Abstract
Purpose
The purpose of this case series was to explore the influence of powered wheelchair standing device (PWSD) use on participants’: (1) activities and participation; (2) quality of life; and (3) lower extremity passive range of motion (LE PROM).
Case description
Eight participants enrolled in the case series (five adults and three children). Outcome measures included: the Canadian Occupational Performance Measure (COPM), the EQ-5D-5L or the EQ-5D-Y, the Patient-Assessment of Constipation Quality of Life Questionnaire (PAC-QOL), LE PROM measurements and PWSD use data automatically collected by each PWSD. Participants were provided with a front wheel-drive PWSD designed for both outdoor and indoor use for up to 12-months of use.
Outcomes
Four participants completed the 12-month case series. Three participants achieved clinically significant improvements in performance on the COPM. Three of the four participants reporting issues with constipation achieved clinically significant improvements in their total PAC-QOL scores. Almost all participants demonstrated changes in some LE PROM.
Conclusions
Applying the Human Activity Assistive Technology model may help to explain differences in both PWSD use and outcomes amongst the individual participants in this case series. The participants who were most successful in using the PWSD were in environments with sufficient space to use the PWSD to perform everyday activities and had higher frequencies of PWSD use. The outcomes of this case series may assist both researchers and clinicians when implementing future PWSD studies recommending PWSDs to their clients/patients.
A wide variety of factors may influence powered wheelchair standing device (PWSD) use.
PWSD use may lead to improvements in activities, participation, quality of life and lower extremity passive range of motion.
The participants who were most successful in using the PWSD were in environments that permitted use of the PWSD during the performance of everyday activities.
COVID-19 restrictions prohibited in-person sessions with a therapist, which could have assisted participants in better integrating the PWSD in their daily lives.
Implications for rehabilitation
A powered wheelchair standing device (PWSD), defined as a powered wheelchair with an integrated, electronic standing feature, provides individuals with the opportunity to stand, and permits them to drive in either sitting or standing [Citation1–3]. The components of a PWSD are configured to meet the unique needs of each individual user, and, depending on the specific type of PWSD, may include coming into standing from either supine or sitting, and allowing either full or partial extension of the hips and knees in standing [Citation2,Citation4]. As such, a PWSD affords individuals the freedom to stand whenever and wherever they desire [Citation1], thereby providing them opportunities to perform activities within the vertical plane and interact with others in a face-to-face manner [Citation1,Citation2,Citation5].
In both children and adults who have neurological conditions, the strongest evidence supports weight bearing within a supported standing position as a means to improve joint mobility in the hip, knees and ankles, and reduce the risk of lower extremity contractures [Citation6,Citation7]. Standing may further help to improve bone health in the lower extremities and spine, and reduce lower extremity spasticity [Citation6,Citation7]. Evidence from lower level research studies suggests other possible benefits of standing including improved bladder and bowel function, increased muscle strength, increased wakefulness, improved participation in activities of daily living (ADLs), enhanced psychological well-being and higher quality of life [Citation6–8]. Evidence from two systematic reviews [Citation7,Citation9] recommends children and adults who have neurological conditions to stand for a minimum of 30–60 min per day, five days per week to achieve the potential benefits of standing [Citation7,Citation9].
In a qualitative study exploring the use of stationary standers in children with cerebral palsy (CP), stationary standers were perceived to allow children to participate in activities they otherwise could not, such as standing to cook or wash the dishes [Citation10]. Limitations to using the stationary standers were also identified and included the need to transfer from wheelchair into the standing frame, a task that often involved at least two people to safely perform [Citation10]. The need to transfer into the standing frame also meant that the children could not stand when and where they wanted [Citation1].
In contrast to stationary standers, standing in a PWSD does not require individuals to transfer into another piece of equipment [Citation1]. Additional functional, emotional, psychosocial, social and health benefits have been specifically attributed to PWSD use [Citation1,Citation2,Citation4,Citation5,Citation11]. A non-randomized, stepped wedge study involving 14 adolescents with Duchenne muscular dystrophy (DMD) reported mental health benefits and maintenance of musculoskeletal status over the first 20 weeks of PWSD use [Citation11]. A single-case design investigating the effects of 6- to 12-months of PWSD use in four boys with DMD found improved hip or knee flexor muscle length in three of the four participants, and identified an array of functional improvements stemming from standing in a PWSD (be able to stand to: eat at a high table with siblings, access the freezer and higher shelves in a refrigerator, to urinate, put things away in kitchen drawers, and play catch with a dog) [Citation4]. Although these studies provide some insights into PWSD use by boys with DMD, they do not reflect PWSD use in children or adults with other conditions.
