ABSTRACT
Theories of behaviour used to understand healthcare professional behaviour often focus on the deliberative processes that drive their behaviour; however, less is known about the role that implicit processes such as habit have on healthcare professional behaviour. This systematic review aimed to critically appraise and synthesise research evidence investigating the association between habit and healthcare professional behaviour. A search of five databases (PsycINFO, EMBASE, Scopus and CINAHL) was conducted up until 29 February 2016 to identify studies reporting correlations between habit and healthcare professional behaviours. Meta-analyses were conducted to assess the overall habit-behaviour association across all behaviours. A subgroup analysis assessed whether the habit-behaviour relationship differed depending on whether the behaviour was objectively measured or assessed by self-report. We identified nine eligible studies involving 1975 healthcare professionals that included 28 habit-behaviour correlations. A combined mean r+ of 0.35 (medium effect) was observed between habit and healthcare professional behaviour. The habit-behaviour correlation was not affected by whether behaviour was measured objectively or by self-report. This review suggests that habit plays a significant role in healthcare professional behaviour. Findings may have implications for considering health professionals’ habit when promoting the provision of evidence-based health care, and for breaking existing habit when de-implementing outdated, non-evidence-based practices.
While considerable resources are invested into the development of evidence-based interventions (Røttingen et al., Citation2013), their translation into routine clinical practice is often slow, and one that necessarily involves health professional behaviour change (Grimshaw, Eccles, Lavis, Hill, & Squires, Citation2012; McGlynn et al., Citation2003; Woolf, Citation2008), amongst other factors (May & Finch, Citation2009). Changing health professionals’ behaviour can be challenging, particularly if it involves changing existing, routinised ways of providing care developed through training, experience and further reinforced through daily repetition (Brennan & Mattick, Citation2013; French, Green, Buchbinder, & Barnes, Citation2010; Naikoba & Hayward, Citation2001). An increasing body of literature has demonstrated that drawing upon theories of behaviour can help to identify which modifiable factors can be leveraged to support healthcare professionals in changing their behaviour as they strive to provide health care informed by the latest evidence (Clarkson et al., Citation2008; Eccles et al., Citation2011; Godin, Bélanger-Gravel, Eccles, & Grimshaw, Citation2008; Walker et al., Citation2003).
Expectancy-value social cognition models that highlight the intentional, reflective factors of behaviour (e.g. Theory of Planned Behaviour (TPB); Ajzen, Citation1991) have been the predominant focus for predicting healthcare professionals’ behaviours to date, with a focus on behaviours such as prescribing, examining, and referring (Eccles et al., Citation2007; Harrell & Bennett, Citation1974; Lambert et al., Citation1997) and the use of clinical guidelines more broadly (Kortteisto, Kaila, Komulainen, Mäntyranta, & Rissanen, Citation2010). In a 2008 systematic review, Godin and colleagues identified 72 studies testing whether factors described in social cognition models (such as the TPB) could predict healthcare professionals’ intention and behaviour. A frequency weighted mean R2 of 0.31 was observed for predicting behaviour, and 0.59 for predicting intention (Godin et al., Citation2008). While highlighting the utility of such models for predicting healthcare professional behaviours, a general criticism of expectancy-value social cognition models extends particularly to understanding healthcare professional behaviour: such models do not explicitly theorise or account for the impact that implicit processes such as habit have on behaviour (Aarts, Citation2007; Gardner, Citation2014; Hofmann, Friese, & Wiers, Citation2008; Sheeran, Gollwitzer, & Bargh, Citation2013) or healthcare professional behaviour (Nilsen, Roback, Broström, & Ellström, Citation2012; Presseau, Johnston, Heponiemi et al., Citation2014).
Habit is defined as a phenomenon whereby internal and external cues trigger automatic reactions, based on a learned stimulus-response association (Gardner, Citation2014). Habit develops when a behaviour is repeatedly performed in the presence of contextual cues (Lally, van Jaarsveld, Potts, & Wardle, Citation2010). For example, healthcare professionals working in a hospital are recommended to routinely disinfect their hands before and after patient contact (Fuller et al., Citation2012). Initially, healthcare professionals may have to actively remember to disinfect their hands each time. However, after time and repetition the behaviour is likely to become an automatic reaction (or habit) to seeing the disinfectant dispenser (Fuller et al., Citation2012). Repetition of behaviour in a specific setting strengthens a mental context-behaviour association, which makes alternative behaviours less accessible in memory (Danner, Aarts, & de Vries, Citation2007, Citation2008).
While habit has often been defined as synonymous with repeated behaviour or frequency of past performance, contemporary habit definitions highlight the central role of automaticity: habitual behaviours are automatic in the sense that they rely on less deliberate thinking and awareness (Bargh, Citation1994; Wood, Quinn, & Kashy, Citation2002). The idea that healthcare professional behaviour may be at least partially driven by habit is consistent with dual process models, which distinguish between two systems of cognitive processing (Hofmann et al., Citation2008; Sladek, Phillips, & Bond, Citation2006). The reflective system includes conscious and effortful decision-making, a perspective consistent with good healthcare clinical practice that includes weighing pros and cons. The impulsive system includes processes such as habit, and is characterised by physical and social environmentally-cued responses that are enacted quickly, with less cognitive effort and with less conscious awareness (Gardner, Citation2014; Hofmann et al., Citation2008). According to the Reflective-Impulsive Model (RIM; Hofmann et al., Citation2008), the reflective and impulsive systems operate in parallel, such that the impulsive system is always active whereas the reflective system may be disengaged. For example, a healthcare professional may use a stethoscope to examine a patient’s lungs during a routine health check without the engagement of the reflective system. However, if the healthcare professional detects any irregularities in breathing (e.g. crackling sound), then the reflective system may the engaged to find a suitable diagnosis (though such diagnostic decisions may also be driven by more impulsive considerations driven by heuristics, such as the availability heuristic (Tversky & Kahneman, Citation1973)). Triandis’ Theory of Interpersonal Behaviour (TIP; Triandis, Citation1977) is another theory that considers habit as a determinant of behaviour. In the TIP, habit is defined as the level of routinisation of a behaviour, or the frequency with which it occurs. The theory poses two habit-related hypotheses: First, that there is a positive relationship between habit and behaviour; and second, that as habit strength increases the relationship between intention and behaviour diminishes. For example, initially nurses in training may only disinfect their hands if they feel motivated and actively remember to do so. However, after sufficient repetition in the presence of relevant cues they may form a habit of disinfecting their hands each time they encounter a disinfectant dispenser, even if they feel tired or unmotivated. Operant Learning Theory (OLT; Skinner, Citation1953) proposes further habit-formation related processes. According to OLT, one way that behaviour changes is in response to exposure to positive reinforcement – positive consequences that lead to repetition of behaviour and thus habit formation. For example, providing healthcare professionals with financial rewards when they engage in a particular practice may positively reinforce that behaviour and lead to repetition, thus promoting habit formation (Flodgren et al., Citation2011). Lastly, there has been theorising on how habit relates to volitional constructs such as implementation intentions (‘If-then’ plans) (Gollwitzer, Citation1999), action planning (planning when, where and how to act), and coping planning (planning how to overcome pre-identified barriers) (Kwasnicka, Presseau, White, & Sniehotta, Citation2013; Sniehotta, Scholz, & Schwarzer, Citation2005; Sniehotta, Scholz, & Schwarzer, Citation2006). There is evidence in healthcare professionals suggesting that planning promotes the formation of mental cue-response links, which enable the habitual enactment of behaviour (Potthoff, Presseau, Sniehotta, Elovainio, & Avery, Citation2017). An example of an action plan could be ‘If a patient’s BMI is out of the recommended range, then I will provide physical activity advice using an evidence-based leaflet’.
