ABSTRACT
Hypertension disproportionately affects people living in African countries, where there are many challenges to appropriate diagnosis and treatment, and many people with hypertension utilise traditional healers as their primary source of healthcare. In this study, we sought to understand factors driving healer utilisation among people with hypertension. We conducted 52 semi-structured interviews with traditional healers, patients and healthcare providers in the Mwanza region of Tanzania. We used the Andersen model of healthcare utilisation to organise our findings on factors driving utilisation of traditional healers for hypertension care. Traditional healers routinely provide care to hypertensive patients and are a critical component of the healthcare landscape. However, healers also operate independently of the biomedical healthcare system, and biomedical providers may hold negative perceptions of healers. Further, healers were described as preferential by patients due to the convenient locations of their practices and perceived improvement of hypertension symptoms with traditional treatment. Finally, healers expressed a desire for more formal collaboration with biomedicine to improve patient care. Our findings may guide future interventions in Tanzanian communities and elsewhere where traditional healers may act as partners to allopathic providers and patients in the continuum of hypertension care.
Introduction
Hypertension is a major risk factor for early onset cardiovascular disease and death (Chow et al., Citation2013), accounting for over 200 million disability-adjusted life years, with nearly 1 billion adults living with hypertension (Forouzanfar et al., Citation2017). As the prevalence of hypertension increases globally, the burden of this chronic disease disproportionately impacts the poor (Global Burden of Diseases, Citation2015). Lower socioeconomic status has been shown to correlate with poor outpatient management of hypertension and higher rates of hypertensive crisis (Ferdinand et al., Citation2017). Over 75% or cardiovascular deaths globally occur in low and middle-income countries (LMICs) (Schutte et al., Citation2021), where less than half of adults are aware of their diagnosis and less than 10% have controlled hypertension (Chow et al., Citation2013).
In Tanzania, hypertensive crisis is the second leading cause of hospital admissions and deaths after HIV (Peck et al., Citation2013). It is estimated that 16% of Tanzanian adults are living with hypertension, yet as many as 65% of patients are unaware of their diagnosis (Kavishe et al., Citation2015). Structural challenges to hypertension prevention and control include poverty, limited facilities and appropriate diagnostic and treatment resources, and an insufficient number of healthcare providers (Seedat, Citation2015; Vedanthan et al., Citation2015). Consequently, engagement with the biomedical healthcare system is suboptimal. One study found that in a 12-month period, only 34% of hypertensive patients sought clinic-based follow-up care (Bovet et al., Citation2008). Of the 34% who returned for follow-up care, less than 10% of patients were taking prescribed antihypertensive medication (Bovet et al., Citation2008)
Outside of formal biomedical facilities, patients in sub-Saharan Africa often seek care from informal healthcare providers, such as traditional healers (TH). Across sub-Saharan Africa, many rely on TH as their primary source of healthcare (Kim et al., Citation2020; Oyebode et al., Citation2016). In Tanzania, up to 80% of the populace utilise traditional medicine (World Health Organization, Citation2019). For hypertension treatment, specifically, previous studies have reported that about 40% of hypertensive patients concurrently receive care from both TH and allopathic providers (Azizah et al., Citation2021; Hughes et al., Citation2013; A. C. Liwa et al., Citation2014). One study conducted in Mwanza, Tanzania found that 25% of patients hospitalised with hypertension-related diseases used traditional medicine (A. Liwa et al., Citation2017). Another study conducted across 12 African countries found that users of TH had poor treatment adherence, and greater odds of severe hypertension and hypertension-related complications (Lassale et al., Citation2022). These studies suggest that TH are an essential component of the healthcare ecosystem in Tanzania and may play a role in shaping their hypertensive clients’ healthcare-seeking trajectory.
Prior studies indicate that patients use TH instead of biomedical facilities because of perceived lower costs of services, ease of access, perceived futility of allopathic medicine and provision of psychosocial support (Kolling et al., Citation2010; Marten, Citation2022; Nnko et al., Citation2015; Oke & Bandele, Citation2004). There are only a few studies considering patients with hypertension using TH specifically. Studies conducted in Nigeria, Zambia, Cameroon and South Africa suggest that TH treat hypertensive clients and have some basic knowledge about symptoms and risk factors for hypertension (Frimpong & Nlooto, Citation2019; Goma et al., Citation2016; Meli et al., Citation2009; Osamor & Owumi, Citation2010). However, there is a dearth of information indicating why patients with hypertension visit TH, or how TH manage their clients with hypertension or display symptoms consistent with hypertensive emergency. These gaps in knowledge limit our ability to improve hypertension outcomes among adults in sub-Saharan Africa who may utilise traditional medicines exclusively or in conjunction with formal biomedical services.
Because little is known on this topic, we conducted an exploratory, qualitative study to capture the perspectives of stakeholders involved in the continuum of hypertension care in our study site of Mwanza, Tanzania. The primary aim of this study was to characterise TH knowledge and practices surrounding hypertension via in-depth qualitative interviews with a sample of traditional healers, clinical providers and adults with hypertension. In this paper, we describe the findings of our study and discuss the implications this may have on future public health interventions for hypertension management and control in similar LMIC contexts.
Methods
Research design and setting
The study region of Mwanza, Tanzania is a port city on Lake Victoria in Northwestern Tanzania and is the second largest city in Tanzania. About 60% of Tanzanians identify as Christians, followed by 35% Muslim. In the study region, as across sub-Saharan Africa, there is an extensive history of practice and utilisation of traditional medicine. TH are ubiquitous in both urban and rural communities. Tanzanian TH are governed by the Tanzanian Traditional and Alternative Medicines Act of 2002 (CitationUnited Republic of Tanzania, n.d.). This law relegates traditional healers as practitioners under the Ministry of Health, and under this law all traditional healers must formally register with the Traditional and Alternative Health Practice Council to legally provide care to clients.