To begin addressing this knowledge gap, this longitudinal case series, carried out over a period of up to 12 months, explored PWSD use related to a number of factors. This publication specifically reports the influence of PWSD use on participants’ [Citation1]: activities and participation [Citation2]; quality of life; and [Citation3] lower extremity passive range of motion (LE PROM). Participants’ patterns of PWSD use (frequency of device use, frequency and duration of standing, etc.) were also assessed. The project was approved by the Scientific Ethics Committee of the Central Denmark Region (case no. 1-10-72-249-19). Consent to participate in the case series was obtained from adult participants whereas parental permission and assent were obtained from child participants. In addition, the case series was conducted in compliance with the General Data Protection Regulation (European Union) 2016/679.
Case descriptions
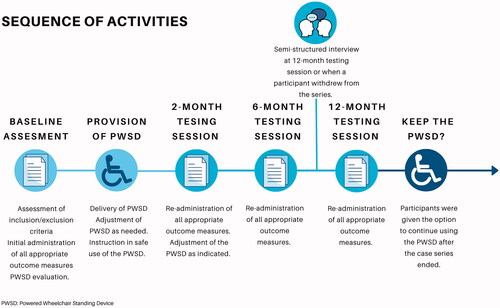
This case series involved providing participants with a PWSD and following them for up to 1 year of PWSD use. outlines the sequence of activities and the three testing sessions conducted during the series. Potential participants were residents of Central Region of Denmark identified through municipality records and through specialized rehabilitation centres in the area. Inclusion criteria related to having mobility limitations necessitating power wheelchair use; an inability to stand without upper extremity support or aids; being able to safely use and stand in a PWSD; and having the cognition and visual skills to support safe PWSD use. Exclusion criteria related to experiencing orthostatic hypotension when standing, requiring a highly customized seating system (to accommodate scoliosis, lack of head control, etc.), the inability to follow instructions regarding safety, and any other factor that would preclude safe PWSD use. If osteoporosis was known or suspected, the participant was referred to their primary physician to have a dual energy X-ray absorptiometry (DEXA) scan and obtain a medical certificate to participate in the case series. A licenced physiotherapist (the first author) and a complex rehabilitation technology (CRT) provider, who was an employee of the PWSD manufacturer, worked in partnership to determine if the specific PWSD used in the case series, a Permobil F5 Corpus VS (Permobil, AB, Timrå, Sweden), could be set-up to meet the specific needs of each potential participant. The municipality reimbursed the manufacturer for the CRT provider’s time. Final decisions regarding potential participants’ ability to safely use the PWSD were made by the licenced physiotherapist.
Figure 1. Sequence of activities in the case series.
Outcome measures
The outcome measures used included: the Danish language version of the Canadian Occupational Performance Measure (COPM) [Citation12,Citation13], the Danish language version of the EQ-5D-5L (for adult participants) [Citation14] or the EQ-5D-Y (for child participants) [Citation15,Citation16] or the EQ-5D-Y proxy version 1 (for children age <8) [Citation17], the Danish language version of the Patient-Assessment of Constipation Quality of Life Questionnaire (PAC-QOL) [Citation18] for participants reporting issues with constipation at the onset of the series, and LE PROM measurements obtained via goniometry [Citation19–25]. Data regarding PWSD use (frequency of standing, angle of standing, etc.) were automatically collected by each PWSD through Permobil Connect (Permobil, AB, Timrå, Sweden) [Citation26]. Capturing such data directly from the device itself provided a unique opportunity to explore actual PWSD use patterns, rather than relying on participants to complete device use diaries. provides descriptions and available psychometric information for each outcome measure. The initial COPM interview was conducted by an occupational therapist experienced in the use of the COPM whilst all LE PROM measurements were obtained by a physiotherapist experienced in the clinical use of the Danish Physiotherapy Association’s standards for measurement [Citation20,Citation23,Citation24]. Testing sessions were scheduled to be performed at baseline, after a 2-month adjustment period of PWSD use, and after 6 months and 12 months of PWSD use; however, restrictions related to the COVID-19 pandemic prevented some testing sessions from occurring. Missed testing sessions due to COVID are indicated in the tables and figures provided in the results section.
Table 1. Descriptions of outcome measures.
