ABSTRACT
Automated telecommunication interventions, including short message service and interactive voice response, are increasingly being used to promote adherence to medications prescribed for cardio-metabolic conditions. This systematic review aimed to comprehensively assess the effectiveness of such interventions to support medication adherence, and to identify the behaviour change techniques (BCTs) and other intervention characteristics that are positively associated with greater intervention effectiveness. Meta-analysis of 17 randomised controlled trials showed a small but statistically significant effect on medication adherence, OR = 1.89, 95% CI [1.51, 2.36], I2 = 89%, N = 25,101. Multivariable meta-regression analysis including eight BCTs explained 88% of the observed variance in effect size (ES). The BCTs ‘tailored’ and ‘information about health consequences’ were positively and significantly associated with ES. Future studies could explore whether the inclusion of these and/or additional techniques (e.g., ‘implementation intentions’) would increase the effect of automated telecommunication interventions, using rigorous designs and objective outcome measures.
Introduction
Cardio-metabolic conditions (i.e., having a diagnosis of two, or more, of diabetes mellitus, stroke, myocardial infraction) are a major public health challenge, and the mortality risk is increasing significantly in people over 60 years old (Di Angelantonio et al., Citation2015; Fuller, Stevens, & Wang, Citation2001; Nathan, Meigs, & Singer, Citation1997). Medication adherence is an important component in both prevention (e.g., statins to lower cholesterol in people without prior cardiovascular conditions) and treatment (e.g., anti-hypertensives to reduce the risk of stroke among stroke survivors; glucose lowering medication for type 2 diabetes) of cardio-metabolic health conditions, and is recommended as an essential part of self-management services (National Institute for Health and Care Excellence [NICE], Citation2014). Given the growing prevalence of cardio-metabolic conditions, and the ageing population (NCD Risk Factor Collaboration, Citation2016), it is likely that there will be an increase in demand for healthcare resources to support medication adherence (Tinetti, Fried, & Boyd, Citation2012). It is also likely that such patients will be prescribed more complex medication regimens, in comparison to those with a single condition, and thus, they will require more regular consultations or other ongoing support.
Although medication is an important component of recommended treatment and prevention strategies, a substantial proportion of patients do not adhere to their prescribed medication regimens (Chowdhury et al., Citation2013; WHO, Citation2003). Non-adherence is defined as discontinuing medication or taking less than the prescribed daily dose. Medication non-adherence reduces the effectiveness of treatment, wastes healthcare resources, and leads to additional consultations, referrals, investigations, prescriptions, and hospital admissions. In England alone, it has been estimated that an increase in adherence to blood pressure medication would result in saving just over £100 million per year (York Health Economics Consortium & School of Pharmacy, University of London, Citation2010). However, current methods to increase adherence are complex and ineffective (Nieuwlaat et al., Citation2014). Thus, there is a need for the development and evaluation of novel interventions to improve adherence (Department of Health, Citation2012; NICE, Citation2009).
Automated telecommunication systems, including voice messaging (IVR: interactive voice response) and text messaging (SMS: short message service), are one way to deliver health care on an ongoing basis and as an adjunct to primary and secondary care consultations. Several systematic reviews suggest that such platforms are inexpensive, acceptable, and promising ways to deliver interventions for health behaviour change (De Jongh, Gurol-Urganci, Vodopivec-Jamsek, Car, & Atun, Citation2012; Orr & King, Citation2015), including adherence to different types of medication (Mistry et al., Citation2015; Park, Howie-Esquivel, & Dracup, Citation2014; Thakkar et al., Citation2016; Vervloet, Linn et al., Citation2012). However, none of these reviews provided evidence on the effectiveness of IVR and SMS interventions to increase adherence in patients with, or at risk of, cardio-metabolic conditions; and none tried to identify the active intervention components associated with their effectiveness. For example, previous reviews combined interventions that used different delivery modes and content, making the identification of the effective and replicable components of the IVR and SMS delivered interventions impossible. To address this gap, the aim of this review was to conduct a comprehensive effect-size (ES) analysis of IVR and SMS interventions to promote adherence to cardio-metabolic medication, to identify components of these interventions that are associated with their effectiveness, and to discuss possible mechanisms of action.
To identify the effective intervention components, the present review had three secondary aims. First, it examined whether the delivery format of the intervention messages (i.e., text or voice) was associated with intervention effectiveness. To facilitate the translation of such interventions into clinical practice, the review also examined whether the presence of an additional delivery mode (e.g., face-to-face, booklet) was associated with intervention effectiveness. Second, other intervention characteristics such as the intervention duration and the frequency and direction of intervention messages, may be associated with intervention effectiveness (Thakkar et al., Citation2016). The identification of such characteristics could have implications for the design of future interventions.
Third, the active and modifiable intervention content has been systematically categorised by the taxonomy of behaviour change techniques (BCTs), and associated with intervention effectiveness (Michie et al., Citation2013). Evidence suggests that several aspects of BCTs are associated with intervention effectiveness. These are (a) the number of BCTs (Michie, Jochelson, Markham, & Bridle, Citation2009); and (b) the presence or absence of a single BCT, or of a combination of BCTs (Michie et al., Citation2013). Currently, the BCTs that are most effective in promoting medication adherence are largely unknown.
Methods
Systematic literature review searches were conducted in multiple databases. A random effects model was used to meta-analyse the effectiveness of the interventions, and meta-regressions were conducted to identify the BCTs and the other intervention characteristics that were associated with intervention effectiveness. This review was not registered.
Selection criteria
Population
Adults aged 18 years and over, who were prescribed oral medication (e.g., anti-hypertensive, anti-glycaemic, statins) to treat or prevent cardio-metabolic conditions were included. Adults whose main prescription was insulin to manage type 1 diabetes mellitus were excluded.