Some evidence suggests that the impulsive component of healthcare professional behaviour is a predictor of guideline-recommended diabetes care, alongside reflective processes (Potthoff et al., Citation2017; Presseau, Johnston, Heponiemi et al., Citation2014). However, it remains unclear to what extent the impulsive system or habit has been investigated in relation to understanding it as a predictor of healthcare professionals’ behaviour. A systematic review and meta-analysis by Gardner, de Bruijn, and Lally (Citation2011) found a medium association between habit and health behaviours (i.e. nutrition and physical activity behaviours) in a general population (23 bivariate correlations, k = 22; fixed: r+ = 0.44; random: r+ = 0.46) (Gardner et al., Citation2011). However, there is currently no systematic review reporting on the impulsive system or habit that synthesises the evidence in relation to healthcare professionals’ behaviour.
The primary aim of the present systematic review was to synthesise the overall strength of association between indicators of habit and healthcare professional behaviour. A secondary aim was to investigate whether a priori defined moderators could explain the strength of the habit-behaviour association including experience, professional role, type of behaviour measure and type of behaviour. We hypothesised that the association between habit and behaviour would be stronger in more experienced healthcare professionals, as they would have repeated the same behaviours more frequently over the years. This is in line with dual process models (Benner, Citation1982; Reyna, Citation2008) which propose that experts often rely on intuitive reasoning rather than analytical reasoning. We also aimed to examine whether professional role (e.g. General Practitioners [GP] vs. nurses) could affect the strength of the habit-behaviour association. We hypothesised that some roles would require performing specific behaviours more frequently which would increase habit strength (e.g. doctors prescribe medication more frequently than nurses) (Godin et al., Citation2008). With regards to the type of behaviour, we hypothesised that habit might play a more important role in behaviours that are performed frequently in a stable context with a clear cue preceding the behaviour (e.g. examining behaviours) (Gardner, Citation2014). Lastly, we hypothesised that the habit-behaviour association would be stronger if behaviour was measured via self-report, because this may inflate the observed effect (Paulhus, Citation1986).
Methods
Search strategy and study selection
This systematic review followed a registered protocol (Potthoff et al., Citation2015). Electronic databases (MEDLINE, PsycINFO, EMBASE, Scopus and CINAHL) were searched for eligible studies published from inception until 29 February 2016 (see search strategy for PsycINFO in Supplementary File 1). A comprehensive search strategy was used, combining keywords, MeSH headings, and synonyms: habit AND healthcare professionals. Two researchers independently screened all references obtained during the search in two stages against predefined eligibility criteria, a third reviewer was consulted to resolve any discrepancies. Stage 1 screening involved screening titles, abstracts, and keywords to source potentially relevant studies. Stage 2 screening involved full-text screening of all articles retained at stage 1 using a standardised study selection form.
Study inclusion and exclusion criteria
We included studies that quantitatively assessed the association between habit and healthcare professional care delivery behaviour (e.g. prescribing, providing referrals, examinations, test ordering) from any health care setting. Studies were included if they were written in English, published in peer review journals, and reported analyses of primary data of the following research designs: randomised controlled trials (RCTs), cluster-randomised controlled trials, prospective cohort studies, and cross-sectional studies. Studies could include any healthcare professionals (e.g. general practitioners, nurses, dentists) involved in delivering care to patients. Studies had to report an objective (e.g. electronic patient records) and/or self-reported (e.g. questionnaire) measure of both habit and healthcare professional behaviour. Healthcare professional behaviour was defined as any behaviour performed by healthcare professionals in any health care setting.
Data extraction
Two reviewers independently extracted data from included studies using a standardised data extraction form assessing: sample size (open), study design, main theory used (open), population characteristics (i.e. role, age, gender and years of experience), behavioural characteristics (i.e. definition and type of measure used to assess behaviour), correlation(s) between habit and healthcare professional behaviour, and means and standard deviations of healthcare professional behaviour and habit. For intervention studies, baseline measures of the correlation between habit and healthcare professional behaviour were extracted and combined for treatment and control groups. Baseline estimates were used to avoid an overestimation of the habit-behaviour relationship that could be expected when using post-intervention correlation estimates.
To appraise the methodological quality of the studies two reviewers (SP and MM) independently assessed the quality of included studies (good, fair or poor) using an adapted version of the quality assessment tool for observational cohort and cross-sectional studies (see Supplementary File 2) (National Heart, Lung, and Blood Institute, Citation2016). The tool assesses methodological criteria relating to study procedures, design, and outcome measure. Inter-rater agreement was calculated using Cohen’s Kappa coefficient (Cohen, Citation1992). Researchers resolved any disagreements through discussion.
