ABSTRACT
The importance of social support for cancer patients is well-established, and mobile applications hold promise for implementation. This systematic review examines app-based interventions with social support components for cancer patients, investigating the use of different support functions from different sources and the impact on cancer-related symptoms and psychological outcomes. A systematic search across five databases (EMBASE, Scopus, PsycINFO, PubMed, Web of Science) yielded 449 records, of which 17 studies (12 controlled designs) were included. Two independent reviewers extracted data and assessed study quality, revealing a high risk of bias across studies. Social support was implemented through different app functions, including contact/chat functions (n = 9), automatic alerts based on app input (n = 6) and discussion forums (n = 5). Social support predominantly focused on informational support (n = 17), mostly from healthcare professionals. Emotional support was less common (n = 7). Results indicated some promising intervention effects for pain, fatigue, nausea/vomiting, insomnia, constipation and overall symptom distress, but heterogeneous effects for health-related quality of life. Overall, results were mixed, but indicate that mobile apps incorporating social support may hold promise for cancer patients. However, future studies should focus on measuring and reporting social support as an intervention mechanism to systematically investigate its specific impact and improve effectiveness.
Apps for cancer patients predominantly include informational social support
Emotional social support is substantially less frequently included
Apps focus on formal support sources like healthcare professionals
First results are somewhat promising for improving cancer-related symptoms
Highlights
Introduction
The influence of social relationships on physical, mental, and functional health is widely recognised (e.g., Berkman et al., Citation2000; Cohen, Citation1988; House et al., Citation1988; Seeman, Citation1996; Uchino, Citation2004). One way through which social relationships might benefit health is social support. Social support has been conceptualised in various ways, often used as an umbrella term encompassing different aspects of supportive interactions (Schwarzer et al., Citation2004; Schwarzer & Knoll, Citation2007). It can be defined as ‘resources provided by others’ (Cohen & Syme, Citation1985, p. 4) and is often ‘used in a broad sense referring to any process through which social relationships might promote health and well-being’ (Cohen, Citation2004, p. 4). Earlier definitions focus on the benefits of social support in times of need and distress (Uchino, Citation2009), while more recent definitions also consider support for goal attainment and thriving independent of stress (Feeney & Collins, Citation2015). From the perspective of the recipient, two different types of social support can be distinguished: perceived available support and actual received support in the past (e.g., Cohen et al., Citation2001; Schwarzer & Knoll, Citation2010). This distinction is crucial as perceived available and actual received support are distinct constructs that do not show a high empirical overlap (Schwarzer & Knoll, Citation2010).
Social support is a multidimensional construct that can serve various functions (e.g., Cohen & Syme, Citation1985; Knoll et al., Citation2018). The number of functions it encompasses varies across the literature, but a prominent categorisation is into emotional, informational, and instrumental social support (e.g., Cohen, Citation2004; House et al., Citation1988). Emotional support involves elements such as empathy, care, trust, reassurance, and understanding. Informational support refers to the assistance with seeking and understanding of information, advice, or guidance. Instrumental support usually encompasses the provision of financial or material aid, resources as well as practical assistance in task-related activities (e.g., Antonucci, Citation1985; House & Kahn, Citation1985; Knoll et al., Citation2018). However, in the medical setting instrumental support has been extended by including aspects of advocacy, i.e., actions to protect from external sources or stress, assistance in medical-decision making in the form of directive guidance, i.e., taking responsibility, taking care and organising the treatment process or organising additional aid (e.g., Arora et al., Citation2007; Rose, Citation1990).
Social support can be provided by a variety of sources. Initially the social support literature focused on social support provided by informal support sources, such as family and friends, emphasising the importance of a personal relationship between provider and recipient (e.g., Cohen et al., Citation2001). More recent research argues that social support can be provided by both these informal support sources and more formal sources such as healthcare professionals (Heaney & Israel, Citation2008). It is assumed that the primary function of social support thereby varies depending on the source of social support (e.g., Agneessens et al., Citation2006; Heaney & Israel, Citation2008; Rose, Citation1990). For example, research in medical settings show that family and friends tend to provide more emotional support (Arora et al., Citation2007; Blanchard et al., Citation1995; Tunin et al., Citation2010) while healthcare professionals typically offer more informational support (e.g., Blanchard et al., Citation1995). Similarly, Hogan et al. (Citation2002) differentiates between natural support systems such as family and friends and more formal support systems including professionals as well as connections within communal or societal networks. They argue that natural support systems cannot be characterised as inherently better or more effective, even though support from family and friends might be more stable and enduring (Hogan et al., Citation2002).
Social support is suggested to have both direct and indirect effects on health by buffering the effect of stress, but also enhancing health by promoting health-enhancing and reducing health-compromising behaviours (Berkman et al., Citation2000; Schwarzer & Leppin, Citation1991). Numerous studies have shown links between social support and the incidence of both physical and mental diseases and multiple health outcomes including mortality rates (Callaghan & Morrissey, Citation1993; Holt-Lunstad et al., Citation2010).
One disease context in which social support is of particular relevance is cancer (e.g., Ell et al., Citation1992; Kroenke, Citation2018; Pinquart & Duberstein, Citation2010). Although cancer is a leading cause of death and disability worldwide, advances in treatment and diagnosis have significantly increased the relative survival rate (American Cancer Society, Citation2022; World Health Organization, Citation2022). However, a cancer diagnosis is not only an extremely stressful life-event evoking emotions such as anxiety (e.g., Stark & House, Citation2000), but can also impact the entirety of a patient's life going forward, as side effects of treatments are often severe and many cancer survivors also report negative long-term symptoms and side effects associated with their disease or the treatment (Boyes et al., Citation2012; Harrington et al., Citation2010). Several studies indicate positive associations between social support and emotional adjustment or coping with a cancer diagnosis (e.g., Drageset & Lindstrom, Citation2005; Dukes Holland & Holahan, Citation2003), quality of life and well-being (e.g., Luszczynska et al., Citation2013), as well as with cancer progression in terms of life expectancy (e.g., Kroenke, Citation2018; Nausheen et al., Citation2009; Pinquart & Duberstein, Citation2010).
The question, however, is how to successfully implement and promote social support during and after treatment. The use of mobile phone interventions has shown beneficial effects on chronic disease management (e.g., Marcolino et al., Citation2018; Q. Yang & Van Stee, Citation2019). More specifically, mobile applications have shown promise in cancer prevention, detection, and care management (e.g., Houghton et al., Citation2019; Jongerius et al., Citation2019; Odeh et al., Citation2015; Pereira-Azevedo & Venderbos, Citation2018; Wesley & Fizur, Citation2015), and the number of cancer-related apps is increasing. Technical features of smartphones not only increase the availability and accessibility of health information but also allow the incorporation of interactive features such as real-time health information tracking and interaction with other users or health professionals (Klasnja & Pratt, Citation2012). However, even though a large number of commercial cancer-related apps is publicly available for download (e.g., Bender et al., Citation2013; Charbonneau et al., Citation2020; Giunti et al., Citation2018) and multiple reviews map the emerging and rapidly evolving field of cancer-related apps (e.g., Ana et al., Citation2020; Collado-Borrell et al., Citation2016; Davis & Oakley-Girvan, Citation2015; Jongerius et al., Citation2019; Putranto & Rochmawati, Citation2020; Rincon et al., Citation2017), the majority of available apps do not yet take full advantage of the technical capabilities of smartphones (Bender et al., Citation2013). Overall, most apps focus on providing static information about cancer and managing treatment and only a small percentage includes interactive features to monitor symptoms or side effects or allow formal or informal social support from healthcare professionals, or peers, family and friends (e.g., Bender et al., Citation2013; Charbonneau et al., Citation2020; Giunti et al., Citation2018). To date, there is no detailed description and characterisation of the few apps that use social support components. Therefore, there is a lack of clarity not only regarding the technical implementation of social support within mobile applications, but also concerning the aspects of social support included. A differentiated description and analysis of social support functions (emotional, informational, instrumental) in connection with the source providing the support (formal, informal) within mobile applications for cancer patients is currently lacking. Consequently, this gap hinders to draw conclusions about the effectiveness of support interventions using mobile applications for cancer patients.
