ABSTRACT
Background: Psychological interventions for managing emotional distress in neurodegenerative diseases are needed, but progressive worsening of symptoms and increasing disability might pose difficulties with engagement. We aimed to synthesise the experiences of engaging with and using psychological interventions in neurodegenerative diseases and identify relevant barriers and facilitators. Methods: Systematic searches were conducted in six electronic databases and results were screened. We included qualitative and mixed methods studies reporting patient or caregivers’ views or experiences of psychological interventions. Qualitative data were extracted and thematically synthesised. Results: 34 papers were included, covering a range of diseases and interventions. Engagement was facilitated by flexible intervention formats and tailoring to the specific needs of people with neurodegenerative diseases. Interventions were sometimes inaccessible or burdensome because of physical and cognitive symptoms, and the time and effort required for the intervention. Participants’ levels of acceptance and readiness often differed and influenced engagement with the intervention. Across different interventions, participants experienced wide-ranging benefits including changes in insight, perspective, self-efficacy, emotions and relationships. Conclusion: Although people with neurodegenerative diseases and caregivers experience benefits from psychological interventions, burden-reducing adaptations and sensitive tailoring to the specific disease context is required to improve acceptability and engagement.
Introduction
Neurodegenerative disease is an umbrella term for diseases that are characterised by progressive degeneration of the structure and function of the nervous system. Common neurodegenerative diseases include Alzheimer’s disease, Parkinson’s disease, Motor Neurone Disease/Amyotrophic Lateral Sclerosis (MND/ALS) and Huntington’s disease. Each of these diseases manifest and progress differently. However, all neurodegenerative diseases have some common features – they are progressive, disabling, and are a major threat to survival (Cummings & Pillai, Citation2016). The psychological impact can also be similar across the diseases because of certain common changes (e.g., decreasing functional status, changes in social roles and experiencing multiple losses as the disease gets worse) (Ovaska-Stafford et al., Citation2021). People with neurodegenerative diseases experience significant psychological distress including anxiety and depression (Dale & van Duijn, Citation2015; Kurt et al., Citation2007; Reijnders et al., Citation2008; Thompson et al., Citation2012). Caregivers also experience burden, depression and anxiety (Aoun et al., Citation2013; Iavarone et al., Citation2014; Martínez-Martín et al., Citation2007) which is sometimes related to the disease severity and neuropsychiatric symptoms experienced by the person with the neurodegenerative condition (Allegri et al., Citation2006; Martínez-Martín et al., Citation2007; Schrag et al., Citation2006; Tramonti et al., Citation2019). Psychological distress can occur early or late in the disease trajectory and can have a negative impact on the quality of life for both people with neurodegenerative diseases and caregivers (Baquero & Martín, Citation2015; Fischer et al., Citation2012).
Psychological interventions have the potential to help people with neurodegenerative diseases and caregivers reduce psychological distress and have a better quality of life. The evidence for the effectiveness of psychological interventions is mixed, especially across different neurodegenerative diseases. For example, there is some evidence to suggest that psychological interventions are effective for improving psychological well-being in Parkinson’s disease and dementia (Orgeta et al., Citation2015; Zarotti, Eccles, et al., Citation2020). In other neurodegenerative diseases (e.g., MND/ALS and Huntington’s Disease) the literature is sparse and the need for more research on interventions has been emphasised (Gould et al., Citation2015; Thomas et al., Citation2006; Zarotti, Dale, et al., Citation2020; Zarotti, Mayberry, et al., Citation2020). For caregiver interventions, there is more evidence for the effectiveness of psychological interventions for caregivers of people with dementia (Cheng et al., Citation2019; Liu et al., Citation2017; Selwood et al., Citation2007). In other diseases like Parkinson’s disease, Huntington’s disease and MND/ALS, there has been less research on interventions for caregivers’ psychological support (Harris et al., Citation2018; Hempel et al., Citation2008). Psychological interventions may be of benefit for people with neurodegenerative diseases and caregivers, but currently evidence is limited or inconclusive.
Researchers and clinicians have identified specific barriers that can affect how patients and caregivers with neurodegenerative diseases might engage with psychological interventions. Approaches like Cognitive Behavioural Therapy (CBT) could be challenging because the progression of physical symptoms is generally irreversible and some negative cognitions about the situation are realistic rather than distorted (Cole & Vaughan, Citation2005; Hind et al., Citation2010). Similarly, with caregivers, the seemingly unchangeable nature of their situation may make some CBT therapeutic goals difficult to achieve (Fowler et al., Citation2021). Approaches like Acceptance and Commitment Therapy (ACT) have been proposed as more suitable and acceptable as they focus on accepting distress and finding new ways to carry out valued activities (Fowler et al., Citation2021; Graham et al., Citation2015).
The level of physical disability and cognitive impairment with neurodegenerative diseases may also affect engagement with psychological interventions. Physical disability can make accessing mental health interventions difficult because of issues with transportation (Dobkin et al., Citation2013; Marconi et al., Citation2016). Additionally, cognitive impairment is typical in Alzheimer’s disease, but it can also present in Parkinson’s disease, multiple sclerosis (MS) and MND/ALS. Cognitive changes can affect how people engage with therapy and interventions (Cole & Vaughan, Citation2005; Weeks et al., Citation2019). Caregivers typically spend several hours a day assisting the person with the neurodegenerative disease or organising care and this can leave little time for other activities (Galvin et al., Citation2018; Zhang et al., Citation2018).
Given ongoing uncertainty about the effectiveness of psychological approaches in many neurodegenerative conditions and the likelihood of significant health-related barriers to engagement, being open to understanding how people experience these interventions is vital. Qualitative research allows for the patient and caregivers’ perspectives to be prioritised and explored in-depth and detail. Whilst qualitative studies of patient and caregivers’ experiences of various psychological interventions for a range of neurodegenerative diseases have been published, this literature has not yet been synthesised. We, therefore, aimed to synthesise and review findings from qualitative research in order to obtain a detailed and comprehensive understanding of engagement and acceptability, identifying issues that are relevant to patients and caregivers with a range of neurodegenerative conditions, therapeutic approaches and delivery modes. Bringing together these findings will offer important insights to guide those involved in planning, delivering and evaluating interventions for patients with neurodegenerative diseases and their caregivers and help drive the development of more acceptable, engaging and effective interventions.
Methods
We conducted a systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Sohrabi et al., Citation2021) and analysed data using a thematic synthesis (Thomas & Harden, Citation2008). The protocol was prospectively registered on PROPSPERO (CRD42021223125). We followed the ENTREQ (enhanced transparency in reporting the synthesis of qualitative research) checklist to facilitate systematic reporting (Tong et al., Citation2012).
Search strategy
A systematic search was carried out in six electronic databases (MEDLINE, PsycINFO, CINAHL Plus, Web of Science, AMED and the Cochrane library). The searches were conducted in October 2020 and updated in October 2021. Search terms were developed from initial literature scoping, consultation with a specialist librarian, and were piloted to ensure relevant studies were being included. The search strategy combined terms relating to psychological interventions, neurodegenerative diseases, and qualitative or mixed methods research (see supplementary file 1 for search terms). Grey literature was also searched (OpenGrey and ProQuest), and references of included studies were hand-searched. No date limits were applied, and results were restricted to those published in English.
Inclusion and exclusion criteria
The detailed inclusion and exclusion criteria are shown in . We sought to identify qualitative and mixed methods studies that had a substantial qualitative component that investigated patient and caregivers’ experiences and views of using psychological interventions. We included neurodegenerative diseases such as Alzheimer’s disease, Huntington’s disease, Parkinson’s disease, Motor neurone disease/Amyotrophic Lateral Sclerosis (MND/ALS), Multiple system atrophy, and multiple sclerosis (MS). We defined psychological interventions as interventions that had psychotherapeutic or psychoeducational content and where the focus/aim was to reduce emotional distress or improve wellbeing or coping skills.
Table 1. Review inclusion and exclusion criteria.
Screening and selection
The search results were exported to EndNote and duplicates were removed. All titles and abstracts were screened for eligibility by one author (CP). 15% were screened independently by a second reviewer (CM) and discrepancies were resolved through discussion and consensus. All full-text screening was conducted by CP and CM independently, any conflicts were resolved through discussion, involving a third reviewer (LD) where necessary.