The study also involved clinical providers and patients with hypertension from the outpatient medical clinics of three hospital facilities in Mwanza City, Tanzania. The three study sites all together serve approximately 3000 adults living with hypertension annually. All clinics were following the national guidelines for treating hypertension (Ministry & Health, Citation2018). Patients pay for services through a combination of insurance, government subsidy and out-of-pocket contributions.
Sampling and recruitment
Purposive sampling was used to identify practicing traditional healers registered under the Traditional and Alternative Medicine Council in Mwanza. Potential participants were contacted by telephone and asked to participate in the study. Those that agreed were then recruited for the study. Eligibility criteria for TH included age ≥18 years and registration to practice in Tanzania. All healers were registered as herbalists. Clinical providers and patients with hypertension were recruited at the clinic by the study team. Outpatients with hypertension were eligible to participate in the study if they were aged 18 years and above, fluent in Kiswahili, and able to provide informed consent. Clinical providers were invited to participate in the study if they were employees of the outpatient hypertension clinic at one of the three hospitals where participants were recruited. Sample size for this study was determined by prior studies indicating thematic saturation of homogenous groups is reached with the completion of 9 to 15 interviews (Hennink et al., Citation2017).
Data collection
Between April and June 2020, 14 traditional healers were invited to participate in a single semi-structured interview. Four Tanzanian research assistants with Bachelor’s degrees in social science, trained in qualitative data collection, and fluent in both Kiswahili and English conducted interviews. Interviews were conducted using a semi-structured interview guide that focused on the following topics: (1) traditional health beliefs and knowledge about HTN; (2) traditional and biomedical strategies to manage HTN and (3) relationships between traditional and biomedical providers. Three interview guides were created and tailored for a single stakeholder group.
Data management and analysis
Tanzanian translators fluent in both Kiswahili and English transcribed audio recordings verbatim in Kiswahili and then translated into English. Authors EP and GK reviewed Kiswahili and English transcripts for translational integrity. Five authors (RA, MP, RS, GK, EP) independently reviewed the English transcripts. Interviews were coded using a priori codes reflecting major components of the Behavioural Model of Health Services use, developed by Andersen (R. Andersen, Citation1968; R. M. Andersen, Citation1995). Coded segments were compared to maximise the reliability of the coding process and the trustworthiness of the analysis. Discrepancies in coding were resolved through consensus such that all coded segments were agreed upon by the five-author coding team.
Andersen’s model was designed to elucidate the utilisation of health services and to help in the development of equitable health systems by drawing attention to both patient-related and contextual determinants of health behaviours (Health Behaviour and Health Education, 2008). It has been more recently updated to include focus on vulnerable populations (Gelberg et al., Citation2000). The Behavioural Model of Health Services use has been widely used to inform qualitative evaluations of health services in global settings (Lederle et al., Citation2021). As such, we selected this theoretical framework to inform our study. We organised qualitative interview content into major categories that correspond to the following domains of the Andersen model: (1) environment; (2) population characteristics; (3) health behaviour and (4) health outcomes. We further distilled codes within each of these categories through repeated engagement with the data set to ensure the validity of results. Representative quotations were selected to illustrate the study findings.
Ethical consideration
This study received ethics approvals from the Medical Research Coordinating Committee (MRCC) in Tanzania (Protocol no. NIMR/HQ/R.8a/Vol. IX/3349) and Weill Cornell Medicine (Protocol no. 19-11021145X). All participants provided written informed consent to participate in audio-recorded interviews. A copy of the signed consent form was given to them for their records. All participants were assigned a de-identified study ID number to maximise confidentiality. All interviews were conducted in private locations. At the completion of the interview, each participant received 10,000 Tanzanian Shillings ($4 USD) as compensation for their time to participate in the study, in accordance with Tanzanian national ethics guidelines.
Results
Participant characteristics are shown in . Most participants were male and married. Approximately half of the participants were Christian (as opposed to Muslim) and completed primary school education or less. The mean age of respondents was 47 years old. Our results are organised by major domains from Andersen’s model as follows. First, environment considers factors about healthcare systems, economic climate and prevailing social norms. Population characteristics refer to demographics, health beliefs, education, and enabling factors and needs of a population. Health behaviour encompasses personal health practices and the use of health services. Finally, health outcomes reflect perceived and evaluated health status and satisfaction with health services. Major themes are summarised in .
Figure 1. Major themes from the data organised according to the Andersen model of healthcare utilisation.
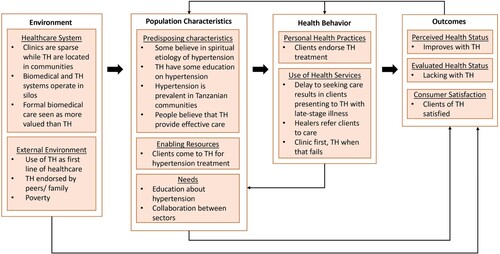
Table 1. Participant’s socio-demographic characteristics.
Environment
Healthcare system
The healthcare system domain refers to pragmatic or structural components of the healthcare landscape that can facilitate or deter engagement with healthcare services for hypertension. The healthcare system in Tanzania is comprised of both formal biomedical clinics and informal TH practices. Formal medical clinics may be sparsely distributed, making them difficult to reach, particularly for rural inhabitants. In contrast, TH practices are located in communities and more accessible to their clients.
Those in town find it easy to go to the hospital, and for those in the village it is easy for them to go for the traditional treatment. – Male TH, age 32
A lot of people go to traditional healers and take traditional medicine to treat hypertension, and some are my neighbors. – Male patient, age 77
I do not prefer attending the clinic because I usually use traditional medicine and also due to prolonged processes when I visit the clinic. – Male patient, age 49
TH and clinicians noted that the traditional and biomedical systems operate in silos. Many TH felt that their knowledge and expertise were not appreciated by biomedical providers.
