ABSTRACT
This study explored the possibility of a common health-related stigma reduction intervention among people living with HIV, leprosy, schizophrenia and diabetes in Indonesia by assessing their perspectives towards others with the same (within group) and different health conditions (across groups), and willingness to participate in such a program. This mixed-methods study was conducted in West Java, Indonesia between March and June 2018. Eighty participants completed a survey with social distance scale (SDS), while 12 focus group discussion were conducted. Participants with HIV, leprosy and diabetes reported lower within-group SDS scores (4.14 ± 3.65; 4.25 ± 3.95; 7.23 ± 5.31, respectively) while those with schizophrenia reported the highest within-group SDS score (7.76 ± 4.63). Participants with diabetes reported a twofold higher across-group SDS score towards people with the other three health conditions (p < 0.05). The qualitative findings showed that the perception of participants towards one another was shaped by knowledge, understanding and relatedness to the experience of living with health-related stigma. Overall, participants supported the idea of a common stigma reduction intervention for different health conditions, but recommended step-wise implementation of such interventions. Accordingly, this study recommends piloting a common stigma reduction intervention with special focus on fostering understanding, awareness and empathy between people living with different health conditions.
Introduction
Health-related stigma negatively affects the lives of people living with a diversity of health conditions and undermines public health response to curb the burden of these diseases (Stangl et al., Citation2019; Van Brakel, Citation2006; Weiss et al., Citation2006). People with infectious diseases such as HIV and leprosy; mental health conditions like schizophrenia and bipolar disorder; and other non-communicable diseases such as diabetes and cancers are known to be stigmatised because of their health condition (Earnshaw & Kalichman, Citation2013; Fujisawa & Hagiwara, Citation2015; González-Torres et al., Citation2007; Gredig & Bartelsen-Raemy, Citation2017; Peters et al., Citation2013). People living with such stigmatised health conditions often live in the same society, but remain isolated and siloed within their own experiences of stigma, suffering its various social, physical and mental health consequences (Corrigan & Rao, Citation2012; Earnshaw & Kalichman, Citation2013; Rai et al., Citation2020).
The existing health-related stigma reduction responses follow a similar scenario of fragmentation across different health conditions (Heijnders & Van Der Meij, Citation2006; Van Brakel, Citation2006; Weiss et al., Citation2006), while largely disregarding those with other health conditions who co-exist in the same society, and also missing out on their unique experiential knowledge on living with a stigmatised health condition. Studies have shown that while the origin of stigma across such diseases may be different depending on the different disease-specific features, the experiences of stigma and its consequences are largely similar across a variety of health conditions (Rai et al., Citation2020; Rao, Citation2010; Van Brakel, Citation2006). In such a case, there may be prospects for effectively responding to health-related stigma in the society by bringing together people living with different stigmatised health conditions and their collective knowledge and experiences. However, it is first important to evaluate the feasibility of such a response by considering how people living with different stigmatised health conditions perceive each other, and if they are willing to be brought together.
While there has been growing interest and calls towards integrating different disease-specific stigma reduction responses (Stangl et al., Citation2019; Van Brakel, Citation2006; Weiss et al., Citation2006), little research has focused on the perceptions that people living with one health condition hold towards others living with either the same condition or other health conditions. Such perceptions that individuals hold towards each other are important as they reveal both the biases and prejudices, and the understanding and relatedness that they perceive towards one another. These insights are important to assess not only the willingness of individuals living with stigmatised conditions to come together, but also the feasibility and sustainability of a common integrated stigma reduction response. This is particularly valuable and in line with the current focus and call for integration of public health programs and their responses by the year 2030 initiated by the United Nations – sustainable development goals (SDGs) (Nunes et al., Citation2016).
In this regard, this study focused on Indonesia – a low-and-middle-income country currently undergoing epidemiological transition with relatively high prevalence and distribution of both communicable and non-communicable diseases (Boutayeb, Citation2006; Omran, Citation2005; Vos et al., Citation2015). Indonesia has one of the highest burdens of the four stigmatised diseases of our interest in the region of South-East Asia (communicable: HIV and leprosy; non-communicable: schizophrenia and diabetes) (IDF, Citation2020; UNAIDS, Citation2017; Vos et al., Citation2015; WHO, Citation2019). Along with the high burden, these four diseases are also known to be stigmatised in the Indonesian society (Hartini et al., Citation2018; Peters et al., Citation2013; Pujilestari et al., Citation2014; Rai et al., Citation2020; Sianturi et al., Citation2019). Hence, this study aimed to explore the cross-perspectives of individuals living with stigmatised conditions: HIV, leprosy, schizophrenia and diabetes towards people living with the same condition (within group) and those with other stigmatised conditions (across groups) and assess their perspectives on the possibility of a common stigma reduction intervention in Indonesia.
Group identification among stigmatised individuals
The within-group and across-group perception of individuals living with stigmatised health conditions may be dependent on the concept of social and group identification. The social identification theory by Tajfel (Tajfel, Citation1974) postulates that people inherently tend to attach themselves to a group that they feel the closest connection to. People who socially identify strongly towards a group based on a commonly shared trait exhibit a sense of group membership wherein they feel closeness, understanding and empathy towards other members of the group (Tajfel, Citation1974; Van Zomeren et al., Citation2012). Such strong sense of group membership is known to help improve the self-esteem and confidence of individuals (Tajfel et al., Citation1979), reject endorsement of negative stereotypes associated their group (Van Zomeren et al., Citation2012) and support in coping with adversities like stigma (Crabtree et al., Citation2010). Further, studies have also reported that positive group identification and sense of group membership can also motivate stigmatised individuals to come together and fight against social stigma (Crabtree et al., Citation2010; Van Zomeren et al., Citation2012; Van Zomeren et al., Citation2012).