In addition to the above testing, after 12 months of PWSD use, or upon a participant’s withdrawal from the case series, participants (if able based on their communication abilities and preferences), participants’ regular therapists, participants’ care assistants, and the parents of child participants were invited to partake in an audio-recorded, semi-structured qualitative interview. Interview questions pertained to experiences and perceptions of PWSD use are provided for each stakeholder group in Appendix 1. Interviews were recorded and conducted either in-person or via Microsoft Teams by the first author, a physiotherapist with 5 years of experience working with children and adults who have physical disabilities. Recordings were transcribed verbatim and de-identified as appropriate.
Intervention
The municipality purchased the PWSDs used in the case series. Participants were provided with a Permobil F5 Corpus VS, a front wheel-drive PWSD designed for both outdoor and indoor use that can be driven in either sitting or standing. The Permobil F5 Corpus VS, shown in , provides a standing position of 45–85° and allows users to transition into standing from either a sitting or supine position. A licenced physiotherapist (the first author) and a CRT provider, worked in partnership with each participant to perform a PWSD evaluation at the onset of the case series. The seating system and the set-up of each participant’s PWSD were customized to meet their individual needs.
Figure 2. The powered wheelchair standing device in sitting and standing. The powered wheelchair standing device allows users access to the vertical plane.

Participants were advised to use the PWSD standing feature at least five times per week for a duration of 30–60 min to achieve the health effects of the standing position [Citation7,Citation9]. Following an initial 2-month adjustment period, each participant was supposed to regularly partake in-person training sessions with an occupational therapist to work on integrating PWSD use, and the PWSD standing feature, into daily life. Restrictions related to the COVID-19 pandemic prevented these training sessions from occurring. As such, participants did not receive any in-person training or support.
Interpretation of outcomes
Changes in baseline COPM scores for each participant were assessed across administrations for clinically significant change in performance using methods outlined in the COPM manual [Citation13] (i.e., an increase of two points in performance was considered clinically significant). Changes in baseline total PAC-QOL scores were assessed using the minimal important difference value of −0.5 points for the total PAC-QOL scores as identified by Marquis et al. [Citation18].
Participant outcomes
Eight participants were enrolled in the case series: five adults (three men and two women, ages 24–74 years) and three children (all girls, ages 8–17 years). An additional participant, participant 6 (an adult), completed baseline testing before it was determined that they would be unable to safely use a PWSD. Therefore, participant 6 was removed from the case series. Two other participants had not stood in many years and were required to undergo a DEXA scan and obtain medical clearance to participate in the case series. Two of the child participants lived at home with their parents during the case series, whilst the third lived at a residential school. Of the adult participants, three lived in their own homes during the case series, one lived in a support apartment program and one lived in a residential facility. Demographics (age, diagnosis, years of wheelchair use, etc.) at the onset of the case series are provided in .
Table 2. Participant demographics at the onset of the case series.
Participants’ duration of PWSD use
Participants 1, 2, 3 and 9 completed the 12-month case series. During the case series, participant 1 underwent a surgical procedure to address toe alignment and reduce toe pain. This resulted in her not using the PWSD for 2 months. Participants 1 and 3 elected to continue using their PWSD after the completion of the case series and were still using their PWSD when this manuscript was written.
Participant 8 used the PWSD for 2 months, was withdrawn from the case series (and discontinued PWSD use), due to health issues resulting in significant hypotension. Participants 4, 5 and 7 discontinued their PWSD use after 6 months. These participants’ reasons for electing to discontinue PWSD use varied. Participant 4 lived in an apartment with limited accessibility and planned to use the PWSD primarily in his accessible workspace and in the community. When COVID-19 restrictions were instituted, he was unable to go to work or be out in the community. Participant 5 felt the footprint of the PWSD was larger than his existing power wheelchair, which he felt impeded his use of the PWSD both at home and in the community. Participant 7 required frequent adjustments to the PWSD and related seating system. When COVID-19 restrictions were instituted, these adjustments could not be made.
Adverse event
One adverse event was reported during the case series. Participant 1 sustained a hairline femur fracture during routine adjustment of the standing feature of the PWSD following one month of PWSD use. She underwent medical treatment to address the fracture and did not use the PWSD for 2 months. Once cleared by a physician to resume PWSD use, the participant elected to resume use of the PWSD within the case series until she underwent toe surgery as noted above.
The influence of PWSD use on participants’ activities and participation
As shown in , at baseline, participants identified a wide variety of occupational performance issues in areas pertaining to cooking, gardening, shopping, housework, work activities, reaching objects on high shelves, etc. across the 2, 6 and 12-month re-administrations of the COPM. Participants 3 and 9 achieved clinically significant improvement in performance on four out of five occupational performance issues. Participant 5 achieved clinically significant improvement on one of five occupational performance issues across the 2 and 6-month re-administrations. Participants 4 and 7 each experienced non-significant clinical change in one occupational performance issue. COPM scores for participants 1 and 2 remained relatively stable across the 12-month period of the case series.