Intervention
Studies where medication adherence was the main focus of the intervention, and where IVR and/or SMS were the main delivery mode of the intervention, were included. Studies where IVR and/or SMS were adopted to facilitate communication of clinical outcomes between the patient and the healthcare provider (e.g., to support blood glucose self-monitoring), but delivered no messages to promote adherence to medication, were excluded.
Design and comparator
Randomised controlled trials (RCTs) with randomisation at the individual patient or cluster (e.g., general practice) level were included. Studies in which the intervention was compared with usual care or a minimal intervention were included. In the latter case, the minimal intervention could be delivered by IVR and/or SMS (e.g., appointment reminders, screen for symptoms), but studies were included only if neither of these modes were used to deliver medication adherence messages in the comparator condition.
Outcome
Medication adherence measured by self-report questionnaires, electronic monitoring devices, pill counts, or electronic pharmacy records.
Search methods for identification of studies
Studies were identified through the following databases: Medline, Embase, CINAHL, PsycINFO (from January 1992 to April 2016), and Cochrane Central Register of Controlled Trials (CENTRAL). A sensitive search strategy was developed using terms for (a) medication adherence, (b) adults with a diagnosis of, or at risk of, a cardio-metabolic condition (e.g., myocardial infarction, type 2 diabetes mellitus, stroke), (c) intervention delivery mode (IVR, SMS), and (d) study design (see Appendix 1). Only studies published in English were included. Results were imported into the reference management software Endnote, duplicates were removed, and the remaining papers were screened by title and abstract.
Abstracts were screened and assessed based on the following criteria: whether they reported information relevant to the targeted (a) behaviour, (b) type of medication, (c) intervention delivery mode, and (d) study design. Abstracts that did not meet all the criteria were excluded from full text screening. Full text articles were examined and included if they met all the following criteria: the article clearly (a) stated that the intervention targeted adults taking medications with the aim to prevent (e.g., type 2 diabetes mellitus), or treat (e.g., acute coronary syndrome), a cardio-metabolic health condition; (b) described the use of IVR and/or SMS, or multiple modes, to deliver the intervention (e.g., voice messages with a booklet or with face-to-face appointments), but the IVR and/or SMS was considered to be the main delivery mode of the intervention; (c) reported that patients (or clusters of patients) were randomised; and (d) included at least one medication adherence outcome.
References from review papers (Cutrona et al., Citation2010; Fjeldsoe, Marshall, & Miller, Citation2009; Kripalani, Yao, & Haynes, Citation2007; Mistry et al., Citation2015; Park, Howie-Esquivel, & Dracup, Citation2014; Thakkar et al., Citation2016; Vervloet, Linn et al., Citation2012) and original studies were screened for relevant papers; forward and backward citation searches for relevant papers were conducted; and primary authors were contacted by email for missing information and/or intervention protocols. S. S. drafted the search strategy. A. K. developed the search strategy, searched the databases, and screened titles, abstracts, and full text against the inclusion and exclusion criteria. During this process, S. S. made comments and queries to A. K.’s notes. Disagreements were resolved through discussion.
Data extraction
A data extraction form was developed and used to extract data from eligible studies. The form contained information on the following: authors, long-term health conditions, recruitment setting (where participants were identified and how they were approached), characteristics of eligible and analysed participants, country, delivery mode, intervention characteristics (e.g., duration of the study; message frequency, duration, and language), and outcome data.
For the medication adherence outcomes, the following information was extracted: (a) the behavioural outcome assessed: taking and/or collecting medication; (b) the definition of the outcome measured: medications not taken, medications taken, days medication was available to participants; (c) the method used to collect each outcome: standardised self-report scales, non-standardised self-report scales with single or multiple items, pill counts, real time medication monitoring devices, electronic pharmacy records; (d) the type of medication measured (e.g., antiplatelets, statins, pravastatin, ACE inhibitors, metformin); (e) the time measurements were collected: at baseline and at follow-up; and (f) the statistical method used: unadjusted or adjusted means (M) and standard deviation (SD), percentage or number of participants who provided outcome data. Medication adherence was defined as taking at least 80% of the prescribed tablets and/or having medications dispensed for at least 95% days of a prescribed period (Ball, Citation1974; Sackett & Haynes, Citation1976).
The methodological quality of the included studies was assessed using the Cochrane risk of bias tool (Higgins, Thompson, Deeks, & Altman, Citation2003). Each study was given a score of high, low, or unclear risk of bias on the seven assessment criteria. However, because it is impossible to blind participants to these interventions, studies that were at high risk of bias on any criterion other than blinding of participants and personnel were considered to have high risk of bias.
Intervention coding
The BCTs were coded using the BCT taxonomy (v1) (Michie et al., Citation2013). Each technique was coded as ‘yes’ or ‘no’, based on whether or not it was described in each intervention. Authors of included studies were contacted to request missing information about the techniques reported in the papers.
The BCTs delivered through IVR and/or SMS interventions only were coded. The BCTs delivered to the comparator group, usually referred as ‘usual care’, could not be coded due to lack of reported information. If studies reported that the intervention group received information relevant to medication adherence using another delivery mode (e.g., letter) that the comparator group did not receive, then this was coded as ‘additional delivery mode’. If the intervention messages used the participant’s first name, they were coded as ‘personalised’; and if interventions delivered different messages to different participants, depending on information gained about them, they were coded as ‘tailored’.