Data synthesis
A meta-analysis was undertaken to determine the overall strength of the association between habit and healthcare professional behaviour (Comprehensive Meta-Analysis Version 2 software; Borenstein, Hedges, Higgins, & Rothstein, Citation2005). The strength of association between habit and healthcare professional behaviour was calculated using Pearson’s product-moment correlation coefficients (r) (Pearson, Citation1929) with Fisher’s Z transformations for weighted average effect sizes (r+), and respective 95% confidence intervals (CIs) (Mudholkar, Citation1983). Random effects models were used to make inferences about the probable effects found in the populations from which the studies have been sampled (Borenstein, Hedges, Higgins, & Rothstein, Citation2009). For datasets that provided multiple behaviour outcomes and therefore multiple habit-behaviour correlations, a weighted mean combined correlation was used (e.g. a composite variable that corresponds to the mean correlation between habit A and behaviour A, and the mean of habit B and behaviour B) (Borenstein et al., Citation2009). In accordance with Cohen’s guidelines (Cohen, Citation1992), correlation coefficients of 0.10, 0.30, and 0.50 were judged to be small, medium, and large in size, respectively. To explore the robustness of the findings, sensitivity analyses were performed to explore whether removing included studies would affect the strength of the overall habit-behaviour association.
Statistical heterogeneity was assessed using Cochran’s Q and I2 (Higgins, Thompson, Deeks, & Altman, Citation2003). When I2 was over 75%, heterogeneity was judged as high, and when below 25% it was judged as low (Borenstein, Hedges, Higgins, & Rothstein, Citation2010).
Subgroup analyses were conducted to assess whether any of the moderator variables would have an effect on the habit-behaviour relationship. Q statistics were calculated to assess between-study variability (QB) associated with potential moderators and to assess heterogeneity within each the subgroups (QW) (Borenstein et al., Citation2009).
Results
Study characteristics
We identified nine studies eligible for inclusion; all were conducted in the United Kingdom (see ). The total sample size was N = 1975 and the mean between-study sample size was N = 247. Seven studies used a cross-sectional design with only one measurement point and two studies used a prospective design with a baseline and a 12-month follow-up. Eight studies were part of three larger predictive studies (Bonetti et al., Citation2010; Bonetti et al., Citation2006; Eccles et al., Citation2007; Eccles et al., Citation2012; Grimshaw et al., Citation2011; Presseau, Johnston, Francis et al., Citation2014; Presseau, Johnston, Heponieni et al., Citation2014) and one study was an independent RCT (Hrisos et al., Citation2008). The studies reported 28 bivariate habit-behaviour relationships related to twelve different healthcare professional behaviours, including prescribing, advising and examining practices (see for all included behaviours). Four studies included General Dental Practitioners and five included General Medical Practitioners. Four studies included an objective measure of healthcare professional behaviour and seven studies included self-reported measures of behaviour, including simulated behaviour measures. Simulated behaviour measures included literature- and expert-informed clinical scenarios wherein healthcare professionals were asked to report the action that they would take in each scenario, and responses were summed to create a total score.
Table 1. Study characteristics.
Habit was measured using self-reported questionnaires in all included studies, with seven using the 2–3 item ‘Evidence of Habit’ measure (Blackman, Citation1974; Bonetti et al., Citation2006; Bonetti et al., Citation2010; Bonetti, Johnston, Clarkson, & Turner, Citation2009; Walker et al., Citation2003), one study using the twelve-item Self-Reported Habit Index (SRHI; Presseau, Jonston, Francis et al., Citation2014; Verplanken & Orbell, Citation2003), and one study using the 4-item Self-Reported Behavioural Automaticity Index (SRBAI; Gardner, Abraham, Lally, & de Bruijn, Citation2012; Presseau, Johnston, Heponiemi et al., Citation2014). Alpha coefficients for the habit measures ranged from α = 0.50–0.96, with the majority of the alphas in the acceptable (α = 0.70) to good (α = 0.90) range. The ‘Evidence of Habit’ measure used two or three items that followed a stem (e.g. ‘When I see a patient’) and focused on automaticity (e.g. ‘I automatically consider taking a radiograph’). The SRHI included a stem describing the behaviour (e.g. ‘Providing advice about weight management’) and the target (e.g. ‘to patients whose BMI is above target is something … ’) followed by twelve items that described three facets of automaticity – lack of awareness (‘ … I do without thinking’), lack of control (‘ … that would require effort not to do’), and efficiency (‘ … I have no need to think about doing’) – behavioural frequency (‘ … I do frequently’) and self-identity (‘ … that’s typically “me”’). The SRBAI used a subset of SRHI items, focusing on automaticity. Eight studies assessed habit as part of an operationalisation of Operant Learning Theory (Blackman, Citation1974) and one study applied a Dual Processing approach.
Methodological quality of included studies
The methodological quality of seven studies were rated as fair (Bonetti et al., Citation2006; Bonetti et al., Citation2009; Bonetti et al., Citation2010; Eccles et al., Citation2006; Eccles et al., Citation2012; Grimshaw et al., Citation2011; Hrisos et al., Citation2008), two studies rated as good quality (Presseau, Johnston, Francis et al., Citation2014; Presseau, Johnston, Heponiemi et al., Citation2014) and no studies were rated as poor (see ). Limitations of studies rated as ‘fair’ related to design (i.e. cross-sectional) and low response rates (i.e. ranging between 21-48%). Studies rated as ‘good’ had prospective designs (habit was measured prior to behaviour), allowing inferences on temporal sequencing, and reported response rates greater than 50%.
Table 2. Quality assessment.