Table 3. Canadian Occupational Performance Measure [Citation11,Citation12] ratings at 2, 6 and 12 months.
The qualitative interview provided additional insights into the influence of the PWSD on participants’ activities and participation. Participant 1 used the standing feature to assist family members with household chores (sorting laundry, cooking) and to hug her mother as noted in the following quote (translated into English):
At home, when I got up and gave my mom a hug…it was just so nice, because then suddenly, I was on the same height with her and could look her in the eye.
She also reported that driving in standing also allowed her to assist with chores more easily. Participant 2 used the standing feature when interacting with small groups of friends at school and to reach objects without assistance. The parents of participant 3 reported that using the PWSD allowed their daughter to get a glass of water by herself, stand whenever she wanted, and stand to play games at home (table football or play with a balloon). Participant 3 enjoyed that the PWSD allowed her to be at eye level with her peers. Participant 9 reported that standing after meals improved his digestion. Several interviews mentioned the size of the PWSD as a potential barrier to carrying out regular everyday activities, that they previously had performed in their previous wheelchairs as exemplified by the following quote (translated into English):
(Because of the size of the PWSD base), I can’t just take a glass of water. I can’t just take a plate. I can’t just make something to eat. Because I can’t get to the kitchen properly (anymore)…
The influence of PWSD use on participants’ on participants’ quality of life
As shown in , where a lower score indicates a better quality of life, on the Health Profile portion of the EQ-5D-Y for child participants, participant 1 reported an initial improvement in Doing usual activities at the 6-month testing session. This decreased back to baseline levels at the 12-month testing session. Participant 2 reported a decline in Looking after myself at the 6-month testing session. This improved back to baseline levels at the 12-month testing session. Participant 3 reported an initial decline in Doing usual activities at the 6-month testing session. This improved to above baseline levels at the 12-month testing session. Participant 3 also reported improvements in Feeling worried, sad or unhappy at the 12-month testing session. Across the study, none of the child participants reported changes in the Mobility or Having pain or discomfort dimensions. As provided in , on the EQ-Visual Analogue Scale (EQ-VAS) (where a score of 100 designates the best imaginable health and a score of 0 indicates the worst imaginable health), participant 1 reported a 15-point decline in global health between baseline and the 12-month testing session. Participants 2 and 3 reported an 18- and 20-point improvement, respectively, in their global health across the same testing sessions.
Figure 3. EQ-5D-Y health profile scores for participants <18 years of age. Lower scores indicate a better quality of life.
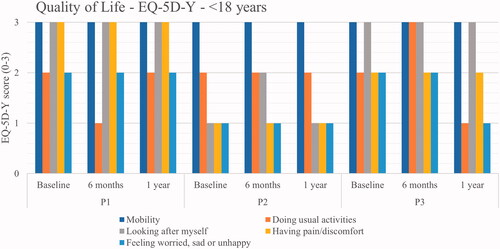
Table 4. EQ-VAS global assessment of health [Citation13, Citation14].
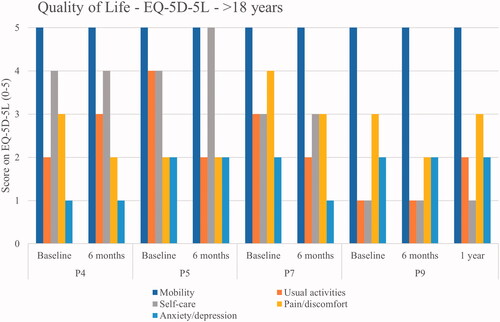
As shown in , where a lower score indicates a better quality of life, on the Health Profile portion EQ-5D-5L for adult participants, Participants 4, 5, and 7 discontinued their use of the PWSD after 6-months. At the 6-month testing session, participant 4 reported an improvement in Pain/discomfort and a decline in Usual activities at the 6-month testing session; participant 5 reported an improvement in Usual activities and a decline in Self-care at the 6-month testing session; and participant 7 reported improvements in Usual activities, Pain/discomfort and Anxiety/depression. Participant 9 reported an improvement in Pain/discomfort at the 6-month testing session. This returned to baseline levels at the 12-month testing session. In addition, participant 9 reported a decline from baseline in Usual activities at the 12-month testing session. Across the study, none of the adult participants reported changes in Mobility. As provided in , (on the EQ-VAS where a score of 100 designates the best imaginable health and a score of 0 indicates the worst imaginable health), at the 6-month testing session, participant 4 reported a 10-point decline in global health and participants 5 and 7 reported no change in global health. Participant 9 reported a 45-point improvement in global health at the 6-month testing session that was sustained through the 12-month testing session.