One more technique was coded, because it was considered to be potentially important for changing behaviour: ‘reporting whether or not the behaviour was performed’. This technique refers to asking a person to report whether he/she has performed a behaviour (e.g., in a voice or text message query), without the person monitoring or recording the behaviour. It therefore differs from the BCT ‘self-monitoring of behaviour’, which refers to monitoring and recording a behaviour (e.g., in a diary or on a pedometer steps sheet). Our decision to include this additional technique was based partly on evidence suggesting that self-reports of behaviour may have a reactive effect on behavioural outcomes (French & Sutton, Citation2010). More information about the rules used to code BCTs as well as the BCTs coded for each study can be found in Appendix 2. In addition, interventions were coded in terms of intervention duration (short term: less than 6 months; long term: 6 months or more), message frequency (more frequent: daily; less frequent: weekly or monthly), and direction of communication (one-way: when participants could not respond to intervention messages; two-way: when participants could respond to intervention messages).
The two reviewers independently conducted data extraction, intervention coding, and risk of bias assessment, for all the included papers. Any disagreements were resolved through discussion.
Data synthesis and statistical analysis
To ensure independence of outcome data in the meta-analysis, the following criteria were developed: (a) when more than one medication adherence outcome was reported, the one that the reviewers judged to be more valid was selected (e.g., electronic pharmacy records or electronic monitoring device, instead of self-reported questionnaire). However, when medication adherence behaviour was measured by more than one objective measurement (e.g., electronic monitoring device and electronic pharmacy records), the measurement assessing medication taking instead of collecting medication was selected; (b) when more than one type of medication was assessed, the one that was described as the primary target of the intervention was selected. However, when authors did not explicitly report the primary target of the intervention, the medication that was most comparable to those used in the other included studies was selected (e.g., Park, Howie-Esquivel, Chung, et al., Citation2014; statins instead of antiplatelets). Each study contributed one ES for medication adherence to the meta-analysis (see supplementary material 1).
To calculate the ES, we used the unadjusted values at the end of the intervention. For continuous data we selected means (M), standard deviations (SD), and sample sizes. When the standard error was reported instead of the SD, we calculated the SD manually. For dichotomous data, we used the number of adherent patients and total sample size in each of the intervention and comparator groups. The ES was reported as an odds ratio (OR). ESs for continuous data were converted to ORs and 95% confidence intervals (CI), so that the studies could be compared. To estimate the effect of the BCTs on the ES, only the (eight) BCTs that were coded in at least three studies were included in the regression analysis.
Three main analyses were conducted:
a meta-analysis of intervention effects on medication adherence;
a series of univariable meta-regression analyses, regressing intervention ES across studies on each of the eight BCTs (present vs. absent), number of BCTs used in the intervention, main delivery mode (SMS vs. IVR), additional delivery mode (present vs. absent), intervention duration (short vs. long), direction of communication (two-way vs. one-way), and message frequency (more frequent vs. less frequent); and
a multivariable meta-regression analysis, regressing intervention ES on the eight BCTs (present vs. absent).
Possible publication bias was assessed by the funnel plot and Egger’s test (Egger, Smith, & Minder, Citation1997). Primary data were entered in the Comprehensive Meta-Analysis software (Borenstein, Hedges, Higgins, & Rothstein, Citation2014), where a database to calculate ESs was created and all the statistical analyses were performed. Statistical significance was set at p < .05.
Results
Description of included studies
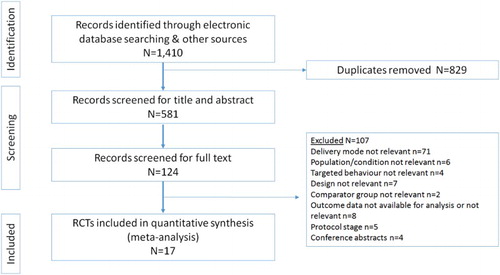
The search method identified 1410 records, of which 124 were assessed in full text. Seventeen studies met the inclusion criteria (see supplementary material 2, for a list of studies excluded at this stage). The PRISMA flow chart showing the selection process is provided in .
In total the 17 studies randomised 38,671 participants to the intervention (n = 23,352) or comparator groups (n = 15,319), of whom 25,037 (65%) completed the measurements at follow-up. Study participants’ mean age was 56.7 years, ranging from 47.5 to 76, and almost half of them were female. Participants were recruited from primary care (k = 7), secondary care (k = 7), and pharmacy (k = 3) settings. The targeted health conditions included coronary heart disease (k = 4), type 2 diabetes mellitus (k = 3), high blood pressure (k = 3), high cholesterol (k = 3), comorbidities of type 2 diabetes mellitus and cardiovascular conditions (k = 2), comorbidities of high blood pressure and high cholesterol (k = 1), and stroke (k = 1). All studies involved prescriptions of complex medication regimens. Regarding the delivery mode, nine studies used SMS and eight used IVR. Nine studies were conducted in the USA; two in Canada; and one in each of Malaysia, the Netherlands, Pakistan, South Africa, Spain, and the UK. The characteristics of the included studies are reported in .
Table 1. Characteristics of included studies.
Self-report questionnaires were the most common method of measuring medication adherence (k = 12), followed by electronic pharmacy records (k = 5), electronic monitoring devices (k = 2), and pill counts (k = 1). Two studies combined self-report questionnaires with electronic monitoring devices, and one study combined self-report questionnaires with electronic pharmacy records. Twelve out of the 17 studies measured outcomes at least 6 months after randomisation. Fifteen out of 17 studies reported the duration of the intervention, with the average length being approximately 5.6 months (M = 169 days; range 25–360 days).