There are barriers between these two groups. Biomedical workers do not take us seriously because they believe we are not educated. We do not know what we are doing, and our treatments do not work … They believe because they went to medical school [they] cannot collaborate with a person who did not go to any school. As traditional healers, we respect them and their profession because they know a lot about causes, symptoms, and treatments of diseases. – Female TH, age 29
Further, many TH describe feeling marginalised, and that formal biomedical care was seen as more valued than their treatments.
The role of traditional medicine has been hidden. It has been infringed … It has no place because our connection with the Ministry of Health is very weak … People have been made to believe that traditional medicine is associated with demons and sometimes the ministry of health tell the people that the medicines from the traditional healers are harmful. – Male TH, age 39
In some cases, TH considered their marginalisation a historical consequence of colonialism, with traditional medicine being devalued through association with satanism.
Traditional medicines treat this disease [hypertension]. Many have been reluctant to use it because of the common belief that once you use traditional medicine, you are satanic. This was the system created by whites, who wanted to promote their own products while devaluing ours for the sake of business. – Male TH, age 41
A nurse agreed that she did not trust TH because their practices and treatments were not formally regulated by the Tanzanian government, in contrast to biomedicine.
In fact, I haven’t done much research on that [traditional medicine]. I can’t lie, and I don’t find them [TH] helpful because I don’t believe in traditional medications. I often use hospital medicines that have been certified by the Tanzania Bureau of Standards. – Female Nurse, age 30
External environment
The external environment considers factors outside the healthcare system that may influence healthcare-seeking behaviour including prevailing social norms, and socioeconomic status of communities and individuals. Patients described TH as a consistent part of the healthcare landscape who frequently served the first line of healthcare. Even biomedical providers agreed that preferential use of TH was typical in sub-Saharan Africa:
We live in an African society in which traditionalism is part and parcel of our culture. Those guys [TH] are more trusted than the biomedical services. – Male doctor, age 49
It is clear that our ancestors used traditional medicine in their daily life. – Male patient, age 62
Further, the use of TH for the treatment of hypertension was endorsed by patients’ peers and family members. Peer recommendations were considered impactful in motivating the receipt of traditional care.
Most patients who start using traditional treatments have been told [by family or friends that] traditional medicine is a more effective treatment for hypertension. We do not persuade patients, but they decide on themselves which is the best treatment. – Female TH, age 29
Sometimes people tell me, ‘You have taken that [allopathic] medicine for a long time, but you don’t seem to improve. Try to use traditional medicine’. – Female patient, age 70
When [the patient] told people he has hypertension, they advised him to use traditional medicine. – Female nurse, age 32
Poverty was described as an important environmental factor motivating the use of TH. When people could not afford clinic-based care, TH serve as a more feasible option:
People do not have money and now the cost of hospitals is high. So, many sick people turn to traditional healers. – Male TH, age 50.
Most people believe in traditional medicine rather than hospital medication. The higher cost involved in hospital medication makes them use traditional medicine. – Female nurse, age 34
[The patient] didn’t have money to pay for his treatment. That’s why he decided to use traditional medicine because, for him, they were cheaper. – Female doctor, age 55
Population characteristics
Predisposing characteristics
Predisposing characteristics include knowledge, health beliefs and other psychosocial characteristics that may shape understanding and utilisation of services for hypertension. Hypertension was perceived as a prevalent disease within Mwanza’s communities and seen as especially problematic for those living in rural areas.
It is dangerous … it is not a recent problem. It has been in existence for a long time and many people have lost their lives. It had made us who live in rural areas to suffer so much … In our language we used to call it “umuna” meaning that someone with hypertension may have symptoms like nose and mouth bleeding or even [bleeding] through the eyes. So, hypertension can occur in different forms, and the form depends on how serious the hypertension is. – Male TH, age 39
Before we started using hospitals and modern medicine, we had this disease [hypertension] in the community … People used herbal medicines. – Male patient, age 62
Hypertension is a common disease now, and anyone can get hypertension, either young or old. – Male patient, age 49
Most healers attributed knowledge about hypertension from experience caring for clients with hypertension. However, some healers referenced academic textbooks, information sharing from other TH, and educational sessions provided by the Ministry of Health and biomedical healthcare workers as their sources of knowledge.
There is one doctor that I met, and he gave me a book … [which has] a large number of diseases in it. So, when the patient explains symptoms of hypertension, I read the book on the part that talks about hypertension and make a comparison between the patient’s explanation and what the book is saying – Male TH, age 62.
Likely due to a lack of common source of knowledge and training, there was a range of understanding of the aetiology and pathophysiology of hypertension among our participating TH. Some TH explained hypertension mirroring biomedical models of disease.
One of the causes [of hypertension] can be due to certain types of foods, body weight or someone may be born with heart disease. There are those who are born with heart problems, but there are those who develop the disease because of the lifestyle. – Male TH, age 45.
Many TH also understood that hypertension is a chronic disease without a cure that must be managed over a lifetime.
Yes, this disease is dangerous especially because we still don't have the cure. Instead, we only have treatment to reduce symptoms. The body must get used to those medicines and make the disease chronic, until it causes death. – Male TH, age 41
TH also reported that some clients attributed hypertension to spiritual causes. This also concern motivated some clients to seek care from TH specifically, rather than from biomedical facilities:
There are other kind of hypertension that are being caused by devils … They can cause hypertension. You would find [the systolic blood pressure] reading as 280, but the person is still walking around. – Male TH, age 32
There are many patients, especially those who believe the source of their hypertension is witchcraft. They usually go to the traditional healers. – Female patient, age 55
Traditional therapies for hypertension were sometimes perceived as superior to biomedical ones because traditional medicines were believed to have curative potential.