Habit-behaviour correlations
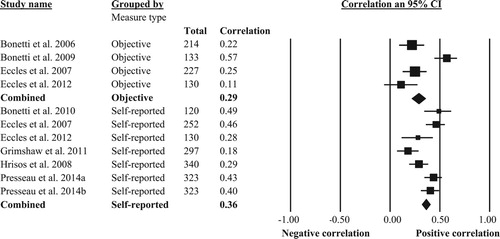
The combined correlation between habit and healthcare professional behaviour across all studies was r+ = 0.35 (k = 9, 95% CI [0.27, 0.43], p < .001), suggesting a moderate association (; see CMA raw data file in Supplementary File 3). The observed correlation was small in four studies (i.e. r < 0.30; Bonetti et al., Citation2006; Eccles et al., Citation2012; Grimshaw et al., Citation2011; Hrisos et al., Citation2008) and the remaining five studies had moderate effects (i.e. r < 0.30; Bonetti et al., Citation2009; Bonetti et al., Citation2010; Eccles et al., Citation2007; Presseau, Johnston, Francis et al., Citation2014; Presseau, Johnston, Heponiemi et al., Citation2014). Visual inspection of residual plots indicated that there were no outliers. There was a large degree of heterogeneity (Q = 37.27, p < .001; I2 = 78.54), suggesting that variance could not be explained by sampling error alone.
Figure 2. Forest plot of pooled correlation between habit and healthcare professional behaviour. For studies that used multiple behaviour outcomes, mean within-study correlations were used to calculate the pooled between-study habit-behaviour correlation.
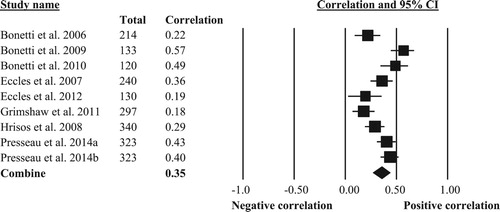
We conducted two sensitivity analyses to explore the robustness of the observed effects in light of studies that contributed more than one effect size (i.e. Eccles et al., Citation2012; Eccles et al., Citation2007; Presseau, Johnston, Francis et al., Citation2014; Presseau, Johnston, Heponiemie et al., Citation2014). Removing any of the included studies from the analysis only marginally affected the overall estimate. Removing the study by Bonetti et al. (Citation2009) resulted in the largest reduction in effect size, however, even with this study being removed there was still a moderate association (r+ = 0.33 [k = 8, p < .001]). Excluding the four studies reporting multiple effect sizes also only marginally affected the overall estimate (r+ = 0.31, k = 5, 95% CI [0.26, 0.36], p < 0.001). These findings support the robustness of the observed overall effect.
Moderator analyses
A subgroup analysis was performed for the moderator ‘Type of behaviour measure’. There was insufficient data available to analyse subgroups for type of behaviour, experience, and professional role. There was no significant difference (Q = 0.63, p = .43) in the strength of association between habit and healthcare professional behaviour between studies with an objective (r+ = 0.30, k = 4, 95% CI [15%, 43%]) or self-report measure of healthcare professional behaviour (r+ = 0.37, k = 7, 95% CI [26%, 46%]) (see ). Screenshots of all the performed analysis can be found in Supplementary File 4.
Discussion
We systematically reviewed the literature to identify studies assessing habit and healthcare professional behaviour and sought to quantify the overall strength of the association between habit and behaviour by means of meta-analysis. Given the continued need for updating clinical practice in light of new research evidence and the persistent finding that the transfer of such evidence into practice remains challenging, there is a need to better understand the factors that promote and limit healthcare professional behaviour change.
Results highlight the potential importance of habit and the role of implicit, cue-driven processes that underlie healthcare professional behaviour though should be interpreted with due care given the small number of studies identified. The observed combined correlation between habit and healthcare professional behaviour across nine studies was r+ = 0.35, consistent with a medium effect size. This correlation is smaller than the combined correlation that was estimated in the review published by Gardner et al. (Citation2011) (r+ = 0.44) that investigated habit and health behaviours in a general population sample. One explanation for the smaller correlation could be that Gardner et al.’s (Citation2011) review included two narrowly defined behaviours (i.e. nutrition and physical activity behaviours), whereas the current review included a range of different healthcare professional behaviours, summarised in five broad categories (i.e. advising, examining, prescribing, providing dental treatment and referring). Furthermore, Gardner et al. (Citation2011) review was restricted to applications of the Self-Reported Habit Index, whereas the present review included three different types of habit measures, which may have increased heterogeneity.
The strength of the association between habit and healthcare professional behaviour did not significantly differ depending on whether behaviour was assessed objectively or by self-report, possibly due to the limited number of studies included. In line with previous research (Godin et al., Citation2008), the combined correlation between habit and objective measures of behaviour was slightly smaller (r+ = 0.30) when compared to that between habit and self-reported measures of behaviour (r+ = 0.37), however, this difference was not significant.
While we aimed to explore a priori defined moderators of the habit-behaviour relationship (e.g. experience, professional role, and type of behaviour), unfortunately, the small number of included studies was insufficient to justify conducting most of these moderator analyses. Further research assessing the relationship between habit and healthcare professional behaviour should hypothesise and test factors that may influence the habit-behaviour relationship, which could draw from theory and evidence from other settings.
For instance, Hoffman et al.’s extension of the Reflective-Impulsive Model (RIM; Hofmann et al., Citation2008) defines a number of situational and dispositional boundary conditions that may influence the habit-behaviour relationship in healthcare professional behaviours, such as low self-regulatory resources (e.g. due to fatigue or stress) which may favour actions driven by the impulsive system (including habitual behaviour). This is consistent with Linder et al. (Citation2014), who found that inappropriate antibiotic prescribing for acute respiratory infection became more likely during the late morning and afternoon clinic session.
Behavioural frequency and stability of the context are also well-theorised characteristics that may help distinguish between behaviours that are more or less conducive to habit formation (Ouellette & Wood, Citation1998). Clinical behaviours preceded by a salient environmental cue (e.g. soap dispenser initiating hand washing) may be more likely to become habitual and could inform interventions targeting implicit processes and habit formation in healthcare professionals. Furthermore, as habit strength increases with repetition over time, research could further explore the follow-up time between the measurement of behaviour and the measurement of habit as a potential moderator (Lally et al., Citation2010).