The number of BCTs used ranged from one to eight (median = 3). The most frequent BCT was ‘prompts and cues’, coded in 12 studies; followed by ‘personalised’ and ‘social support (unspecified)’ each coded in 8 studies; ‘tailored’ and ‘information about health consequences’ each coded in 7 studies; ‘habit formation’ and ‘report whether or not the behaviour was performed’ each coded in 5 studies; ‘problem solving’ coded in 3 studies’; ‘social support (practical)’ coded in 2 studies, ‘social reward’, ‘information about social and environmental consequences’, ‘adding objects to the environment’, ‘self-talk’, ‘self-monitoring of behaviour’, ‘feedback on behaviour’, and ‘reduce prompts/cues’, each coded in 1 study. No BCTs were coded for any of the following the taxonomy clusters: shaping knowledge, comparison of behaviour, comparison of outcomes, regulation, identity, scheduled consequences, and covert learning.
All studies reported the frequency of the intervention messages, with frequency ranging from multiple messages per day to two messages per total intervention duration. Only a few studies reported the duration of the IVR messages (e.g., 40 seconds), whereas for the SMS studies it was assumed that each text was a maximum of 160 characters. In 6 out of 17 studies, there was an additional delivery mode (i.e., additional to SMS/IVR) that was used in the intervention condition but not in the comparator condition.
Nine studies compared the intervention to usual care, usually described as visits to a physician or pharmacist without reporting detailed information on the content of the care provided. Four studies described usual care as a minimal intervention (e.g., reminder postcards, medication dispenser, educational material). Four studies compared the intervention with a minimal intervention delivered by IVR or SMS, but the latter did not include BCTs to support medication adherence (see ).
Risk of bias arising from lack of blinding of participants or personnel was coded in all studies. Lack of blinding of adherence outcome measurement was also coded in the majority of studies, due to the use of self-report or lack of information on whether or not the assessor was blinded to allocation group (for objective measurements). Ten out of 17 studies showed low attrition bias. Overall, 14 of the 17 studies were assessed as having a high risk of bias (see ).
Table 2. Risk of bias.
Meta-analysis
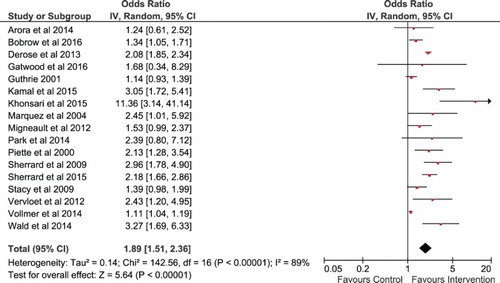
On average, the interventions had a small but statistically significant effect on medication adherence, OR = 1.89, 95% CI [1.51, 2.36], N = 25,101. Heterogeneity among studies was high and statistically significant, Q = 143, p < .001, I2 = 88.8% ().
The funnel plot (see Appendix 3) and statistically significant Egger’s test, p = .021, suggested possible publication bias, with relatively few of the less precise studies having ESs that fell below the average ES. On the other hand, the fail-safe N was reassuringly large (735).
Meta-regression analysis
Univariable meta-regressions of intervention ES on each of the eight BCTs coded in at least three studies, showed significant associations for only two BCTs: ‘information about health consequences’, T2 = 0.04, R2 = 0.67, p = .006, and ‘reporting whether or not the behaviour was performed’, T2 = 0.11, R2 = 0.21, p = .027. In both cases, the use of each BCT was associated with a larger intervention ES. The number of BCTs included in the intervention was not significantly associated with ES. None of the other intervention characteristics were associated with ES, although there was a marginally non-significant tendency for two-way communication, T2 = 0.05, R2 = 0.62, p = .056, and higher message frequency, T2 = 0.12, R2 = 0.11, p = .056, to be positively associated with larger intervention effects.
Multivariable meta-regression analysis showed that the presence or absence of the eight BCTs together explained 88% of the variance in intervention ES. Moreover, the goodness-of-fit test was not statistically significant, T2 = 0.01, I2 = 30.7%, Q = 11.6, df = 8, p = .172, suggesting that the ES does not vary across studies that use the same BCTs. The BCTs ‘tailored’ and ‘information about health consequences’ were positively and significantly associated with a larger intervention ES, when the remaining BCTs were controlled for. None of the other six BCTs were significantly associated with intervention ES. However, there was a marginally non-significant association for ‘problem solving’, with a negative coefficient showing that, controlling for other BCTs, interventions that used this BCT tended to have smaller ESs (see ).
Table 3. Multivariable meta-regression analysis regressing intervention ES on all eight behaviour change techniques.
Discussion
This systematic review and meta-analysis of 17 RCTs (N = 25,101) found that automated IVR or SMS interventions on average almost double the odds (OR = 1.89) of adherence to cardio-metabolic medications compared with usual care. Taking into consideration the large reach and potential low cost of the delivery modes (Orr & King, Citation2015; Smith et al., Citation2016), such interventions could have a significant impact on public health if applied on a large scale. The present study also identified BCTs that are positively associated with larger intervention ES: ‘tailored’, ‘information about health consequences’, and ‘reporting whether or not the behaviour was performed’; although only the first two of these were significant in the multivariable model. There was also a suggestion that two-way communication and more frequent messages (i.e., daily) may enhance effectiveness, but whether and how these intervention characteristics impact on effectiveness need to be further investigated. The number of BCTs, the main delivery mode, the additional delivery mode, and the intervention duration were not associated with the intervention effectiveness.
Previous reviews recommended the potential of such platforms to deliver advice on adherence to different types of prescribed medication (Mistry et al., Citation2015; Park, Howie-Esquivel, & Dracup, Citation2014). However, to our knowledge this is the first systematic review with meta-analysis that has comprehensively investigated the effectiveness of IVR or SMS interventions to promote adherence to cardio-metabolic medications. This review not only showed that such interventions are effective in promoting adherence among participants who have been prescribed complex medication regimens, but also identified BCTs that are associated with their effectiveness. Given the lack of evidence on effective methods to promote medication adherence, reported by previous reviews (Mistry et al., Citation2015; Nieuwlaat et al., Citation2014), these findings are a valuable contribution to our knowledge and could inform recommendations for future interventions.