Data extraction and quality appraisal
The data was extracted into a table and included data about study characteristics, participants and the interventions. All qualitative data (participant quotes and interpretations of findings) from the results and discussion sections were imported to NVivo for analysis and synthesis.
All included studies were assessed for quality using the Critical Appraisal Skills Programme (CASP) qualitative research checklist (Campbell et al., Citation2012; Mays & Pope, Citation2000). The CASP is a well-recognised checklist for assessing quality in qualitative studies and has been previously used to assess qualitative studies which seek to understand experiences of interventions in other disease groups (Cox et al., Citation2017; Maund et al., Citation2019). Details of the quality assessment for each included study can be found in Supplementary file 2. We did not exclude low-quality studies but took quality ratings into account when describing and interpreting the confidence in the findings.
Analysis and synthesis
Data were analysed using a thematic synthesis (Thomas & Harden, Citation2008). We selected this method because it allowed us to stay close to the original context of the primary studies, and draw conclusions about participants’ experiences across a heterogeneous group of neurodegenerative diseases and intervention types through developing analytic themes which go beyond the interpretations presented in the primary studies. Extracted data was managed and coded using NVivo software. An inductive line-by-line coding of the data was carried out for each primary study. The list of ‘free’ codes for each study was then systematically compared, similar codes were combined and grouped into descriptive themes, paying attention to and recording whether the theme was represented in interventions with patients, caregivers or both groups. The wider review team then discussed the descriptive themes in relation to the review question. The descriptive themes were compared with each other and diagrams were used to identify specific issues with engagement and acceptability. Abstract or analytic themes that went beyond the content of original studies were developed, the descriptive themes were examined in light of these analytic themes, and changes to the analytic themes were made iteratively. This process was repeated until the analytic themes sufficiently captured the descriptive themes and answered the review question. The analytic themes were further refined during the process of writing up the results.
We used the GRADE CERQual approach (Lewin et al., Citation2018) as a systematic and transparent way to evaluate confidence in our principal review findings (i.e., our analytic themes). GRADE CERQual considers four components: methodological limitations, coherence, adequacy of data and relevance; ratings were assigned through discussions between CP and LD.
Results
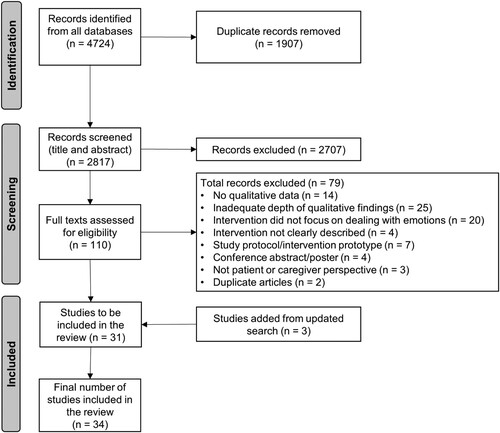
shows the studies identified and included and excluded at different stages of the screening and selection process. Thirty-four papers met the inclusion criteria and were included in the review. The different neurodegenerative diseases included were dementia (n = 19), MS (n = 9), Parkinson’s disease (n = 3), MND/ALS (n = 2) and Huntington’s disease (n = 1). Thirteen papers included people with neurodegenerative diseases as participants, 14 included caregivers as participants and 7 papers included both people with neurodegenerative diseases and caregivers together. The different types of interventions covered were mindfulness (n = 15), ACT (n = 6), multicomponent psychoeducational interventions (n = 6), CBT (n = 5), dignity therapy (n = 1) and compassion-focussed therapy (n = 1). Further details about the included papers can be found in .
Table 2. Summary table of included studies.
Assessment of quality and confidence in review findings
Individual study quality ratings can be found in Supplementary file 2. Overall, studies were of high quality, with papers scoring 7 or higher on a scale from 1 to 10 on the CASP checklist. Studies tended to be weaker on reporting the relationship between researchers and participants, and reporting data analysis methods sufficiently. Included studies scored well on clearly stating the aims of the research and appropriate use of qualitative methodology.
The GRADE CERQual evaluation found that in addition to the included studies being of high quality, a large number of studies contributed to the development of each analytic theme, the studies had rich data, and the themes were relevant across different diseases and intervention types (see Supplementary file 3). The evaluation process, therefore, concluded that there was high confidence in three analytic themes and moderate confidence in one analytic theme. Overall, we are confident that the review findings are a reasonable representation of the experiences of psychological interventions among people with neurodegenerative diseases and caregivers.
Themes
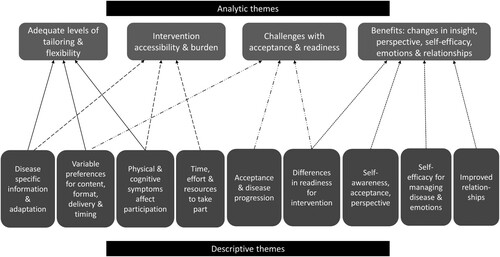
We developed four analytic themes; outlines the descriptive and analytic themes and the relationship between them. These themes were common for people with neurodegenerative diseases and caregivers. Where specific differences occur between these two participant groups, they are discussed within each theme.
Adequate levels of tailoring and flexibility
Engagement with psychological interventions was either facilitated or hindered by adequate intervention tailoring and flexibility. Disease-specific tailoring was often used to adapt the intervention content and activities to the specific disease or the specific needs of caregivers. People with neurodegenerative diseases and caregivers found disease-specific information and advice helpful (Adams, Citation2018; Bogosian et al., Citation2021; de Wit et al., Citation2019; Dennison et al., Citation2013; Eccles et al., Citation2020; Gottberg et al., Citation2016; Hind et al., Citation2010; Kazmer et al., Citation2018; Nehrig, Shifrin, et al., Citation2019; Simpson et al., Citation2018; Simpson et al., Citation2019) and discussed the importance of therapists or facilitators having disease-specific knowledge (Craig et al., Citation2018; de Wit et al., Citation2019; Dennison et al., Citation2013; Gottberg et al., Citation2016; Kazmer et al., Citation2018; Martin et al., Citation2015; Simpson et al., Citation2019). Caregivers also appreciated interventions that were targeted to their own unique needs and difficulties (de Wit et al., Citation2019; Larochette et al., Citation2020; Nehrig, Shifrin, et al., Citation2019) and appreciated the ability to choose intervention modules that were relevant to their situation (de Wit et al., Citation2019; Larochette et al., Citation2020).
I don’t think you can have mixed abilities walking round and everybody happy … I just felt the delivery needed to be a bit more sensitive to the needs of people with MS and MS is very different from chronic fatigue or any other thing like that.. it might have been better to have somebody who has actually been ill or not been well to have an input into the delivery on the course. [person with MS, mindfulness intervention (Simpson et al., Citation2019)]
Similarly, intervention formats and delivery methods need to be flexible to accommodate people with different symptoms and needs or levels of ability. This could be through ensuring flexibility in intervention duration. Some participants preferred shorter intervention durations (Berk et al., Citation2019; Giovannetti et al., Citation2020; Simpson et al., Citation2018; Simpson et al., Citation2019), whereas others wanted more time to enable learning, practising and group work (Berk et al., Citation2019; Bogosian et al., Citation2016; Bogosian et al., Citation2021; Craig et al., Citation2018; de Wit et al., Citation2019; Dennison et al., Citation2013; Eccles et al., Citation2020; Giovannetti et al., Citation2020; Larochette et al., Citation2020; Martin et al., Citation2015; Nehrig & Chen, Citation2019; Nehrig, Gillooly, et al., Citation2019; Nehrig, Shifrin, et al., Citation2019; Pegler, Citation2017; Potter et al., Citation2021; Sessanna et al., Citation2021; Simpson et al., Citation2018; Simpson et al., Citation2019; Tahsin et al., Citation2021). Interventions also require some flexibility in terms of mode of delivery. Face-to-face options were valued because of the bond and rapport created between participants or between participants and therapists which made it easier to talk about difficult issues (de Wit et al., Citation2019; Dennison et al., Citation2013; Gottberg et al., Citation2016; Potter et al., Citation2021; Sessanna et al., Citation2021). However, face-to-face sessions were difficult if people had problems with mobility, transportation or had other conflicting commitments (Berk et al., Citation2019; Eccles et al., Citation2020; Gottberg et al., Citation2016; Marconi et al., Citation2016; Simpson et al., Citation2018). Accessing the intervention remotely (online or by telephone/at home) was convenient, easy to use, and could be completed at the individual’s own pace (Bogosian et al., Citation2021; de Wit et al., Citation2019; Dennison et al., Citation2013; Hind et al., Citation2010; Johnston et al., Citation2016; Sessanna et al., Citation2021) but difficulties with concentration, technology and the lack of human interaction could make engagement challenging (de Wit et al., Citation2019; Dennison et al., Citation2013; Hind et al., Citation2010; Sessanna et al., Citation2021).