Features of the clinical behaviour itself may also be moderators. For instance, the complexity of a given clinical behaviour may moderate the habit-behaviour relationship, with less complex behaviours (e.g. hand washing) potentially being more conducive to habit formation than more complex behaviours (e.g. providing smoking cessation advice) (Wood et al., Citation2002). Finally, in line with Self-Determination Theory, intrinsically motivated behaviours may be more likely to become habitual (Gardner & Lally, Citation2013; Ryan & Deci, Citation2000). Clinical behaviours that fulfil the need for relatedness, competence, and autonomy may be more satisfying, and may prompt repetition and habit formation (Ryan & Deci, Citation2000). To our knowledge, this has not yet been investigated in health care professional behaviours.
All studies identified in our review relied on self-reported measures of habit strength. Examining habit using self-reported measures is problematic because one of the defining facets of habit is that it operates outside a person’s awareness. When participants are asked to rate to what extent a given behaviour was automatic they were most likely making an inference about their behaviour based on the consequence of the habit (e.g. hand washing habit inferred from empty soap dispenser) (Sniehotta & Presseau, Citation2012). Another issue is the construct validity of measures such as the SRHI, which may conflate habit with constructs that are not necessarily part of habit (i.e. behaviour frequency and self-identity) (Gardner, Citation2014). The 4-item SRBAI, a subscale of the SRHI which focuses on automaticity as the core facet of habit, may offer a theoretically parsimonious alternative that can be administered in a healthcare setting with little response burden (Gardner et al., Citation2012). The present review did not identify any other forms of habit measures used in a clinical setting, however, there are alternative – possibly more accurate – ways of measuring habit. For example, video observations in combination with qualitative analyses (e.g. conversation analysis) might offer a promising way of examining cues and habitual behaviours by studying interaction, acknowledging both verbal and non-verbal cues (Drew, Chatwin, & Collins, Citation2001).
Another way of advancing measurement could involve investigating physiological correlates of habit such as pupil dilation or skin conductance response (Juvrud et al., Citation2018). Virtual reality presents novel opportunities for creating immersive environments with visual and acoustic cues that mirror the clinical context and allow repetition of clinical behaviours to enable the measurement of habit formation (or the breaking of habit). This technology could be used with novel intra-individual designs (McDonald et al., Citation2017) further allowing the personalisation of cues. Such designs have already been applied in general population samples to examine habit formation (Lally et al., Citation2010) and their utility in studying cognitive processes in healthcare professionals has also been demonstrated (Johnston et al., Citation2015).
This systematic review highlighted that most current studies assessed habit and behaviour at the same time. Cross-sectional designs are problematic because of the lack of capacity to ascribe an order of effect and because of common method variance (Lindell & Whitney, Citation2001). While the problem of common method variance does not apply to those studies which measured healthcare professional behaviour using objective measures, only four studies used objective measures of behaviour (Bonetti et al., Citation2006; Bonetti et al., Citation2009; Eccles et al., Citation2007; Eccles et al., Citation2012). Another limitation of included studies was the low response rate (below 50%) in seven of the nine studies. These results compare unfavourably with other postal survey studies in healthcare professionals which typically have response rates of at least 61% (Cook, Dickinson, & Eccles, Citation2009). Future studies should try to incorporate effective recruitment and retention strategies, using financial compensation or other ways of rewarding completion of questionnaires (Flodgren et al., Citation2011). Furthermore, studies could embed habit measures alongside trials of intervention aiming to change (create or break) healthcare professionals’ habits (Presseau et al., Citation2018). This could involve a process evaluation whereby habit is measured at baseline and after an active habit change intervention. Such designs would help to substantiate findings from correlational studies and further clarify the role of habit in relation to healthcare professional behaviour.
Strengths and limitations of this systematic review
A key limitation of the current meta-analysis is the small number of included studies. While sensitivity analyses largely support the robustness of observed effects, findings should be interpreted with caution as a relatively small number of studies with null or smaller effect sizes could substantially alter the conclusion of this review. While findings point to the potential relevance of habit as a construct of interest in understanding healthcare professional behaviour, there is a clear need for additional primary studies to ensure that more precise estimates of effect can be synthesised in the future.
All included studies were conducted in the UK and many involved the same authors. While this favoured consistency in measurement of behaviour and habit, there is a need to conduct studies examining the habit–behaviour relationship in other countries by other teams using consistent or improved measurement.
Although we found a significant overall correlation between habit and healthcare professional behaviour, we also found a high level of heterogeneity between studies that could not (fully) be accounted for by the moderator that we were able to examine. The limited number of studies limits the conclusions that can be drawn from the moderator analysis, as non-significant effects may be due to low statistical power (Borenstein et al., Citation2009). Although inspection of publication bias did not reveal significant asymmetry, this may be due to low power in detecting real asymmetries as a result of the limited number of studies (Sterne & Egger, Citation2001). As this literature matures, there will be further opportunities for studies to continue to hypothesise and test potential moderators of the habit-behaviour relationship healthcare professionals as outlined herein.
Conclusions
To our knowledge this is the first systematic review aiming to quantify the strength of association between habit and healthcare professional behaviour. The review showed that many aspects of healthcare have an element of measurable routine that accounts for variability in the healthcare provided. Habit allows healthcare professionals to use their skills and training quickly and efficiently, minimising the cognitive load of active weighing of pros and cons in every clinical situation. However, when clinical guidelines of best practice change as new evidence and new interventions come to light, so too must behaviour. This review discussed current conceptualisations of habit and how these relate to healthcare professional behaviour. This review also suggests that future research should focus on further theorising the processes and mechanisms involved in habit formation and breaking habit, as well as the boundary conditions that trigger the impulsive system driving habit, as well as primary studies testing such models.
PRISMA and MARS
The reported meta-analyses and systematic review comply with international standards and a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement is included as part of the supplementary files (see Supplementary File 5) for the review.