The results of this review suggest that interventions should be tailored, provide information about the health consequences of adhering (or not) to prescribed medications, and ask participants to report whether or not they have taken their tablets as prescribed. This review did not investigate the mechanisms by which these BCTs may increase adherence. However, we briefly outline some possible mechanisms based on existing findings and theories.
Tailoring, in which different messages are sent to different participants depending on information obtained from or about them, was used in nine of the included studies. Automated IVR and SMS systems are ideally suited to delivering tailored messages, including dynamic tailoring in which messages are automatically modified using new or updated information obtained from the user during the course of the intervention. However, the nature of the tailoring, including the variables that were used to tailor the information, varied widely in the included studies. For example, in Khonsari et al. (Citation2015) text message reminders were simply tailored on medication quantity (dose), medication name and time, as well as using the patient’s name (which we coded as ‘personalised’). By contrast, the messages used by Gatwood et al. (Citation2016) were tailored according to participants’ responses to a series of theory-based questions on severity, susceptibility, benefits, motivation, and other constructs (see Gatwood et al., Citation2014). There is substantial evidence that tailored interventions are more effective than generic interventions (e.g., Hartmann-Boyce, Lancaster, & Stead, Citation2014). Tailored interventions may be seen by recipients as more personally relevant, so they will be more likely to attend to, read, understand, and act on them. In addition, tailored interventions are designed to change determinants of the target behaviour that are relevant to particular individuals (or to small subgroups of individuals); they therefore more precisely target the determinants of the individual’s behaviour. There is scope for developing more highly tailored interventions for medication adherence using IVR, SMS, and other digital platforms, although the potential benefit of increased effectiveness has to be balanced against the increased burden of measurement and greater complexity.
Providing information about health consequences, used in six of the included studied, may address intentional non-adherence (Barber, Citation2002) or, more specifically, what Horne calls ‘necessity beliefs’ (Horne et al., Citation2013). Some patients may have doubts about the effectiveness of their medication, and providing information about the health consequences (either the benefits of adherence or the disbenefits of non-adherence) may help to assuage these doubts.
Such techniques may be more or less effective depending on the presence of other factors, which Peters, de Bruin, and Crutzen (Citation2015) refer to as ‘parameters of effectiveness’. For example, to the extent that presenting the disbenefits of non-adherence arouses concern among non-adherent patients, such information may be more effective if the recipients are already high on self-efficacy and perceived response efficacy or if the intervention messages include efficacy statements (Tannenbaum et al., Citation2015).
Used as a technique for changing behaviour, asking participants to report whether or not they have taken their tablets may work partly through fear of social disapproval or desire for social approval, even when they are reporting their behaviour to an automated system rather than directly to another person. Of course, participants may overstate the extent of their adherence, that is, their reports may not be valid. Nevertheless, knowing that they will be asked to report their adherence may increase their adherence. This effect and potential mechanisms are worthy of investigation in future studies.
The most frequently coded BCT was ‘prompts/cues’. Reminding patients to take their medication would be expected to be an effective technique because it directly addresses non-intentional non-adherence. However, use of this BCT was not associated with larger intervention ESs. There are many ways of operationalising reminders, and in some of the included studies this may not have been done in an effective way. For example, intervention participants in Guthrie (Citation2001) received only two telephone reminders during the 5-month intervention period. Marquez Contreras et al. (Citation2004) sent two SMS reminder messages per week between 11 am and 2 pm on randomly chosen weekdays. In neither study were the messages individually tailored. By contrast, Park, Howie-Esquivel, Chung, et al. (Citation2014) sent tailored SMS reminders twice a day at times selected by participants related to their medication schedule (e.g., an antiplatelet reminder in the morning and a statin reminder in the evening) and asked them to confirm receipt, e.g., ‘John, take Plavix 75 mg at 9.00 AM. Respond with 1’.
Although a range of BCTs were used in the included interventions, some techniques that have been shown in other studies to be effective in promoting adherence, such as ‘implementation intentions’ (Farmer et al., Citation2012), or ‘action planning’ in the BCT taxonomy, were not used in any of the interventions studied here. One reason could be that the delivery modes of IVR and SMS may not be suited to conveying these techniques. Nevertheless, intervention developers could consider including such techniques in future IVR and SMS interventions to promote adherence. Like reminders, implementation intention interventions may address non-intentional non-adherence but may have a more sustained effect by effectively helping to create a new habit (Gollwitzer & Bargh, Citation2005).
The findings of this review may have been affected by publication bias, with small studies having small effects perhaps being less likely to be published. Moreover, only studies published in the English language were included, which may limit the generalisability of the results. However, among the included studies eight interventions delivered messages in languages other than English, suggesting that the results may apply to non-English-speaking populations. The targeted population of this review had a mean age of 57 years and were prescribed complex medication regimens, which highlights the potential effectiveness of such interventions to support adherence in people with cardio-metabolic multi-morbidities (Di Angelantonio et al., Citation2015; WHO, Citation2016).
This review combined collecting and taking medications. Although this approach was used in previous reviews (e.g., Mistry et al., Citation2015), collecting a prescription from a pharmacy and taking tablets as prescribed are distinct behaviour that may differ in important ways, including frequency and the role of habit, and may require somewhat different interventions or BCTs. This distinction warrants investigation in future studies.
The majority of the studies included in this review used self-report measures of adherence, which are likely to overestimate the true effect of adherence (a social desirability effect). This would be a particular problem if there was differential bias, i.e., if overestimation was greater in the intervention condition than in the comparator condition. However, the small number of studies that used electronic monitoring devices to measure adherence also had positive ESs, which supports the overall conclusions. It should be noted that objective measures of adherence may also have limitations that need to be considered when interpreting the findings; for example, electronic monitoring may have a reactive effect on behaviour (Sutton et al., Citation2014).