Objectives
The aim of the present review was to synthesise and assess research on mobile applications for cancer patients that incorporate social support components from different sources (formal, informal). The overarching research question was: What social support interventions using mobile applications exist to improve cancer outcomes and how effective are they? Thus, the aim of the review was two-fold. Our first aim was to present a detailed overview of how social support is realised and implemented in mobile applications. Thereby, we aimed to examine social support aspects in detail, differentiating between three common functions of social support (emotional, informational, instrumental) and different support sources (formal, informal) that have previously been described as important and helpful by cancer patients (Arora et al., Citation2007; Bol et al., Citation2022; Luszczynska et al., Citation2013; Rose, Citation1990). Besides providing a descriptive overview, the second aim of the review was to examine the effectiveness of the included interventions in relation to the improvement of cancer-related symptoms and psychological outcomes such as quality of life, anxiety, or depression. As many publicly available cancer-related apps lack scientific evaluation (see e.g., Bender et al., Citation2013; Charbonneau et al., Citation2020), we focused on app-based interventions with a social support component published in academic literature instead of searching app stores. It was not a pre-requisite that social support was mentioned explicitly as a primary intervention strategy and/or that the study measured whether the intervention was successful to increase social support. The health behaviour change literature (e.g., smoking cessation, Faseru et al., Citation2018) indicates that intervention studies on social support often do not explicitly assess subjective reports of received social support.
Method
This study was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA; Page et al., Citation2021) statement guidelines (see appendix 4, Table A2 and A3). This systematic review protocol is registered with the Prospective Register of Systematic Reviews database (ID number: CRD42022303720; submitted January 14th, 2022).
Search strategy
A comprehensive systematic literature search was conducted in January 2022 across five electronic databases: EMBASE, Scopus, PsycINFO, PubMed, and Web of Science (Core Collection). Search terms focused on the following themes critical to the research question: cancer, mHealth, social support, cancer outcomes, and intervention (see supplemental data 1 for the entire search term specified for each data base). Terms were mapped to controlled vocabulary (e.g., MeSH terms) and Boolean operators were employed to combine the themes. Searches were limited to publications since 2008 as the use of smartphone-based applications is a more recent development. Reference lists of included studies and relevant systematic reviews and meta-analyses were also searched to identify other potentially eligible studies.
Inclusion and exclusion criteria
Studies were eligible for inclusion if they focused on adults aged 18 years or more with any type or stage of cancer, and applied an intervention focusing on social support delivered through a mobile health application. Social support was defined as resources provided by others, as coping assistance, or as an exchange of resources (Schwarzer & Knoll, Citation2010). Social support could fulfil emotional functions such as providing empathy and understanding. It could also serve informational functions such as to empower patients with information they need to successfully cope with the situation or provide guidance and advice to increase understanding of the situation or perception of control. Finally, support could also provide instrumental functions including the concrete assistance during symptom management such as adjusting treatment or medication or directive guidance in terms of taking responsibility and managing treatment options. Social support could be provided from both, formal (e.g., healthcare professionals) or informal (e.g., family, friends, peers) support sources. Studies were included if they measured and reported at least one cancer-related symptom or psychological outcome such as quality of life. Both controlled trials (randomised and non-randomised) without any restriction on the type of control condition, and trials using a pre-post design were eligible for inclusion. Exclusion criteria included interventions offered to a population other than cancer patients; patients <18 years; interventions delivered via websites, messaging services, telephone, or videoconference only without a mobile app component; delivery of the social support components outside the app and publication not available in English language.
Data selection and extraction
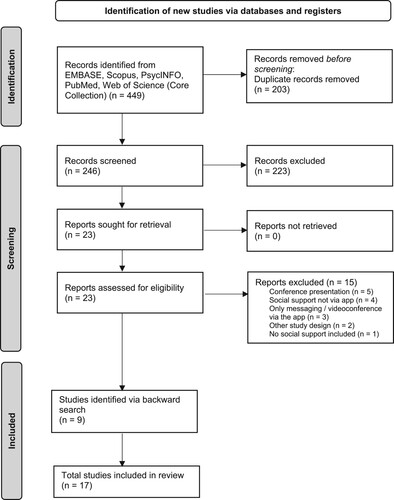
Results of database searches were imported into the Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia, available at www.covidence.org) and duplicates were removed. Articles were screened in a two-step screening process assessing (1) title and abstracts and (2) remaining full-text articles by two trained independent reviewers. Any disagreement regarding eligibility was resolved through discussions between reviewers and the review team until a consensus was reached. displays a PRISMA flowchart for the study selection process.
Data were systematically extracted following the ‘template for intervention description and replication’ (TIDieR; Hoffmann et al., Citation2014) and a custom-designed data extraction form implemented in Covidence. Data extraction included information on population characteristics, intervention design and implementation, social support, theoretical background, inclusion of patient’s perspective and outcome measures. Data were extracted and coded by two trained reviewers independently and any disagreement in extracted data was resolved through discussions between reviewers and the study team. In addition, behaviour change techniques (BCTs; Michie et al., Citation2013) were coded to provide a comprehensive overview of techniques used in the intervention also beyond social support.
To examine the effectiveness of the intervention, effects on the most commonly assessed cancer-related symptoms (appetite loss, constipation, diarrhoea, dyspnea, fatigue, insomnia, nausea/vomiting, pain, overall symptom distress, and overall symptom strength) were evaluated. Examined psychological outcomes were health-related quality of life (including the subscales emotional, cognitive, social, and role functioning/well-being), as well as anxiety/worry, depression and self-efficacy.
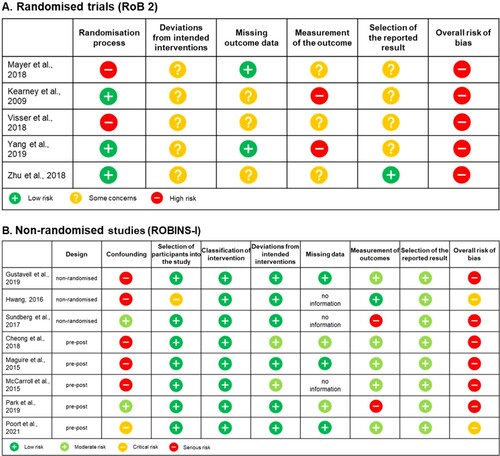
Risk of bias assessment
Risk of bias was assessed according to the Cochrane Collaboration guidelines for randomised trials (RoB 2; Higgins et al., Citation2019; Sterne et al., Citation2019) and non-randomised studies (ROBIN-I, Sterne et al., Citation2016). Risk of bias for randomised trials was rated as low or high risk, or having some concerns and an overall score was calculated following the assessment scheme for randomised trials (RoB 2; Higgins et al., Citation2019; Sterne et al., Citation2019). Risk of bias of non-randomised studies was rated as low, moderate, serious or critical risk or no information and an overall score was calculated following the guidelines for non-randomised studies (ROBIN-I, Sterne et al., Citation2016).