Figure 4. EQ-5D-5L health profile scores for participants <18 years of age. Lower scores indicate a better quality of life.
As indicated in , where a lower score indicates a better quality of life, three of the four participants (participants 1, 5 and 9) who reported issues with constipation at the onset of the series achieved clinically significant improvements in their total PAC-QOL scores between the baseline and final PAC-QOL administrations. The fourth participant’s (participant 4) total PAC-QOL score approached clinical significance.
Table 5. Patient-Assessment of Constipation Quality of Life Questionnaire scores.
The qualitative interview provided additional insights into the influence of the PWSD on participants’ quality of life. Participant 1 reported that the PWSD improved her quality of life and the ability to stand when she wanted, gave her a sense of freedom, as exemplified in the following quote (translated into English):
The thing about being able to stand up whenever you want…it gives (you) a huge (feeling of) freedom and quality of life. And it’s just nice to be able to stand up and be on the same wavelength with the others…
She further described how being in a sitting position made her feel small, but how standing in the PWSD allowed her to be at eye level with other people. Participant 3’s parents observed how happy she was driving around in the PWSD and how proud she seemed to be to show others the PWSD. Participant 3 felt the PWSD made her less dependent on adults, because she can stand up on her own more easily. Although participant 9 liked standing in the PWSD and feeling “tall again”, he also reported feeling more disabled when driving in public with the PWSD than when self-propelling in his manual wheelchair, primarily due to the joystick and headrest on the PWSD as illustrated in the following quote (translated into English):
There’s got to be some psyche and robustness in you, when you’re driving out into the world with joystick and headrest, I think – you’re seen a bit differently, you’re (seen as) a bit more disabled, and you have to be ready for that.
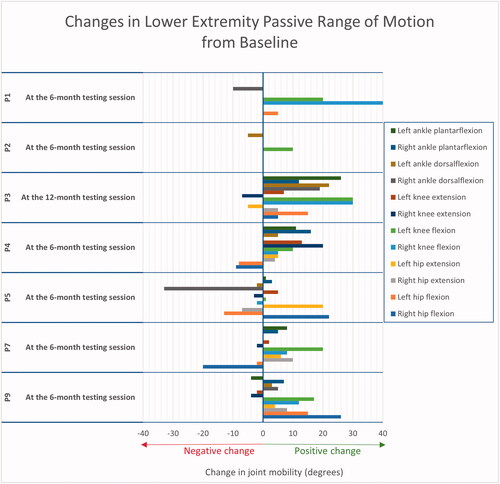
The influence of PWSD use on participants’ LE PROM
As indicated in , almost all participants demonstrated increases in some LE PROM measurements. Participants 1, 2, 3, 4, 7 and 9 gained between 5° and 40° of passive knee flexion at one or more knee. Participants 3, 4, 5, 7 and 9 gained between 5° and 20° of passive hip extension at one or more hip. Participant 3, who used the PWSD standing feature the most as reported below, demonstrated large gains in passive hip flexion, hip extension, knee flexion, ankle dorsiflexion and ankle plantarflexion, as well as a slight improvement in passive left knee extension. Participants 1, 2, 7 and 9 experienced no changes in knee extension.
Participants’ patterns of PWSD use
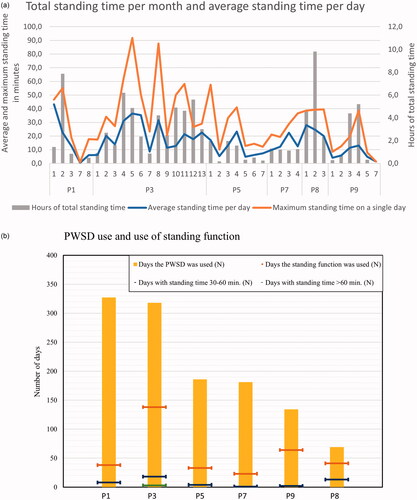
As shown in and detailed in Appendix 2, participants’ days of PWSD use, days using the standing feature, and mean duration of standing time varied. Permobil Connect data could not be analysed for participants 2 and 4 due to connectivity issues resulting in device use data not being transferred to the cloud storage service. Of the remaining participants, participant 3 used the PWSD standing feature the most and had the highest average total standing time per day. Participant 9 had the second highest use of the PWSD standing feature and stood primarily for very short periods of time. As shown in , none of the participants achieved the recommended standing dosage of at least five times per week for 30–60 min each time to achieve the health effects of the standing position [Citation7,Citation9]. Participant 3 achieved the recommended daily standing duration on 21 out of the 135 days she used the standing feature (21/135 = 15.5%). Six out of the participants stood for ≥30 min at least once during their participation in the case series.