Similar to previous studies (e.g., Peters et al., Citation2015), this review used a multivariable meta-regression model that included several BCTs. However, even though the model could explain a considerable amount of the observed heterogeneity, the variance inflation factor was rather high for most of the BCTs, meaning that they are correlated with each other, and that it is therefore difficult to estimate their independent effects. There may also be study-level characteristics relating to participants, setting, intervention, design, or measures that may partly explain the associations observed between the BCTs and the intervention ES or mask true associations (Peters et al., Citation2015). Examples of possible confounding factors include the socioeconomic status of the participants, follow-up period, and study quality indicators.
In this review, we were unable to code the BCTs used in the comparator groups, due to limited information included in the studies. In similar way to the intervention group, variation in the comparator groups, such as the content, frequency, and duration of information relevant to medication adherence could have influenced the findings of this review (De Bruin, Viechtbauer, Hospers, Schaalma, & Kok, Citation2009; Peters et al., Citation2015). Thus, it would be helpful if future studies provided a full description of the comparator interventions to enable meta-regressions to focus on the differences between the BCTs used in the intervention and comparator conditions.
In conclusion, the findings of this review suggest that automated IVR and SMS interventions can increase medication adherence but highlight the need for intervention studies with better quality designs and objective outcome measures. Future research could also investigate the mechanisms by which the identified BCTs may increase adherence (Kassavou & Sutton, Citation2017). Moreover, future intervention studies could usefully explore the effect of additional techniques (e.g., ‘implementation intentions’) to promote objectively measured medication adherence.
Supplementary Materials
Download Zip (221.3 KB)Acknowledgements
We would like to acknowledge Dr Anna de Simoni for advising on the clinical outcomes. S. S. and A. K. designed the study. A. K. conducted all stages of the review, under the supervision of S. S. Both authors independently conducted data extraction and coding. A. K. drafted and S. S. provided substantial input in writing this manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- *Arora, S., Peters, A. L., Burner, E., Lam, C. N., & Menchine, M. (2014). Trial to examine text message-based mHealth in emergency department patients with diabetes (TExT-MED): A randomized controlled trial. Annals of Emergency Medicine, 63(6), 745–754.e6. doi: 10.1016/j.annemergmed.2013.10.012
- Ball, W. L. (1974). Improving patient compliance with therapeutic regimens: Hamilton symposium examines the problems and solutions. Canadian Medical Association Journal, 3(111), 272–282, PMCID: PMC1947678.
- Barber, N. (2002). Should we consider non-compliance a medical error? Quality and Safety in Health Care, 11(1), 81–84. doi: 10.1136/qhc.11.1.81
- *Bobrow, K., Farmer, A. J., Springer, D., Shanyinde, M., Yu, L. M., Brennan, T., … Levitt, N. (2016). Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-Text Adherence Support [StAR]): A single-blind, randomized trial. Circulation, 133(6), 592–600. doi: 10.1161/CIRCULATIONAHA.115.017530
- Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2014). Comprehensive meta-analysis (version 3). Englewood, NJ: Biostat.
- Chowdhury, R., Khan, H., Heydon, E., Shroufi, A., Fahimi, S., Moore, C., … Franco, O. H. (2013). Adherence to cardiovascular therapy: A meta-analysis of prevalence and clinical consequences. European Heart Journal, 34(38), 2940–2948. doi: 10.1093/eurheartj/eht295
- Cutrona, S. L., Choudhry, N. K., Fischer, M. A., Servi, A., Liberman, J. N., Brennan, T. A., & Shrank, W. H. (2010). Modes of delivery for interventions to improve cardiovascular medication adherence. American Journal of Managed Care, 16(12), 929–942.
- De Bruin, M., Viechtbauer, W., Hospers, H. J., Schaalma, H. P., & Kok, G. (2009). Standard care quality determines treatment outcomes in control groups of HAART-adherence intervention studies: Implications for the interpretation and comparison of intervention effects. Health Psychology, 28(6), 668–674. doi: 10.1037/a0015989
- De Jongh, T., Gurol-Urganci, I., Vodopivec-Jamsek, V., Car, J., & Atun, R. (2012). Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database of Systematic Reviews, 12, CD007459. doi: 10.1002/14651858.CD007459.pub2
- Department of Health. (2012). Improving the use of medicines for better outcomes and reduced waste. An action plan. A report commissioned by the Department of Health.
- *Derose, S. F., Green, K., Marrett, E., Tunceli, K., Cheetham, T. C., Chiu, V. Y., … Scott, R. D. (2013). Automated outreach to increase primary adherence to cholesterol-lowering medications. JAMA Internal Medicine, 173(1), 38–43. doi: 10.1001/2013.jamainternmed.717
- Di Angelantonio, E., Kaptoge, S., Wormser, D., Willeit, P., Butterworth, A. S., Bansal, N., … Danesh, J. (2015). Association of cardiometabolic multimorbidity with mortality. JAMA, 314(1), 52–60. doi: 10.1001/jama.2015.7008
- Egger, M., Smith, G. D., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315, 629–634. doi: 10.1136/bmj.315.7109.629
- Farmer, A., Hardeman, W., Hughes, D., Prevost, A. T., Kim, Y., Craven, A., … Kinmonth, A. L. (2012). An explanatory randomised controlled trial of a nurse-led, consultation-based intervention to support patients with adherence to taking glucose lowering medication for type 2 diabetes. BMC Family Practice, 13, 30. doi: 10.1186/1471-2296-13-30
- Fjeldsoe, B. S., Marshall, A. L., & Miller, Y. D. (2009). Behaviour change interventions delivered by mobile telephone short-message service. American Journal of Preventive Medicine, 36(2), 165–173. doi: 10.1016/j.amepre.2008.09.040
- French, D. P., & Sutton, S. (2010). Reactivity of measurement in health psychology: How much of a problem is it? What can be done about it? British Journal of Health Psychology, 15, 453–468. doi: 10.1348/135910710X492341
- Fuller, J. H., Stevens, L. K., & Wang, S. L. (2001). Risk factors for cardiovascular mortality and morbidity: The WHO multinational study of vascular disease in diabetes. Diabetologia, 44(Suppl. 2), S54–S64.