Using these concepts of group identification and membership, this study aims to assess how individuals living with a stigmatised health condition perceive those with the same health condition and those with other health conditions, and their willingness to work together to address health-related stigma.
Methods
Study location and population
The study was conducted in Jakarta and Cirebon, West Java, Indonesia, from March to June 2018. The study population consisted of people with different stigmatised heath conditions – HIV, leprosy, schizophrenia and diabetes. A purposive convenience sampling technique was used to recruit participants through local partners (e.g. non-governmental organisations and community-based organisations working with different disease groups). People younger than 18 years were excluded from the research. There were no specific inclusion criteria for participants with HIV, leprosy and diabetes. However, in case of schizophrenia, only participants who were under medication and either in remission or with controlled symptoms were included in the study to ascertain their active and engaged participation. Participation was voluntary and participants could decide to discontinue any time.
Research design
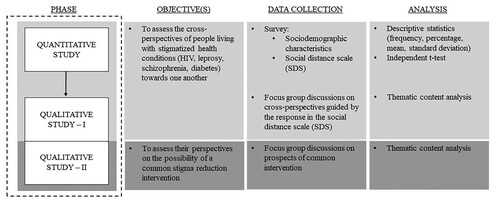
A mixed-methods approach was employed in the study with an explanatory concurrent design (Creswell & Clark, Citation2017) ().
This study consisted of two parts – quantitative and qualitative, conducted concurrently. In order to answer the first part of the research question on exploration of cross-perspectives of people living with the four health conditions, the participants were first asked to fill a survey questionnaire as part of the quantitative study, and then were invited to participate in a focus group discussion (FDG) (qualitative study).
A total of 12 FGDs (3 FGDs per disease group) were conducted. The FGDs were structured into two successive sessions. The first session of FGDs referred to the responses of the participants in the quantitative survey and aimed to not only triangulate, but also explain or elaborate on the quantitative responses/findings. This was followed by a second session of FGDs which focused on answering the second part of the research question and consisted of participants’ discussion on their opinions and willingness to participate in a common stigma reduction intervention. The specific methods used for the quantitative and qualitative phases of the study are described below.
Quantitative phase
For the quantitative phase, Social Distance Scale (SDS) (Bogardus, Citation1933) was used to assess perceived social distance as a measure of perception of persons living with one stigmatised condition towards others living with either the same or different stigmatised condition. The scale was validated in previous studies and translated to the local language, Bahasa Indonesia (Peters et al., Citation2014). SDS includes seven questions representing the following social relationships: renting a room, common place of work, neighbourhood, member of the same social circle, personal job brokering, marriage into one's family and child care. Respondents could indicate on a Likert scale to what extent they would, in the situation presented, accept the person living with either of the four health conditions. The score range was 0–21; 0 indicating the lowest perceived social distance and 21 indicating the highest perceived social distance. Cronbach alpha (α) for the SDS across the conditions ranged from 0.737 to 0.940, which fulfills Nunnaly's (Nunnally, Citation1994) threshold for acceptable reliability coefficient (i.e. α > 0.70).
Qualitative phase
To obtain the qualitative data, FGDs were performed. An FGD guide was developed through multiple consultations with research experts, and relevant stakeholders including representatives from the different disease groups. The first part of the FGD guide outlined the following components: perception towards others with the four health conditions (same and different health conditions); knowledge or familiarity in regards to the four diseases; perceived similarities, differences, and other comparisons of experiences of stigma across different stigmatised health conditions. The second part of the guide inquired the perceptions of respondents on whether people living with different stigmatised health conditions can work together and the stigma associated with different health conditions that exist in the community can be tackled together.
Data collection and analysis
Four research assistants collected data in Bahasa Indonesia under the supervision of the main researcher (SR). They were trained by SSR and II to collect both quantitative and qualitative data. Quantitative data was collected by asking the respondents to complete a survey on sociodemographic information and SDS. Data was analysed using statistical software package SPSS 21. Descriptive analysis (number, frequency, percentage and mean with standard deviation) was used to summarise the characteristics of participants. Within-group and across-group mean SDS scores were compared using independent t-test. Significance level was set at a p-value of <0.05.
The FGDs were recorded electronically, transcribed verbatim, translated to English, and managed with the qualitative software package Atlas.ti. Thematic analysis was used to analyse the data in which the data was iteratively coded and thematically categorised to derive inference. The thematic content analysis processes and emerging codes and categories were discussed in each stage among the co-authors (SSR & EVS) and agreed upon by all authors to ensure the quality and validity of the findings.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Atma Jaya Catholic University, Indonesia (Approval ID: FR-UAJ-26-13/R0).
Results
In this section, we first describe the findings from the quantitative phase on the reported SDS scores from participants with the four health conditions, and then support those inferences with reasoning and explanations offered by the findings from the qualitative phase.