Figure 6. (a) Total standing time per month, average standing time per day, and maximum standing time during a single day.(b) Number of days of powered wheelchair standing device use and use of the standing feature. Permobil Connect data could not be analysed for participants 2 and 4.
Discussion
This longitudinal case series has explored the influence of a PWSD on participants’ activities and participation, quality of life, and LE PROM, as well as assessed participants’ patterns of PWSD use. The COPM and PAC-QOL appeared to effectively capture outcomes of PWSD use. The Permobil Connect data also effectively captured PWSD use in all but two participants. Although quick and easy to administer, the specific emphasis on “walking” in the mobility item on the EQ-5D-5L and the EQ-5D-Y limited the effectiveness of these measures in capturing outcomes of wheelchair use. Future versions of the EQ-5D-5L and the EQ-5D-Y should consider modifying the mobility item to include wheelchair use. In addition, the use of the EQ-5D-Y via caregiver proxy, i.e., the caregiver ratings were based on their own perceptions of their child’s health-related quality of life, must be used, and interpreted in light of the potential for proxy-respondent bias [Citation17,Citation27,Citation28].
The goal of providing an assistive technology device, such as a PWSD, is to enable a user to maximize their function and independence within the contexts of their daily life. Yet, within this case series, differences in both PWSD use and outcomes were observed amongst the individual participants. The innovative Human Activity Assistive Technology (HAAT) model [Citation29,Citation30] provides a way to explore both assistive technology adoption and rejection. As such, the HAAT may help to explain and understand these observed differences by examining the interaction of four key elements: the human, the assistive technology device, the activity and the context.
When viewed through the lens of the HAAT, the human element in this case series was represented by each of the individual participants; the assistive technology element by the PWSD, the activity element by each participants’ specific goals for activity and participation using the PWSD, and the contextual element by the physical, social, cultural and institutional factors faced by each specific participant during the case series.
The interaction between the participant and the PWSD
Matching mobility technology, in this case the PWSD, to the needs of the individual is an important aspect of wheelchair provision, and ultimately may determine whether implementation of a mobility device is successful [Citation1,Citation31,Citation32]. For some participants, including participants 1 and 3 who opted to continue using the PWSD after the case series, the interaction between the participant and the PWSD seems to have been successful. Furthermore, the importance of matching PWSD use to the specific medical and safety needs of each participant was further observed in participants 6 and 8, who were withdrawn from the study due to concerns related to their abilities to safety use the PWSD, and in participant 1 who sustained a hairline femur fracture.
The interaction of the device and the participants may have also influenced the amount of time a participant used the PWSD, how often they used the standing feature, and ultimately, the outcomes achieved in the study. Similar to the diary-based findings of Townsend et al. [Citation4], none of the participants in the current case series achieved the minimum recommended standing for health benefits [Citation7,Citation9]. It is possible, however, that participants in this case series used the PWSD standing feature primarily for short-duration, functional purposes as exemplified by the device use patterns exhibited by participant 9. Future studies exploring both the device-use data captured directly from the device itself and diaries regarding function are warranted.
The interaction amongst the participant, the device and context
One contextual element that may have influenced participants’ use of the PWSD, and the PWSD standing feature, was the COVID-19 pandemic. The International Classification of Function, Disability, and Health [Citation33] depicts the use of assistive technology devices, such as the PWSD and related standing feature, as both an environmental factor (the individual has the device) and a personal factor (the individual knows how to use the device). Yet, COVID-19 restrictions put in place shortly after the start of this case series prohibited the planned in-person training sessions with an occupational therapist to work on integrating PWSD use into daily life. As such, the case series reflects the participants’ use of the PWSD without any in-person support from a therapist. Young et al. [Citation34] reported on the collaborative strategies provided to support PWSD use in three cases involving the use of PWSD in boys who were termed “High Use” users (standing in the PWSD 32–42 times per week). These collaborative strategies involved an occupational therapist working with each child and family early to manage barriers and enablers to PWSD use prior to providing the PWSDs, and providing sustained intervention strategies following provision of the PWSD [Citation34].
In addition, the COVID-19 restrictions may have limited participants’ abilities to perform and partake in desired activities. As noted in , multiple participants identified occupational performance issues in the community, school and work contexts. Activities such as participating in group fitness classes or social gatherings, ordering coffee, performing tasks at work, or using the blackboard at school may have all been prohibited by COVD-19 restrictions.