Acknowledgements
The authors would like to acknowledge and thank Mr Andrew Bryant and Dr Colin Muirhead for their statistical advice.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Sebastian Potthoff http://orcid.org/0000-0003-4580-8532
Falko F. Sniehotta http://orcid.org/0000-0003-1738-4269
Fiona Beyer http://orcid.org/0000-0002-6396-3467
Leah Avery http://orcid.org/0000-0003-3578-1209
Justin Presseau http://orcid.org/0000-0002-2132-0703
Additional information
Funding
References
- Aarts, H. (2007). Health and goal-directed behavior: The nonconscious regulation and motivation of goals and their pursuit. Health Psychology Review, 1(1), 53–82. doi: 10.1037/0022-3514.92.2.165
- Ajzen, I. (1991). The theory of planned behaviour. Organizational Behaviour and Human Decision Processes, 50, 179–211. doi: 10.1016/0749-5978(91)90020-T
- Bargh, J. A. (1994). The four horsemen of automaticity: Awareness, intention, efficiency, and control in social cognition. In R. S. Wyer & T. K. Srull (Eds.), Handbook of social cognition (pp. 1–40). Hillsdale, NJ: Lawrence Erlbaum.
- Benner, P. (1982). From novice to expert. AJN The American Journal of Nursing, 82(3), 402–407. doi: 10.2307/3462928
- Blackman, D. (1974). Operant conditioning: An experimental analysis of behavior. London: Methuen.
- Bonetti, D., Johnston, M., Clarkson, J. E., Grimshaw, J., Pitts, N. B., Eccles, M., … Glidewell, L. (2010). Applying psychological theories to evidence-based clinical practice: Identifying factors predictive of placing preventive fissure sealants. Implementation Science, 5(1), 25. doi: 10.1186/1748-5908-5-25
- Bonetti, D., Johnston, M., Clarkson, J., & Turner, S. (2009). Applying multiple models to predict clinicians’ behavioural intention and objective behaviour when managing children's teeth. Psychology and Health, 24(7), 843–860. doi: 10.1080/08870440802108918
- Bonetti, D., Pitts, N. B., Eccles, M., Grimshaw, J., Johnston, M., Steen, N., … Clarkson, J. E. (2006). Applying psychological theory to evidence-based clinical practice: Identifying factors predictive of taking intra-oral radiographs. Social Science & Medicine, 63(7), 1889–1899. doi: 10.1016/j.socscimed.2006.04.005
- Borenstein, M., Hedges, L. V., Higgins, J., & Rothstein, H. R. (2005). Comprehensive meta-analysis version 2. Engelwood, NJ: Biostat.
- Borenstein, M., Hedges, L. V., Higgins, J., & Rothstein, H. R. (2009). Introduction to meta-analysis. Chichester: Wiley & Sons.
- Borenstein, M., Hedges, L. V., Higgins, J., & Rothstein, H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. doi: 10.1002/jrsm.12
- Brennan, N., & Mattick, K. (2013). A systematic review of educational interventions to change behaviour of prescribers in hospital settings, with a particular emphasis on new prescribers. British Journal of Clinical Pharmacology, 75(2), 359–372. doi: 10.1111/j.1365-2125.2012.04397.x
- Clarkson, J. E., Turner, S., Grimshaw, J. M., Ramsay, C. R., Johnston, M., Scott, A., … Ibbetson, R. (2008). Changing clinicians’ behavior: A randomized controlled trial of fees and education. Journal of Dental Research, 87(7), 640–644. doi: 10.1177/154405910808700701
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155. doi: 10.1037/0033-2909.112.1.155
- Cook, J. V., Dickinson, H. O., & Eccles, M. P. (2009). Response rates in postal surveys of healthcare professionals between 1996 and 2005: An observational study. BMC Health Services Research, 9(1), 160. doi: 10.1186/1472-6963-9-160
- Danner, U. N., Aarts, H., & de Vries, N. K. (2007). Habit formation and multiple means to goal attainment: Repeated retrieval of target means causes inhibited access to competitors. Personality and Social Psychology Bulletin, 33(10), 1367–1379. doi: 10.1177/0146167207303948
- Danner, U. N., Aarts, H., & de Vries, N. K. (2008). Habit vs. intention in the prediction of future behaviour: The role of frequency, context stability and mental accessibility of past behaviour. British Journal of Social Psychology, 47(Pt 2), 245–265. doi: 10.1348/014466607X230876
- Drew, P., Chatwin, J., & Collins, S. (2001). Conversation analysis: A method for research into interactions between patients and health-care professionals. Health Expectations, 4(1), 58–70. doi: 10.1046/j.1369-6513.2001.00125.x
- Eccles, M. P., Grimshaw, J. M., Johnston, M., Steen, N., Pitts, N. B., Thomas, R., … Walker, A. (2007). Applying psychological theories to evidence-based clinical practice: Identifying factors predictive of managing upper respiratory tract infections without antibiotics. Implementation Science, 2(1), 26. doi: 10.1186/1748-5908-2-26
- Eccles, M. P., Grimshaw, J. M., MacLennan, G., Bonetti, D., Glidewell, L., Pitts, N. B., … Johnston, M. (2012). Explaining clinical behaviors using multiple theoretical models. Implementation Science, 7(1), 99. doi: 10.1186/1748-5908-7-99
- Eccles, M. P., Hrisos, S., Francis, J. J., Kaner, E. F. S., Dickinson, H. O., Beyer, F., & Johnston, M. (2006). Do self-reported intentions predict clinicians’ behaviour: A systematic review. Implementation Science, 1, doi: 10.1186/1748-5908-1-28
- Eccles, M. P., Hrisos, S., Francis, J. J., Stamp, E., Johnston, M., Hawthorne, G., … Presseau, J. (2011). Instrument development, data collection, and characteristics of practices, staff, and measures in the improving quality of care in diabetes (iQuaD) study. Implementation Science, 6(1), 61. doi: 10.1186/1748-5908-6-61
- Flodgren, G., Eccles, M. P., Shepperd, S., Scott, A., Parmelli, E., & Beyer, F. R. (2011). An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database of Systematic Reviews, 7(7). doi: 10.1002/14651858.CD009255
- French, S. D., Green, S., Buchbinder, R., & Barnes, H. (2010). Interventions for improving the appropriate use of imaging in people with musculoskeletal conditions. The Cochrane Library, doi: 10.1002/14651858