Quantitative findings
Participants characteristics
A total of 89 participants consented to participate in this study, out of which 80 (HIV: 23; leprosy: 16; schizophrenia: 19; diabetes: 22) were included in the final analysis as the remaining 9 had over 80% missing data. The mean age of participants was 41.3 years and most participants had education higher than senior high school (72.2%) and were employed (64.5%). The majority of the participants were Muslims (70.9%), female (50.6%), and had the disease for less than 10 years (69.3%). highlights the participant's characteristics in detail.
Table 1. Participants’ characteristics (N = 80).
Perceived social distance towards different health conditions
presents the participants’ perceived SDS scores towards others living with the four health conditions (within-group and across-group).
Table 2. Perceived SDS scores across four conditions.
Participants with HIV, leprosy and diabetes reported lower within-group SDS scores indicating a closer proximity and less stigma towards people from the same group, whereas those with schizophrenia reported the highest SDS score towards others living with schizophrenia.
In regards to perceived social distance towards other groups (), participants with diabetes reported higher mean SDS scores (across-group) towards all three other conditions compared to within-group SDS score. Participants with HIV reported the highest SDS score towards people affected by schizophrenia whereas participants with leprosy reported higher SDS score towards people with HIV. Those with schizophrenia reported the lowest SDS score towards people with diabetes.
Comparison of differences in SDS scores across different conditions
shows the comparison of within-group SDS scores of each of the four disease groups with their reported across-group SDS scores towards other groups. There were significant differences in the perceived SDS score of participants with diabetes towards the other three groups (p < 0.05) in comparison to the within-group SDS score. This indicated that participants from the diabetes group perceived higher social distance towards people from the other three groups. Among participants with HIV, the perceived social distance towards those with schizophrenia was significantly higher (p < 0.05) when compared to perceived social distance others with HIV (within-group).
Table 3. Comparison between within-group and across-group SDS scores.
Qualitative findings
Participants characteristics
A total of 12 FGDs (3 FG in each disease group) were conducted with 60 participants who had also previous answered the quantitative survey (HIV: 16; leprosy: 15; schizophrenia: 16; diabetes: 13). The proportion of male and female were similar (50.6% female). The mean age of the participants were 41.1 years, with most having lived with their health condition for less than 10 years (69.3%). The majority of the participants were Muslim (70.1%), employed (66.2%) and had education higher than senior high school level (72.7%).
Perceptions towards people with the same health condition (within-group perceptions)
In line with the findings from the quantitative study, participants with HIV, leprosy and diabetes described less hesitation and more willingness to socially interact with others with the same health condition. They described feeling empathetic towards them. They reported how the feeling of empathy came from understanding the adversities associated with the disease through their own experience of living with the disease. Those with HIV and leprosy further explained how they could ‘relate’ to others with the same condition on the basis of shame and stigma they experience in their daily lives.
They also talked about how having the same disease united them and fostered feelings of brotherhood or being in the same group. One participant with diabetes noted this feeling and elaborated why she felt closer to other people with diabetes:
Because I have diabetes, I feel more comfortable with other people as me [those with diabetes]. I feel like we are part of a family. We share similar experiences [of living with diabetes]. (Female, Diabetes)
Participants with schizophrenia also reported feeling empathetic towards others with the disease. They expressed how difficult it was to live with the disease, and understood what others with the disease had to go through. They explained how society perceived them as ‘abnormal’, which they found degrading and dehumanising.
However, when asked about their responses to the SDS, participants with schizophrenia reported giving higher scores to schizophrenia. They explained that just like them, others with schizophrenia are at risk of relapse if they do not adhere to their medication and treatment. They talked about how relapse is scary and dangerous, because they can lose control of themselves, hallucinate, and even show aggressive behaviour. This discouraged them from rating schizophrenia with lower SDS score as compared to other disease groups who could still be ‘mentally normal’ and conform to the societal rules.
Perceptions towards people with different health conditions (across-group perceptions)
Contrary to the findings from the quantitative study, all participants during the FGDs reported of having feelings of empathy towards other disease groups. However, there were notable differences in regards to how they perceived other diseases and people who had them. This was based on the knowledge, perception, and attitude (KPA) of the participants with regards to the different health conditions and people affected by them.
Prior knowledge of the disease was reported to shape people's perception of how they look at other disease groups. Participants with leprosy and diabetes reported the highest social distance scores towards people with HIV in the survey, which some described was because they believed HIV to be a very infectious disease, with less knowledge of how it is passed. One person with leprosy said:
HIV is contagious, and there is no cure for it … so it is scary. (Male, Leprosy)
However, to some who were aware of HIV and the pathways of transmission, they felt less distance with HIV:
With HIV, I learned that it can't be transmitted from shaking hands or touching. So socially, I won't distance myself from them. The signs [advertisements] about how the disease can be transmitted are everywhere. So, we don't have to be afraid. (Male, Leprosy)
Participants with HIV, leprosy and diabetes described feeling empathy towards those with schizophrenia based on the adversities they have to face as a result of their health condition. However, they also talked about how the lack of enough knowledge and understanding coupled with the prevalent negative stereotypes associated with the disease shaped their perception towards people with schizophrenia, which in turn incited feelings of fear towards them. Participants talked about the stereotypes in the society on how people with schizophrenia are considered ‘crazy’ and ‘aggressive’, and that they suspected those with schizophrenia would not be able to control such behaviour. A few people also mentioned superstitions about people with schizophrenia that they are possessed by ‘evil spirits’ that can also harm others.