Results
Database searches yielded 449 articles. After removing duplicates, titles and abstracts of 246 articles and 23 resulting full-texts were screened, identifying eight studies meeting all inclusion criteria. In addition, nine studies were identified via a backward search, resulting in a total of 17 studies included in the systematic review (see supplemental data 2 for a list of all included studies). The full description for article exclusion is presented in the PRISMA diagram ().
Study characteristics
An overview of the main study details and characteristics is presented in and in Table A1 in supplemental data 3. Studies were published between 2009 and 2021 and conducted in Europe (n = 7), Asia (n = 6) or North America (n = 4). The majority of studies employed a controlled design (n = 12) including five randomised controlled designs, three study protocols of randomised trials, three non-randomised trials and one study protocol of a quasi-experimental design. The interventions were compared to usual care (n = 10), no-treatment waitlist (n = 1) and an offline intervention (n = 1). The remaining five studies were pre-post studies analysing changes over time.
Table 1. Overview of included studies.
Across all 17 studies, implemented or planned intervention duration ranged from two to 144 weeks (M = 17.84, SD = 21.88). A follow-up assessment was included in six studies (Spahrkas et al., Citation2020; Sundberg et al., Citation2017; Visser et al., Citation2018; Vistad et al., Citation2021; Zhu et al., Citation2017, Citation2018) ranging from three months to three years. To implement the intervention, 13 different apps or app combinations were used across the 17 studies. Only two studies used commercially available apps (McCarroll et al., Citation2015; Visser et al., Citation2018), while the majority of the apps was developed or adapted by the research team for the purpose of the intervention. The majority of interventions (n = 13) focused on providing care or information and/or symptom management as an addition during treatment or rehabilitation. Only two studies reported that enhancing/facilitating social support and care was the primary goal of the intervention (Poort et al., Citation2021; Visser et al., Citation2018), while the remaining two studies (Mayer et al., Citation2018; McCarroll et al., Citation2015) focused on life-style changes (see ). In total, only six studies (Lin et al., Citation2021; Mayer et al., Citation2018; McCarroll et al., Citation2015; Poort et al., Citation2021; Zhu et al., Citation2017, Citation2018) offered insight into the theoretical background underlying the development of the studies. However, even in those studies, the information regarding how the theoretical background informed app development was rather limited. Further, also only six studies included patients during the development process of the app by co-designing and testing the app together with patients (Sundberg et al., Citation2017), assessing patient preferences and opinions via interviews (Gustavell et al., Citation2019), conducting focus group/user panel meetings (Kearney et al., Citation2009; Maguire et al., Citation2015; Poort et al., Citation2021; Vistad et al., Citation2021), or testing a beta version of the app with patients to receive specific feedback (Kearney et al., Citation2009; Maguire et al., Citation2015; Poort et al., Citation2021).
Demographic characteristics are described across the 13 studies reporting study results. Across these studies, the mean sample size was 84.62 (SD = 55.32; range 11–227) with a total of 1100 participants. Mean age of participants ranged from 28 to 69 years (M = 56.46, SD = 10.27). Across participants, 60% were women with two studies focusing solely on women (McCarroll et al., Citation2015; Zhu et al., Citation2018) and one study solely on men (Sundberg et al., Citation2017). Patients with a wide range of cancer types were included in the studies with breast cancer being the most common cancer diagnosis (n = 7; see Table A1 in supplemental data 3). Stage of cancer varied between studies, but also within studies as studies included patients from different cancer stages and across different treatment stages. In the majority of studies (n = 11), participants received ongoing cancer treatment while participating in the intervention (see Table A1 in supplemental data 3).
Outcome assessment
In total, eight studies (Cheong et al., Citation2018; Gustavell et al., Citation2019; Kearney et al., Citation2009; Maguire et al., Citation2015; Spahrkas et al., Citation2020; Sundberg et al., Citation2017; Vistad et al., Citation2021; J. Yang et al., Citation2019) assessed self-reported symptoms within the app using mainly self-developed questionnaires and items to assess frequency, severity, and distress associated with symptoms. The number of assessed symptoms ranged from two to 15. Frequency of assessment varied twice daily (Kearney et al., Citation2009) to once a month (Vistad et al., Citation2021), partly supplemented by additional event-based assessments.
To analyse the effect of the intervention, all studies also assessed outcome measures outside the app with additional questionnaires during and/or at the end of the intervention. Based on the great diversity of included cancer types, the type and number of recorded cancer-related symptoms varied substantially between studies. Cancer-related symptoms were assessed via various multi-symptom scales (e.g., European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30), MD Anderson Symptom Inventory (MDASI), Edmonton Symptom Assessment Scale), and/or cancer-type specific symptom scales and individual symptoms or symptom lists. In addition, symptoms of side effects of ongoing treatments or consequences such as unscheduled hospital visits were recorded (see Table A1 in supplemental data 3). In terms of psychological outcomes, the majority of studies assessed health-related quality of life, using the general or cancer-type specific EORTC QLQ-C30 or the general or cancer-type specific FACT (Functional Assessment of Cancer Therapy). In addition, different measures of anxiety, worry/fear, depression, self-efficacy, and distress were reported, using a variety of different measures and questionnaires (see Table A1 in supplemental data 3).
Risk of bias assessment
Overall the assessment of the Cochrane Collaboration Risk of Bias indicated a potential high risk of bias in all randomised controlled trials, with concerns in multiple domains (see (a)) and a potential serious to critical risk of bias in all non-randomised studies (see (b)). However, the nature of the intervention needs to be considered for the interpretation of results for both study designs. In particular, the use of an app for continuous symptom assessment introduces a potential risk of influencing the outcome assessment and achieving complete blinding of both participants and study personnel is not feasible for the type of intervention under investigation.
Figure 2. Risk of bias assessment of (a) randomised trials and (b) non-randomised studies. Note that risk of bias rating varies between randomised trials and non-randomised studies. According to the respective guideline, risk of bias is rated as low or high risk, or having some concerns for (a) randomised trials and as low, moderate, serious or critical risk or no information for (b) non-randomised studies. Overall risk of bias of (a) randomised trials is rated as high if a study is judged either at high risk in at least one domain or if a study is judged to have some concerns for multiple domains. Overall risk of bias of (b) non-randomised studies is rated as serious if a study is judged at serious risk in at least one domain, but not at critical risk in any domain and rated as critical if a study is judged at critical risk in at least one domain (see Higgins et al., Citation2019; Sterne et al., Citation2016, Citation2019).
What app-based interventions including social support exist?
The first aim of the study was to provide a detailed description of how and what type of social support is realised and implemented in app-based interventions. Content and integration of social support in the app varied between studies with different forms, combinations and functions applied (see for a detailed overview). Most commonly contact/chat functions of the app were used (n = 9), followed by the use of alerts to evoke supportive reactions (e.g., from healthcare professionals) based on app input (n = 6), discussion forums and communication platforms (n = 5), private chat functions and social networking spaces (n = 2).
Social support sources
Across studies, social support was considered from both formal sources, like (healthcare) professionals, and informal support sources, such as family, friends or peers. The analysis revealed a notably higher frequency of inclusion of social support from formal support sources (n = 15) compared to social support from informal support sources (n = 7). In total, 10 studies exclusively included social support from formal sources, whereas only two interventions focused on facilitating support from informal sources such as family, friends or peers (Poort et al., Citation2021; Spahrkas et al., Citation2020). The remaining studies (n = 5) combined both formal and informal support. Notably, none of the five studies that integrated formal and informal support specifically aimed at increasing support from close personal networks, such as friends or family, but only from peers.
Social support function
The function of social support varied between studies. Informational social support was present in all studies (n = 17), and accompanied with instrumental social support in the majority of studies (n = 9). Only 7 studies included forms of emotional social support.
