by Schiff and colleagues, who described that limited resources may force HCPs to focus training on the mechanics of injection and neglect the emotional aspects patients may experience[Citation14]. Of note, the topic centered on explaining differences between new and prior injection devices was also infrequently discussed, which may be increasingly problematic as new injection devices are introduced into practice.
4.1.4. Biologic initiation topics – importance
Our results showed no obvious agreement in relative topic importance between the HCP and patient samples. In the HCP sample, there was a strong correlation between the frequency of topics relayed and their perceived importance. This correlation was less pronounced in the patient group, which may reflect the high degree of variability observed among our small sample of patients. Moreover, while some topics (e.g. dosing frequency) were considered uniformly important across the HCP and patient groups by Q methodology, others (e.g. establishing medication management routines, review of quick reference guide) had far less agreement. It is possible that patients’ perceived importance was influenced by their own experiences and how the information was initially relayed to them. In the aforementioned report by Kessels, the author argues that the amount of correctly recalled information is closely related to the subjective importance of the material. He goes on to recommend that HCPs place instructions at the beginning of their messages and express them specifically rather than generally to emphasize importance[Citation52]. It could therefore be the case that the perceived importance patients expressed in our study was influenced by what was most emphasized by their own HCPs during initiation or the chosen forum for instruction if formal training was not offered.
4.2. Rationale for training gaps
4.2.1. HCPs receive minimal biologic-specific professional instruction
Our study results support the hypothesis that very little formal guidance is provided to HCPs on biologic initiation, as nearly all HCPs reported relying on a trial-and-error approach to develop their practices. Although common patient communication and tailoring techniques emerged, they were not consistently practiced by HCPs and likely established through individual heuristics rather than established standards.
“My people skills come from about 40 years of interviewing many patients on a near daily basis. Most helpful in communicating with patients is to be real, calm, and go over the details of the injection step-by-step in a methodical, constructive way.” [P11 – Dermatology]
This concept of lack of standardization in physician-patient communication has been supported by prior literature. One early review of physician communication skills found little consistency in physician-patient communication techniques across the 26 studies analyzed[Citation55]. Another qualitative analysis of physician communication practices across 92 adult primary care visits in Southern California showed similar variation in behaviors; communication practices associated with patient dissatisfaction included rushing the session/not prioritizing patient time, interrupting patient speech, and failing to provide detailed explanations using simple language[Citation16]. Through trial-and-error, HCPs learn to adopt practices that produce positive patient responses and avoid those that do not. However, as many HCP participants reported in our study, this course correction takes years of experience and inevitably requires negative patient interactions to facilitate learning. A more structured, consistent resource centered on biologic initiation could avoid this issue and offer substantial benefit to both HCPs and patients.
4.2.2. Nuanced injection use-steps are not universally understood
Many HCPs in our study did not recognize common use errors when presented with videos of self-injection. We intentionally selected videos of patients using different injection devices to explore relative familiarity with the devices across the HCP specialties represented. Although it is difficult to draw any conclusions from this comparison given our small sample size and unequal distribution of specialties, there was one notable observation. Interestingly, our enrolled neurologist recognized no errors, while our cardiologists and endocrinologists only recognized errors associated with wet injections, the most commonly identified error overall. Considering the indications for the self-injected drugs depicted in the videos (mostly autoimmune diseases), it is unlikely any of these three specialties would have any experience with the devices shown. Although it is unclear if these HCPs would have recognized errors associated with devices more commonly used in their specialties, this finding may reflect the experience certain specialties have with injection devices relative to others. As more monoclonal antibodies and other therapeutic proteins are introduced into new disease areas, ensuring equal ability to adequately train patients regardless of HCP experience will become even more critical.
4.2.3. No one stakeholder currently ‘owns’ the training process
Patients in our study overwhelmingly expressed the expectation that the responsibility for biologic training lies with the prescribing clinician.
“I’m simply the person that got diagnosed with a disease that I don’t want - I’m the layman in this situation. I need someone who has given a shot before to teach me how to do it correctly, we do not understand how to do this. It’s your job to train me, not just to prescribe me.” [BxE3 – Multiple sclerosis]
To our knowledge, this is the first purposeful exploration of perceptions of ownership in self-injection training. One study did report that HCPs who did not perform self-injection training relied on pharmacies to do so[Citation11]. This presumption may produce similarly inconsistent training results observed in this study, as pharmacists’ ability to perform thorough injection device training may be dependent on location, dispensing model, and prior experience with injectable therapies [Citation56,Citation57]. Similar to patients, biologic brands explicitly designate trained professionals to take responsibility for training on their injection devices. However, our study indicates that HCPs do not share this viewpoint, and rather insist that self-injection training is a shared effort between themselves, pharmaceutical manufacturers, and patients.