Interaction amongst the participant, the device, activities and context
Several of the adult participants found the size of the PWSD to be a barrier to its use in their living spaces, making it more difficult for them to perform certain activities in their homes. Most of the adult participants had been using their previous wheelchair for more than seven years. As such, they had adapted their homes, ADLs, and habits to accommodate the height, width and length of their previous wheelchair. Changing habits and routines within ADLs to conform to a wheelchair with a larger base and different drive configuration may have been challenging for these adult participants, particularly without any in-person support from a therapist.
Participants’ motivation to use and incorporate the PWSD standing feature into their daily lives likely also played a role in the frequency at which participant’s used the device for specific activities within a particular context. Young et al. [Citation34] reported similar findings in that the three boys with DMD, who used the PWSD the most all shared a positive attitude towards the PWSD, a desire for increased autonomy in everyday life, and supportive surroundings where there was room for the PWSD [Citation34].
Limitations
As a case series lacks the control of a research study, there are many possible alternative explanations for the outcomes achieved in this series. Participants’ improved scores on the various self-reported or parent-reported outcome measures may have reflected participants and parents desires for improvements in activities, participant and quality of life. Completion of the self-reported or parent-reported measures may also have been influenced by participants’ or parents’ attitudes and values, as well as by their perceptions of their own quality of life. Although using a single type of PWSD in this case series may be viewed as a limitation, it also provided consistency in terms of the equipment used across participants. Finally, it is possible that participants may have experienced improvements in their activities, participant, quality of life and LE PROM without using a PWSD or that the seat-to-floor height or width of the wheelchair could have influenced performance of activities.
Conclusions
This case series provides insights into PWSD use in children and adults with a variety of conditions. Applying the HAAT model to explore PWSD use in this case series illustrates how something that worked well for one participant, during a specific activity completed within a particular context, may not have been successful for another participant, or a different activity, or under different contextual circumstances. The participants who were most successful in using the PWSD were in environments that permitted use of the PWSD during the performance of everyday activities. Furthermore, participants with the higher frequencies of PWSD use appeared to experience a more positive influence of PWSD use on their activities and participation, quality of life, and LE PROM. The outcomes of this case series may assist researchers in designing and implementing future PWSD studies and may guide clinicians to consider elements of the HAAT model when recommending PWSDs to their clients/patients.
Acknowledgements
The authors gratefully acknowledge Permobil for their assistance in obtaining the Permobil Connect data.
Disclosure statement
This case series was conducted within clinical practice and was supported through the municipality’s health department. The first author’s time to analyse the data and write up the article was provided as part of his employment through the municipality. The authors disclose Permobil’s assistance in obtaining the Permobil Connect data.
References
- Kenyon LK, Harrison KL, Huettner MK, et al. Stakeholder perspectives of pediatric powered wheelchair standing devices: a qualitative study. Dev Med Child Neurol. 2021;63(8):969–975.
- Dicianno BE, Morgan A, Lieberman J, et al. Rehabilitation Engineering & Assistive Technology Society (RESNA) position on the application of wheelchair standing devices: 2013 current state of the literature. Assist Technol. 2016;28(1):57–62.
- Schofield C, Evans K, Young H, et al. The development of a consensus statement for the prescription of powered wheelchair standing devices in Duchenne muscular dystrophy. Disabil Rehabil. 2022;44(10):1889–1897.
- Townsend EL, Bibeau C, Holmes TM. Supported standing in boys with Duchenne muscular dystrophy. Pediatr Phys Ther. 2016;28(3):320–329.
- Arva J, Paleg G, Lange M, et al. RESNA position on the application of wheelchair standing devices. Assist Technol. 2009;21(3):161–168.
- Glickman LB, Geigle PR, Paleg GS. A systematic review of supported standing programs. J Pediatr Rehabil Med. 2010;3(3):197–213.
- Paleg G, Smith B, Glickman L. Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs. Pediatr Phys Ther. 2013;25(3):232–247.
- Nordström B, Näslund A, Ekenberg L, et al. The ambiguity of standing in standing devices: a qualitative interview study concerning children and parents experiences of the use of standing devices. Physiother Theory Pract. 2014;30(7):483–489.
- Paleg G, Livingstone R. Systematic review and clinical recommendations for dosage of supported home-based standing programs for adults with stroke, spinal cord injury and other neurological conditions. BMC Musculoskelet Disord. 2015;16:358.