Further, participants with HIV described their rationale on why they gave higher SDS scores to people with schizophrenia based on the misinformation and/or lack of better understanding of the disease. One participant with HIV described how lack of enough understanding affected his view of the disease:
I don't understand the disease [schizophrenia]. I'll empathize with them, but I'm not sure if I would want to interact with them because I only have a little clue. (Male, HIV)
Consistent with the quantitative finding on how people with diabetes reported higher social distance scores across-groups, the FGDs found that despite the reported empathy towards other groups, people with diabetes preferred to distance themselves from others. The respondents with diabetes reported perceiving little to no stigma, because they considered diabetes to be harmless compared to other diseases. They considered their condition ‘non-contagious’ compared to HIV and leprosy, and ‘mentally sound’ compared to schizophrenia. This sense of acceptance and endorsement of one's condition as normal was found to then contrast with their perspectives towards others who they considered diseased and dangerous.
There is no problem [with having diabetes] … I don't feel embarrassed at all. I have diabetes but it's not an infectious disease or a mental illness. I don't put anyone in danger … so why should we [people living with diabetes] be ashamed? (Female, Diabetes)
People with other diseases seemed to agree too that diabetes was a common and harmless condition that did not require social distancing.
Possibility of a common stigma reduction intervention
Participants reacted positively when asked about the idea of bringing people with different health conditions together for a common stigma reduction intervention. They largely supported the idea of a common program that would bring together and involve people from all four disease groups. They discussed their thoughts on this topic in terms of utility, feasibility, and conditions/pre-requisites.
In regards to utility, they reported positively that such a united response was ‘interesting’ and could be ‘helpful’ to all those involved. One participant with leprosy talked about how despite the differences, people with different health conditions strive for similar needs, and coming together can help serve all:
Just like those who have schizophrenia or HIV - who have their own special needs, strengths and weaknesses – us with leprosy also have our own needs and experiences. However, we can focus on our similarities to walk and work together, and to accomplish things that serve us all. (Male, Leprosy)
Participants were also positive about the feasibility of such an idea to bring people together. Some also talked about how they were already involved in similar efforts where people from different walks of life were working together for a common cause. One participant with HIV talked about being involved in such an inter-group alliance and expressed openness to be involved in more diverse collaborations:
We [people living with HIV] are too absorbed and comfortable in our social circle. That is why we need to go out … we need to learn and share across different circles. Right now, we are partnering with women who have disabilities, maybe there is a chance we will partner up with those who have schizophrenia, leprosy. We need to diversify and collaborate with people - even beyond different health conditions – like affiliating with migrant workers. We are all marginalized groups in the same community … we fight for the same thing. We need to understand this. (Female, HIV)
Participants also discussed the conditions and requisites to having a common stigma reduction intervention. While most participants talked about being open to and supportive of such an initiative, a few participants talked about how it would be important to be cautious when deciding which groups to bring together at the same time. Participants with HIV talked about how diabetes was a common disease, and that those with diabetes might further stigmatise or disclose the identity of a person with HIV. Participants with HIV, leprosy and diabetes also expressed concern in regards to those with schizophrenia, specifically on their ability to participate in such a cause. Even though such concerns were raised regarding schizophrenia, participants largely supported the idea of coming together depending on how ‘in-control’ an individual is of him/herself and open towards others.
Participants stressed that in order to implement a common intervention to address health-related stigma associated with these diseases, it would be important to focus on the planning and designing of the intervention and carry out such a program in a stepwise manner: not to immediately include participants from all four groups but start from two or three, at the same time fostering awareness and understanding about the different diseases and lived experiences among the involved participants. One participant with HIV said:
It is important to plan and design [the intervention] well. It is also important to make sure different groups are educated about each other well. Once everybody knows about each other then it is easy to build trust and work together. So, the intervention depends on socialization between the groups. (Male, HIV)
Discussion
This mixed-method study explored the possibility of a common stigma reduction intervention among people living with HIV, leprosy, schizophrenia and diabetes in Indonesia by assessing their perceptions towards others with the same condition (within group) and different stigmatised health conditions (across group), and willingness to participate in such a venture. This study found that the perception of people living with stigmatised health conditions towards one another was driven by knowledge, understanding and relatedness to the diseases and experience of living with stigma. Overall, the participants supported the idea of a common stigma reduction intervention across the health conditions. The main findings of this study are discussed below.
Within-group empathy guided by relatedness
This study found that people living with HIV, leprosy and diabetes were generally empathetic towards others with the same health condition. The feeling of empathy came from understanding the adversities associated with the disease that the person himself/herself experienced, and the awareness and the ability to relate to what others with the health condition may be going through. Studies have shown that stigmatised individuals show connection and interrelatedness towards others with the same disease and identify themselves as a part of a group, demonstrating empathy and support towards other group members (Crabtree et al., Citation2010; Latner et al., Citation2008). Since most of the participants in this study were recruited from community-based organisations and were most likely affiliated with peer-support groups, there are possibilities that they already had a well-developed identity as a part of a stigmatised group wherein they felt supported and also provided support for others.