Informational support. Informational social support encompassed providing advice and guidance for managing symptoms, self-care, disease management, as well as specific information and education about the illness, rehabilitation, coping strategies, and adjusting to life post-cancer diagnosis. For example, in the study of Cheong et al. (Citation2018) patients received an individualised rehabilitation exercise programme with the ability to communicate in real-time with a health expert through the app to receive feedback and information. Likewise, patients in the study of Hwang (Citation2016) could communicate with experts through the app, asking questions and addressing concerns about their uploaded wound pictures. Further, Lin et al. (Citation2021) included gynecological cancer-specific education helping patients better predict and understand their illness and related symptoms to reduce uncertainty in illness and symptom distress. Different communication forums were used to provide informational support from credible authorities (healthcare providers) including advice related to posted messages and the option for all patients to contact and seek advice or guidance from the healthcare team. Similarly, to provide informational support to women with breast cancer, Zhu et al. (Citation2017, Citation2018) included a communication forum to facilitate the interaction with both healthcare professionals and peers. The platform allowed the sharing and receiving of information and advice on symptom management, as well as on how to live and cope with the disease. In addition, patients had the option to interact with healthcare professionals receiving expert advice and consultation as needed. J. Yang et al. (Citation2019) used a automatic alarm system to facilitate patient communication with a healthcare team via a real-time chat-based consultation feature. This allowed patients to report pain and other symptoms, engage in discussions to understand potential causes of the pain, and receive advice on how to address and manage the pain.
Instrumental support. Content of informational and instrumental social support was related in most studies, as most not only provided information and advice but also provided assistance with symptom/disease management, and/or assistance with exercise performance. For example, to facilitate instrumental and informational social support six of the studies used an automatic alert system based on symptom reports, i.e., healthcare providers or the patient themselves received an alarm if reported symptoms reached a threshold to initiate contact and support for symptom management (see ). In the majority of those studies (n = 4; Gustavell et al., Citation2019; Kearney et al., Citation2009; Maguire et al., Citation2015; Sundberg et al., Citation2017) patients were contacted by healthcare professionals if their symptom reports triggered an alert. Depending on the severity of symptoms the time span until patients were contacted differed. However, once contacted, patients received assistance in medical-decision making. This involved healthcare professionals performing a clinical assessment to discuss and address symptom management, as well as initiating appropriate management strategies.
Emotional social support. Emotional social support was provided via functions that enabled users to exchange personal experience and connect with peers. For example, Poort et al. (Citation2021) aimed to improve psychological care for young cancer patients by creating an engaged community where patients could connect and share personal content with peers. The app facilitated interaction between patients through private messaging, a virtual waiting room to connect and interact with other patients, as well as a community feed where patients could share experiences and discuss posts with others. Similarly, Mayer et al. (Citation2018) included a social networking space with messaging, and a discussion forum for sharing experiences and connecting with other cancer patients. Zhu et al. (Citation2017, Citation2018) implemented a moderated discussion forum for patients to interact and share personal experiences with other cancer patients. Lin et al. (Citation2021) described an app-based programme enabling patients and caregivers to discuss and share experiences in a discussion centre and separate forums in order to exchange personal experiences and connect with peers. Similarly, Visser et al. (Citation2018) included nurse-led online support groups to increase psycho-social support and foster the exchange and discussion of personal experiences and the interaction with other cancer patients. In addition, the study by Spahrkas et al. (Citation2020) included the option to invite friends and family to an app-based self-management programme to help/motivate to work with the app and to manage symptoms of fatigue together. However, the concrete implementation of the support from family and friends was not described in detail.
How effective are app-based interventions including social support to improve cancer-related outcomes?
The following reported effects on outcome measures refer to the effect of the entire intervention. Due to the small number of studies, additional separate analyses based on the source of social support (formal vs informal) or different social support features within the app were not possible.
Cancer-related symptoms. The effect on cancer-related symptoms was analysed across eight studies (see Table A1 in supplemental data 3 for a detailed overview). While the specific symptoms assessed varied between studies, in multiple symptom areas the majority of studies demonstrated positive effects of the intervention compared to a control condition or over time (see (a)). Nevertheless, as illustrated in (a), results were also mixed across studies with a combination of positive effects and no effects, and in isolated cases even a negative effect, e.g., a significant increase for pain (Maguire et al., Citation2015) and diarrhoea (Sundberg et al., Citation2017) over time.
Figure 3. Overview of study results displaying differences between intervention and control group and changes over time for (a) cancer-related symptoms and (b) psychological outcomes.
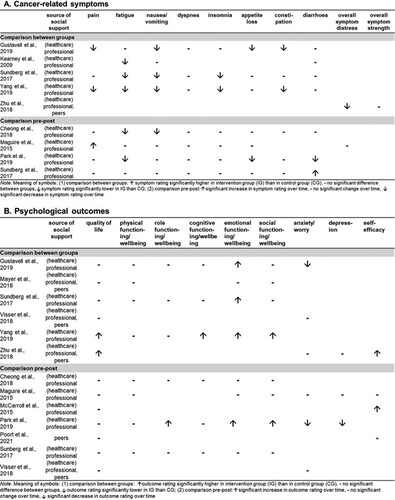
Psychological outcomes. Intervention effects regarding psychological outcomes were analysed across eleven studies (see Table A1 in supplemental data 3 for a detailed overview). Overall results regarding psychological outcomes were less clear across the analysed studies (see (b)). Specifically, as (b) displays, only two studies (J. Yang et al., Citation2019; Zhu et al., Citation2018) indicated a positive effect on overall health-related quality of life while the majority of studies did not find any effects on overall health-related quality of life, neither between groups nor over time. Similarly, the effects on anxiety/worry, depression and self-efficacy did not present a consistent pattern.
Mediator. Perceived social support was only measured in a total of three studies (Poort et al., Citation2021; Visser et al., Citation2018; Zhu et al., Citation2018). Perceived social support was positively associated with app usage (Zhu et al., Citation2018) and satisfaction ratings (Visser et al., Citation2018), and showed a slightly positive, but non-significant, trend over time (Poort et al., Citation2021). Potential effects of social support on outcome measures were not examined in any of these studies. However, Zhu et al. (Citation2018) examined the correlation between app usage and psychological outcomes, which could be an indicator of potential social support. While positive associations emerged between app usage and self-efficacy both after three months (r = .290, p = .03) and six months (r = .329, p = .01), app usage was only positively associated with quality of life after three months (r = .273, p = .04), and negatively with anxiety after six months (r = -.300, p = .03). Similarly, McCarroll et al. (Citation2015) examined the potential beneficial effect of frequency of interaction with healthcare professionals. However, data showed no support for more interaction via the app being positively associated with psychological outcomes.
Discussion
The present systematic review aimed to provide an overview of mobile applications facilitating social support for cancer patients and examine their effectiveness for cancer-related symptoms and psychological outcomes. Across 17 studies, diverse implementations of social support through mobile apps were found. App-based provided social support predominantly focused on informational support (e.g., how to manage symptoms) mainly from formal support sources such as (healthcare) professionals. In contrast, emotional support and informal support, such as from family or friends, were substantially less commonly addressed by the apps. Results in terms of the effectiveness were mixed and need to be interpreted with caution as risk of bias assessment indicated an overall high risk of bias across studies. However, some promising effects were observed in addressing cancer-related symptoms and encouragingly, with the exception of two studies (Maguire et al., Citation2015; Sundberg et al., Citation2017), no negative effects of the app-based interventions emerged on any cancer-related or psychological outcome.