I think the difference with biomedical treatment [for hypertension] is that a patient has to continue taking medication for the rest of their life. But with traditional medicine a patient will take medication in a short period of time, and they will be cured. – Female TH, age 29
Enabling resources
Enabling resources are determinants of healthcare seeking, such as convenience or previous use, that motivate the utilisation of health services for hypertension. TH reported that patients tended to seek their care because they employ a patient-centred approach to disease management, examining individual risk factors for hypertension for each patient.
The first thing I would look at what caused the hypertension. If the problem is caused by severe stress or anger, the first treatment for him before taking any medicine is counseling. If hypertension has been caused by the food he is eating, I will focus my advice on food. – Male TH, age 50
Needs
Needs include both subjective and objective needs regarding hypertension care. One TH explicitly mentioned the need to dispel the belief of hypertension as being caused by devils.
People lack education on hypertension. Sometimes when people have [hypertension] they think that they have been bewitched. This is because when this disease comes to you, it comes with many symptoms. – Male TH, age 45
Additionally, many TH commented on the need for collaboration between biomedical providers and TH to improve patient care. Some TH called on improved governmental support in the form of funding, validation of traditional medicine, removing the stigma around TH, increased funding for mass production of traditional medicine and research support. Other TH saw collaboration as a necessity to improve care for their hypertensive patients. There was a call to formally integrate TH into biomedical health centres and for formalised educational opportunities for THs.
We should have a committee that will consist of herbalists and medical doctors … then there won’t be any controversy of where and how to treat the patient because all doctors will consult each other on how to take care of each person. – Male TH, age 47.
TH frequently advocated for multimodal management of hypertension.
There should be collaboration and good working relationship between traditional healers and hospital doctors. I mean, once the patient has got some tests done at the hospital, they should bring him to the right place where he will get proper treatment for hypertension. – Male TH, age 30
Health behaviour
Personal health practices
Some patients strongly endorsed the use of traditional medicines for the treatment of hypertension. This was due to the perception that traditional medications did not have harmful side effects, and therefore could be taken without reservation.
We usually take [traditional medicine] without considering the amount to be taken or required because we believe that it has no toxin, which can harm the body if taken excessively. – Male patient, age 70
Some [patients] decide to use traditional medicine. They have been told that hospital medications are poisoning their body. – Female nurse, age 42
Use of health services
TH often described receiving clients with symptoms of hypertensive emergency, or late-stage illness. In these instances, TH would refer their clients to hospitals.
The patients shouldn't wait until they are at their worst stage … If he stays without treatment for a long time, he will be in serious condition, and he might die. – Male TH, age 55
It is challenging especially when a patient has arrived in a critical condition and sometimes may complain about having blurred vision, fast heartbeat, or severe exhaustion in the extent that they are unable to move. That is a challenge. But in order to help the patient you can take him to hospital or call his relatives to take him to the hospital – Male TH, age 46
Sometimes you can go to a traditional healer, who tells you that you need to go to the hospital for this problem. – Male patient, age 60
For less critically ill clients, TH would explain to them that their hypertension could be treated with traditional medicines or at clinic-based facilities. TH would leave it to their client to decide which modality of care to use.
I will tell them, ‘I have medicine to treat hypertension but also hospitals have hypertension treatments so it is your choice as a patient to choose the treatment that you will prefer.’ – Male TH, age 35
Healers described other instances in which clients would initially present to biomedical clinics for hypertensive care, but when hospital treatment did not improve their symptoms, they sought out traditional medicines.
Most people go directly to the hospital, but when they go to the hospital and use the medicine from the hospital and see that they don't get better, then they start looking for an alternative place to go to. – Male TH, age 39
After that [acute care at the emergence department], they [patient's relatives] took him [patient] to a traditional healer who was using herbal medicine. – Female nurse, age 42
Outcomes
Perceived health status
Perceived health status refers to how individuals subjectively understand their health status about hypertension. Some TH clients perceive successful symptom management using traditional medicines after biomedical treatments had failed.
The patient … was told that he has hypertension. So, he was prescribed with some medications and started to use them … I gave him the task of going back again for the checkup and bring me the results. When he brought the results, I realized that he still had hypertension, so I gave him [herbal] medication. After using the medicine for the time I had prescribed, he came back and told me the symptoms that he used to have disappeared. – Male TH, age 45
In contrast, hospital treatments were sometimes described as not improving perceived status health.
Our roles are to provide treatment to our patients, and we need support from the Government because until the patients come to my clinic they have already gone to hospital for treatments without any relief. – Male TH, age 35
Evaluated health status
Evaluated health status considers how objective measures of health impact the utilisation of healthcare services for hypertension. Some biomedical patients did not endorse using traditional medicines. Often, these patients doubted TH because they lacked formal diagnostic testing and could not objectively treat or evaluate health conditions.
I have never been to a traditional healer. Personally, I don’t believe in them and their treatments. They do not have proper therapies because they don’t have any medical tests. – Male patient, age 60
A traditional healer cannot prescribe the medication according to your illness and may treat you differently; you can get another problem rather than recover. – Female patient, age 62
The problem with traditional healers is that they have no specific measurement for their medication – Female patient, age 56
Consumer satisfaction
Consumer satisfaction refers to people’s contentment following the utilisation of health services for hypertension. Patients often felt satisfied with TH and their treatment. This satisfaction was typically based on improved symptoms following TH treatment.
Before coming to the hospital, I was sick, and I went to a traditional healer. And they [TH] gave me medication, and I did get better. – Male patient, age 77
Yeah, it [traditional medicine] helps me because if I take it, I will stay for an extended time without feeling any problem arising from hypertension. – Female patient, age 55
Discussion
In this study, we sought to elucidate knowledge and attitudes about hypertension from Tanzanian TH as well as develop an understanding of factors driving TH utilisation among people with hypertension. We found that patients with hypertension routinely seek care from TH, and TH are considered a ubiquitous component of the healthcare landscape in Tanzania. However, TH often operate independently of the biomedical healthcare system. Biomedical providers may have negative perceptions of TH that are not reciprocated. Further, TH were described as preferential by patients due to convenient locations of their practices and perceived improvement of hypertension symptoms with traditional medicines. Lastly, TH expressed a desire for more formal collaboration with biomedicine to improve patient care. These data can inform strategies to improve the diagnosis and management of hypertension in similar settings where outcomes are currently suboptimal.