With MS you can become very isolated because of your disability … So, I think when working with something that is a computer programme it makes you feel even more like you’re not speaking to someone face to face. You don’t get the empathy there. [person with MS, computerised CBT (Hind et al., Citation2010)]
I think the program came at a good time. That everything is still relatively new for you, and can put your own things into perspective and that you receive support. Otherwise, you will keep going in circles for too long. [caregiver for person with MND/ALS, ACT intervention (de Wit et al., Citation2019)]
Intervention accessibility and burden
Some psychological interventions or some components of the intervention were experienced as inaccessible or burdensome, and this could act as a barrier to engaging with the intervention. People with neurodegenerative diseases found it difficult to take part in and complete intervention activities because of physical and cognitive symptoms (Adams, Citation2018; Berk et al., Citation2019; Craig et al., Citation2018; Marconi et al., Citation2016; Martin et al., Citation2015; Sessanna et al., Citation2021; Swannell, Citation2017). Difficulties with cognition (in particular, concentration or memory difficulties) impacted their ability to sustain attention during the intervention, learn and practice new techniques/strategies (Adams, Citation2018; Berk et al., Citation2019; Craig et al., Citation2018; Douglas et al., Citation2021; Hind et al., Citation2010; Marconi et al., Citation2016; Martin et al., Citation2015; Swannell, Citation2017). Cognitive difficulties also made information processing difficult if information is too much or too technical (Adams, Citation2018; Berk et al., Citation2019; Martin et al., Citation2015); therefore, having adequate time and clear instructions when learning new activities was important (Douglas et al., Citation2021; Martin et al., Citation2015; Sessanna et al., Citation2021).
Participants discussed the impact cognitive decline had on being able to practice MBSR (Mindfulness-based stress reduction). This varied from remembering to practice, to being unable to hold on to, or understand, the concept of mindfulness. Some participants felt it improved their concentration, while others felt it was not beneficial for people with dementia. [study author, dementia, mindfulness intervention, (Swannell, Citation2017)]
My brain just couldn’t cope with it because it was so busy just trying not to fall over … and of course sometimes there’s no feeling in your feet … so no, that was very challenging. [person with MS, mindfulness intervention, (Simpson et al., Citation2018)]
The participants became aware that CBT is essentially a continuous process, with no pause between the sessions, but they also became aware that they did not always have enough time and energy in their everyday lives to focus on changing themselves. [study author, MS, CBT intervention, (Gottberg et al., Citation2016)]
Participants requested further flexibility to adapt the spacing of the reading they had to complete each week to maximise their ability to engage with the text in the light of their caring responsibilities, which sometimes changed dramatically week to week. [study author, MS, ACT intervention, (Potter et al., Citation2021)]
Challenges with acceptance and readiness
With neurodegenerative diseases, acceptance of the diagnosis and progressive symptoms can happen gradually and at different stages, and this influences how willing and how well participants can engage with interventions. Participants described how accepting the diagnosis and thinking about the future and symptom progression is difficult and anxiety provoking (Bogosian et al., Citation2016; de Wit et al., Citation2019; Douglas et al., Citation2021; Fitzpatrick et al., Citation2010; Gottberg et al., Citation2016; Johannessen et al., Citation2015; Johnston et al., Citation2016; Larochette et al., Citation2020; Nehrig, Gillooly, et al., Citation2019; Nehrig, Shifrin, et al., Citation2019; Vandenberg et al., Citation2019). Intervention activities that triggered thoughts about the future and progression could also be challenging. For example, participants reported being anxious about meeting people with the same condition or finding out about other people’s experiences, as this may show them what might happen to them in the future (Berk et al., Citation2019; Bogosian et al., Citation2016; de Wit et al., Citation2019; Eccles et al., Citation2020; Fitzpatrick et al., Citation2010; Giovannetti et al., Citation2020; Simpson et al., Citation2018).
Everybody seemed to be worse than me and I thought ‘I don’t think this is going to work for me’ I’ve said before, ‘if I don’t see it I haven’t got it’. There was one lady who said ‘come and join us at the Parkinson’s society’ and I thought ‘I’m not ready for that’. [person with Parkinson’s disease, mindfulness intervention, (Fitzpatrick et al., Citation2010)]
The ‘memory box’ activity, which was demonstrated by the course champion, was something some participants already did. Others felt worried this was linked to thinking about death. The tutors reemphasized that the focus of the activity was on having a place where photographs or items relating to happy memories are kept and used as a resource to enjoy. Additionally, the activities around increasing happiness and sharing successes were seen positively as they both drew attention to previous achievements and current strengths. [study author, dementia, psychoeducation intervention, (Martin et al., Citation2015)]
Those 6 weeks, they really helped to sort things out again. But you gradually notice that you start to forget things. Things change so much with ALS. When I look at how I experienced it in the beginning and in the final phase, it is so different. So I would like to give it as advice to offer the program several times. It simply helps you to make conscious choices. [caregiver for person with MND, ACT intervention, (de Wit et al., Citation2019)]
One factor that appeared to influence whether a participant benefited from and was satisfied with their therapy experience was the degree to which they related to and engaged with the approach. Participants’ identified this as ‘buying into’ therapy and described being open-minded, willing to open up to the therapist and give the approach a fair chance as important. [study author, MS, CBT intervention, (Dennison et al., Citation2013)]
Benefits: changes in insight, perspective, self-efficacy, emotions and relationships
People with neurodegenerative diseases and caregivers reported a number of benefits from psychological interventions. The interventions helped participants become more open and accepting of the impact of the disease (Adams, Citation2018; Berk et al., Citation2019; Bogosian et al., Citation2016; Bogosian et al., Citation2021; Craig et al., Citation2018; de Wit et al., Citation2019; Dennison et al., Citation2013; Douglas et al., Citation2021; Fitzpatrick et al., Citation2010; Giovannetti et al., Citation2020; Gottberg et al., Citation2016; Hoppes et al., Citation2012; Johannessen et al., Citation2015; Kazmer et al., Citation2018; Larochette et al., Citation2020; Lavoie et al., Citation2005; Nehrig, Shifrin, et al., Citation2019; Pegler, Citation2017; Simpson et al., Citation2018; Simpson et al., Citation2019; Swannell, Citation2017; Vandenberg et al., Citation2019). They were more self-aware, particularly of their thoughts and how this impacted their feelings and responses to situations (Berk et al., Citation2019; Bogosian et al., Citation2016; Dennison et al., Citation2013; Douglas et al., Citation2021; Eccles et al., Citation2020; Fitzpatrick et al., Citation2010; Giovannetti et al., Citation2020; Gottberg et al., Citation2016; Han et al., Citation2021; Swannell, Citation2017; Vandenberg et al., Citation2019). This awareness or insight was key to changing their perspective on the disease and their situation. They thought about their disease or situation differently, and considered other perspectives (Adams, Citation2018; Bogosian et al., Citation2016; Bogosian et al., Citation2021; de Wit et al., Citation2019; Dennison et al., Citation2013; Giovannetti et al., Citation2020; Gottberg et al., Citation2016; Hoppes et al., Citation2012; Johnston et al., Citation2016; Larochette et al., Citation2020; Marconi et al., Citation2016; Nehrig, Gillooly, et al., Citation2019; Nehrig, Shifrin, et al., Citation2019; Vandenberg et al., Citation2019). This perspective-taking was an important part of coping especially when there was no cure or treatment. Participants developed a more self-compassionate and positive approach to coping with neurodegenerative diseases. They placed more value on themselves and carved time out for self-care, (Berk et al., Citation2019; Bogosian et al., Citation2016; Craig et al., Citation2018; de Wit et al., Citation2019; Dennison et al., Citation2013; Douglas et al., Citation2021; Giovannetti et al., Citation2020; Glueckauf et al., Citation2012; Han et al., Citation2021; Kazmer et al., Citation2018; Larochette et al., Citation2020; Lavoie et al., Citation2005; Nehrig, Gillooly, et al., Citation2019; Nehrig, Shifrin, et al., Citation2019; Pegler, Citation2017) were less critical or kinder to themselves, (Adams, Citation2018; Craig et al., Citation2018; Dennison et al., Citation2013; Douglas et al., Citation2021; Han et al., Citation2021; Simpson et al., Citation2018; Simpson et al., Citation2019; Swannell, Citation2017) and focused on the things they could still do, appreciated things more, and overall developed a more positive outlook (Bogosian et al., Citation2016; Dennison et al., Citation2013; Douglas et al., Citation2021; Hoppes et al., Citation2012; Martin et al., Citation2015; Pegler, Citation2017; Sessanna et al., Citation2021; Simpson et al., Citation2018).