“It is the responsibility of the HCP, patient, and manufacturer. It is a multifaceted responsibility. Obviously, the patients bear the brunt of the responsibility because they will be actually performing the injections.” [N3 – Rheumatology]
This position combined with limited time and resources may help explain the suboptimal training results described in this study. Based on commentary from HCP participants, it seems unlikely that all facilities will have the capacity to provide consistent biologic initiation experiences for patients, even under ideal circumstances. Moreover, HCPs expressed that pharmaceutical representatives currently do not play a role in providing training resources despite frequent visits. Overall, these findings suggest that pharmaceutical manufacturers and/or other stakeholders may be required to play larger roles in biologic initiation to ensure more predictable outcomes.
4.2.4. Support offered by HCPs and manufacturers is perceived as biased
HCPs expressed unconscious bias toward self-injection throughout the study, routinely minimizing the difficulty of the injection process and the amount of training/practice patients require.
“I’ve learned my patients turn out to be very intelligent and smart in figuring out things. What doesn’t work is talking down to patients, telling them ‘I will teach you how to use this,’ since these are easy, simple devices to use.” [P8 – Gastroenterology]
Surprisingly, this bias was not reflected in our analysis of participants’ PETS assessments, which revealed that HCPs find the process of locating and learning about medical information more difficult compared to patients. The rationale for this result is unclear; however, we hypothesize that HCPs perceive self-injections to be straightforward, but not the act of obtaining credible material and understanding injection-related elements outside of what is offered by the brand (i.e. healthy foods to eat, changes in treatment, and reasons they’re prescribed certain therapies). Presenting the parallel assessment subscales to a larger sample to power significance and probing qualitatively on perspective ratings would be a useful future analysis.
Patient participants discussed the shortcomings of materials offered by biologic brands, which likely deter a large portion of the population away from official resources and to the internet for medical information.
“The drug company’s website does list a lot of information on the medication that is biased in my personal opinion, it does not give actual account of patients. It gives a summary of the lighter side of medication … not blunt information you can find on the internet through social media sites and support groups.” [BxN21 – Migraine]
YouTube currently has over a billion users visiting each month and has been used effectively as an educational tool[Citation58]. However, as it is largely unregulated, posted videos may contain misleading or inaccurate information. A study assessing video use for methotrexate injection training found that less than 20% of the videos on YouTube contained accurate information that would be useful for patients. Despite being accurate, these videos, uploaded primarily by universities or professional organizations, were not preferentially viewed by patients over videos that were misleading. Moreover, unregulated videos uploaded by individual patients accounted for over 73% of the total views, and while not considered directly misleading, such personal videos could still pose a risk for other patients to be exposed to inaccurate information and build improper techniques[Citation59]. These results suggest that when given the option, patients tend to view ‘authentic’ videos preferentially, regardless of medical correctness. Pharmaceutical companies can leverage this dynamic but must also create an avenue for patients to select useful videos from reliable sources.
4.2.5. The emotional burden of self-injection is not accounted for
Our results show that the training and support patients receive early in biologic initiation can have significant effects on their perceived burden of treatment and confidence with self-injections. Regardless of training experience, patients reported negative physical and mental experiences during initiation.
“One of the things I did not share [with my HCP] was when I first was informed that I was going to do injections, I cried, I felt my life was over, so I just cried and cried and cried.” [BxE4 – Type 2 Diabetes]
Prior studies suggests that support and encouragement during the early stages of treatment can enable patients to overcome psychological barriers more quickly; however, the ability for facilities to provide this support is currently insufficient and highly variable [Citation12,Citation15].