Our data provide further insight into the complex relationship between traditional and biomedical health systems. All TH in our study held biomedicine in high regard and often considered themselves informally collaborating with biomedicine. TH deferred to the use of biomedicine to establish the diagnosis of hypertension, disease progression and treatment effectiveness. TH described a deep respect for biomedicine and referred patients to seek biomedical treatment in case of hypertensive emergency. This finding is consistent with other studies that have shown ethnomedical health care is supportive of biomedicine and welcomes collaboration to improve patient care (Schausberger et al., Citation2021; Sieverding & Beyeler, Citation2016). Despite this, many TH perceive bias and discrimination against them from biomedical providers who consider traditional healing illegitimate. These findings are similar to those from Mozambique, where TH had generally positive opinions of biomedicine, though frequently reported being mistreated by medical providers (Sundararajan et al., Citation2021). This barrier to collaboration is well-documented in other African countries outside of Tanzania (Audet et al., Citation2013; James et al., Citation2018; Krah et al., Citation2018). Consequently, addressing biomedical providers’ prejudice against TH may be transformative in the design and structure of future public health interventions, and could optimally support patients who are willing to seek care across health systems (Hoyler et al., Citation2018).
Additionally, interviewed healers were in support of further collaboration with biomedicine, and many had ideas for formal collaboration and implementation of this collaboration. There are scant examples of strategies to create integrative health systems in the literature (Appiah et al., Citation2018; Kwame, Citation2021; Mwaka et al., Citation2018). Historically, integration of TH into the biomedical system has been seen as controversial, as studies have shown that TH use leads to delay of appropriate medical care in sub-Saharan Africa (Appelbaum Asuzu et al., Citation2019; Belisle et al., Citation2015; Moshabela et al., Citation2011, Citation2017; Shippee et al., Citation2013). While our data do show that TH patients may present symptomatic and in advanced stages of the disease, our qualitative data do not suggest TH themselves provide counseling or recommendations that create delays to care. Many healers reported that their patients first presented to biomedical clinics and seek TH services after feeling unsatisfied with the services and care offered at biomedical facilities. However, because traditional and allopathic health systems exist in silos, patients easily fall through the cracks and can suffer deleterious outcomes.
Our findings are also pertinent to the shortage of formal healthcare workers in sub-Saharan Africa, which has led to the exploration of ‘task shifting’ for the management of chronic conditions (Afriyie et al., Citation2019; Limbani et al., Citation2019). Recent studies have shown task shifting is effective in hypertension management and control by utilising religious leaders and non-physician clinic support staff (Anand et al., Citation2019; Lee et al., Citation2016; Limbani et al., Citation2019; Vedanthan et al., Citation2020). Similarly, TH are effective adherence support workers in providing HIV care (Audet et al., Citation2017). In conjunction with prior studies that have established TH as preferred providers for more convenient and culturally competent care (Sundararajan et al., Citation2020; Sundararajan et al., Citation2021), continued patient use of TH may provide a powerful avenue for hypertension-focused intervention as well. Like religious leaders, TH may be considered ‘trusted messengers’ in their communities who can improve hypertension management (Anyan & Knizek, Citation2018; Lambert et al., Citation2021; Limbani et al., Citation2019). With training, TH can provide support by promoting hypertension education, counseling, and referral. Further research is needed to study the effects of utilising TH as part of the formal treatment cascade in Tanzania and regions where their use is common.
Limitations
We acknowledge certain limitations of this study. As an exploratory qualitative study, it lacks the power of causal relationship but aids in the development of important contextual knowledge when considering implementation strategies. Qualitative research is meant to be highly contextual and drive hypothesis generation. While data is from a sample of healers in the Mwanza region of Tanzania, we believe our findings will be consistent among this stakeholder group and are supported by quantitative data from different regions where traditional medicine is practiced. By using a priori codes from the Andersen Model, we recognise that emerging themes may not have been captured in our analysis. We hope that our findings will guide future work on this topic using a phenomenological or grounded theory approach. Lastly, traditional healers included in this study were registered as herbalists. Though herbalists are the most common form of traditional healers, other types of traditional healers may be present with differing experiences and perspectives.
Conclusion
Tanzanian TH understand that hypertension is a serious disease and commonly provide care to hypertensive clients. TH could be partners to improve community awareness of hypertension, and support clients in hypertension care. Our findings can guide future interventions to address hypertension in Tanzanian communities that could include traditional healers.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Deidentified study data may be shared upon reasonable request to the corresponding author.
Additional information
Funding
References
- Afriyie, D. O., Nyoni, J., & Ahmat, A. (2019). The state of strategic plans for the health workforce in Africa. BMJ Global Health, 44(Suppl 9), e001115. https://doi.org/10.1136/bmjgh-2018-001115
- Anand, T. N., Joseph, L. M., Geetha, A. V., Prabhakaran, D., & Jeemon, P. (2019). Task sharing with non-physician health-care workers for management of blood pressure in low-income and middle-income countries: A systematic review and meta-analysis. The Lancet Global Health, 7(6), e761–e771. https://doi.org/10.1016/S2214-109X(19)30077-4
- Andersen, R. (1968). A behavioral model of families' use of health services. Research Series, 25. Chicago: Center for Health Administration Studies, University of Chicago.
- Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter?. Journal of Health and Social Behavior, 36(1), 1–10. https://doi.org/10.2307/2137284
- Anyan, F., & Knizek, B. L. (2018). The coping mechanisms and strategies of hypertension patients in Ghana: The role of religious faith, beliefs and practices. Journal of Religion and Health, 57(4), 1402–1412. https://doi.org/10.1007/s10943-017-0517-7
- Appiah, B., Amponsah, I. K., Poudyal, A., & Mensah, M. L. K. (2018). Identifying strengths and weaknesses of the integration of biomedical and herbal medicine units in Ghana using the WHO Health Systems Framework: A qualitative study. BMC Complementary and Alternative Medicine, 18(1), 286. https://doi.org/10.1186/s12906-018-2334-2
- Asuzu, C. C., Akin-Odanye, E. O., Asuzu, M. C., & Holland, J. (2019). A socio-cultural study of traditional healers role in African health care. Infectious Agents and Cancer, 14(1), 15. https://doi.org/10.1186/s13027-019-0232-y
- Audet, C. M., Salato, J., Blevins, M., Amsalem, D., Vermund, S. H., & Gaspar, F. (2013). Educational intervention increased referrals to allopathic care by traditional healers in three high HIV-prevalence rural districts in Mozambique. PLOS ONE, 8(8), e70326. https://doi.org/10.1371/journal.pone.0070326
- Audet, C. M., Salato, J., Vermund, S. H., & Amico, K. R. (2017). Adapting an adherence support workers intervention: Engaging traditional healers as adherence partners for persons enrolled in HIV care and treatment in rural Mozambique. Implementation Science, 12(1), 50. https://doi.org/10.1186/s13012-017-0582-z
- Azizah, N., Halimah, E., Puspitasari, I. M., & Hasanah, A. N. (2021). Simultaneous Use of herbal medicines and antihypertensive drugs Among hypertensive patients in the community: A review. Journal of Multidisciplinary Healthcare, 14, 259–270. https://doi.org/10.2147/JMDH.S289156
- Belisle, A., Hennink, H., Ordóñez, M., John, C. E., Ngubane-Joye, S., Hampton, E., Sunpath, J., Preston-Whyte, H., Marconi, E., & C, V. (2015). Concurrent use of traditional medicine and ART: Perspectives of patients, providers and traditional healers in Durban, South Africa. Global Public Health, 10(1), 71–87. https://doi.org/10.1080/17441692.2014.967709
- Bovet, P., Gervasoni, J.-P., Mkamba, M., Balampama, M., Lengeler, C., & Paccaud, F. (2008). Low utilization of health care services following screening for hypertension in Dar es Salaam (Tanzania): A prospective population-based study. BMC Public Health, 8(1), 407. https://doi.org/10.1186/1471-2458-8-407
- Chow, C. K., Teo, K. K., Rangarajan, S., Islam, S., Gupta, R., Avezum, A., Bahonar, A., Chifamba, J., Dagenais, G., Diaz, R., Kazmi, K., Lanas, F., Wei, L., Lopez-Jaramillo, P., Fanghong, L., Ismail, N. H., Puoane, T., Rosengren, A., Szuba, A., … PURE (Prospective Urban Rural Epidemiology) Study investigators. (2013). Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA, 310(9), 959–968. https://doi.org/10.1001/jama.2013.184182
- Ferdinand, K. C., Yadav, K., Nasser, S. A., Clayton-Jeter, H. D., Lewin, J., Cryer, D. R., & Senatore, F. F. (2017). Disparities in hypertension and cardiovascular disease in blacks: The critical role of medication adherence. The Journal of Clinical Hypertension, 19(10), 1015–1024. PRIME. https://doi.org/10.1111/jch.13089
- Forouzanfar, M. H., Liu, P., Roth, G. A., Ng, M., Biryukov, S., Marczak, L., Alexander, L., Estep, K., Hassen Abate, K., Akinyemiju, T. F., Ali, R., Alvis-Guzman, N., Azzopardi, P., Banerjee, A., Bärnighausen, T., Basu, A., Bekele, T., Bennett, D. A., Biadgilign, S., … Murray, C. J. L. (2017). Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA, 317(2), 165–182. https://doi.org/10.1001/jama.2016.19043
- Frimpong, E., & Nlooto, M. (2019). Tswana traditional health practitioners’ perspectives on the management of diabetes and hypertension: A qualitative study using focus group discussions. Pan African Medical Journal, 34(93), Article 93. https://doi.org/10.11604/pamj.2019.34.93.19112
- Gelberg, L., Andersen, R. M., & Leake, B. D. (2000). The Behavioral Model for Vulnerable Populations: Application to medical care use and outcomes for homeless people. Health Services Research, 34(6), 1273–1302.
- Glanz, K., Rimer, B. K., & Viswanath, K. (Eds.). (2008). Health behavior and health education: Theory, research, and practice, 4th ed (pp. xxxiii, 552). Jossey-Bass.