Yes, I’d say I’m more at ease with my situation. I can accept things more the way they are and think it’s OK. [person with MS, CBT intervention, (Gottberg et al., Citation2016)]
I think I remind myself now … that I'm actually doing a good job. Looking after my mum and everything else I'm dealing with … and sometimes I forget and I take a step back and I think “damn, you've been through a lot.” So cut yourself some slack … [caregiver for person with dementia, compassion-focused therapy, (Craig et al., Citation2018)]
Through learning to be mindful, participants gained freedom to choose how they wished to respond to situations. This choice was empowering as people gained control over themselves and their responses. [study author, MS, mindfulness intervention, (Bogosian et al., Citation2016)]
The findings show that the intervention contributed to making the caregivers feeling safer, giving them a better understanding of the disorder. Also, the intervention helped them to be more open about their situation and more prepared for the future. [study author, dementia, psychoeducation intervention, (Johannessen et al., Citation2015)]
Some reported an improvement in their relationships, where there was more understanding between the person with the neurodegenerative condition and family, (de Wit et al., Citation2019; Douglas et al., Citation2021; Hoppes et al., Citation2012; Kazmer et al., Citation2018; Larochette et al., Citation2020; Nehrig, Shifrin, et al., Citation2019; Vandenberg et al., Citation2019) less conflict, (Berk et al., Citation2019; Giovannetti et al., Citation2020; Han et al., Citation2021; Hoppes et al., Citation2012; Kazmer et al., Citation2018; Larochette et al., Citation2020; Lavoie et al., Citation2005; Nehrig, Gillooly, et al., Citation2019; Nehrig, Shifrin, et al., Citation2019; Pegler, Citation2017; Simpson et al., Citation2018) less isolation, (Berk et al., Citation2019; Douglas et al., Citation2021; Swannell, Citation2017) more connection and communication, (Adams, Citation2018; Berk et al., Citation2019; Craig et al., Citation2018; Larochette et al., Citation2020; Lavoie et al., Citation2005; Marconi et al., Citation2016; Swannell, Citation2017) more openness, (Bogosian et al., Citation2021; de Wit et al., Citation2019; Giovannetti et al., Citation2020; Sessanna et al., Citation2021; Vandenberg et al., Citation2019) and overall better interactions with others (Berk et al., Citation2019; Giovannetti et al., Citation2020; Hoppes et al., Citation2012; Simpson et al., Citation2018; Vandenberg et al., Citation2019). Participants felt more confident with social interactions, and did not avoid social situations (Dennison et al., Citation2013; Fitzpatrick et al., Citation2010; Giovannetti et al., Citation2020; Johannessen et al., Citation2015; Vandenberg et al., Citation2019).
Some participants reported that the training had influenced their relationship as a couple. Caregivers were better able to prevent or deal with quarrels. They felt more connected. [study author, dementia, mindfulness intervention, (Berk et al., Citation2019)]
A minority of participants reported little or no change from therapy. This tended to be more common for the SL (supportive listening – control group) participants and those who disagreed with the logic of their intervention. Other participants felt that they were already coping very well with MS, and so found they had little to gain from therapy. [study author, MS, CBT intervention, (Dennison et al., Citation2013)]
Discussion
We synthesised the experiences of people with neurodegenerative diseases and caregivers and identified barriers and facilitators that are relevant to engagement and acceptability of psychological interventions. Many participants valued the post-intervention changes in insight, perspective, self-efficacy, emotions and relationships. However, important things to consider include adequate levels of intervention tailoring and flexibility, intervention accessibility and burden, and challenges with acceptance and readiness among participants. The four themes presented in this review need to be considered in conjunction when developing or evaluating interventions, as they can interact with each other. For example, adequate tailoring might help reduce intervention burden; insight and perspective may be valued outcomes but may depend on acceptance or readiness from participants; or accessibility can be improved with dedicated tailoring strategies. summarises key considerations when developing engaging and acceptable interventions for people with neurodegenerative diseases and caregivers based on the findings from our review.
Table 3. Key considerations when developing psychological interventions for people with neurodegenerative diseases and caregivers.
With neurodegenerative diseases, it is important to tailor intervention content to the specific disease and adapt activities or advice so that people with various physical and cognitive symptoms can participate and feel that the intervention is designed for the problems and context they are facing. Disease-specific therapy manuals have been developed and used to improve psychological outcomes for patients and caregivers in some neurodegenerative diseases like Parkinson’s disease, dementia, and MS (Chan et al., Citation2017; Dobkin et al., Citation2007; Moss-Morris et al., Citation2013). However, psychological support interventions need to move beyond a one-size-fits-all approach for specific disorders and personalise interventions based on individual and contextual factors (Purgato et al., Citation2021). Our findings show that additional tailoring and flexibility is required with interventions for neurodegenerative diseases because of the variability in symptoms, disease stages, coping preferences, and preferences for therapy. Individual differences in terms of levels of acceptance and readiness are also important considerations, particularly with neurodegenerative conditions, where thinking about disease progression can be distressing (Moss-Morris et al., Citation2013). People with neurodegenerative diseases can experience rapid changes in their medical and psychological condition, and therefore their needs within different phases in psychological interventions may also change. Although this level of personalisation of interventions is important, it may also be challenging to execute in very structured, manualised therapies or in interventions that are conducted in a group setting, compared to one-to-one interventions facilitated by trained professionals. Our review also found very few interventions that offered individuals a choice regarding the type of therapy and therapeutic activities. Having options for different kinds of psychological support could be a way forward to further personalise interventions by allowing people to choose content and activities that match their needs and preferences.
Recent reviews of the effectiveness of psychological interventions for wellbeing in neurodegenerative diseases noted that so far there is more evidence for certain therapeutic approaches (e.g., CBT and mindfulness) and less research on other therapeutic approaches (Zarotti, Eccles, et al., Citation2020; Zarotti, Mayberry, et al., Citation2020). Our current synthesis of intervention experiences mirrors the types of interventions covered in these reviews with mindfulness-based interventions being most common. Noteworthy in our review is the use of therapeutic approaches that originate from clinical psychology, and few studies that use health psychology theory and frameworks. Health psychology approaches often have a focus on beliefs about the disease or symptoms, and cognitive and behavioural strategies in relation to illness-related threats (e.g., Leventhal’s common-sense model of self-regulation or Moss-Morris’ model of adjustment to chronic illness) (Leventhal et al., Citation1998; Moss-Morris, Citation2013). Our review showed that some beliefs about the illness, particularly how people thought about future disease progression and the level of acceptance of the impact of the illness on their life can also play a role in how people engage with interventions. Integrating theoretical frameworks from health psychology and psychological therapy models can potentially improve engagement and make intervention programmes more effective (Karekla et al., Citation2019).