Examining social support research for cancer patients that is not app-based, most studies focus on emotional social support from informal sources, such as peers, family or friends (Decker, Citation2007; Luszczynska et al., Citation2013). In contrast, the predominant function of social support across studies in this review was informational social support and it was majorly provided by formal support sources. Multiple studies have highlighted the importance and benefit of emotional support for cancer patients (e.g., Dukes Holland & Holahan, Citation2003; Dunkel-Schetter, Citation1984). For example, research on perceived helpfulness of received social support showed that after a diagnosis, cancer patients perceive emotional support both from family and friends and from healthcare professionals as helpful (Arora et al., Citation2007). The Theory of Optimal Matching (Cutrona, Citation1990; Cutrona & Russell, Citation1990) and the Social Support Effectiveness Framework (Rini & Dunkel Schetter, Citation2010) emphasise that the effectiveness of social support depends on how well it meets the specific needs of the recipients. In light of this, it seems highly beneficial to incorporate more options in mobile applications to seek and provide emotional social support to address the emotional support needs of cancer patients, thereby most likely enhancing the effectiveness of such mobile interventions.
The main source of social support across studies included in this review was formal support from professionals such as healthcare providers or experts. Even though reviews demonstrate the value and benefits of peer support for cancer patients (Campbell et al., Citation2004; Dunn et al., Citation2003; Hoey et al., Citation2008; Hu et al., Citation2019), only seven studies included informal support from peers using private messaging or community feeds. Similarly, a review and content analysis of almost 300 publicly available cancer-related apps revealed that very few cancer-related apps include peer support (Bender et al., Citation2013). Social support provided is likely to differ between sources of social support (Heaney & Israel, Citation2008). In the context of cancer, research has shown that cancer patients typically seek informational support from (healthcare) professionals (e.g., Blanchard et al., Citation1995), and emotional support from family in forms of caring, empathising and comforting (Arora et al., Citation2007; Blanchard et al., Citation1995; Tunin et al., Citation2010). In addition, in five of the included studies, social support can be interpreted as rather low as the interaction between patients and healthcare professionals was only initiated when a certain threshold of symptom severity or distress was reached triggering an automated alarm system to start patient-healthcare provider interaction supporting patients in symptom management. Overall, current cancer-related apps seem to underutilise smartphones’ potential for real-time communication, networking, and personalised support. Future apps should leverage these capabilities to increase support for cancer patients, and to allow customisation to meet individual needs.
Although the systematic review included the provision or facilitation of social support through the app as an inclusion criterion, social support was not the central intervention component in most studies. A unified approach to transparently highlight all intervention components using a shared terminology as e.g., offered by the behaviour change techniques technologies (e.g., Di Maio et al., Citation2024; Marques et al., Citation2023; Michie et al., Citation2013) still is not standard in this area of research, but urgently should be. Overall, only a small subset of studies not only incorporated social support but also explicitly measured and assessed perceived social support. Some of these studies were able to demonstrate positive associations with app usage or satisfaction with the app. While this is encouraging, future studies should focus on assessing and examining the actual receipt of social support as mediating mechanism of the app intervention in addition to a rather stable measure of perceived availability of support (Schwarzer & Knoll, Citation2010). Further, assessing the effect of the three different functions of support (emotional, informational, instrumental) as well as exploring and comparing the effects of the different support functions in relation to the source providing the support (formal, informal) and depending on treatment stage or cancer type would offer valuable insights (e.g., see Heaney & Israel, Citation2008; Kroenke, Citation2018). However, as most analysed studies combined multiple functions of social support and due to the limited number of studies incorporating emotional support, it was not possible to conduct such a comparison in the present review.
The presented review has certain limitations. First, to identify relevant studies the term social support was included as a criterion in the search term. However, backward searches indicated that the term social support might not always be used in the title or abstract if the main focus of the studies is not facilitating or providing social support. To address this problem and to ensure that we did not miss substantial studies in our search, we performed an intensive backward search screening the entire full texts for social support components. Second, as mentioned above, included studies did not solely concentrate on social support aspects as their primary intervention strategy, but rather tested interventions that include social support components as one aspect of their intervention along with a range of other techniques and strategies (see also and Table A1 in supplemental data 3 for a detailed overview of the content of each app and general BCTs used). Therefore, only the entire intervention effect could be examined as studies did not provide information on the effectiveness of the intervention in relation to social support only. This calls for a greater transparency of all intervention components used in mobile applications for cancer patients. Using a common terminology as offered by the behaviour change techniques taxonomies (e.g., Di Maio et al., Citation2024; Marques et al., Citation2023; Michie et al., Citation2013) seems to be a constructive approach to tackle this problem. To specifically analyse the effectiveness of social support and different functions of social support on outcomes, future research using controlled intervention designs are needed systematically varying functions included in the app. Third, as quality assessment of included studies indicated an overall high risk of bias across studies and only a small number of studies based the design of their intervention on established theories or implemented a participatory approach by including patient’s perspective in the app development process, results of the review need to be interpreted with caution. Consequently, future studies need to urgently address this problem by using rigorous methodology. Finally, studies included a great diversity of cancer diagnoses and patients varied substantially in the stages of the disease and treatment. Due to the small number of studies, this heterogeneity could not be addressed. Previous work, however, suggests that support needs differ and have different effects across different stages and between cancer types (e.g., Kroenke, Citation2018; Nausheen et al., Citation2009; Pinquart & Duberstein, Citation2010). However, not only the support needs of patients might differ depending on the phase or stage of the disease, but also the ability of support providers to meet those needs. Thus, differentiated analyses separated by type and stage of cancer are needed to provide more insight into the extent to which social support or which function of social support is at what time point and under what circumstances most effective regarding cancer-related outcomes or related psychological aspects.
To conclude, the present systematic review demonstrated that app-based interventions for cancer patients including social support components predominantly include informational social support from formal sources, i.e., (healthcare) professionals while emotional social support and support from informal sources like friends or peers is rarely incorporated. Further, only a few studies themselves focused on social support as a primary intervention strategy. First results are somewhat promising regarding the use of mobile apps that include social support in improving cancer-related symptoms. However, the technical possibilities are far from being fully exploited. In particular, the potential of using smartphones to facilitate emotional support and informal support from family and friends seems hardly untapped so far, even though smartphones offer a unique opportunity to connect cancer patients with their informal support network anywhere and anytime. However, to enable informed decisions and improve effectiveness, future efforts should focus on measuring and systematically testing the specific impact of app-based interventions targeting social support.
Author contribution
KV developed the review protocol and the search strategy, conducted the searches, screened the search results for inclusion, extracted and synthesised the data, conducted the risk of bias assessment, drafted the paper and approved the final manuscript.
CB developed the review protocol and the search strategy, advised on the data extraction and risk of bias assessment, contributed to the synthesis and presentation of the results, and provided feedback and approved the final manuscript.
US developed the review protocol and the search strategy, advised on the data extraction, contributed to the synthesis and presentation of the results, and provided feedback and approved the final manuscript.
Supplemental Material
Download PDF (617.8 KB)Acknowledgements
We thank all student assistants and master students for their valuable support in the screening process of the records and the extraction of the data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Agneessens, F., Waege, H., & Lievens, J. (2006). Diversity in social support by role relations: A typology. Social Networks, 28(4), 427–441. https://doi.org/10.1016/j.socnet.2005.10.001
- American Cancer Society. (2022). The cancer atlas: Cancer survival. https://canceratlas.cancer.org/the-burden/cancer-survival/.
- Ana, F.-A., Loreto, M.-S., José, L.-M. M., Pablo, S. M., María Pilar, M. J., & Myriam, S.-L. A. (2020). Mobile applications in oncology: A systematic review of health science databases. International Journal of Medical Informatics, 133, 104001. https://doi.org/10.1016/j.ijmedinf.2019.104001
- Antonucci, T. (1985). Personal characteristics, social support, and social behavior. In R. H. Binstock & E. Shanas (Eds.), Handbook of aging and the social sciences (pp. 94–128). Van Nostrand-Reinhold.