“Anxiety makes [self-injection] a big deal and what we’re searching for may not be a big, long lecture, what we’re searching for is comfort knowing that we can do this.” [BxE14 – Type 2 Diabetes]
Involving caregivers in patient training may be a promising means to help facilitate patient support. In fact, in a prior patient/nurse focus group centered on self-injection, participants recommended involving family members whenever possible[Citation15]. Still, there may be limitations with this approach as well, as estimates indicate that nearly half of caregivers never receive medication-related training from any source [Citation60]. Another interesting technique that has the potential to reduce emotional overwhelm is the development of self-injection rituals. This concept was first observed in an ethnographic study by Schiff and colleagues, where patients developed rituals to help them mitigate their fears and anxieties associated with self-injection, ultimately increasing their confidence[Citation14]. As the authors suggested, empowering patients to develop their own personalized self-injection rituals could offer substantial benefit, and this may be of interest to pharmaceutical manufacturers when developing patient support materials. Overall, the use of medication-related rituals is an area that requires further exploration.
4.3. Biologic-naïve focus groups
Responses in our focus group session indicated that many of the training gaps discussed in the remote portion of our study may be exacerbated in injection-naïve patients. In some cases, these patients had far more demanding expectations of biologic initiation than what we and other authors have observed. Injection-naïve patients expressed a strong preference for lengthy training sessions where HCPs utilize visual demonstrations, repeated practice, and hands-on training with demo-devices, all of which are at-odds with what experienced patients reported in our study.
“Probably a couple of hours, I would say I wouldn’t want anything shorter. I expect to learn it both by watching somebody and having a manual … definitely practice on a dummy as many times as I needed. [Practicing] gives you more confidence, I mean just watching somebody do it once, you’ll have questions after that.” [INJ-N2 – Lupus]
This mismatch in expectations may be problematic, as our results suggest patients will leave biologic initiations feeling frustrated, disappointed, and potentially anxious about their ability to successfully self-inject on their own. Further, with biologics now recommended as first-line therapies in some disease areas[Citation61], the proportion of treatment-naïve patients initiated on injection therapy may be primed to increase in the future.
4.4. Recommendations
Based on our results, we offer several recommendations to improve patient initiation when starting biologic therapy to decrease inconsistencies in technical training and support: 1) Distribute injection training over a series of short, frequent sessions, rather than a single-instance event. 2) Provide patients with the resources to perform JIT training before their injections in the early stages of therapy, especially when dosing is infrequent. 3) Develop avenues to employ teach-back methods through video or other means to access more patients and eliminate the reliance on in-person demonstration. 4) Develop a structured, consistent resource for biologic initiation that establishes a standard for HCP communication strategies and instruction techniques regardless of time in practice or therapy experience. 5) Emphasize the importance of establishing routines, managing emotions, and adapting lifestyles to self-injection therapy, rather than solely injection mechanics and safety. 6) Consider patient feedback on resource shortcomings, and produce ‘authentic’ material aimed at showcasing actual patient experiences, the reality of injections, and potential solutions to mitigate fear and anxiety. 7) Explore rituals, as they may be of interest to pharmaceutical manufacturers when developing patient support materials ().
Table 5. Evidence-based recommendations to improve self-injection initiation
4.5. Limitations
Participants were not dyads, and we were therefore unable to conduct direct analysis between HCP and patient pairs. While recruiting dyads may have yielded more insightful results, this approach would have likely severely restricted our sample size. Still, we believe our approach to enroll patients and HCPs in common disease areas helped to mitigate this shortcoming. Conducting a similar study on HCP-patient dyads would be useful to confirm or deny the generalized gaps in biologic initiation described in our research. Second, our data set represented HCPs who frequently train patients on self-injection therapies and did not encompass the perspectives of HCPs who do not offer formal injection training to their patients. Third, although we used purposeful sampling, the majority of our patient participants were women (remote study: 87%, focus groups: 80%). While some of our target disease states are far more prevalent in women compared to men (e.g. rheumatoid arthritis, multiple sclerosis, systemic lupus erythematosus) this difference alone does not explain the bias toward women in our sample. With that said, male patients did not express notably different opinions from female patients. Fourth, due to practical limitations on the ability to recruit individuals with <6 months of experience injecting their current therapies, we could not enroll patients who had just recently been initiated or observe their initiation experiences directly. All accounts of practices were therefore reported retrospectively, which poses risk of recall bias. Fifth, patients under the age of 18 (and their potential caregivers) were excluded from our sample. Including this population would have increased recruiting complexity and impacted our study design, as not all represented medications are approved for pediatric use. Exploring how our findings translate to pediatric patients would be an interesting future analysis, especially in light of the relative dearth of high-quality evidence in this population and increasing interest in pediatric drug development. Finally, the qualitative nature of this study and small sample did not allow us to adequately test for differences in types of perspectives and experiences according to factors such as medical specialty, race/ethnicity, geography, education level and socioeconomic status. We encourage future research conducted on a larger sample of patients to confirm our findings with appropriate statistical power.