There also needs to be greater flexibility with how psychological interventions are delivered for people with neurodegenerative diseases and caregivers. Therapists working with long-term conditions have expressed a need for a model of therapy that has greater flexibility in terms of session frequency, attendance policies, mode of delivery, and session location because of issues with mobility, unpredictable symptoms, time involved and fatigue (Carroll et al., Citation2021). Additionally, physical and cognitive symptoms can make engaging with therapy difficult or burdensome for people with neurodegenerative diseases (Dennison & Moss-Morris, Citation2010; Dobkin et al., Citation2013; Van Groenestijn et al., Citation2015). With psychological interventions, the structure and timing of sessions, and aspects such as homework can act as barriers to starting or continuing therapy (Barnes et al., Citation2013; Rice et al., Citation2020). Being flexible with the structure of psychological services or providing necessary resources/support can help reduce this treatment burden (May et al., Citation2014; Rice et al., Citation2020). Carefully considering a biopsychosocial framework when developing interventions (biological aspects – e.g., changes in symptoms, psychological aspects – e.g., level of acceptance, social aspects – e.g., support from services or family) could also guide interventions to be more flexible in terms of their delivery.
Based on our review findings, we have made some recommendations for future research. Going forward researchers need to focus on issues with engagement and acceptability when developing interventions for people with neurodegenerative diseases and caregivers. User needs should be evaluated using qualitative methods by adopting a more user-centred or co-production approach. There is a gap in our understanding of how engagement differs with different types of psychological interventions and with different methods of intervention delivery, and how different levels of engagement can impact outcomes. This needs to be explored in future research. We also recommend more detailed and consistent reporting of intervention development, content, and delivery, including the steps taken to adapt or tailor the intervention to specific populations as this can impact the acceptability and engagement with the intervention. Our review highlighted the range of benefits people with neurodegenerative diseases and caregivers experience from psychological interventions, which go beyond changes usually anticipated in trials such as improvements in mood or well-being. It would be useful to measure these broader changes (e.g., changes in self-awareness, thinking and attitudes, self-efficacy) quantitatively as outcomes of intervention trials (Berk et al., Citation2019; Eccles et al., Citation2020; Meek et al., Citation2021; Nehrig, Gillooly, et al., Citation2019; Tang & Chan, Citation2016) as well as undertake research to determine what outcomes are valued or appropriate to use as indicators of therapeutic success, especially in progressive diseases where symptoms will get worse with time.
Strengths and limitations
Analysing data from qualitative studies provided a unique insight into issues of acceptability and engagement, and we were able to identify common factors that impact acceptability and engagement across different neurodegenerative diseases. We also need to be conscious that these studies may represent experiences of those who have agreed to take part in a psychological intervention and agreed to give feedback. There may be other barriers or views among those who did not take part, or who dropped out or did not benefit from the intervention. It is not always easy to capture these perspectives through research studies, however, we need to be cognisant that the review findings may present a more optimistic view of participants’ experiences.
The majority of the interventions were mindfulness-based, conducted face-to-face and in a group setting. Some of the facilitators and barriers identified by this review may have been influenced by this. For example, difficulties with accessibility and burden may reflect the group and face-to-face format as well as the relatively longer duration of sessions. Additional research with other intervention types and formats may yield different insights into engagement issues. The majority of the studies included people/caregivers of people with dementia or MS and this may have influenced review findings. However, after assessing confidence in each of the review themes, we are confident that our findings did not come solely from particular diseases but were derived from experiences across the different neurodegenerative diseases.
Conclusion
We have identified specific barriers and facilitators to using psychological interventions with people with neurodegenerative diseases and their family/informal caregivers. It was important to tailor information and advice beyond the specific neurodegenerative disease and be flexible to participants’ needs and preferences. This was particularly important so that interventions were accessible to people with different physical and cognitive symptoms, and so that interventions were not experienced as burdensome. Different levels of acceptance and readiness can make intervention engagement and acceptability challenging and interventionists need to be sensitive to this and adapt the intervention or their approach accordingly. Once these factors are considered, individuals can experience wide-ranging benefits from psychological interventions including changes in insight, perspective, self-efficacy, emotions and relationships. It is useful to consider and measure the range of potential benefits from psychological interventions, especially with neurodegenerative diseases where physical deterioration and limited prognoses can make interpreting the outcomes of psychological interventions more challenging.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Cathryn Pinto
Cathryn Pinto designed the review protocol, conducted the searches, screened the search results for inclusion, extracted the data, conducted the quality assessment and GRADE CERQual assessment, carried out a thematic synthesis of the data, drafted the paper and has approved the final manuscript.
Adam W. A. Geraghty
Dr Adam W. A. Geraghty contributed to the design of the review, development of search strategy, and review methods, advised on the data extraction and quality assessment, contributed to the thematic synthesis and presentation of the results, and provided feedback and approved the final manuscript of the paper.
Charlotte McLoughlin
Charlotte McLoughlin undertook the title and abstract screening and full-text screening of the search results, and provided feedback and approved the final manuscript of the paper.
Francesco Pagnini
Dr Francesco Pagnini provided feedback on the results of the thematic synthesis, contributed to and approved the final manuscript of the paper.
Lucy Yardley
Prof Lucy Yardley advised on the design of the review, development of search strategy and review methods, and provided feedback and approved of the final manuscript of the paper.
Laura Dennison
Dr Laura Dennison contributed to the design of the review, development of search strategy and review methods, assisted with the screening of results and inclusion decisions, advised on the data extraction, quality assessment and GRADE CERQual assessment, contributed to the thematic synthesis and presentation of the results, and provided feedback and approved the final manuscript of the paper.
References
- Adams, J. (2018). Mindfulness and meditation interventions in dementia: Experiences, adaptations and effects of well-being (Doctoral dissertation). University of Hull.
- Allegri, R. F., Sarasola, D., Serrano, C. M., Taragano, F. E., Arizaga, R. L., Butman, J., & Loñ, L. (2006). Neuropsychiatric symptoms as a predictor of caregiver burden in Alzheimer’s disease. Neuropsychiatric Disease and Treatment, 2(1), 105.
- Aoun, S. M., Bentley, B., Funk, L., Toye, C., Grande, G., & Stajduhar, K. J. (2013). A 10-year literature review of family caregiving for motor neurone disease: Moving from caregiver burden studies to palliative care interventions. Palliative Medicine, 27(5), 437–446. https://doi.org/10.1177/0269216312455729
- Baquero, M., & Martín, N. (2015). Depressive symptoms in neurodegenerative diseases. World Journal of Clinical Cases, 3(8), 682. https://doi.org/10.12998/wjcc.v3.i8.682
- Barnes, M., Sherlock, S., Thomas, L., Kessler, D., Kuyken, W., Owen-Smith, A., Lewis, G., Wiles, N., & Turner, K. (2013). No pain, no gain: Depressed clients’ experiences of cognitive behavioural therapy. British Journal of Clinical Psychology, 52(4), 347–364. https://doi.org/10.1111/bjc.12021
- Berk, L., Warmenhoven, F., Stiekema, A. P., Van Oorsouw, K., Van Os, J., de Vugt, M., & Van Boxtel, M. (2019). Mindfulness-based intervention for people with dementia and their partners: Results of a mixed-methods study. Frontiers in Aging Neuroscience, 11(April 24), 92. https://doi.org/10.3389/fnagi.2019.00092
- Bogosian, A., Hughes, A., Norton, S., Silber, E., & Moss-Morris, R. (2016). Potential treatment mechanisms in a mindfulness-based intervention for people with progressive multiple sclerosis. British Journal of Health Psychology, 21(4), 859–880. https://doi.org/10.1111/bjhp.12201
- Bogosian, A., Hurt, C. S., Hindle, J. V., McCracken, L. M., Vasconcelos e Sa, D. A., Axell, S., Tapper, K., Stevens, J., Hirani, P. S., Salhab, M., & Ye, W. (2021). Acceptability and feasibility of a mindfulness intervention delivered via videoconferencing for people with Parkinson’s. Journal of Geriatric Psychiatry and Neurology, 35(1), 155–167. https://doi.org/10.1177/0891988720988901
- Campbell, R., Pound, P., Morgan, M., Daker-White, G., Britten, N., Pill, R., Yardley, L., Pope, C., & Donovan, J. (2012). Evaluating meta ethnography: Systematic analysis and synthesis of qualitative research. Health Technology Assessment, 15(43). https://doi.org/10.3310/hta15430
- Carroll, S., Moss-Morris, R., Hulme, K., & Hudson, J. (2021). Therapists’ perceptions of barriers and facilitators to uptake and engagement with therapy in long-term conditions. British Journal of Health Psychology, 26(2), 307–324. https://doi.org/10.1111/bjhp.12475
- Chan, J., Churcher Clarke, A., Royan, L., Stott, J., & Spector, A. (2017). A Mindfulness program manual for people with dementia. Behavior Modification, 41(6), 764–787. https://doi.org/10.1177/0145445517715872
- Cheng, S.-T., Au, A., Losada, A., Thompson, L. W., & Gallagher-Thompson, D. (2019). Psychological interventions for dementia caregivers: What we have achieved, what we have learned. Current Psychiatry Reports, 21(7), 1–12. https://doi.org/10.1007/s11920-019-1045-9
- Cole, K., & Vaughan, F. L. (2005). The feasibility of using cognitive behaviour therapy for depression associated with Parkinson's disease: A literature review. Parkinsonism & Related Disorders, 11(5), 269–276. https://doi.org/10.1016/j.parkreldis.2005.03.002
- Cox, A., Lucas, G., Marcu, A., Piano, M., Grosvenor, W., Mold, F., … Ream, E. (2017). Cancer survivors’ experience with telehealth: A systematic review and thematic synthesis. Journal of Medical Internet Research, 19(1), e11. https://doi.org/10.2196/jmir.6575
- Craig, C., Hiskey, S., Royan, L., Poz, R., & Spector, A. (2018). Compassion focused therapy for people with dementia: A feasibility study. International Journal of Geriatric Psychiatry, 33(12), 1727–1735. https://doi.org/10.1002/gps.4977
- Cummings, J. L., & Pillai, J. A. (2016). Neurodegenerative Diseases: Unifying Principles. Oxford University Press.