- Gatwood, J., Balkrishnan, R., Erickson, S. R., An, L. C., Piette, J. D., & Farris, K. B. (2014). Addressing medication nonadherence by mobile phone: Development and delivery of tailored messages. Research in Social and Administrative Pharmacy, 10, 809–23. doi: 10.1016/j.sapharm.2014.01.002
- *Gatwood, J., Balkrishnan, R., Erickson, S. R., An, L. C., Piette, J. D., & Farris, K. B. (2016). The impact of tailored text messages on health beliefs and medication adherence in adults with diabetes: A randomized pilot study. Research in Social and Administrative Pharmacy, 12(1), 130–140. doi: 10.1016/j.sapharm.2015.04.007
- Gollwitzer, P. M., & Bargh, J. A. (2005). Automaticity in goal pursuit. In A. J. Elliot & C. S. Dweck (Eds.), Handbook of competence and motivation (pp. 624–646). New York, NY: The Guilford Press.
- *Guthrie, R. M. (2001). The effects of postal and telephone reminders on compliance with pravastatin therapy in a national registry: Results of the first myocardial infarction risk reduction program. Clinical Therapeutics, 23(6), 970–980.
- Hartmann-Boyce, J., Lancaster, T., & Stead, L. F. (2014). Print-based self-help interventions for smoking cessation. Cochrane Database Systematic Reviews, 6, CD001118. doi: 10.1002/14651858.CD001118.pub3
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327, 557–560. doi: 10.1136/bmj.327.7414.557
- Horne, R., Chapman, S. C., Parham, R., Freemantle, N., Forbes, A., & Cooper, V. (2013). Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the necessity-concerns framework. PLoS ONE, 8(12), e80633. doi: 10.1371/journal.pone.0080633
- *Kamal, A. K., Shaikh, Q., Pasha, O., Azam, I., Islam, M., Memon, A. A., … Khoja, S. (2015). A randomized controlled behavioral intervention trial to improve medication adherence in adult stroke patients with prescription tailored Short Messaging Service (SMS)-SMS4Stroke study. BMC Neurology, 15(1), 2095. doi: 10.1186/s12883-015-0471-5
- Kassavou, A., & Sutton, S. (2017). Reasons for non-adherence to medication and acceptability of an interactive voice response intervention in patients with hypertension and type 2 diabetes in primary care. A qualitative study. BMJ Open. 7:e015597. doi:10.1136/bmjopen-2016-015597
- *Khonsari, S., Subramanian, P., Chinna, K., Latif, L. A., Ling, L. W., & Gholami, O. (2015). Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. European Journal of Cardiovascular Nursing, 14(2), 170–179. doi: 10.1177/1474515114521910
- Kripalani, S., Yao, X., & Haynes, R. B. (2007). Interventions to enhance medication adherence in chronic medical conditions: A systematic review. Archives of Internal Medicine, 167(6), 540–550.
- *Marquez Contreras, E., de la Figuera vov Wichmann, M., Guillen, V. G., Ylla-Catala, A., Figueras, M., Balana, M., & Naval, J. (2004). Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert). Atención Primaria, 34(8), 399–407.
- Michie, S., Jochelson, K., Markham, W. A., & Bridle, C. (2009). Low-income groups and behaviour change interventions: A review of intervention content, effectiveness and theoretical frameworks. Journal of Epidemiology and Community Health, 63(8), 610–622. doi: 10.1136/jech.2008.078725
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., … Wood, C. E. (2013). The behaviour change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behaviour change interventions. Annals of Behavioural Medicine, 46(1), 81–95. doi: 10.1136/jech.2008.078725
- *Migneault, J. P., Dedier, J. J., Wright, J. A., Heeren, T., Campbell, M. K., Morisky, D. E., … Friedman, R. H. (2012). A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: A randomized controlled trial. Annals of Behavioural Medicine, 43(1), 62–73. doi: 10.1007/s12160-011-9319-4
- Mistry, N., Keepanasseril, A., Wilczynski, N. L., Nieuwlaat, R., Ravall, M., & Haynes, R. B. (2015). Technology-mediated interventions for enhancing medication adherence. Journal of the American Medical Informatics Association, 22(e1), e177–193. doi: 10.1093/jamia/ocu047
- Nathan, D. M., Meigs, J., & Singer, D. E. (1997). The epidemiology of cardiovascular disease in type 2 diabetes mellitus: How sweet it is … or is it? Lancet, 350, SI4–SI9. doi: 10.1016/S0140-6736(97)90021-0
- National Institute for Health and Care Excellence. (2009). Medicine adherence. Involving patients in decisions about prescribed medicines and supporting adherence (NICE Clinical Guideline 76). London: NICE.