Within-group biases among people living with schizophrenia
While in the FGDs participants with schizophrenia expressed feelings of empathy towards others with the same condition, they reported the highest perceived within-group social distance in the SDS. They attributed this decision to the risk of relapse and mental/behavioural instability among people living with schizophrenia, and agreed to the socially held beliefs that people with the disease can be aggressive and a possible threat in the society. This indicates not only the existence of biases towards others with schizophrenia, but also the presence of self-stigma as a result of participants’ endorsement of negative stereotypes and norms present in the Indonesian society in regards to mental illnesses.
Other studies have also shown how in Indonesia, people living with mental illnesses like schizophrenia experience self-stigma in the form of shame, self-blame and guilt because of their own experience of psychosis which is common among those with active schizophrenia or who have relapsed (Subandi et al., Citation2020; Subandi & Good, Citation2018), and internalisation of the socially held beliefs and stereotypes (Hartini et al., Citation2018; Rai et al., Citation2020). Watson et al. (Citation2007) found that such endorsement of the negative stereotypes and biases related to one's disease not only affects the self-esteem of individuals with mental illness, but also hampers their positive identification with the group of persons with mental illnesses. This absence of group identification may be the reason why people with schizophrenia reported higher social distance scores towards others with the same disease.
Role of knowledge and social stereotypes in moderating perception and attitude
While the within-group perceptions were driven more by relatedness and understanding of the experiences of living with the health condition, knowledge and prevalent social stereotypes related to the diseases were the main drivers of perception and attitude in regards to across-group comparisons. Participants with all health conditions reported lower social distance towards the diabetes group, which they attributed to knowing that diabetes is a ‘common’ and ‘manageable’ condition. A study by Soewondo et al. (Soewondo et al., Citation2013) reported this very idea of how the higher prevalence and commonality of diabetes in the community has normalised its existence in many Indonesian communities. In regards to the perceptions among those with diabetes, due to the less stigmatising status of this condition, people with diabetes seemed to feel more normal and privileged. They also separated themselves from others with HIV, leprosy and schizophrenia as evident from the twofold higher SDS scores they reported for other groups. However, during the FGDs, they described having empathy and compassion towards people with HIV, schizophrenia and leprosy, and were well aware of the intricacies of having those diseases. Studies that have explored the development of social identity in individuals have shown that besides empathy, common experience of stigma and discrimination and the level of interrelatedness to those experiences are paramount in improving not only intergroup perception, but also building common group identity between members of the same group (Cortland et al., Citation2017; Crabtree et al., Citation2010; Gaertner et al., Citation1993). Participants with diabetes, though empathetic, lacked such understanding and relatedness towards stigma experiences of other groups as they reported experiencing little or no stigma themselves. This may have been the reason why even though they expressed empathy, they reported higher social distance towards the other groups.
Participants with HIV, leprosy and diabetes, while empathetic towards those with schizophrenia, also expressed lack of enough knowledge and understanding and resultant fear in regards to the disease. It is well known that people with mental health disorders experience social stigma and discrimination everywhere in the world (Henderson et al., Citation2013; Thornicroft et al., Citation2016). In Indonesia, prejudices and misconceptions about schizophrenia are embedded in the local culture where people consider schizophrenics as crazy and possessed by evil spirits (Minas & Diatri, Citation2008; Rai et al., Citation2020). Further, the negative stereotypes related to the aggressive and mentally unstable nature of the disease is fuelled by misinformation and lack of enough knowledge on the disease (Hartini et al., Citation2018).
However, in regards to HIV and leprosy, participants were more aware of the diseases, and their mode of transmission and treatment. This was attributed to participants being receptive and empathetic towards people with these two health conditions. Several nation-wide health awareness campaigns have been implemented across Indonesia aimed to raise awareness on HIV and leprosy (Ibrahim et al., Citation2010; Rachmani et al., Citation2013). Thus an increasing number of people now know about HIV and leprosy in Indonesia, and this situation may have been reflected in the findings of this study.
Implications for a common stigma reduction intervention
This study found that people living with stigmatised health conditions saw value in coming together for a common cause, and expressed willingness to participate in a common stigma reduction intervention. They also stressed on the importance of proper planning and designing of such initiative, considering the level of knowledge and awareness of prospective participants on the different diseases. It was also proposed that such interventions be implemented in a stepwise manner, ensuring a safe and healthy environment for all participants.
Based on the findings of this study, a pilot intervention is recommended among chosen groups of health conditions whereby mutual understanding and cooperation is fostered. In this regard, it may also be beneficial to follow a participatory approach/process such as interactive learning and action (ILA) that focuses on trust building among different groups and stakeholders and incorporates their values and experiential knowledge into the paradigm (Betten et al., Citation2013). It is recommended to incorporate additional components into the intervention such as disease-specific health education and awareness, and platform for sharing personal experiences and testimonies between people with different health conditions to highlight the commonalities between them (e.g. similarities in experiences of stigma, clinical management, long-term treatment etc.), that can further help foster mutual understanding and empathy among and between the groups. Such programs can help transform perceptions of groups from ‘us Vs them’ to ‘we’, and develop positive ingroup identity (Gaertner et al., Citation1993). Finally, considering the contextual nature of stigma and its variance across different geographical locations and cultures (Stangl et al., Citation2019; Van Brakel, Citation2006; Weiss et al., Citation2006), it is recommended to take into account the local context and cultural beliefs while designing integrated stigma reduction programs in Indonesia and elsewhere.