- Dale, M., & van Duijn, E. (2015). Anxiety in Huntington’s disease. The Journal of Neuropsychiatry and Clinical Neurosciences, 27(4), 262–271. https://doi.org/10.1176/appi.neuropsych.14100265
- de Wit, J., Vervoort, S. C., van Eerden, E., van den Berg, L. H., Visser-Meily, J. M., Beelen, A., & Schröder, C. D. (2019). User perspectives on a psychosocial blended support program for partners of patients with amyotrophic lateral sclerosis and progressive muscular atrophy: A qualitative study. BMC Psychology, 7(1), 1–13. https://doi.org/10.1186/s40359-019-0308-x
- Dennison, L., & Moss-Morris, R. (2010). Cognitive–behavioral therapy: What benefits can it offer people with multiple sclerosis? Expert Review of Neurotherapeutics, 10(9), 1383–1390. https://doi.org/10.1586/ern.10.111
- Dennison, L., Moss-Morris, R., Yardley, L., Kirby, S., & Chalder, T. (2013). Change and processes of change within interventions to promote adjustment to multiple sclerosis: Learning from patient experiences. Psychology & Health, 28(9), 973–992. https://doi.org/10.1080/08870446.2013.767904
- Dobkin, R. D., Allen, L. A., & Menza, M. (2007). Cognitive-behavioral therapy for depression in Parkinson's disease: A pilot study. Movement Disorders, 22(7), 946–952. https://doi.org/10.1002/mds.21455
- Dobkin, R. D., Rubino, J. T., Friedman, J., Allen, L. A., Gara, M. A., & Menza, M. (2013). Barriers to mental health care utilization in Parkinson’s disease. Journal of Geriatric Psychiatry and Neurology, 26(2), 105–116. https://doi.org/10.1177/0891988713481269
- Douglas, S., Stott, J., Spector, A., Brede, J., Hanratty, É, Charlesworth, G., Noone, D., Payne, J., Patel, M., & Aguirre, E. (2021). Mindfulness-based cognitive therapy for depression in people with dementia: A qualitative study on participant, carer and facilitator experiences. Dementia (Basel, Switzerland). https://doi.org/10.1177/14713012211046150
- Eccles, F. J., Craufurd, D., Smith, A., Davies, R., Glenny, K., Homberger, M., … Skitt, Z. (2020). A feasibility investigation of mindfulness-based cognitive therapy for people with Huntington’s disease. Pilot and Feasibility Studies, 6(1), 1–13. https://doi.org/10.1186/s40814-020-00631-z
- Fischer, C. E., Ismail, Z., & Schweizer, T. A. (2012). Impact of neuropsychiatric symptoms on caregiver burden in patients with Alzheimer’s disease. Neurodegenerative Disease Management, 2(3), 269–277. https://doi.org/10.2217/nmt.12.19
- Fitzpatrick, L., Simpson, J., & Smith, A. (2010). A qualitative analysis of mindfulness-based cognitive therapy (MBCT) in Parkinson's disease. Psychology and Psychotherapy: Theory, Research and Practice, 83(2), 179–192. https://doi.org/10.1348/147608309X471514
- Fowler, N. R., Judge, K. S., Lucas, K., Gowan, T., Stutz, P., Shan, M., … Johns, S. A. (2021). Feasibility and acceptability of an acceptance and commitment therapy intervention for caregivers of adults with Alzheimer’s disease and related dementias. BMC Geriatrics, 21(1), 1–10. https://doi.org/10.1186/s12877-021-02078-0
- Galvin, M., Carney, S., Corr, B., Mays, I., Pender, N., & Hardiman, O. (2018). Needs of informal caregivers across the caregiving course in amyotrophic lateral sclerosis: A qualitative analysis. BMJ Open, 8(1), e018721. https://doi.org/10.1136/bmjopen-2017-018721
- Giovannetti, A. M., Quintas, R., Tramacere, I., Giordano, A., Confalonieri, P., Messmer Uccelli, M., … Pakenham, K. I. (2020). A resilience group training program for people with multiple sclerosis: Results of a pilot single-blind randomized controlled trial and nested qualitative study. PLoS ONE, 15(4), e0231380. https://doi.org/10.1371/journal.pone.0231380
- Glueckauf, R. L., Davis, W. S., Willis, F., Sharma, D., Gustafson, D. J., Hayes, J., … Murray, L. (2012). Telephone-based, cognitive-behavioral therapy for African American dementia caregivers with depression: Initial findings. Rehabilitation Psychology, 57(2), 124. https://doi.org/10.1037/a0028688
- Gottberg, K., Chruzander, C., Backenroth, G., Johansson, S., Ahlström, G., & Ytterberg, C. (2016). Individual face-to-face cognitive behavioural therapy in multiple sclerosis: A qualitative study. Journal of Clinical Psychology, 72(7), 651–662. https://doi.org/10.1002/jclp.22288
- Gould, R. L., Coulson, M. C., Brown, R. G., Goldstein, L. H., Al-Chalabi, A., & Howard, R. J. (2015). Psychotherapy and pharmacotherapy interventions to reduce distress or improve well-being in people with amyotrophic lateral sclerosis: A systematic review. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration, 16(5-6), 293–302. https://doi.org/10.3109/21678421.2015.1062515
- Graham, C. D., Simmons, Z., Stuart, S. R., & Rose, M. R. (2015). The potential of psychological interventions to improve quality of life and mood in muscle disorders. Muscle & Nerve, 52(1), 131–136. https://doi.org/10.1002/mus.24487
- Han, A., Yuen, H. K., Jenkins, J., & Yun Lee, H. (2021). Acceptance and Commitment therapy (ACT) guided online for distressed caregivers of persons living with dementia. Clinical Gerontologist, 1–12. https://doi.org/10.1080/07317115.2021.1908475
- Harris, M., Thomas, G., Thomas, M., Cafarella, P., Stocks, A., Greig, J., & McEvoy, R. D. (2018). Supporting wellbeing in motor neurone disease for patients, carers, social networks, and health professionals: A scoping review and synthesis. Palliative and Supportive Care, 16(2), 228–237. https://doi.org/10.1017/S1478951517000700
- Hempel, S., Norman, G., Golder, S., Aguiar-Ibáñez, R., & Eastwood, A. (2008). Psychosocial interventions for non-professional carers of people with Parkinson’s disease: A systematic scoping review. Journal of Advanced Nursing, 64(3), 214–228. https://doi.org/10.1111/j.1365-2648.2008.04806.x
- Hind, D., O’Cathain, A., Cooper, C. L., Parry, G. D., Isaac, C. L., Rose, A., … Sharrack, B. (2010). The acceptability of computerised cognitive behavioural therapy for the treatment of depression in people with chronic physical disease: A qualitative study of people with multiple sclerosis. Psychology and Health, 25(6), 699–712. https://doi.org/10.1080/08870440902842739
- Hoppes, S., Bryce, H., Hellman, C., & Finlay, E. (2012). The effects of brief mindfulness training on caregivers’ well-being. Activities, Adaptation & Aging, 36(2), 147–166. https://doi.org/10.1080/01924788.2012.673154
- Iavarone, A., Ziello, A. R., Pastore, F., Fasanaro, A. M., & Poderico, C. (2014). Caregiver burden and coping strategies in caregivers of patients with Alzheimer’s disease. Neuropsychiatric Disease and Treatment, 10, 1407. 10.2147/NDT.S58063
- Johannessen, A., Bruvik, F. K., & Hauge, S. (2015). Family carers’ experiences of attending a multicomponent psychosocial intervention program for carers and persons with dementia. Journal of Multidisciplinary Healthcare, 8, 91. https://doi.org/10.2147/JMDH.S76093