- Arora, N. K., Finney Rutten, L. J., Gustafson, D. H., Moser, R., & Hawkins, R. P. (2007). Perceived helpfulness and impact of social support provided by family, friends, and health care providers to women newly diagnosed with breast cancer. Psycho-Oncology, 16(5), 474–486. https://doi.org/10.1002/pon.1084
- Bender, J. L., Yue, R. Y. K., To, M. J., Deacken, L., & Jadad, A. R. (2013). A lot of action, but not in the right direction: Systematic review and content analysis of smartphone applications for the prevention, detection, and management of cancer. Journal of Medical Internet Research, 15(12), e287. https://doi.org/10.2196/jmir.2661
- Berkman, L. F., Glass, T., Brissette, I., & Seeman, T. E. (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51(6), 843–857. https://doi.org/10.1016/S0277-9536(00)00065-4
- Blanchard, C. G., Albrecht, T. L., Ruckdeschel, J. C., Grant, C. H., & Hemmick, R. M. (1995). The role of social support in adaptation to cancer and to survival. Journal of Psychosocial Oncology, 13(1–2), 75–95. https://doi.org/10.1300/J077V13N01_05
- Bol, N., Rising, C. J., & van Weert, J. C. M. (2022). Perceived emotional and informational support for cancer: Patients’ perspectives on interpersonal versus media sources. Eurpean Journal of Communication, 47(2), 171–194. https://doi.org/10.1515/commun-2019-0196
- Boyes, A. W., Girgis, A., D’Este, C., & Zucca, A. C. (2012). Prevalence and correlates of cancer survivors’ supportive care needs 6 months after diagnosis: A population-based cross-sectional study. BMC Cancer, 12(1), 150. https://doi.org/10.1186/1471-2407-12-150
- Callaghan, P., & Morrissey, J. (1993). Social support and health: A review. Journal of Advanced Nursing, 18(2), 203–210. https://doi.org/10.1046/j.1365-2648.1993.18020203.x
- Campbell, H. S., Phaneuf, M. R., & Deane, K. (2004). Cancer peer support programs—Do they work? Patient Education and Counseling, 55(1), 3–15. https://doi.org/10.1016/j.pec.2003.10.001
- Charbonneau, D. H., Hightower, S., Katz, A., Zhang, K., Abrams, J., Senft, N., Beebe-Dimmer, J. L., Heath, E., Eaton, T., & Thompson, H. S. (2020). Smartphone apps for cancer: A content analysis of the digital health marketplace. Digital Health, 6, 2055207620905413. https://doi.org/10.1177/2055207620905413
- Cheong, I. Y., An, S. Y., Cha, W. C., Rha, M. Y., Kim, S. T., Chang, D. K., & Hwang, J. H. (2018). Efficacy of mobile health care application and wearable device in improvement of physical performance in colorectal cancer patients undergoing chemotherapy. Clinical Colorectal Cancer, 17(2), e353–e362. https://doi.org/10.1016/j.clcc.2018.02.002
- Cohen, S. (1988). Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology, 7(3), 269–297. https://doi.org/10.1037/0278-6133.7.3.269
- Cohen, S. (2004). Social relationships and health. American Psychologist, 59(8), 676–684. https://doi.org/10.1037/0003-066X.59.8.676
- Cohen, S., Gottlieb, B. H., & Underwood, L. G. (2001). Social relationships and health: Challenges for measurement and interventions. Advances in Mind-Body Medicine, 17(2), 129–141.
- Cohen, S., & Syme, L. (1985). Issues in the study and application of social support. In S. Cohen & S. L. Syme (Eds.), Social support and health (pp. 3–22). Academic Press.
- Collado-Borrell, R., Escudero-Vilaplana, V., Ribed-Sánchez, A., Ibáñez-García, S., Herranz-Alonso, A., & Sanjurjo-Sáez, M. (2016). Smartphone applications for cancer patients; What we know about them? Farmacia Hospitalaria, 40(1), 25–35. http://www.redalyc.org/articulo.oa?id=365964174004
- Cutrona, C. E. (1990). Stress and social support—In search of optimal matching. Journal of Social and Clinical Psychology, 9(1), 3–14. https://doi.org/10.1521/jscp.1990.9.1.3
- Cutrona, C. E., & Russell, D. W. (1990). Type of social support and specific stress: Toward a theory of optimal matching. In B. R. Sarason, I. G. Sarason, & G. R. Pierce (Eds.), Social support: An interactional view (pp. 319–266). John Wiley & Sons.
- Davis, S. W., & Oakley-Girvan, I. (2015). MHealth education applications along the cancer continuum. Journal of Cancer Education, 30(2), 388–394. https://doi.org/10.1007/s13187-014-0761-4
- Decker, C. L. (2007). Social support and adolescent cancer survivors: A review of the literature. Journal of Psychosocial Oncology, 16(1), 1–11. https://doi.org/10.1002/pon.1073
- Di Maio*, S., Villinger, K*., Knoll, N., Scholz, U., Stadler, G., Gawrilow, C., & Berli, C. (2024). Compendium of dyadic intervention techniques (DITs) to change health behaviours: A systematic review. Health Psychology Review, 34(1), 1–36. https://doi.org/10.1080/17437199.2024.2307534. *Shared first authorship.
- Drageset, S., & Lindstrom, T. C. (2005). Coping with a possible breast cancer diagnosis: Demographic factors and social support. Journal of Advanced Nursing, 51(3), 217–226. https://doi.org/10.1111/j.1365-2648.2005.03495.x
- Dukes Holland, K., & Holahan, C. K. (2003). The relation of social support and coping to positive adaptation to breast cancer. Psychology & Health, 18(1), 15–29. https://doi.org/10.1080/0887044031000080656
- Dunkel-Schetter, C. (1984). Social support and cancer: Findings based on patient interviews and their implications. Journal of Social Issues, 40(4), 77–98. https://doi.org/10.1111/j.1540-4560.1984.tb01108.x
- Dunn, J., Steginga, S. K., Rosoman, N., & Millichap, D. (2003). A review of peer support in the context of cancer. Journal of Psychosocial Oncology, 21(2), 55–67. https://doi.org/10.1300/J077v21n02_04
- Ell, K., Nishimoto, R., Mediansky, L., Mantell, J., & Hamovitch, M. (1992). Social relations, social support and survival among patients with cancer. Journal of Psychosomatic Research, 36(6), 531–541. https://doi.org/10.1016/0022-3999(92)90038-4
- Faseru, B., Richter, K. P., Scheuermann, T. S., & Park, E. W. (2018). Enhancing partner support to improve smoking cessation. Cochrane Database of Systematic Reviews, 2018(9), 1–42. https://doi.org/10.1002/14651858.CD002928.pub4
- Feeney, B. C., & Collins, N. L. (2015). A new look at social support: A theoretical perspective on thriving through relationships. Personality and Social Psychology Review, 19(2), 113–147. https://doi.org/10.1177/1088868314544222
- Giunti, G., Giunta, D. H., Guisado-Fernandez, E., Bender, J. L., & Fernandez-Luque, L. (2018). A biopsy of breast cancer mobile applications: State of the practice review. International Journal of Medical Informatics, 110, 1–9. https://doi.org/10.1016/j.ijmedinf.2017.10.022
- Gustavell, T., Sundberg, K., Segersvärd, R., Wengström, Y., & Langius-Eklöf, A. (2019). Decreased symptom burden following surgery due to support from an interactive app for symptom management for patients with pancreatic and periampullary cancer. Acta Oncologica, 58(9), 1307–1314. https://doi.org/10.1080/0284186X.2019.1633473
- Harrington, C. B., Hansen, J. A., Moskowitz, M., Todd, B. L., & Feuerstein, M. (2010). It’s not over when it’s over: Long-term symptoms in cancer survivors—A systematic review. The International Journal of Psychiatry in Medicine, 40(2), 163–181. https://doi.org/10.2190/PM.40.2.c
- Heaney, C. A., & Israel, B. A. (2008). Social networks and social support. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behavior and health education: Theory, research, and practice (Vol. 4, pp. 179). John Wiley & Sons.