5. Conclusion
In conclusion, the current paradigm for biologic initiation does not meet the needs and expectations of patients who are currently prescribed self-injection therapies or may be in the future. Our study reveals significant gaps in technical training and patient support during biologic initiation and several elements that, if optimized, could facilitate more consistent and successful initiations. Development of more formal and structured training sessions, improved HCP knowledge and awareness of injection devices, use of demo-devices for injection practice, and focus on both the emotional and mechanical aspects of training have the potential to increase patient confidence, reduce training burden on HCPs, and improve the probability of patient success on biologic therapy.
Declaration of interest
A Rinaldi, D Katsaros, J Hawthorne, M D’Auria, K Brigham, E Bajars, C Franzese, M Coyne are employees of Matchstick. Matchstick received consulting fees and research support from Noble. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have received an honorarium from Expert Opinion on Drug Delivery for their review work, but have no other relevant financial relationships to disclose.
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, take responsibility for integrity of the work as a whole, and have given final approval to the version to be published. Secondary research of literature: D Katsaros, J Hawthorne, C Franzese, M Coyne; study design, execution, and data analysis: A Rinaldi, M D’Auria, K Brigham, E Bajars, M Coyne; substantial contributions to manuscript preparation: A Rinaldi, C Franzese, M Coyne; critical revision of manuscript for important intellectual content: A Rinaldi, C Franzese, M Coyne; review of manuscript for clinical accuracy: C Franzese; final approval of publication: A Rinaldi, C Franzese, M Coyne.
EODD-2021-FT-0064.R1_Supplementary_Information.docx
Download MS Word (271.5 KB)Acknowledgments
The authors would like to acknowledge Ale Linares for her graphic design contribution to this manuscript and Samantha Chang and Jessica Litmanovich for their contribution to collecting, transcribing, and coding video submissions.
Supplementary material
Supplemental data for this article can be accessed here
Additional information
Funding
References
- Tran V-T, Montori VM, Ravaud P. Is my patient overwhelmed? Mayo Clin Proc. 2020;95(3):504–512.
- Schwartzman S, Morgan GJ. Does route of administration affect the outcome of TNF antagonist therapy? Arthritis Res Ther. 2004;6(S2). DOI:10.1186/ar996
- Navarro-Millán I, Herrinton LJ, Chen L, et al. Comparative effectiveness of etanercept and adalimumab in patient reported outcomes and injection-related tolerability. Bamias G, ed. Plos One. 2016;11(3):e0149781.
- Hirsch LJ, Strauss KW. The injection technique factor: what you don’t know or teach can make a difference. Clin Diabetes. 2019;37(3):227–233.
- Oleen-Burkey M, Pardo G. Examining the influence of behavioral factors on compliance and persistence with glatiramer acetate injection for relapsing-remitting multiple sclerosis. J Neurol Neurophysiol. 2014;05:03.
- Applying human factors and usability engineering to medical devices: guidance for industry and food and drug administration staff. US Food and Drug Administration (FDA); 2016.
- Weinhold T, Del Zotto M, Rochat J, et al. Improving the safety of disposable auto-injection devices: a systematic review of use errors. AAPS Open. 2018;4(1). DOI:10.1186/s41120-018-0027-z
- Potera C. Misuse of Autoinjectors and Inhalers. AJN Am J Nurs. 2015;115(3):17.
- CIMZIA (certolizumab pegol) [package insert]. Smyrna, GA: UCB, Inc. 2019. cited 2021 Feb 3. Available from: https://www.cimzia.com/themes/custom/cimzia/docs/CIMZIA_full_prescribing_information.pdf
- FASENRA (benralizumab) [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals. 2019.
- Lang VA, Nalan D Combination product patient training: how are patients trained and who conducts the training? In: 2018 Design of Medical Devices Conference. Minneapolis, Minnesota, USA. American Society of Mechanical Engineers; 2018. doi:10.1115/DMD2018-6956
- Brod M, Rousculp M, Cameron A. Understanding compliance issues for daily self-injectable treatment in ambulatory care settings. Patient Prefer Adherence. 2008;2:129–136.