- Global Burden of Diseases. (2015). Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England), 386, 2287–2323. https://doi.org/10.1016/S0140-6736(15)00128-2
- Goma, F., Prasha, L., Kalungia, C. A., Bwalya, A., Hamachil, A., Mutati, R. K., Zingani, E., Mwila, C., & Musoke, P. (2017). Extraction and demonstration of uterotonic activity from the root of steganotaenia araliacea hochst. Medical Journal of Zambia, 44(3), Article 3. https://doi.org/10.55320/mjz.44.3.80
- Hennink, M. M., Kaiser, B. N., & Marconi, V. C. (2017). Code saturation versus meaning saturation Qualitative Health Research, 27(4), 591–608. https://doi.org/10.1177/1049732316665344
- Hoyler, E., Martinez, R., Mehta, K., Nisonoff, H., & Boyd, D. (2018). Beyond medical pluralism: Characterising health-care delivery of biomedicine and traditional medicine in rural Guatemala. Global Public Health, 13(4), 503–517. https://doi.org/10.1080/17441692.2016.1207197
- Hughes, G. D., Aboyade, O. M., Clark, B. L., & Puoane, T. R. (2013). The prevalence of traditional herbal medicine use among hypertensives living in South African communities. BMC Complementary and Alternative Medicine, 13(1), 38. https://doi.org/10.1186/1472-6882-13-38
- James, P. B., Wardle, J., Steel, A., & Adams, J. (2018). Traditional, complementary and alternative medicine use in Sub-Saharan Africa: A systematic review. BMJ Global Health, 3(5), e000895. https://doi.org/10.1136/bmjgh-2018-000895
- Kavishe, B., Biraro, S., Baisley, K., Vanobberghen, F., Kapiga, S., Munderi, P., Smeeth, L., Peck, R., Mghamba, J., Mutungi, G., Ikoona, E., Levin, J., Bou Monclús, M. A., Katende, D., Kisanga, E., Hayes, R., & Grosskurth, H. (2015). High prevalence of hypertension and of risk factors for non-communicable diseases (NCDs): A population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Medicine, 13(1), 126. https://doi.org/10.1186/s12916-015-0357-9
- Kim, J. K., Kim, K. H., Shin, Y. C., Jang, B.-H., & Ko, S.-G. (2020). Utilization of traditional medicine in primary health care in low- and middle-income countries: A systematic review. Health Policy and Planning, 35(8), 1070–1083. https://doi.org/10.1093/heapol/czaa022
- Kolling, M., Winkley, K., & von Deden, M. (2010). "For someone who's rich, it's not a problem". Insights from Tanzania on diabetes health-seeking and medical pluralism among Dar es Salaam's urban poor. Globalization and Health, 6(1), 8. https://doi.org/10.1186/1744-8603-6-8
- Krah, E., de Kruijf, J., & Ragno, L. (2018). Integrating traditional healers into the health care system: Challenges and opportunities in rural northern Ghana. Journal of Community Health, 43(1), 157–163. https://doi.org/10.1007/s10900-017-0398-4
- Kwame, A. (2021). Integrating traditional medicine and healing into the Ghanaian mainstream health system: Voices from within. Qualitative Health Research, 31(10), 1847–1860. https://doi.org/10.1177/10497323211008849
- Lambert, V. J., Kisigo, G. A., Nzali, A., Laizer, E., Paul, N., Walshe, L., Kalokola, F., Okello, E. S., Sundararajan, R., Mwakisole, A. H., Downs, J. A., & Peck, R. N. (2021). Religious leaders as trusted messengers in combatting hypertension in rural Tanzanian communities. American Journal of Hypertension, 34(10), 1042–1048. https://doi.org/10.1093/ajh/hpab080
- Lassale, C., Gaye, B., Diop, I. B., Mipinda, J. B., Kramoh, K. E., Kouam Kouam, C., Ikama, M. S., Takombe, J. L., Damorou, J. M., Toure, I. A., Balde, D. M., Dzudie, A., Houenassi, M., Kane, A., Kimbally-Kaki, S. G., Kingue, S., Limbole, E., Mfeukeu Kuate, L., Ferreira, B., … Jouven, X. (2022). Use of traditional medicine and control of hypertension in 12 African countries. BMJ Global Health, 7(6), e008138. https://doi.org/10.1136/bmjgh-2021-008138
- Lederle, M., Tempes, J., & Bitzer, E. M. (2021). Application of Andersen’s behavioural model of health services use: A scoping review with a focus on qualitative health services research. BMJ Open, 11(5), e045018. https://doi.org/10.1136/bmjopen-2020-045018
- Lee, E. S., Vedanthan, R., Jeemon, P., Kamano, J. H., Kudesia, P., Rajan, V., Engelgau, M., & Moran, A. E. (2016). Quality improvement for cardiovascular disease care in low- and middle-income countries: A systematic review. PLOS ONE, 11(6), e0157036. https://doi.org/10.1371/journal.pone.0157036
- Limbani, F., Thorogood, M., Gómez-Olivé, F. X., Kabudula, C., & Goudge, J. (2019). Task shifting to improve the provision of integrated chronic care: Realist evaluation of a lay health worker intervention in rural South Africa. BMJ Global Health, 4(1), e001084. https://doi.org/10.1136/bmjgh-2018-001084
- Liwa, A., Roediger, R., Jaka, H., Bougaila, A., Smart, L., Langwick, S., & Peck, R. (2017). Herbal and alternative medicine use in Tanzanian adults admitted with hypertension-related diseases: A mixed-methods study. International Journal of Hypertension, 2017(5692572). https://doi.org/10.1155/2017/5692572
- Liwa, A. C., Smart, L. R., Frumkin, A., Epstein, H.-A. B., Fitzgerald, D. W., & Peck, R. N. (2014). Traditional herbal medicine use among hypertensive patients in sub-Saharan Africa: A systematic review. Current Hypertension Reports, 16(6), 437. https://doi.org/10.1007/s11906-014-0437-9
- Marten, M. G. (2022). The countersyndemic potential of medical pluralism among people living with HIV in Tanzania. Global Public Health, 17(6), 957–970. https://doi.org/10.1080/17441692.2021.1882529
- Meli, J., Nkeh-Chungag, B. N., Doumtsop Tatou, J. G., Mope, J. S., & Kingue, S. (2009). Perceptions of the etiology and treatment of hypertension among some traditional healers in Cameroon. The Open Public Health Journal, 2(1), 39–43. https://doi.org/10.2174/1874944500902010039
- Ministry of Health. (2018). Mohcdec. Standard treatment guidelines and essential medicines lists for children and adolescents. Republic of Tanzania, Ministry of Health, Community Development, Gender, Elderly and Children.