Special focus on reducing self-stigma and building self-esteem and positive group identity is also warranted for people with mental health conditions like schizophrenia, who perceive higher self-stigma and biases towards others with the same condition. In this study all participants with schizophrenia were under medication where adverse symptoms such as hallucinations and psychosis were under control, but they feared of possible relapse. Studies have shown that with long-term adherence to medication and psychosocial support and care, people with schizophrenia can reach a stage of recovery whereby psychological functioning (hope, self-acceptance, de-stigmatisation, empowerment), cognition and quality of life of an individual is significantly improved (Liberman & Kopelowicz, Citation2005; Warner, Citation2009). It is therefore important in such a context to involve people with schizophrenia currently in remission into programs like mutual-help groups or peer-support groups that help build positive group identity, empower them and lead them to the road of recovery (Crabtree et al., Citation2010; Liberman & Kopelowicz, Citation2005).
The overall study findings show promise of a common stigma reduction intervention wherein people with different stigmatised health conditions can come together and share their experiences, knowledge and successful strategies to manage stigma. Further, the findings also show prospects of programmatic integration across different disease groups in which their individual efforts, resources and knowledge can be put together for a stronger public health response.
Strengths and limitations
There have, to our knowledge, not been previous studies describing the perceptions that people from different stigmatised groups have towards each other, and this study is one of the first which included participants from four different disease groups simultaneously. By doing this research, it was feasible to understand people's perspectives regarding different conditions, and how a person's own knowledge, understanding and relatedness of the disease and the experience of living with the disease might shape the perception towards another stigmatised person. However, there are limitations to this study that need to be taken into consideration. First, the small sample size might have affected the results of the quantitative analysis. Because of the low sample size and high variance of scores between the different groups, a distinct cut-off point could not be established to further improve the inference from the SDS. Relative comparisons were thus used to infer the results of SDS. However, this issue was addressed by the mixed-methods design of the study where the qualitative findings largely supported and validated the quantitative findings. Second, the convenient sampling which was used to select the participants might have skewed the results as the participants were mostly recruited through community-based organisations and peer support groups. Although participants of the FGDs often knew each other, the collected opinions were diverse and were valuable for the research. Third, this study did not address the variance in regards to individual identities and characteristics that exist within the different health conditions (e.g. people with leprosy with and without disability; different sub-population with HIV – injecting drug users, sex worker, sexual minorities, etc.). Such differences could affect the perceptions of those with other stigmatised health conditions. Hence, it is recommended that such differences be taken into consideration while designing future collective stigma reduction strategies. Lastly, the qualitative results might be skewed due to social desirability bias. To reduce the effect of such bias, the researchers asked additional questions on the same topic to ascertain the consistency of response.
Conclusion
The findings of this study not only highlight the possibility of a common and collective response to stigma but also to the prospects of wider integration across different health conditions for stronger public health response. The study findings recommend piloting a common stigma reduction intervention to assess the actual feasibility of such a response with special focus on fostering understanding, awareness and empathy between people living with different health conditions.
Author contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by SSR. Data analysis was performed by SSR and EVS. The first draft of the manuscript was written by SSR and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Acknowledgments
We would like to thank Ms. Annisa Ika Putri for her support in data collection, Ms. Altana Mikhakhanova for help in data analysis, and Mr. Durwin Lynch for his review and suggestions on the final draft of this manuscript. We sincerely thank all participants, research assistants, resources persons, community leaders and CBOs for their contribution in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author [SSR], upon reasonable request.
Additional information
Funding
References
- Betten, A. W., Roelofsen, A., & Broerse, J. E. (2013). Interactive learning and action: Realizing the promise of synthetic biology for global health. Systems and Synthetic Biology, 7(3), 127–138. https://doi.org/https://doi.org/10.1007/s11693-013-9113-7
- Bogardus, E. S. (1933). A social distance scale. Sociology & Social Research, 17(1), 265–271.
- Boutayeb, A. (2006). The double burden of communicable and non-communicable diseases in developing countries. Transactions of the Royal Society of Tropical Medicine and Hygiene, 100(3), 191–199. https://doi.org/https://doi.org/10.1016/j.trstmh.2005.07.021
- Corrigan, P. W., & Rao, D. (2012). On the self-stigma of mental illness: Stages, disclosure, and strategies for change. The Canadian Journal of Psychiatry, 57(8), 464–469. https://doi.org/https://doi.org/10.1177/070674371205700804
- Cortland, C. I., Craig, M. A., Shapiro, J. R., Richeson, J. A., Neel, R., & Goldstein, N. J. (2017). Solidarity through shared disadvantage: Highlighting shared experiences of discrimination improves relations between stigmatized groups. Journal of Personality and Social Psychology, 113(4), 547. https://doi.org/https://doi.org/10.1037/pspi0000100
- Crabtree, J. W., Haslam, S. A., Postmes, T., & Haslam, C. (2010). Mental health support groups, stigma, and self-esteem: Positive and negative implications of group identification. Journal of Social Issues, 66(3), 553–569. https://doi.org/https://doi.org/10.1111/j.1540-4560.2010.01662.x
- Creswell, J. W., & Clark, V. L. P. (2017). Designing and conducting mixed methods research. Sage Publications.