- Schneider A, Kolrep H, Jordi C, et al. How to prevent medication errors: a multidimensional scaling study to investigate the distinguishability between self-injection platform device variants. Expert Opin Drug Deliv. 2019;16(8):883–894.
- Schiff M, Saunderson S, Mountian I, et al. Chronic disease and self-injection: ethnographic investigations into the patient experience during treatment. Rheumatol Ther. 2017;4(2):445–463.
- Zimmer PA, Braun LT, Fraser R, et al. Promoting success in self-injection: listening to patients. Medsurg Nurs Off J Acad Med-Surg Nurses. 2015;24(4):279–282.
- Tallman K. Communication practices of physicians with high patient-satisfaction ratings. Perm J. 2007;11(1). DOI:10.7812/TPP/06-106
- Mohr DC, Cox D, Epstein L, et al. Teaching patients to self-inject: pilot study of a treatment for injection anxiety and phobia in multiple sclerosis patients prescribed injectable medications. J Behav Ther Exp Psychiatry. 2002;33(1):39–47.
- Cox D, Stone J. Managing self-injection difficulties e page in patients with relapsing-remitting CE multiple sclerosis. J Neurosci Nurs. 2006;38(3):5.
- Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits: time allocation in primary care. Health Serv Res. 2007;42(5):1871–1894.
- Young RA, Burge SK, Kumar KA, et al. A time-motion study of primary care physicians’ work in the electronic health record era. Fam Med. 2018;50(2):91–99.
- Leung JM, Bhutani M, Leigh R, et al. Empowering family physicians to impart proper inhaler teaching to patients with chronic obstructive pulmonary disease and asthma. Can Respir J. 2015;22(5):266–270.
- Kottak N, Tesser J, Leibowitz E, et al. Ethnographic observational study of the biologic initiation conversation between rheumatologists and biologic-naive rheumatoid arthritis patients. Arthritis Care Res. 2018;70(7):997–1004.
- Sicherer SH, Forman JA, Noone SA. Use assessment of self-administered epinephrine among food-allergic children and pediatricians. Pediatrics. 2000;105(2):359–362.
- Rogers E, Yost K, Rosedahl J, et al. Validating the Patient Experience with Treatment and Self-Management (PETS), a patient-reported measure of treatment burden, in people with diabetes. Patient Relat Outcome Meas. 2017;8:143–156.
- Keininger D, Coteur G. Assessment of self-injection experience in patients with rheumatoid arthritis: psychometric validation of the Self-Injection Assessment Questionnaire (SIAQ). Health Qual Life Outcomes. 2011;9(1):2.
- Tran G, Dube B, Kingsbury SR, et al. Investigating the patient acceptable symptom state cut-offs: longitudinal data from a community cohort using the shoulder pain and disability index. Rheumatol Int. 2020;40(4):599–605.
- Aldiabat KM, Navenec C-L-L. Data saturation: the mysterious step in grounded theory method. Qual Rep. 2018;23(1):19.
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–1760.
- Sandelowski M, Leeman J. Writing usable qualitative health research findings. Qual Health Res. 2012;22(10):1404–1413.
- Krueger RA. Focus groups: a practical guide for applied research. 5th ed. SAGE Publications, Thousand Oaks, California; 2014.
- Baggott C, Chan A, Hurford S, et al. Patient preferences for asthma management: a qualitative study. BMJ Open Access. 2020;10:e037491. Published online.
- Ridgeway JL, Egginton JS, Tiedje K, et al. Factors that lessen the burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Prefer Adherence. 2014 Mar 19;8:339-51.
- Zabala A qmethod: a package to explore human perspectives using Q methodology. R J. 2014;6:11.
- Lautenschlager GJ. A comparison of alternatives to conducting monte carlo analyses for determining parallel analysis criteria. Multivar Behav Res. 1989;24(3):365–395.
- Humphreys LG Jr. An investigation of the parallel analysis criterion for determining the number of common factors. Multivar Behav Res. 1975;10(2):193–205.
- Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas. 1960;20(1):141–151.
- Clark SE. Training decay selection for usability validation. Proc Int Symp Hum Factors Ergon Health Care. 2016;5(1):76–83.
- Nakatani Y, Matsumura M, Monden T, et al. Improvement of glycemic control by re-education in insulin injection technique in patients with diabetes mellitus. Adv Ther. 2013;30(10):897–906.
- Arthur W Jr, Bennett W Jr, Stanush PL, et al. Factors that influence skill decay and retention: a quantitative review and analysis. Hum Perform. 1998;11(1):57–101.