- Johnston, B., Lawton, S., McCaw, C., Law, E., Murray, J., Gibb, J., … Rodriguez, C. (2016). Living well with dementia: Enhancing dignity and quality of life, using a novel intervention, dignity therapy. International Journal of Older People Nursing, 11(2), 107–120. https://doi.org/10.1111/opn.12103
- Karekla, M., Karademas, E. C., & Gloster, A. T. (2019). The common sense model of self-regulation and acceptance and commitment therapy: Integrating strategies to guide interventions for chronic illness. Health Psychology Review, 13(4), 490–503. https://doi.org/10.1080/17437199.2018.1437550
- Kazmer, M. M., Glueckauf, R. L., Schettini, G., Ma, J., & Silva, M. (2018). Qualitative analysis of faith community nurse–led cognitive-behavioral and spiritual counseling for dementia caregivers. Qualitative Health Research, 28(4), 633–647. https://doi.org/10.1177/1049732317743238
- Kurt, A., Nijboer, F., Matuz, T., & Kübler, A. (2007). Depression and anxiety in individuals with amyotrophic lateral sclerosis. CNS Drugs, 21(4), 279–291. https://doi.org/10.2165/00023210-200721040-00003
- Larochette, C., Wawrziczny, E., Papo, D., Pasquier, F., & Antoine, P. (2020). An acceptance, role transition, and couple dynamics-based program for caregivers: A qualitative study of the experience of spouses of persons with young-onset dementia. Dementia (Basel, Switzerland), 19(8), 2714–2731. https://doi.org/10.1177/1471301219854643
- Lavoie, J.-P., Ducharme, F., Lévesque, L., Hébert, R., Vézina, J., Gendron, C., … Voyer, L. (2005). Understanding the outcomes of a psycho-educational group intervention for caregivers of persons with dementia living at home: A process evaluation. Aging & Mental Health, 9(1), 25–34. https://doi.org/10.1080/13607860412331323827
- Leventhal, H., Leventhal, E. A., & Contrada, R. J. (1998). Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychology & Health, 13(4), 717–733. https://doi.org/10.1080/08870449808407425
- Lewin, S., Bohren, M., Rashidian, A., Munthe-Kaas, H., Glenton, C., Colvin, C. J., … Tunçalp, Ö. (2018). Applying GRADE-CERQual to qualitative evidence synthesis findings—Paper 2: How to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implementation Science, 13(1), 11–23. https://doi.org/10.1186/s13012-017-0697-2
- Liu, Y., & Gellatly, J. (2021). Barriers and facilitators of engagement in psychological therapies among older adults with depression: A systematic review and thematic synthesis. Journal of Psychiatric and Mental Health Nursing, 28(4), 509–520. https://doi.org/10.1111/jpm.12697
- Liu, Z., Chen, Q.-L., & Sun, Y.-Y. (2017). Mindfulness training for psychological stress in family caregivers of persons with dementia: A systematic review and meta-analysis of randomized controlled trials. Clinical Interventions in Aging, 12, 1521. 10.2147/CIA.S146213
- Marconi, A., Gragnano, G., Lunetta, C., Gatto, R., Fabiani, V., Tagliaferri, A., … Pagnini, F. (2016). The experience of meditation for people with amyotrophic lateral sclerosis and their caregivers–a qualitative analysis. Psychology, Health & Medicine, 21(6), 762–768. https://doi.org/10.1080/13548506.2015.1115110
- Martin, F., Turner, A., Wallace, L. M., Stanley, D., Jesuthasan, J., & Bradbury, N. (2015). Qualitative evaluation of a self-management intervention for people in the early stage of dementia. Dementia (Basel, Switzerland), 14(4), 418–435. https://doi.org/10.1177/1471301213498387
- Martínez-Martín, P., Forjaz, M. J., Frades-Payo, B., Rusinol, A. B., Fernández-García, J. M., Benito-León, J., … Catalán, M. J. (2007). Caregiver burden in Parkinson's disease. Movement Disorders, 22(7), 924–931. https://doi.org/10.1002/mds.21355
- Maund, E., Dewar-Haggart, R., Williams, S., Bowers, H., Geraghty, A. W., Leydon, G., … Kendrick, T. (2019). Barriers and facilitators to discontinuing antidepressant use: A systematic review and thematic synthesis. Journal of Affective Disorders, 245(15), 38–62. https://doi.org/10.1016/j.jad.2018.10.107
- May, C. R., Eton, D. T., Boehmer, K., Gallacher, K., Hunt, K., MacDonald, S., … Richardson, A. (2014). Rethinking the patient: Using burden of treatment theory to understand the changing dynamics of illness. BMC Health Services Research, 14(1), 1–11. https://doi.org/10.1186/1472-6963-14-1
- Mays, N., & Pope, C. (2000). Assessing quality in qualitative research. BMJ, 320(7226), 50–52. https://doi.org/10.1136/bmj.320.7226.50
- Meek, C., Moghaddam, N. G., Evangelou, N., Oates, L. L., Topcu, G., Allen, C., & das Nair, R. (2021). Acceptance-based telephone support around the time of transition to secondary progressive multiple sclerosis: A feasibility randomised controlled trial. Journal of Contextual Behavioral Science, 21(July 2021), 158–170. https://doi.org/10.1016/j.jcbs.2021.07.001
- Moss-Morris, R. (2013). Adjusting to chronic illness: Time for a unified theory. British Journal of Health Psychology, 18(4), 681–686. https://doi.org/10.1111/bjhp.12072
- Moss-Morris, R., Dennison, L., Landau, S., Yardley, L., Silber, E., & Chalder, T. (2013). A randomized controlled trial of cognitive behavioral therapy (CBT) for adjusting to multiple sclerosis (the saMS trial): Does CBT work and for whom does it work? Journal of Consulting and Clinical Psychology, 81(2), 251. https://doi.org/10.1037/a0029132
- Nehrig, N., & Chen, C. K. (2019). How to address the needs of non-responders to REACH VA: A qualitative analysis. Aging & Mental Health, 23(9), 1203–1208. https://doi.org/10.1080/13607863.2018.1484885
- Nehrig, N., Gillooly, S., Abraham, K., Shifrin, M., & Chen, C. K. (2019). What is a nonresponder? A qualitative analysis of nonresponse to a behavioral intervention. Cognitive and Behavioral Practice, 26(2), 411–420. https://doi.org/10.1016/j.cbpra.2018.07.006
- Nehrig, N., Shifrin, M., Abraham, K., & Chen, C. K. (2019). The benefits and limitations of a behavioral intervention for caregivers of dementia patients: A qualitative study. Cognitive and Behavioral Practice, 26(3), 562–574. https://doi.org/10.1016/j.cbpra.2018.10.004
- Orgeta, V., Qazi, A., Spector, A., & Orrell, M. (2015). Psychological treatments for depression and anxiety in dementia and mild cognitive impairment: Systematic review and meta-analysis. The British Journal of Psychiatry, 207(4), 293–298. https://doi.org/10.1192/bjp.bp.114.148130
- Ovaska-Stafford, N., Maltby, J., & Dale, M. (2021). Literature review: Psychological resilience factors in people with neurodegenerative diseases. Archives of Clinical Neuropsychology, 36(2), 283–306. https://doi.org/10.1093/arclin/acz063
- Pegler, R. (2017). A feasibility study of acceptance and commitment therapy to promote the wellbeing of carers of people with dementia: & clinical research portfolio. University of Glasgow.