- Earnshaw, V. A., & Kalichman, S. C. (2013). Stigma experienced by people living with HIV/AIDS. In P. Liamputtong (Ed.), Stigma, discrimination and living with HIV/AIDS (pp. 23–38). Springer.
- Fujisawa, D., & Hagiwara, N. (2015). Cancer stigma and its health consequences. Current Breast Cancer Reports, 7(3), 143–150. https://doi.org/https://doi.org/10.1007/s12609-015-0185-0
- Gaertner, S. L., Dovidio, J. F., Anastasio, P. A., Bachman, B. A., & Rust, M. C. (1993). The common ingroup identity model: Recategorization and the reduction of intergroup bias. European Review of Social Psychology, 4(1), 1–26. https://doi.org/https://doi.org/10.1080/14792779343000004
- González-Torres, M. A., Oraa, R., Arístegui, M., Fernández-Rivas, A., & Guimon, J. (2007). Stigma and discrimination towards people with schizophrenia and their family members. Social Psychiatry and Psychiatric Epidemiology, 42(1), 14–23. https://doi.org/https://doi.org/10.1007/s00127-006-0126-3
- Gredig, D., & Bartelsen-Raemy, A. (2017). Diabetes-related stigma affects the quality of life of people living with diabetes mellitus in Switzerland: Implications for healthcare providers. Health and Social Care in the Community, 25(5), 1620–1633. https://doi.org/https://doi.org/10.1111/hsc.12376
- Hartini, N., Fardana, N. A., Ariana, A. D., & Wardana, N. D. (2018). Stigma toward people with mental health problems in Indonesia. Psychology Research and Behavior Management, 11, 535. https://doi.org/https://doi.org/10.2147/PRBM.S175251
- Heijnders, M., & Van Der Meij, S. (2006). The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychology, Health and Medicine, 11(3), 353–363. https://doi.org/https://doi.org/10.1080/13548500600595327
- Henderson, C., Evans-Lacko, S., & Thornicroft, G. (2013). Mental illness stigma, help seeking, and public health programs. American Journal of Public Health, 103(5), 777–780. https://doi.org/https://doi.org/10.2105/AJPH.2012.301056
- Ibrahim, K., Songwathana, P., Boonyasopun, U., & Francis, K. (2010). The HIV/AIDS epidemic in Indonesia: Does primary health care as a prevention and intervention strategy work? International Journal of Nursing Practice, 16(2), 87–91. https://doi.org/https://doi.org/10.1111/j.1440-172X.2010.01816.x
- IDF. (2020). Diabetes in Indonesia. International Diabetes Federation. Retrieved June 26, 2020, from https://idf.org/our-network/regions-members/western-pacific/members/104-indonesia.html
- Latner, J. D., O'Brien, K. S., Durso, L. E., Brinkman, L. A., & MacDonald, T. (2008). Weighing obesity stigma: The relative strength of different forms of bias. International Journal of Obesity, 32(7), 1145–1152. https://doi.org/https://doi.org/10.1038/ijo.2008.53
- Liberman, R. P., & Kopelowicz, A. (2005). Recovery from schizophrenia: A concept in search of research. Psychiatric Services, 56(6), 735–742. https://doi.org/https://doi.org/10.1176/appi.ps.56.6.735
- Minas, H., & Diatri, H. (2008). Pasung: Physical restraint and confinement of the mentally ill in the community. International Journal of Mental Health Systems, 2(1), 8. https://doi.org/https://doi.org/10.1186/1752-4458-2-8
- Nunes, A. R., Lee, K., & O'Riordan, T. (2016). The importance of an integrating framework for achieving the sustainable development goals: The example of health and well-being. BMJ Global Health, 1(3), e000068. https://doi.org/https://doi.org/10.1136/bmjgh-2016-000068
- Nunnally, J. C. (1994). Psychometric theory 3E. Tata McGraw-Hill Education.
- Omran, A. R. (2005). The epidemiologic transition: A theory of the epidemiology of population change. The Milbank Quarterly, 83(4), 731–757. https://doi.org/https://doi.org/10.1111/j.1468-0009.2005.00398.x
- Peters, R. M., Dadun, L., Miranda-Galarza, M., van Brakel, B., Zweekhorst, W. H., Damayanti, M. B., Seda, R., Bunders, F. S., & & Irwanto, J. F. (2013). The meaning of leprosy and everyday experiences: An exploration in cirebon, Indonesia. Journal of Tropical Medicine, 2013, 507034. https://doi.org/https://doi.org/10.1155/2013/507034
- Peters, R. M., Van Brakel, W. H., Zweekhorst, M. B., Damayanti, R., & Bunders, J. F. (2014). The cultural validation of two scales to assess social stigma in leprosy. PLoS Neglected Tropical Diseases, 8(11), e3274. https://doi.org/https://doi.org/10.1371/journal.pntd.0003274
- Pujilestari, C. U., Nawi Ng, M. H., & Eriksson, M. (2014). “It is not possible for me to have diabetes”–community perceptions on diabetes and Its risk Factors in Rural Purworejo District, Central Java, Indonesia. Global Journal of Health Science, 6(5), 204. https://doi.org/https://doi.org/10.5539/gjhs.v6n5p204
- Rachmani, E., Hsu, C. Y., & Kurniadi, A. (2013). How health information system could help the leprosy control program in Indonesia? International Conference on Instrumentation, Communications, Information Technology and Biomedical Engineering, 2013, 16–20. https://doi.org/https://doi.org/10.1109/ICICI-BME.2013.6698457
- Rai, S. S., Irwanto, I., Peters, R. M., Syurina, E. V., Putri, A. I., Mikhakhanova, A., Naniche, D., & Zweekhorst, M. B. (2020). Qualitative exploration of experiences and consequences of health-related stigma among Indonesians with HIV, leprosy, schizophrenia and diabetes. Kesmas: National Public Health Journal, 15(1), 7–16. https://doi.org/https://doi.org/10.21109/kesmas.v15i1.3306
- Rao, P. (2010). Study on differences and similarities in the concept and origin of leprosy stigma in relation to other health-related stigma. Indian Journal of Leprosy, 82(3), 117–121.