- Garafalo J, Li H, Lau M. The impact of a training device on perception and performance by novice users of an autoinjector. Proc Int Symp Hum Factors Ergon Health Care. 2019;8(1):192–196.
- Niles D, Sutton RM, Donoghue A, et al. “Rolling Refreshers”: a novel approach to maintain CPR psychomotor skill competence. Resuscitation. 2009;80(8):909–912.
- Cheng A, Brown LL, Duff JP, et al. Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES study): a randomized clinical trial. JAMA Pediatr. 2015;169(2):137–144.
- Kessler D, Pusic M, Chang TP, et al. Impact of Just-in-Time and Just-in-Place Simulation on Intern Success With Infant Lumbar Puncture. Pediatrics. 2015;135(5):e1237–e1246.
- Grgurich E, Arnemann C, Amon K, et al. Just-in-Time video laryngoscopy versus direct laryngoscopy for neonatal intubation. Neonatal Nurs. 2016;(4):367-371. Published online.
- Olivieri LJ, Su L, Hynes CF, et al. “Just-In-Time” simulation training using 3-D printed cardiac models after congenital cardiac surgery. World J Pediatr Congenit Heart Surg. 2016;7(2):164–168.
- Branzetti JB, Adedipe AA, Gittinger MJ, et al. Randomised controlled trial to assess the effect of a Just-in-Time training on procedural performance: a proof-of-concept study to address procedural skill decay. BMJ Qual Saf. 2017;26(11):881–891.
- Gelhorn HL, Balantac Z, Ambrose CS, et al. Patient and physician preferences for attributes of biologic medications for severe asthma. Patient Prefer Adherence. 2019;13:1253–1268.
- Zhang M, Brenneman S, Carter C, et al. Patient-reported treatment satisfaction and choice of dosing frequency with biologic treatment for moderate to severe plaque psoriasis. Patient Prefer Adherence. 2015 June;777. Published online. DOI:10.2147/PPA.S85773
- Hong Y-R, Jo A, Cardel M, et al. Patient-provider communication with teach-back, patient-centered diabetes care, and diabetes care education. Patient Educ Couns. 2020;103(12):2443–2450.
- Bryan RL, Kreuter MW, Brownson RC. Integrating adult learning principles into training for public health practice. Health Promot Pract. 2009;10(4):557–563.
- Yen PH, Leasure AR. Use and effectiveness of the teach-back method in patient education and health outcomes. Fed Pract. 2019 Jun; 36(6): 284–289.
- Kessels RPC Patients’ memory for medical information. 2003;96:4.
- Murre JMJ, Dros J. Replication and analysis of Ebbinghaus’ forgetting curve. Chialvo DR, ed. Plos One. 2015;10(7):e0120644.
- Hu SG, Liu Y, Chen TP, et al. Emulating the Ebbinghaus forgetting curve of the human brain with a NiO-based memristor. Appl Phys Lett. 2013;103(13):133701.
- Cegala DJ, Lenzmeier Broz S. Physician communication skills training: a review of theoretical backgrounds, objectives and skills: physician communication skills training: theoretical backgrounds, objectives and skills. Med Educ. 2002;36(11):1004–1016.
- Bonner L. Beyond vaccines: pharmacists improve patient access to injectable medications. Pharm Today. 2018;24(2):34–37.
- Lin C, Strauss R, Hong J, et al. Impact of a pharmacist-administered long-acting injectable antipsychotic service in a supermarket-based community pharmacy on medication adherence. J Am Coll Clin Pharm. 2019;2(4):343–348.
- Katz SJ, Leung S. Teaching methotrexate self-injection with a web-based video maintains patient care while reducing healthcare resources: a pilot study. Rheumatol Int. 2015;35(1):93–96.
- Rittberg R, Dissanayake T, Katz SJ. A qualitative analysis of methotrexate self-injection education videos on YouTube. Clin Rheumatol. 2016;35(5):1329–1333.
- Reinhard S, Levine C, Samis S Home alone: family caregivers providing complex chronic care. AARP Public Policy Institute and The United Hospital Fund; 2012:50.
- Singh JA, Guyatt G, Ogdie A, et al. Special article: 2018 American College of Rheumatology/National Psoriasis Foundation guideline for the treatment of psoriatic arthritis. Arthritis Rheumatol Hoboken NJ. 2019;71(1):5–32.