- Potter, K.-J., Golijana-Moghaddam, N., Evangelou, N., Mhizha-Murira, J. R., & Das Nair, R. (2021). Self-help acceptance and commitment therapy for carers of people with multiple sclerosis: A feasibility randomised controlled trial. Journal of Clinical Psychology in Medical Settings, 28(2), 279–294. https://doi.org/10.1007/s10880-020-09711-x
- Purgato, M., Singh, R., Acarturk, C., & Cuijpers, P. (2021). Moving beyond a ‘one-size-fits-all’ rationale in global mental health: Prospects of a precision psychology paradigm. Epidemiology and Psychiatric Sciences, 30, e63. https://doi.org/10.1017/S2045796021000500
- Reijnders, J. S., Ehrt, U., Weber, W. E., Aarsland, D., & Leentjens, A. F. (2008). A systematic review of prevalence studies of depression in Parkinson's disease. Movement Disorders, 23(2), 183–189. https://doi.org/10.1002/mds.21803
- Rice, D. B., Carboni-Jiménez, A., Cañedo-Ayala, M., Turner, K. A., Chiovitti, M., Levis, A. W., & Thombs, B. D. (2020). Perceived benefits and facilitators and barriers to providing psychosocial interventions for informal caregivers of people with rare diseases: A scoping review. The Patient-Patient-Centered Outcomes Research, 13, 1–49. https://doi.org/10.1007/s40271-020-00441-8
- Schrag, A., Hovris, A., Morley, D., Quinn, N., & Jahanshahi, M. (2006). Caregiver-burden in Parkinson's disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism & Related Disorders, 12(1), 35–41. https://doi.org/10.1016/j.parkreldis.2005.06.011
- Selwood, A., Johnston, K., Katona, C., Lyketsos, C., & Livingston, G. (2007). Systematic review of the effect of psychological interventions on family caregivers of people with dementia. Journal of Affective Disorders, 101(1-3), 75–89. https://doi.org/10.1016/j.jad.2006.10.025
- Sessanna, L., Nisbet, P., Alanazi, N., Lorissaint, D., Auerbach, S. L., Chang, Y.-P., & Lorenz, R. A. (2021). The experience of participating in an 8-week Mindfulness based stress reduction plus sleep retraining course among women Living with multiple sclerosis. Clinical Nursing Research, 30(5), 558–566. https://doi.org/10.1177/1054773820958125
- Simpson, R., Byrne, S., Wood, K., Mair, F. S., & Mercer, S. W. (2018). Optimising mindfulness-based stress reduction for people with multiple sclerosis. Chronic Illness, 14(2), 154–166. https://doi.org/10.1177/1742395317715504
- Simpson, R., Simpson, S., Wood, K., Mercer, S. W., & Mair, F. S. (2019). Using normalisation process theory to understand barriers and facilitators to implementing mindfulness-based stress reduction for people with multiple sclerosis. Chronic Illness, 15(4), 306–318. https://doi.org/10.1177/1742395318769354
- Sohrabi, C., Franchi, T., Mathew, G., Kerwan, A., Nicola, M., Griffin, M., Agha, M., & Agha, R. (2021). PRISMA 2020 statement: What's new and the importance of reporting guidelines. International Journal of Surgery, 88(April 1), 105918. https://doi.org/10.1016/j.ijsu.2021.105918
- Swannell, E. J. (2017). Exploring mindfulness interventions for people with dementia and their family caregivers. Canterbury Christ Church University.
- Tahsin, F., Stanyon, W., Sun, W., & Gamble, B. (2021). A single mindfulness session with informal caregivers of seniors living with dementia: A pilot qualitative descriptive study. Aging Clinical and Experimental Research, 33(2), 391–397. https://doi.org/10.1007/s40520-020-01548-6
- Tang, W. K., & Chan, C. Y. J. (2016). Effects of psychosocial interventions on self-efficacy of dementia caregivers: A literature review. International Journal of Geriatric Psychiatry, 31(5), 475–493. https://doi.org/10.1002/gps.4352
- Theed, R., Eccles, F. J., & Simpson, J. (2018). Understandings of psychological difficulties in people with the Huntington's disease gene and their expectations of psychological therapy. Psychology and Psychotherapy: Theory, Research and Practice, 91(2), 216–231. https://doi.org/10.1111/papt.12157
- Thomas, J., & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8(1), 1–10. https://doi.org/10.1186/1471-2288-8-45
- Thomas, P. W., Thomas, S., Hillier, C., Galvin, K., & Baker, R. (2006). Psychological interventions for multiple sclerosis. Cochrane Database of Systematic Reviews, 1. https://doi.org/10.1002/14651858.CD004431.pub2
- Thompson, J. C., Harris, J., Sollom, A. C., Stopford, C. L., Howard, E., Snowden, J. S., & Craufurd, D. (2012). Longitudinal evaluation of neuropsychiatric symptoms in Huntington's disease. The Journal of Neuropsychiatry and Clinical Neurosciences, 24(1), 53–60. https://doi.org/10.1176/appi.neuropsych.11030057
- Tong, A., Flemming, K., McInnes, E., Oliver, S., & Craig, J. (2012). Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Medical Research Methodology, 12(1), 1–8. https://doi.org/10.1186/1471-2288-12-181
- Tramonti, F., Bonfiglio, L., Bongioanni, P., Belviso, C., Fanciullacci, C., Rossi, B., … Carboncini, M. C. (2019). Caregiver burden and family functioning in different neurological diseases. Psychology, Health & Medicine, 24(1), 27–34. https://doi.org/10.1080/13548506.2018.1510131
- Van Groenestijn, A. C., Schröder, C. D., Visser-Meily, J. M., Reenen, E. T. K.-V., Veldink, J. H., & Van Den Berg, L. H. (2015). Cognitive behavioural therapy and quality of life in psychologically distressed patients with amyotrophic lateral sclerosis and their caregivers: Results of a prematurely stopped randomized controlled trial. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration, 16(5–6), 309–315. https://doi.org/10.3109/21678421.2015.1038276
- Vandenberg, B. E., Advocat, J., Hassed, C., Hester, J., Enticott, J., & Russell, G. (2019). Mindfulness-based lifestyle programs for the self-management of Parkinson’s disease in Australia. Health Promotion International, 34(4), 668–676. https://doi.org/10.1093/heapro/day021
- Weeks, K. R., Gould, R. L., Mcdermott, C., Lynch, J., Goldstein, L. H., Graham, C. D., … Al-Chalabi, A. (2019). Needs and preferences for psychological interventions of people with motor neuron disease. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration, 20(7–8), 521–531. https://doi.org/10.1080/21678421.2019.1621344
- Zarotti, N., Dale, M., Eccles, F., & Simpson, J. (2020). Psychological interventions for people with Huntington’s disease: A call to arms. Journal of Huntington's Disease (Preprint), 9(3), 231–243. https://doi.org/10.3233/JHD-200418
- Zarotti, N., Eccles, F. J., Foley, J. A., Paget, A., Gunn, S., Leroi, I., & Simpson, J. (2020). Psychological interventions for people with Parkinson’s disease in the early 2020s: Where do we stand? Psychology and Psychotherapy: Theory, Research and Practice, 94(3), 760–797. https://doi.org/10.1111/papt.12321
- Zarotti, N., Mayberry, E., Ovaska-Stafford, N., Eccles, F., & Simpson, J. (2020). Psychological interventions for people with motor neuron disease: A scoping review. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration, 22(1-2), 1–11. https://doi.org/10.1080/21678421.2020.1788094
- Zhang, M., Chang, Y.-P., Liu, Y. J., Gao, L., & Porock, D. (2018). Burden and strain among familial caregivers of patients with dementia in China. Issues in Mental Health Nursing, 39(5), 427–432. https://doi.org/10.1080/01612840.2017.1418034