- Fuller, C., Michie, S., Savage, J., McAteer, J., Besser, S., Charlett, A., … Duckworth, G. (2012). The feedback intervention trial (FIT) – improving hand-hygiene compliance in UK healthcare workers: A stepped wedge cluster randomised controlled trial. PLoS One, 7(10), e41617. doi: 10.1371/journal.pone.0041617
- Gardner, B. (2014). A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behaviour. Health Psychology Review, 1–19. doi: 10.1080/17437199.2013.876238
- Gardner, B., Abraham, C., Lally, P., & de Bruijn, G.-J. (2012). Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the self-report habit index. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 112. doi: 10.1186/1479-5868-9-102
- Gardner, B., de Bruijn, G.-J., & Lally, P. (2011). A systematic review and meta-analysis of applications of the self-report habit index to nutrition and physical activity behaviours. Annals of Behavioral Medicine, 42(2), 174–187. doi: 10.1007/s12160-011-9282-0
- Gardner, B., & Lally, P. (2013). Does intrinsic motivation strengthen physical activity habit? Modeling relationships between self-determination, past behaviour, and habit strength. Journal of Behavioral Medicine, 36(5), 488–497. doi: 10.1007/s10865-012-9442-0
- Godin, G., Bélanger-Gravel, A., Eccles, M. P., & Grimshaw, J. (2008). Healthcare professionals’ intentions and behaviours: A systematic review of studies based on social cognitive theories. Implementation Science, 3(1), 36. doi: 10.1186/1748-5908-3-36
- Gollwitzer, P. M. (1999). Implementation intentions: Strong effects of simple plans. American Psychologist, 54, 493–503. doi: 10.1037/0003-066X.54.7.493
- Grimshaw, J. M., Eccles, M. P., Lavis, J. N., Hill, S. J., & Squires, J. E. (2012). Knowledge translation of research findings. Implementation Science, 7(1), 50. doi: 10.1186/1748-5908-7-50
- Grimshaw, J. M., Eccles, M. P., Steen, N., Johnston, M., Pitts, N. B., Glidewell, L., … Walker, A. (2011). Applying psychological theories to evidence-based clinical practice: Identifying factors predictive of lumbar spine x-ray for low back pain in UK primary care practice. Implementation Science, 6(1), 55. doi: 10.1186/1748-5908-6-55
- Harrell, G. D., & Bennett, P. D. (1974). An evaluation of the expectancy value model of attitude measurement for physician prescribing behavior. Journal of Marketing Research, 269–278. doi: 10.2307/3151142
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560. doi: 10.1136/bmj.327.7414.557
- Hofmann, W., Friese, M., & Wiers, R. W. (2008). Impulsive versus reflective influences on health behavior: A theoretical framework and empirical review. Health Psychology Review, 2(2), 111–137. doi: 10.1080/17437190802617668
- Hrisos, S., Eccles, M., Johnston, M., Francis, J., Kaner, E. F. S., Steen, N., & Grimshaw, J. (2008). An intervention modelling experiment to change GPs’ intentions to implement evidence-based practice: Using theory-based interventions to promote GP management of upper respiratory tract infection without prescribing antibiotics# 2. BMC Health Services Research, 8(1), 10. doi: 10.1186/1472-6963-8-10
- Johnston, D., Bell, C., Jones, M., Farquharson, B., Allan, J., Schofield, P., … Johnston, M. (2015). Stressors, appraisal of stressors, experienced stress and cardiac response: A real-time, real-life investigation of work stress in nurses. Annals of Behavioral Medicine, 50(2), 187–197. doi: 10.1007/s12160-015-9746-8
- Juvrud, J. C., Gredebäck, G., Åhs, F., Lerin, N., Nyström, P., Kastrati, G., & Rosén, J. (2018). The immersive virtual reality lab: Possibilities for remote experimental manipulations of autonomic activity on a large scale. Frontiers in Neuroscience, 12, 305. doi: 10.3389/fnins.2018.00305
- Kortteisto, T., Kaila, M., Komulainen, J., Mäntyranta, T., & Rissanen, P. (2010). Healthcare professionals’ intentions to use clinical guidelines: A survey using the theory of planned behaviour. Implementation Science, 5(1), 51. doi: 10.1186/1748-5908-5-51
- Kwasnicka, D., Presseau, J., White, M., & Sniehotta, F. F. (2013). Does planning how to cope with anticipated barriers facilitate health-related behaviour change? A systematic review. Health Psychology Review, 7(2), 129–145. doi: 10.1080/17437199.2013.766832
- Lally, P., van Jaarsveld, C. H. M., Potts, H. W. W., & Wardle, J. (2010). How are habits formed: Modelling habit formation in the real world. European Journal of Social Psychology, 40(6), 998–1009. doi: 10.1002/ejsp.674
- Lambert, B. L., Salmon, J. W., Stubbings, J., Gilomen-Stūdy, G., Valuck, R. J., & Kezlarian, K. (1997). Factors associated with antibiotic prescribing in a managed care setting: An exploratory investigation. Social Science & Medicine, 45(12), 1767–1779. doi: 10.1016/S0277-9536(97)00108-1
- Lindell, M. K., & Whitney, D. J. (2001). Accounting for common method variance in cross-sectional research designs. Journal of Applied Psychology, 86(1), 114. doi: 10.1037//0021-9010.86.1.114
- Linder, J. A., Doctor, J. N., Friedberg, M. W., Nieva, H. R., Birks, C., Meeker, D., & Fox, C. R. (2014). Time of Day and the decision to prescribe antibiotics. JAMA Internal Medicine, 174(12), 2029–2031. doi: 10.1001/jamainternmed.2014.5225
- May, C., & Finch, T. (2009). Implementing, embedding, and integrating practices: An outline of normalization process theory. Sociology, 43(3), 535–554. doi: 10.1177/0038038509103208
- McDonald, S., Quinn, F., Vieira, R., O’Brien, N., White, M., Johnston, D. W., & Sniehotta, F. F. (2017). The state of the art and future opportunities for using longitudinal n-of-1 methods in health behaviour research: A systematic literature overview. Health Psychology Review, 11(4), 307–323. doi: 10.1080/17437199.2017.1316672
- McGlynn, E. A., Asch, S. M., Adams, J., Keesey, J., Hicks, J., DeCristofaro, A., & Kerr, E. A. (2003). The quality of health care delivered to adults in the United States. New England Journal of Medicine, 348(26), 2635–2645. doi: 10.1056/NEJMsa022615
- Mudholkar, G. S. (1983). Fisher's Z-transformation. Encyclopedia of Statistical Sciences, 3, 130–135.