- Moshabela, M., Bukenya, D., Darong, G., Wamoyi, J., McLean, E., Skovdal, M., Ddaaki, W., Ondeng’e, K., Bonnington, O., Seeley, J., Hosegood, V., & Wringe, A. (2017). Traditional healers, faith healers and medical practitioners: The contribution of medical pluralism to bottlenecks along the cascade of care for HIV/AIDS in Eastern and Southern Africa. Sexually Transmitted Infections, 93(Suppl 3). https://doi.org/10.1136/sextrans-2016-052974
- Moshabela, M., Pronyk, P., Williams, N., Schneider, H., & Lurie, M. (2011). Patterns and implications of medical pluralism Among HIV/AIDS patients in rural South Africa. AIDS and Behavior, 15(4), 842–852. https://doi.org/10.1007/s10461-010-9747-3
- Mwaka, A. D., Tusabe, G., Orach Garimoi, C., & Vohra, S. (2018). Turning a blind eye and a deaf ear to traditional and complementary medicine practice does not make it go away: A qualitative study exploring perceptions and attitudes of stakeholders towards the integration of traditional and complementary medicine into medical school curriculum in Uganda. BMC Medical Education, 18(1), 310. https://doi.org/10.1186/s12909-018-1419-4
- Nnko, S., Bukenya, D., Kavishe, B. B., Biraro, S., Peck, R., Kapiga, S., Grosskurth, H., & Seeley, J. (2015). Chronic diseases in north-west Tanzania and southern Uganda. Public perceptions of terminologies, aetiologies, symptoms and preferred management. PLOS ONE, 10(11), e0142194. https://doi.org/10.1371/journal.pone.0142194
- Oke, D. A., & Bandele, E. O. (2004). Misconceptions of hypertension. Journal of the National Medical Association, 96(9), 1221–1224.
- Osamor, P. E., & Owumi, B. E. (2010). Complementary and alternative medicine in the management of hypertension in an urban Nigerian community. BMC Complementary and Alternative Medicine, 10(1), 36. https://doi.org/10.1186/1472-6882-10-36
- Oyebode, O., Kandala, N.-B., Chilton, P. J., & Lilford, R. J. (2016). Use of traditional medicine in middle-income countries: A WHO-SAGE study. Health Policy and Planning, 31(8), 984–991. https://doi.org/10.1093/heapol/czw022
- Peck, R. N., Green, E., Mtabaji, J., Majinge, C., Smart, L. R., Downs, J. A., & Fitzgerald, D. W. (2013). Hypertension-related diseases as a common cause of hospital mortality in Tanzania. Journal of Hypertension, 31(9), 1806–1811. https://doi.org/10.1097/HJH.0b013e328362bad7
- Schausberger, B., Mmema, N., Dlamini, V., Dube, L., Aung, A., Kerschberger, B., Ciglenecki, I., Vambe, D., Mukooza, E., & Wringe, A. (2021). “We have to learn to cooperate with each other”: a qualitative study to explore integration of traditional healers into the provision of HIV self-testing and tuberculosis screening in Eswatini. BMC Health Services Research, 21(1), 1314. https://doi.org/10.1186/s12913-021-07323-1
- Schutte, A. E., Srinivasapura Venkateshmurthy, N., Mohan, S., & Prabhakaran, D. (2021). Hypertension in low- and middle-income countries. Circulation Research, 128(7), 808–826. https://doi.org/10.1161/CIRCRESAHA.120.318729
- Seedat, Y. (2015). Why is control of hypertension in sub-Saharan Africa poor? Cardiovascular Journal of Africa, 26(4), 193–195. https://doi.org/10.5830/CVJA-2015-065
- Shippee, T., Henning-Smith, C., Shippee, N., Pintor, J. K., Call, K. T., McAlpine, D., & Johnson, P. J. (2013). Discrimination in medical settings and attitudes toward complementary and alternative medicine: The role of distrust in conventional providers. 6(1).
- Sieverding, M., & Beyeler, N. (2016). Integrating informal providers into a people-centered health systems approach: Qualitative evidence from local health systems in rural Nigeria. BMC Health Services Research, 16(1), 526. https://doi.org/10.1186/s12913-016-1780-0
- Sundararajan, R., Langa, P. V., Morshed, T., & Manuel, S. (2021a). Traditional healers as client advocates in the HIV-endemic region of Maputo, Mozambique: Results from a qualitative study. SAHARA – Journal of Social Aspects of HIV/AIDS, 18(1), 77–85. https://doi.org/10.1080/17290376.2021.1909492
- Sundararajan, R., Mwanga-Amumpaire, J., King, R., & Ware, N. C. (2020). Conceptual model for pluralistic healthcare behaviour: Results from a qualitative study in southwestern Uganda. BMJ Open, 10(4), e033410. https://doi.org/10.1136/bmjopen-2019-033410
- Sundararajan, R., Ponticiello, M., Lee, M. H., Strathdee, S. A., Muyindike, W., Nansera, D., King, R., Fitzgerald, D., & Mwanga-Amumpaire, J. (2021b). Traditional healer-delivered point-of-care HIV testing versus referral to clinical facilities for adults of unknown serostatus in rural Uganda: A mixed-methods, cluster-randomised trial. The Lancet Global Health, 9(11), e1579–e1588. https://doi.org/10.1016/S2214-109X(21)00366-1
- United Republic of Tanzania. (n.d.) The Traditional and Alternative Medicine Act, 23.
- Vedanthan, R., Kamano, J. H., Bloomfield, G. S., Manji, I., Pastakia, S., & Kimaiyo, S. N. (2015). Engaging the entire care cascade in western Kenya: A model to achieve theCardiovascular disease secondary prevention roadmap goals. Global Heart, 10(4), 313–317. https://doi.org/10.1016/j.gheart.2015.09.003
- Vedanthan, R., Kumar, A., Kamano, J. H., Chang, H., Raymond, S., Too, K., Tulienge, D., Wambui, C., Bagiella, E., Fuster, V., & Kimaiyo, S. (2020). Effect of nurse-based management of hypertension in rural western Kenya. Global Heart, 15(1), Article 1. https://doi.org/10.5334/gh.856
- World Health Organization. (2019). WHO global report on traditional and complementary medicine 2019. World Health Organization. https://apps.who.int/iris/handle/10665/312342.