- Sianturi, E., Perwitasari, D., Islam, M. A., & Taxis, K. (2019). The association between ethnicity, stigma, beliefs about medicines and adherence in people living with HIV in a rural area in Indonesia. BMC Public Health, 19(1), 55. https://doi.org/https://doi.org/10.1186/s12889-019-6392-2
- Soewondo, P., Ferrario, A., & Tahapary, D. L. (2013). Challenges in diabetes management in Indonesia: A literature review. Globalization and Health, 9(1), 63. https://doi.org/https://doi.org/10.1186/1744-8603-9-63
- Stangl, A. L., Earnshaw, V. A., Logie, C. H., van Brakel, W. L. C. S., Barre, I., & Dovidio, J. F. (2019). The health stigma and discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine, 17(1), 31. https://doi.org/https://doi.org/10.1186/s12916-019-1271-3
- Subandi, M., & Good, B. J. (2018). Shame as a cultural index of illness and recovery from psychotic illness in Java. Asian Journal of Psychiatry, 34, 33–37. https://doi.org/https://doi.org/10.1016/j.ajp.2018.04.005
- Subandi, M., Praptomojati, A., Marchira, C. R., DelVecchio Good, M.-J., & Good, B. J. (2020). Cultural explanations of psychotic illness and care-seeking of family caregivers in Java, Indonesia. Transcultural Psychiatry, https://doi.org/https://doi.org/10.1177/1363461520916290
- Tajfel, H. (1974). Social identity and intergroup behaviour. Information (International Social Science Council), 13(2), 65–93.
- Tajfel, H., Turner, J. C., Austin, W. G., & Worchel, S. (1979). An integrative theory of intergroup conflict. In M.J. Hatch & M. Schultz (Eds.), Organizational Identity: A Reader (pp. 56-65). Oxford University Press.
- Thornicroft, G., Mehta, N., Clement, S., Evans-Lacko, S., Doherty, M., Rose, D., Koschorke, M., Shidhaye, R., O'Reilly, C., & Henderson, C. (2016). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet, 387(10023), 1123–1132. https://doi.org/https://doi.org/10.1016/S0140-6736(15)00298-6
- UNAIDS. (2017). Indonesia. Retrieved February 6, 2019, from http://www.unaids.org/en/regionscountries/countries/indonesia
- Van Brakel, W. H. (2006). Measuring health-related stigma—A literature review. Psychology, Health & Medicine, 11(3), 307–334. https://doi.org/https://doi.org/10.1080/13548500600595160
- Van Zomeren, M., Leach, C. W., & Spears, R. (2012a). Protesters as “passionate economists” a dynamic dual pathway model of approach coping with collective disadvantage. Personality and Social Psychology Review, 16(2), 180–199. https://doi.org/https://doi.org/10.1177/1088868311430835
- Van Zomeren, M., Postmes, T., & Spears, R. (2012b). On conviction's collective consequences: Integrating moral conviction with the social identity model of collective action. British Journal of Social Psychology, 51(1), 52–71. https://doi.org/https://doi.org/10.1111/j.2044-8309.2010.02000.x
- Vos, T., Barber, R. M., Bell, B., Bertozzi-Villa, A., Biryukov, S., Bolliger, I., Charlson, F., Davis, A., Degenhardt, L., & Dicker, D. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global burden of disease study 2013. The Lancet, 386(9995), 743–800. https://doi.org/https://doi.org/10.1016/S0140-6736(15)60692-4
- Warner, R. (2009). Recovery from schizophrenia and the recovery model. Current Opinion in Psychiatry, 22(4), 374–380. https://doi.org/https://doi.org/10.1097/YCO.0b013e32832c920b
- Watson, A. C., Corrigan, P., Larson, J. E., & Sells, M. (2007). Self-stigma in people with mental illness. Schizophrenia Bulletin, 33(6), 1312–1318. https://doi.org/https://doi.org/10.1093/schbul/sbl076
- Weiss, M. G., Ramakrishna, J., & Somma, D. (2006). Health-related stigma: Rethinking concepts and interventions. Psychology, Health & Medicine, 11(3), 277–287. https://doi.org/https://doi.org/10.1080/13548500600595053
- WHO. (2019). Global leprosy update, 2018: Moving towards a leprosy-free world. Weekly Epidemiological Record, 94(35/36), 389–412.