- Higgins, J. P. T., Savović, J., Page, M. J., Elbers, R. G., & Sterne, J. A. (2019). Assessing risk of bias in a randomized trial. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, & V. A. Welch (Eds.), Cochrane handbook for systematic reviews of interventions (pp. 205–228). Wiley.
- Hoey, L. M., Ieropoli, S. C., White, V. M., & Jefford, M. (2008). Systematic review of peer-support programs for people with cancer. Patient Education and Counseling, 70(3), 315–337. https://doi.org/10.1016/j.pec.2007.11.016
- Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D., Altman, D. G., Barbour, V., Macdonald, H., Johnston, M., Lamb, S. E., Dixon-Woods, M., McCulloch, P., Wyatt, J. C., Chan, A.-W., & Michie, S. (2014). Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ, 348(3), g1687–g1687. https://doi.org/10.1136/bmj.g1687
- Hogan, B. E., Linden, W., & Najarian, B. (2002). Social support interventions. Clinical Psychology Review, 22(3), Article 3. https://doi.org/10.1016/S0272-7358(01)00102-7
- Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7(7), e1000316. https://doi.org/10.1371/journal.pmed.1000316
- Houghton, L. C., Howland, R. E., & McDonald, J. A. (2019). Mobilizing breast cancer prevention research through smartphone apps: A systematic review of the literature. Frontiers in Public Health, 7, 298. https://doi.org/10.3389/fpubh.2019.00298
- House, J. S., & Kahn, R. L. (1985). Measures and concepts of social support. In S. Cohen & L. Syme (Eds.), Social support and health (pp. 83–108). Academic Press.
- House, J. S., Landis, K. R., & Umberson, D. (1988). Social relationships and health. Science, 241(4865), 540–545. https://doi.org/10.1126/science.3399889
- Hu, J., Wang, X., Guo, S., Chen, F., Wu, Y., Ji, F., & Fang, X. (2019). Peer support interventions for breast cancer patients: A systematic review. Breast Cancer Research and Treatment, 174(2), 325–341. https://doi.org/10.1007/s10549-018-5033-2
- Hwang, H. (2016). Electronic wound monitoring after ambulatory breast cancer surgery: Improving patient care and satisfaction using a smart phone app. British Colombia Medical Journal, 58(8), 6.
- Jongerius, C., Russo, S., Mazzocco, K., & Pravettoni, G. (2019). Research-tested mobile apps for breast cancer care: Systematic review. JMIR MHealth and UHealth, 7(2), e10930. https://doi.org/10.2196/10930
- Kearney, N., McCann, L., Norrie, J., Taylor, L., Gray, P., McGee-Lennon, M., Sage, M., Miller, M., & Maguire, R. (2009). Evaluation of a mobile phone-based, advanced symptom management system (ASyMS©) in the management of chemotherapy-related toxicity. Supportive Care in Cancer, 17(4), 437–444. https://doi.org/10.1007/s00520-008-0515-0
- Klasnja, P., & Pratt, W. (2012). Healthcare in the pocket: Mapping the space of mobile-phone health interventions. Journal of Biomedical Informatics, 45(1), 184–198. https://doi.org/10.1016/j.jbi.2011.08.017
- Knoll, N., Scholz, U., & Ditzen, B. (2018). Social support and family processes. In T. A. Revenson & R. A. R. Gurung (Eds.), The handbook of health psychology (Vol. 3, pp. 279–289). Psychology Press.
- Kroenke, C. H. (2018). A conceptual model of social networks and mechanisms of cancer mortality, and potential strategies to improve survival. Translational Behavioral Medicine, 8(4), 629–642. https://doi.org/10.1093/tbm/ibx061
- Lin, H., Chan, S. W., Ye, M., Wang, Y., Liu, H., Li, M., Liu, S., & Zhu, J. (2021). A multi-centre randomized controlled trial of mobile gynaecological cancer support program for patients with gynaecological cancer undergoing chemotherapy: Study protocol. Journal of Advanced Nursing, 77(5), 2539–2548. https://doi.org/10.1111/jan.14809
- Luszczynska, A., Pawlowska, I., Cieslak, R., Knoll, N., & Scholz, U. (2013). Social support and quality of life among lung cancer patients: A systematic review. Journal of Psychosocial Oncology, 22(10), 2160–2168. https://doi.org/10.1002/pon.3218
- Maguire, R., Ream, E., Richardson, A., Connaghan, J., Johnston, B., Kotronoulas, G., Pedersen, V., McPhelim, J., Pattison, N., Smith, A., Webster, L., Taylor, A., & Kearney, N. (2015). Development of a novel remote patient monitoring system: The advanced symptom management system for radiotherapy to improve the symptom experience of patients with lung cancer receiving radiotherapy. Cancer Nursing, 38(2), E37–E47. https://doi.org/10.1097/NCC.0000000000000150
- Marcolino, M. S., Oliveira, J. A. Q., D’Agostino, M., Ribeiro, A. L., Alkmim, M. B. M., & Novillo-Ortiz, D. (2018). The impact of mHealth interventions: Systematic review of systematic reviews. JMIR MHealth and UHealth, 6(1), e23. https://doi.org/10.2196/mhealth.8873
- Marques, M. M., Wright, A. J., Corker, E., Johnston, M., West, R., Hastings, J., Zhang, L., & Michie, S. (2023). The behaviour change technique ontology: Transforming the behaviour change technique taxonomy v1. Wellcome Open Research, 8, 308. https://doi.org/10.12688/wellcomeopenres.19363.1
- Mayer, D. K., Landucci, G., Awoyinka, L., Atwood, A. K., Carmack, C. L., Demark-Wahnefried, W., McTavish, F., & Gustafson, D. H. (2018). SurvivorCHESS to increase physical activity in colon cancer survivors: Can we get them moving? Journal of Cancer Survivorship, 12(1), 82–94. https://doi.org/10.1007/s11764-017-0647-7
- McCarroll, M. L., Armbruster, S., Pohle-Krauza, R. J., Lyzen, A. M., Min, S., Nash, D. W., Roulette, G. D., Andrews, S. J., & von Gruenigen, V. E. (2015). Feasibility of a lifestyle intervention for overweight/obese endometrial and breast cancer survivors using an interactive mobile application. Gynecologic Oncology, 137(3), 508–515. https://doi.org/10.1016/j.ygyno.2014.12.025
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M. P., Cane, J., & Wood, C. E. (2013). The Behavior Change Technique Taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. https://doi.org/10.1007/s12160-013-9486-6
- Nausheen, B., Gidron, Y., Peveler, R., & Moss-Morris, R. (2009). Social support and cancer progression: A systematic review. Journal of Psychosomatic Research, 67(5), 403–415. https://doi.org/10.1016/j.jpsychores.2008.12.012
- Odeh, B., Kayyali, R., Nabhani-Gebara, S., & Philip, N. (2015). Optimizing cancer care through mobile health. Supportive Care in Cancer, 23(7), 2183–2188. https://doi.org/10.1007/s00520-015-2627-7
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, 105906. https://doi.org/10.1016/j.ijsu.2021.105906
- Park, S., Kim, J. Y., Lee, J. C., Kim, H. R., Song, S., Kwon, H., Ji, W., & Choi, C. M. (2019). Mobile phone app–based pulmonary rehabilitation for chemotherapy-treated patients with advanced lung cancer: Pilot study. JMIR MHealth and UHealth, 7(2), e11094. https://doi.org/10.2196/11094
- Pereira-Azevedo, N. M., & Venderbos, L. D. F. (2018). EHealth and mHealth in prostate cancer detection and active surveillance. Translational Andrology and Urology, 7(1), 170–181. https://doi.org/10.21037/tau.2017.12.22
- Pinquart, M., & Duberstein, P. R. (2010). Associations of social networks with cancer mortality: A meta-analysis. Critical Reviews in Oncology/Hematology, 75(2), 122–137. https://doi.org/10.1016/j.critrevonc.2009.06.003
- Poort, H., Ryan, A., MacDougall, K., Malinowski, P., MacDonald, A., Markin, Z., Pirl, W., Greer, J., & Fasciano, K. (2021). Feasibility and acceptability of a mobile phone app intervention for coping with cancer as a young adult: Pilot trial and thematic analysis. Journal of Medical Internet Research, 23(6), e25069. https://doi.org/10.2196/25069
- Putranto, D., & Rochmawati, E. (2020). Mobile applications for managing symptoms of patients with cancer at home: A scoping review. International Journal of Nursing Practice, 26(4), e12842. https://doi.org/10.1111/ijn.12842
- Rincon, E., Monteiro-Guerra, F., Rivera-Romero, O., Dorronzoro-Zubiete, E., Sanchez-Bocanegra, C. L., & Gabarron, E. (2017). Mobile phone apps for quality of life and well-being assessment in breast and prostate cancer patients: Systematic review. JMIR MHealth and UHealth, 5(12), e187. https://doi.org/10.2196/mhealth.8741
- Rini, C., & Dunkel Schetter, C. (2010). The effectiveness of social support attempts in intimate relationships. In K. T. Sullivan & J. Davila (Eds.), Support processes in intimate relationships (pp. 26–68). Oxford University Press.