- National Institute for Health and Care Excellence. (2014). Behaviour change: General approaches. Public health guidelines. Retrieved from: https://www.nice.org.uk/guidance/ph6/evidence/review-decision-2014-545971069
- NCD Risk Factor Collaboration. (2016). Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants. The Lancet, 386(10027), 1513–1530. doi: 10.1016/S0140-6736(16)00618-8
- Nieuwlaat, R., Wilczynski, N., Navarro, T., Hobson, N., Jeffery, R., Keepanasseril, A., … Haynes, R. B. (2014). Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews, 11, Cd000011. doi: 10.1002/14651858.CD000011.pub4
- Orr, J. A., & King, R. J. (2015). Mobile phone SMS messages can enhance healthy behaviour: A meta-analysis of randomised controlled trials. Health Psychology Reviews, 9(4), 397–416. doi: 10.1080/17437199.2015.1022847
- *Park, L. G., Howie-Esquivel, J., Chung, M. L., & Dracup, K. (2014). A text messaging intervention to promote medication adherence for patients with coronary heart disease: A randomized controlled trial. Patient Education and Counselling, 94(2), 261–268. doi: 10.1016/j.pec.2013.10.027
- Park, L. G., Howie-Esquivel, J., & Dracup, K. (2014). A quantitative systematic review of the efficacy of mobile phone interventions to improve medication adherence. Journal of Advanced Nursing, 70(9), 1932–1953. doi: 10.1111/jan.12400
- Peters, G. J. Y., de Bruin, M., & Crutzen, R. (2015). Everything should be as simple as possible, but no simpler: Towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions. Health Psychology Review, 9(1), 1–14. doi: 10.1080/17437199.2013.848409
- *Piette, J. D., Weinberger, M., & McPhee, S. J. (2000). The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: A randomized, controlled trial. Medical Care, 38(2), 218–230.
- Sackett, D. L., & Haynes, B. R. (1976). Compliance with therapeutic regimens. Baltimore, MD: The John Hopkins University Press.
- *Sherrard, H., Duchesne, L., Wells, G., Kearns, S. A., & Struthers, C. (2015). Using interactive voice response to improve disease management and compliance with acute coronary syndrome best practice guidelines: A randomized controlled trial. Canadian Journal of Cardiovascular Nursing, 25(1), 10–15.
- *Sherrard, H., Struthers, C., Kearns, S. A., Wells, G., Chen, L., & Mesana, T. (2009). Using technology to create a medication safety net for cardiac surgery patients: A nurse-led randomized control trial. Canadian Journal of Cardiovascular Nursing, 19(3), 9–15.
- Smith, D. H., O’Keefee-Rosetti, M., Owen-Smith, A. A., Rand, C., Tom, J., Vupputuri, S., … Vollmer, V. W. (2016). Improving adherence to cardiovascular therapies: An economic evaluation of a randomized pragmatic trial. Value Health, 19(2), 176–184. doi: 10.1016/j.jval.2015.11.013
- *Stacy, J. N., Schwartz, S. M., Ershoff, D., & Shreve, M. S. (2009). Incorporating tailored interactive patient solutions using interactive voice response technology to improve statin adherence: Results of a randomized clinical trial in a managed care setting. Population Health Management, 12(5), 241–254. doi: 10.1089/pop.2008.0046
- Sutton, S., Kinmonth, A. L., Hardeman, W., Hughes, D., Boase, S., Prevost, A., … Farmer, A. (2014). Does electronic monitoring influence adherence to medication? Randomized controlled trial of measurement reactivity. Annals of Behavioural Medicine, 48(3), 293–299. doi: 10.1007/s12160-014-9595-x
- Tannenbaum, M. B., Hepler, J., Zimmerman, R. S., Saul, L., Jacobs, S., Wilson, K., & Albarracin, D. (2015). Appealing to fear: A meta-analysis of fear appeal effectiveness and theories. Psychological Bulletin, 141(6), 1178–1204. doi: 10.1037/a0039729
- Thakkar, J., Kurup, R., Laba, T. L., Santo, K., Thiagalingam, A., Rodgers, A., … Chow, C. K. (2016). Mobile telephone text messaging for medication adherence in chronic disease: A meta-analysis. JAMA Internal Medicine, 176(3), 340–349. doi: 10.1001/jamainternmed.2015.7667
- Tinetti, M. E., Fried, T. R., & Boyd, C. M. (2012). Designing health care for the most common chronic conditions-multimorbidity. JAMA, 307(23), 2493–2494. doi: 10.1001/jama.2012.5265
- *Vervloet, M., Linn, A. J., van Weert, J. C., de Bakker, D. H., Bouvy, M. L., & van Dijk, L. (2012). The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: A systematic review of the literature. Journal of American Medical Informatics Association, 19(5), 696–704. doi: 10.1136/amiajnl-2011-000748
- Vervloet, M., van Dijk, L., Santen-Reestman, J., van Vlijmen, B., van Wingerden, P., Bouvy, M. L., & de Bakker, D. H. (2012). SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. International Journal of Medical Informatics, 81(9), 594–604. doi: 10.1016/j.ijmedinf.2012.05.005
- *Vollmer, W. M., Owen-Smith, A. A., Tom, J. O., Laws, R., Ditmer, D. G., Smith, D. H., … Rand, C. S. (2014). Improving adherence to cardiovascular disease medications with information technology. American Journal of Managed Care, 20(11), SP502–SP510.
- *Wald, D. S., Bestwick, J. P., Raiman, L., Brendell, R., & Wald, N. J. (2014). Randomised trial of text messaging on adherence to cardiovascular preventive treatment (INTERACT trial). PLoS One, 9(12), e114268. doi:10.1371/journal.pone.0114268.
- WHO. (2003). Adherence to long-term therapies. Evidence for action.
- WHO. (2016). Cardiovascular diseases. Retrieved from http://www.who.int/cardiovascular_diseases/en/
- York Health Economics Consortium & School of Pharmacy, University of London. (2010). Evaluation of the scale, causes and costs of waste medicines. Report commissioned by the Department of Health.