- Goodwin J, Lecouturier J, Crombie S, et al. Understanding frames: a qualitative study of young people’s experiences of using standing frames as part of postural management for cerebral palsy. Child Care Health Dev. 2018;44(2):203–211.
- Bayley K, Parkinson S, Jacoby P, et al. Benefits of powered standing wheelchair devices for adolescents with Duchenne muscular dystrophy in the first year of use. J Paediatr Child Health. 2020;56(9):1419–1425.
- Larsen AE, Morville AL, Hansen T. Translating the Canadian Occupational Performance Measure to Danish, addressing face and content validity. Scand J Occup Ther. 2019;26(1):33–45.
- Law M, Baptiste S, McColl M, et al. Canadian Occupational Performance Measure. 2nd ed. Ottawa: CAOT publications ACE; 1998.
- Feng YS, Kohlmann T, Janssen MF, et al. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res. 2021;30(3):647–673.
- Wille N, Badia X, Bonsel G, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res. 2010;19(6):875–886.
- Ravens-Sieberer U, Wille N, Badia X, et al. Feasibility, reliability, and validity of the EQ-5D-Y: results from a multinational study. Qual Life Res. 2010;19(6):887–897.
- Perez Sousa MÁ, Olivares Sánchez-Toledo PR, Gusi Fuerte N. Parent–child discrepancy in the assessment of health-related quality of life using the EQ-5D-Y Questionnaire. Arch Argent Pediatr. 2017;115(6):541–546.
- Marquis P, De La Loge C, Dubois D, et al. Development and validation of the Patient Assessment of Constipation Quality of Life Questionnaire. Scand J Gastroenterol. 2005;40(5):540–551.
- Gogia PP, Braatz JH, Rose SJ, et al. Reliability and validity of goniometric measurements at the knee. Phys Ther. 1987;67(2):192–195.
- Jakobsen TL, Christensen M, Christensen SS, et al. Reliability of knee joint range of motion and circumference measurements after total knee arthroplasty: does tester experience matter? Reliability of knee joint assessment. Physiother Res Int. 2010;15(3):126–134.
- Kim DH, An DH, Yoo WG. Validity and reliability of ankle dorsiflexion measures in children with cerebral palsy. BMR. 2018;31(3):465–468.
- Mutlu A, Livanelioglu A, Gunel MK. Reliability of goniometric measurements in children with spastic cerebral palsy. Med Sci Monit. 2007;13(7):CR323–CR329.
- Mätzke Rasmussen H, Torp-Pedersen L. Manual – Opfølgningsprogram for cerebral parese – Fysioterapeut protokol [Internet]. CPOP; 2014. Available from: http://www.cpop.dk/wp-content/uploads/2014.07.03-Fysioterapeut-manual.pdf
- Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry. 5th ed. Philadelphia: F.A. Davis Company; 2016. 571 pp.
- Elveru RA, Rothstein JM, Lamb RL. Goniometric reliability in a clinical setting. Phys Ther. 1988;68(5):672–677.
- Permobil. Information about Permobil Connect [Internet]; 2022 [cited 2022 Feb 23]. Available from: https://www.permobil.com/en-us/products/power-wheelchairs/functions/permobil-connect
- Rajmil L, López AR, López-Aguilà S, et al. Parent–child agreement on health-related quality of life (HRQOL): a longitudinal study. Health Qual Life Outcomes. 2013;11:101.
- Li M, Harris I, Lu ZK. Differences in proxy-reported and patient-reported outcomes: assessing health and functional status among medicare beneficiaries. BMC Med Res Methodol. 2015;15:62.
- Cook & Hussey’s assistive technologies: principles and practice. 3rd ed. St. Louis: Mosby Elsevier; 2008. xvi, 571 pp.
- Giesbrecht E. Application of the Human Activity Assistive Technology model for occupational therapy research. Aust Occup Ther J. 2013;60(4):230–240.
- Livingstone R, Field D. The child and family experience of power mobility: a qualitative synthesis. Dev Med Child Neurol. 2015;57(4):317–327.
- Gudgeon S, Kirk S. Living with a powered wheelchair: exploring children’s and young people’s experiences. Disabil Rehabil Assist Technol. 2015;10(2):118–125.
- World Health Organization. International Classification of Functioning, Disability and Health: ICF. Classification internationale du fonctionnement, du handicap et de la santé: CIF [Internet]; 2001. Available from: https://apps.who.int/iris/handle/10665/42407
- Young H, Bray P, McKinnon K, et al. Everyday life participation using powered wheelchair standing devices by boys with DMD. OTJR. 2021;41(3):175–184.