- Rose, J. H. (1990). Social support and cancer: Adult patients’ desire for support from family, friends, and health professionals. American Journal of Community Psychology, 18(3), 439. https://doi.org/10.1007/BF00938117
- Schwarzer, R., & Knoll, N. (2007). Functional roles of social support within the stress and coping process: A theoretical and empirical overview. International Journal of Psychology, 42(4), 243–252. https://doi.org/10.1080/00207590701396641
- Schwarzer, R., & Knoll, N. (2010). Social support. In J. W. Kaptein & J. Weinman (Eds.), Health psychology (pp. 283–293). Blackwell.
- Schwarzer, R., Knoll, N., & Rieckmann, N. (2004). Social support. In A. Kaptein & J. Weinman (Eds.), Health psychology (pp. 158–181). Blackwell.
- Schwarzer, R., & Leppin, A. (1991). Social support and health: A theoretical and empirical overview. Journal of Social and Personal Relationships, 8(1), 99–127. https://doi.org/10.1177/0265407591081005
- Seeman, T. E. (1996). Social ties and health: The benefits of social integration. Annals of Epidemiology, 6(5), 442–451. https://doi.org/10.1016/S1047-2797(96)00095-6
- Spahrkas, S., Looijmans, A., Sanderman, R., & Hagedoorn, M. (2020). Beating cancer-related fatigue with the Untire mobile app: Protocol for a waiting list randomized controlled trial. JMIR Research Protocols, 9(2), e15969. https://doi.org/10.2196/15969
- Stark, D. P. H., & House, A. (2000). Anxiety in cancer patients. British Journal of Cancer, 83(10), 1261–1267. https://doi.org/10.1054/bjoc.2000.1405
- Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., Boutron, I., Carpenter, J. R., Chan, A.-W., Churchill, R., Deeks, J. J., Hróbjartsson, A., Kirkham, J., Jüni, P., Loke, Y. K., Pigott, T. D., … Higgins, J. P. T. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 4919, 355:i4919. https://doi.org/10.1136/bmj.i4919
- Sterne, J. A., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H.-Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., … Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 4898, 366:l4898. https://doi.org/10.1136/bmj.l4898
- Sundberg, K., Wengström, Y., Blomberg, K., Hälleberg-Nyman, M., Frank, C., & Langius-Eklöf, A. (2017). Early detection and management of symptoms using an interactive smartphone application (Interaktor) during radiotherapy for prostate cancer. Supportive Care in Cancer, 25(7), 2195–2204. https://doi.org/10.1007/s00520-017-3625-8
- Tunin, R., Uziely, B., & Woloski-Wruble, A. C. (2010). First degree relatives of women with breast cancer: Who’s providing information and support and who’d they prefer. Psycho-Oncology, 19(4), 423–430. https://doi.org/10.1002/pon.1596
- Uchino, B. N. (2004). Social support and physical health: Understanding the health consequences of relationships. Yale University Press.
- Uchino, B. N. (2009). Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspectives on Psychological Science, 4(3), 236–255. https://doi.org/10.1111/j.1745-6924.2009.01122.x
- Visser, A., Prins, J., Jansen, L., Radema, S., Schlooz, M., van Dalen, T., & van Laarhoven, H. (2018). Group medical consultations (GMCs) and tablet-based online support group sessions in the follow-up of breast cancer: A multicenter randomized controlled trial. The Breast, 40, 181–188. https://doi.org/10.1016/j.breast.2018.05.012
- Vistad, I., Skorstad, M., Demmelmaier, I., Smastuen, M., Lindemann, K., Wisloff, T., van de Poll-franse, L., & Berntsen, S. (2021). Lifestyle and empowerment techniques in survivorship of gynaecologic oncology (LETSGO study): A study protocol for a multicentre longitudinal interventional study using mobile health technology and biobanking. BMJ OPEN, 11(7), e050930. https://doi.org/10.1136/bmjopen-2021-050930
- Wesley, K., & Fizur, P. (2015). A review of mobile applications to help adolescent and young adult cancer patients. Adolescent Health, Medicine and Therapeutics, 141, 141–148. https://doi.org/10.2147/AHMT.S69209
- World Health Organization. (2022). Cancer fact sheet. https://www.who.int/news-room/fact-sheets/detail/cancer.
- Yang, J., Weng, L., Chen, Z., Cai, H., Lin, X., Hu, Z., Li, N., Lin, B., Zheng, B., Zhuang, Q., Du, B., Zheng, Z., & Liu, M. (2019). Development and testing of a mobile app for pain management among cancer patients discharged from hospital treatment: Randomized controlled trial. JMIR MHealth and UHealth, 7(5), e12542. https://doi.org/10.2196/12542
- Yang, Q., & Van Stee, S. K. (2019). The comparative effectiveness of mobile phone interventions in improving health outcomes: Meta-analytic review. JMIR MHealth and UHealth, 7(4), e11244. https://doi.org/10.2196/11244
- Zhu, J., Ebert, L., Liu, X., & Chan, S. (2017). A mobile application of breast cancer e-support program versus routine care in the treatment of Chinese women with breast cancer undergoing chemotherapy: Study protocol for a randomized controlled trial. BMC Cancer, 17, 291. https://doi.org/10.1186/s12885-017-3276-7
- Zhu, J., Ebert, L., Liu, X., Wei, D., & Chan, S. (2018). Mobile breast cancer e-support program for Chinese women with breast cancer undergoing chemotherapy (Part 2): Multicenter randomized controlled trial. JMIR MHealth and UHealth, 6(4), e104. https://doi.org/10.2196/mhealth.9438