- Naikoba, S., & Hayward, A. (2001). The effectiveness of interventions aimed at increasing handwashing in healthcare workers-a systematic review. Journal of Hospital Infection, 47(3), 173–180. doi: 10.1053/jhin.2000.0882
- National Heart, Lung, and Blood Institute. (2016). Quality assessment tool for observational cohort and cross-sectional studies. Retrieved from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Nilsen, P., Roback, K., Broström, A., & Ellström, P.-E. (2012). Creatures of habit: Accounting for the role of habit in implementation research on clinical behaviour change. Implementation Science, 7(1), 53. doi: 10.1186/1748-5908-7-53
- Ouellette, J. A., & Wood, W. (1998). Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin, 124(1), 54. doi: 10.1037/0033-2909.124.1.54
- Paulhus, D. L. (1986). Self-deception and impression management in test responses. In A. Angleitner & J. S. Wiggins (Eds.), Personality assessment via questionnaires (pp. 143–165). Heidelberg: Springer.
- Pearson, E. S. (1929). Some notes on sampling tests with two variables. Biometrika, 21, 337–360.
- Potthoff, S., Presseau, J., Sniehotta, F. F., Elovainio, M., & Avery, L. (2017). Planning to be routine: Habit as a mediator of the planning-behaviour relationship in healthcare professionals. Implementation Science, 12(24), doi: 10.1186/s13012-017-0551-6
- Potthoff, S., Rasul, O., Sniehotta, F. F., Marques, M., Beyer, F., Thomson, R., … Presseau, J. (2015). The relationship between habit and healthcare professional behaviour in clinical practice: A systematic review and meta-analysis. PROSPERO 2015 CRD42015020024. Retrieved from http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42015020024
- Presseau, J., Mackintosh, J., Hawthorne, G., Francis, J. J., Johnston, M., Grimshaw, J. M., Steen, N., Coulthard, T., Brown, H., Kaner, E. & Elovainio, M. (2018). Cluster randomised controlled trial of a theory-based multiple behaviour change intervention aimed at healthcare professionals to improve their management of type 2 diabetes in primary care. Implementation Science, 13(1), 65.
- Presseau, J., Johnston, M., Francis, J. J., Hrisos, S., Stamp, E., Steen, N., … Hunter, M. (2014). Theory-based predictors of multiple clinician behaviors in the management of diabetes. Journal of Behavioral Medicine, 37(4), 607–620. doi: 10.1007/s10865-013-9513-x
- Presseau, J., Johnston, M., Heponiemi, T., Elovainio, M., Francis, J. J., Eccles, M. P., … Sniehotta, F. F. (2014). Reflective and automatic processes in health care professional behaviour: A dual process model tested across multiple behaviours. Annals of Behavioral Medicine, 48(3), 347–358. doi: 10.1007/s12160-014-9609-8
- Reyna, V. F. (2008). A theory of medical decision making and health: Fuzzy trace theory. Medical Decision Making, 28(6), 850–865. doi: 10.1177/0272989X08327066
- Røttingen, J.-A., Regmi, S., Eide, M., Young, A. J., Viergever, R. F., Årdal, C., … Terry, R. F. (2013). Mapping of available health research and development data: What's there, what's missing, and what role is there for a global observatory? The Lancet, 382(9900), 1286–1307. doi: 10.1016/S0140-6736(13)61046-6
- Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68. doi: 10.1037110003-066X.55.1.68
- Sheeran, P. L., Gollwitzer, P. M., & Bargh, J. A. (2013). Acknowledges the role of unconscious processes in health psychology. Health Psychology, 32(5), 460–473. doi: 10.1037/a0029203
- Skinner, B. F. (1953). Science and human behavior. New York: Macmillan.
- Sladek, R. M., Phillips, P. A., & Bond, M. J. (2006). Implementation science: A role for parallel dual processing models of reasoning? Implementation Science, 1, 12. doi: 10.1186/1748-5908-1-12
- Sniehotta, F. F., & Presseau, J. (2012). The habitual use of the self-report habit index. Annals of Behavioral Medicine, 43(1), 139–140. doi: 10.1007/s12160-011-9305-x
- Sniehotta, F. F., Scholz, U., & Schwarzer, R. (2005). Bridging the intention–behaviour gap: Planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychology & Health, 20(2), 143–160. doi: 10.1080/08870440512331317670
- Sniehotta, F. F., Scholz, U., & Schwarzer, R. (2006). Action plans and coping plans for physical exercise: A longitudinal intervention study in cardiac rehabilitation. British Journal of Health Psychology, 11(1), 23–37. doi: 10.1348/135910705X43804
- Sterne, J. A. C., & Egger, M. (2001). Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. Journal of Clinical Epidemiology, 54(10), 1046–1055. doi: 10.1016/S0895-4356(01)00377-8
- Triandis, H. C. (1977). Interpersonal behavior. Monterey: Brooks/Cole.
- Tversky, A., & Kahneman, D. (1973). Availability: A heuristic for judging frequency and probability. Cognitive Psychology, 5(2), 207–232. doi: 10.1016/0010-0285(73)90033-9
- Verplanken, B., & Orbell, S. (2003). Reflections on past behavior: A self-report index of habit strength. Journal of Applied Social Psychology, 33(6), 1313–1330. doi: 10.1111/j.1559-1816.2003.tb01951.x
- Walker, A. E., Grimshaw, J., Johnston, M., Pitts, N., Steen, N., & Eccles, M. (2003). PRIME–Process modelling in ImpleMEntation research: Selecting a theoretical basis for interventions to change clinical practice. BMC Health Services Research, 3(1), 22. doi: 10.1186/1472-6963-3-22
- Wood, W., Quinn, J. M., & Kashy, D. A. (2002). Habits in everyday life: Thought, emotion, and action. Journal of Personality and Social Psychology, 83(6), 1281–1297. doi: 10.1037//0022-3514.83.6.1281
- Woolf, S. H. (2008). The meaning of translational research and why it matters. JAMA, 299(2), 211–213. doi: 10.1001/jama.2007.26